A Review of Smartphone Apps Used for Toric Intraocular Lens Calculation and Alignment
Abstract
:1. Introduction
2. Material and Methods
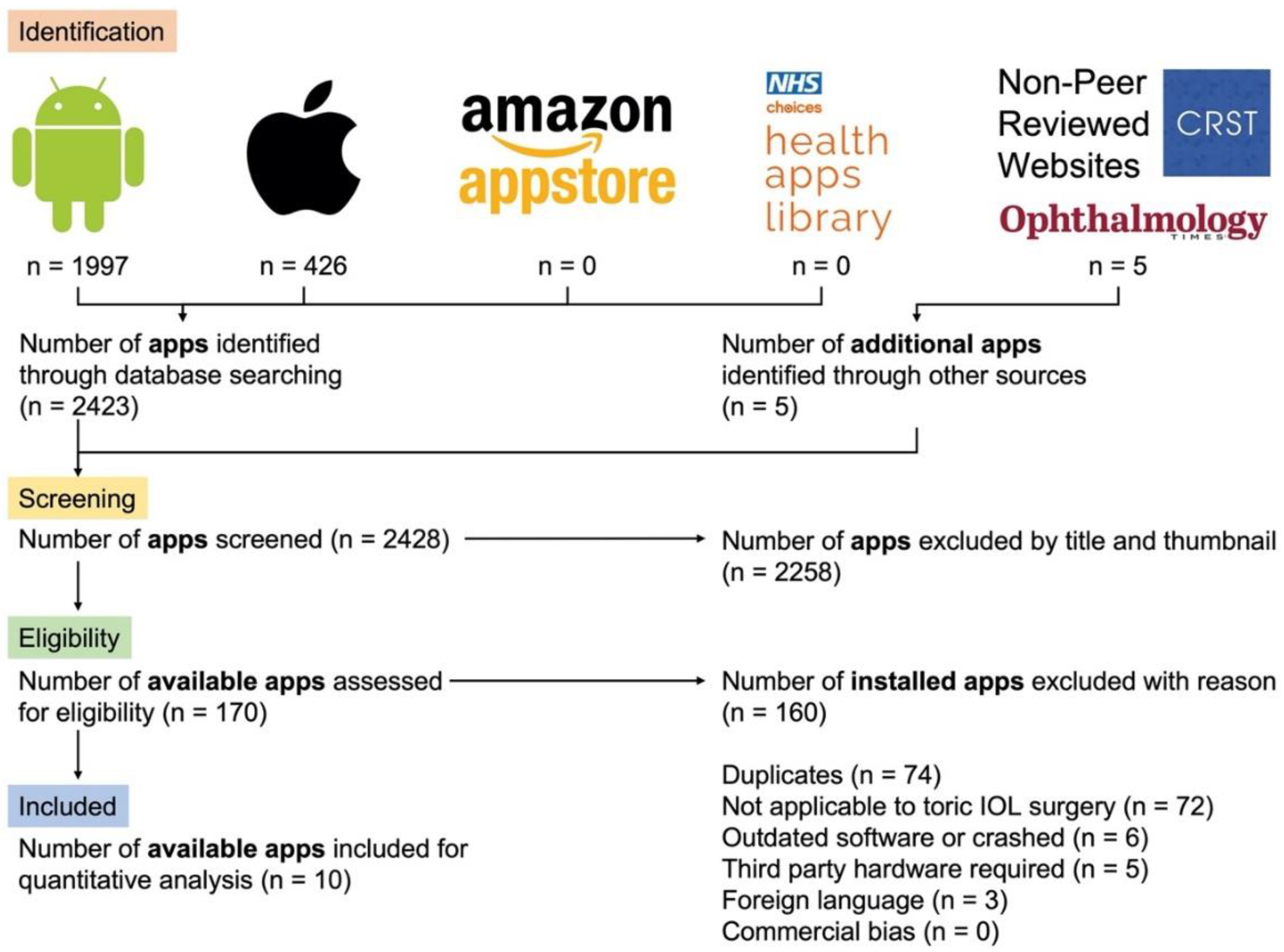
2.1. Phase I. A Review of All Available Smartphone Apps for Toric IOL Calculations and Axis Alignment
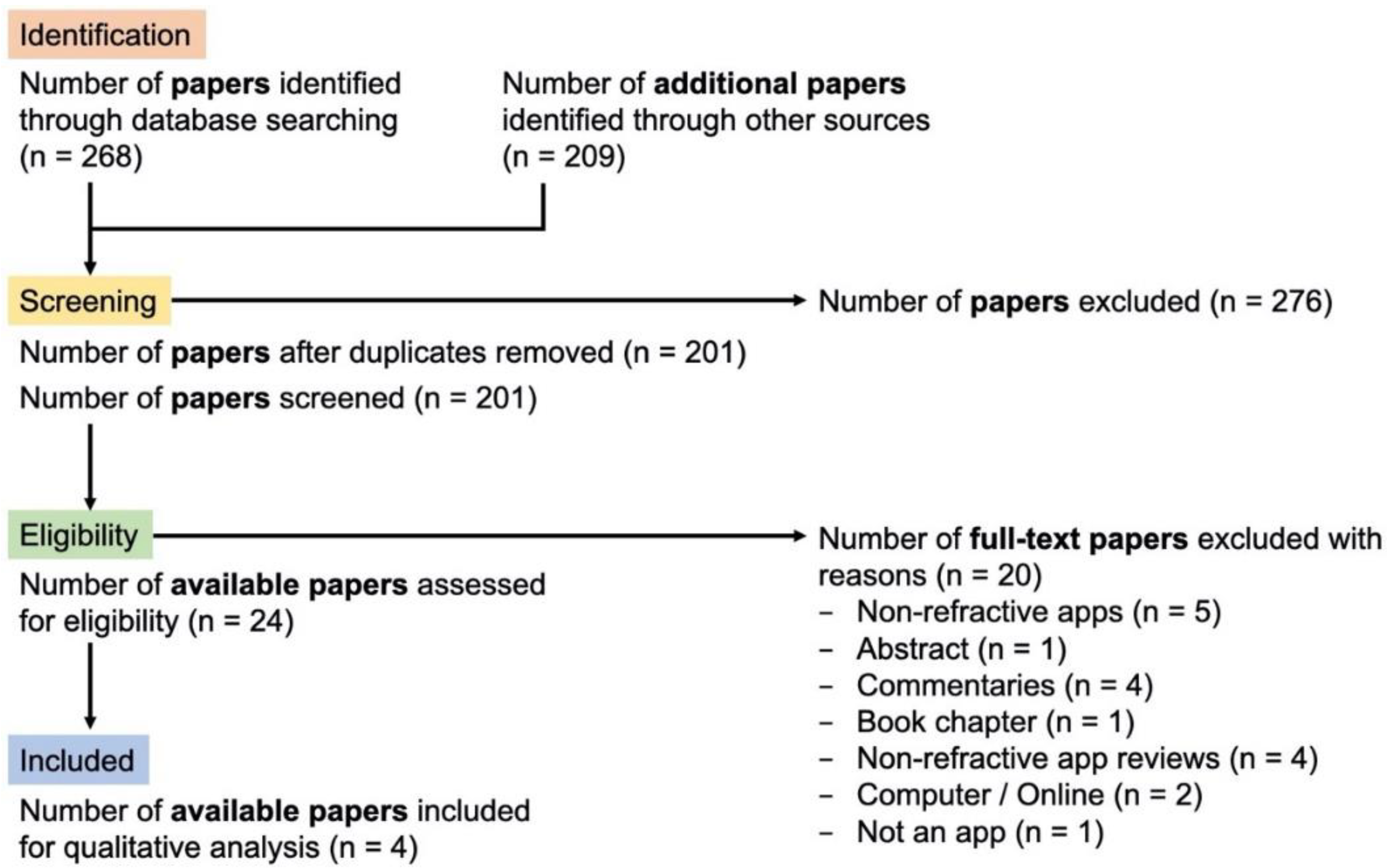
2.2. Phase II. Systematic Review to Identify Studies That Included the Smartphone Apps Identified in Phase I
2.3. Phase III. Objective Scoring of the Included Apps Using the Validated Mobile App Rating Scale (MARS)
3. Results
3.1. Phase I. A Review of All Available Smartphone Apps for Toric IOL Calculations and Axis Alignment
3.2. Phase II. Systematic Review to Identify Studies That Included the Smartphone Apps Identified in Phase I
3.3. Phase III. Objective Scoring of the Included Apps Using the Validated Mobile App Rating Scale (MARS)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nanavaty, M.A.; Bedi, K.K.; Ali, S.; Holmes, M.; Rajak, S. Toric Intraocular Lenses versus Peripheral Corneal Relaxing Incisions for Astigmatism between 0.75 and 2.5 Diopters during Cataract Surgery. Am. J. Ophthalmol. 2017, 180, 165–177. [Google Scholar] [CrossRef] [PubMed]
- Nanavaty, M.A.; Teeluck, K.; Bardan, A.S.; Bedi, K.K.; Ali, S. Residual Refractive Astigmatism following Toric Intraocular Lens Implantation without Consideration of Posterior Corneal Astigmatism during Cataract Surgery with Low Anterior Keratometric Astigmatism upto 2.5 Dioptres. Curr. Eye Res. 2019, 44, 1399–1406. [Google Scholar] [CrossRef] [PubMed]
- Kaur, M.; Shaikh, F.; Falera, R.; Titiyal, J.S. Optimizing outcomes with toric intraocular lenses. Indian J. Ophthalmol. 2017, 65, 1301–1313. [Google Scholar]
- Tognetto, D.; Perrotta, A.A.; Bauci, F.; Rinaldi, S.; Antonuccio, M.; Pellegrino, F.A.; Fenu, G.; Stamatelatos, G.; Alpins, N. Quality of images with toric intraocular lenses. J. Cataract Refract. Surg. 2018, 44, 376–381. [Google Scholar] [CrossRef] [PubMed]
- Hirnschall, N.; Findl, O.; Bayer, N.; Leisser, C.; Norrby, S.; Zimper, E.; Hoffmann, P. Sources of Error in Toric Intraocular Lens Power Calculation. J. Refract. Surg. 2020, 36, 646–652. [Google Scholar] [CrossRef]
- Oshika, T.; Inamura, M.; Inoue, Y.; Ohashi, T.; Sugita, T.; Fujita, Y.; Miyata, K.; Nakano, S. Incidence and Outcomes of Repositioning Surgery to Correct Misalignment of Toric Intraocular Lenses. Ophthalmology 2018, 125, 31–35. [Google Scholar] [CrossRef] [Green Version]
- Kim, E.C.; Hwang, K.Y.; Lim, S.A.; Yi, R.; Joo, C.-K. Accuracy of toric intraocular lens implantation using automated vs manual marking. BMC Ophthalmol. 2019, 19, 169. [Google Scholar] [CrossRef] [Green Version]
- Khatib, Z.I.; Haldipurkar, S.S.; Shetty, V. Verion digital marking versus smartphone-assisted manual marking and isolated manual marking in toric intraocular lens implantation. Indian J. Ophthalmol. 2020, 68, 455–458. [Google Scholar] [CrossRef]
- Zvornicanin, E.; Zvornicanin, J.; Hadziefendic, B. The Use of Smart phones in Ophthalmology. Acta Inform. Med. 2014, 22, 206–209. [Google Scholar] [CrossRef] [Green Version]
- Georgiou, M. Developing a Healthcare App in 2021: What Do Patients Really Want? Imaginovation. 2020. Available online: https://www.imaginovation.net/blog/developing-a-mobile-health-app-what-patients-really-want/ (accessed on 30 October 2021).
- Chhablani, J.; Kaja, S.; Shah, V.A. Smartphones in ophthalmology. Indian J. Ophthalmol. 2012, 60, 127–131. [Google Scholar]
- Moradian, S.; Safi, S. Application of Mobile Phones in Ophthalmology. J Ophthalmic Vis. Res. 2015, 10, 200–205. [Google Scholar] [CrossRef]
- Pallas, A.; Yeo, T.K.; Trevenen, M.; Barrett, G. Evaluation of the Accuracy of Two Marking Methods and the Novel toriCAM Application for Toric Intraocular Lens Alignment. J. Refract. Surg. 2018, 34, 150–155. [Google Scholar] [CrossRef] [Green Version]
- Clark, K.D. Toric intraocular lens outcomes with a new protocol for IOL selection and implantation. J. Fr. Ophtalmol. 2018, 41, 145–151. [Google Scholar] [CrossRef]
- Lipsky, L.; Barrett, G. Comparison of toric intraocular lens alignment error with different toric markers. J. Cataract Refract. Surg. 2019, 45, 1597–1601. [Google Scholar] [CrossRef] [PubMed]
- Dias, F.A.F.; Dias, V.J.F.; Dutra, B.D.A.L.; Marques, A.C.S.; Marçal, E.; Lucena, A.D.R.; Crispim Ribeiro, J. Mobile App for Pre-and Intraoperative Assessment of Astigmatism Correction with Toric Intraocular Lenses in Cataract Surgery. J. Ophthalmol. 2020, 2020, 8354140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stoyanov, S.R.; Hides, L.; Kavanagh, D.J.; Zelenko, O.; Tjondronegoro, D.; Mani, M. Mobile app rating scale: A new tool for assessing the quality of health mobile apps. JMIR mHealth uHealth 2015, 3, e27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Health Service (NHS). NHS Apps Library. 2021. Available online: https://www.nhs.uk/apps-library/ (accessed on 26 August 2021).
- Google. Google Play Store. 2021. Available online: https://play.google.com/store (accessed on 1 February 2021).
- Apple (UK). App Store. 2021. Available online: https://www.apple.com/uk/app-store/ (accessed on 1 February 2021).
- Amazon. Amazon Appstore. Available online: https://www.amazon.co.uk/mobile-apps/b?ie=UTF8&node=1661657031 (accessed on 1 February 2021).
- Ophthalmology Times. 2021. Available online: https://www.ophthalmologytimes.com/ (accessed on 1 February 2021).
- Eye News. 2021. Available online: https://www.eyenews.uk.com/ (accessed on 1 February 2021).
- Cataract & Refractive Surgery Today (CRST). CRSToday. 2021. Available online: https://crstoday.com/ (accessed on 1 February 2021).
- American Academy of Ophthalmology (AAO). For Ophthalmologists—American Academy of Ophthalmology. 2021. Available online: https://www.aao.org/ophthalmologists (accessed on 1 February 2021).
- Medscape. Ophthalmology Section. 2021. Available online: https://www.medscape.com/ophthalmology (accessed on 1 February 2021).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; British Medical Journal Publishing Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef] [Green Version]
- fnd. Experience the App Store and iTunes Anywhere. 2021. Available online: https://fnd.io/#/ (accessed on 1 February 2021).
- Milne-Ives, M.; Lam, C.; van Velthoven, M.; Meinert, E. Mobile Fitness and Weight Management Apps: Protocol for a Quality Evaluation. JMIR Res. Protoc. 2020, 9, e17685. [Google Scholar] [CrossRef]
- Mandracchia, F.; Llauradó, E.; Tarro, L.; Valls, R.M.; Solà, R. Mobile Phone Apps for Food Allergies or Intolerances in App Stores: Systematic Search and Quality Assessment Using the Mobile App Rating Scale (MARS). JMIR mHealth uHealth 2020, 8, e18339. [Google Scholar] [CrossRef] [PubMed]
- Ho, L.; Macnab, A.; Matsubara, Y.; Peterson, K.; Tsang, B.; Stothers, L. Rating of Pelvic Floor Muscle Training Mobile Applications for Treatment of Urinary Incontinence in Women. Urology 2021, 150, 92–98. [Google Scholar] [CrossRef]
- Lu, D.J.; Girgis, M.; David, J.M.; Chung, E.M.; Atkins, K.M.; Kamrava, M. Evaluation of mobile health applications to track patient-reported outcomes for oncology patients: A systematic review. Adv. Radiat. Oncol. 2021, 6, 100576. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Li, X. Effects of the aesthetic design of icons on app downloads: Evidence from an android market. Electron. Commer. Res. 2017, 17, 83–102. [Google Scholar] [CrossRef]
- Fu, B.; Lin, J.; Li, L.; Faloutsos, C.; Hong, J.; Sadeh, N. Why People Hate Your App: Making Sense of User Feedback in a Mobile App Store. In Proceedings of the 19th ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, Chicago, IL, USA, 11–14 August 2013; Association for Computing Machinery: New York, NY, USA, 2013. [Google Scholar]
- Schultz, M.; Oberheide, U.; Kermani, O. Comparability of an image-guided system with other instruments in measuring corneal keratometry and astigmatism. J. Cataract Refract. Surg. 2016, 42, 904–912. [Google Scholar] [CrossRef] [PubMed]
- Elhofi, A.H.; Helaly, H.A. Comparison Between Digital and Manual Marking for Toric Intraocular Lenses: A Randomized Trial. Medicine 2015, 94, e1618. [Google Scholar] [CrossRef] [PubMed]
- Mayer, W.J.; Kreutzer, T.; Dirisamer, M.; Kern, C.; Kortuem, K.; Vounotrypidis, E.; Priglinger, S.; Kook, D. Comparison of visual outcomes, alignment accuracy, and surgical time between 2 methods of corneal marking for toric intraocular lens implantation. J. Cataract Refract. Surg. 2017, 43, 1281–1286. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Jiang, W.; Lin, Z.; Li, X.; Li, J.; Lin, H.; Chen, W.; Wang, Q. Comparative meta-analysis of toric intraocular lens alignment accuracy in cataract patients: Image-guided system versus manual marking. J. Cataract Refract. Surg. 2019, 45, 1340–1345. [Google Scholar] [CrossRef] [PubMed]
- Daintith, J. A Dictionary of Physics, 6th ed.; Oxford University Publishing: Oxford, UK, 2009. [Google Scholar]
- Powell, A.C.; Landman, A.B.; Bates, D.W. In Search of a Few Good Apps. JAMA 2014, 311, 1851–1852. [Google Scholar] [CrossRef] [PubMed]
| Inclusion Criteria: |
|---|
|
| Exclusion Criteria: |
|
| Engagement | Entertainment, Interest, Customisation, Interactivity, Target Group |
|---|---|
| Functionality | Performance, ease of use, navigation, gestural design |
| Aesthetics | Layout, graphics, visual appeal (how good does the app look?) |
| Information quality | Accuracy of app description, goals, quality of information, visual information, credibility, evidence base |
| Subjective quality | Would you recommend this app? How many times do you think you would use this app? Would you pay for this app? What is your overall star rating of the app? |
| Mean app quality (MAQ) | The MAQ can be calculated using the mean scores of engagement, functionality, aesthetics and information quality from the objective domains above. |
| A. Summary of Toric IOL Calculation Apps (n = 6). | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rank | App Name | Operating System (OS) | Cost (GBP) | Engagement | Functionality | Aesthetics | Information Quality | Subjective Quality | Mean App Quality Score (MAQ) | App Rating 1 (1–5) | Reviews 2 (n) | Developer(s) |
| 1 | Toric Calculator for iPhone | iOS | 3.99 | 4.0 | 4.5 | 4.0 | 4.0 | 4.0 | 4.13 | - | 0 | App Developers and Industry |
| 2 | Eye Tools | iOS | 4.99 | 4.0 | 4.0 | 3.5 | 4.0 | 3.5 | 3.88 | 4.0 | 1 | App Developers and Industry |
| 3 | Biotech Calculators | Android | 0.00 | 2.5 | 3.5 | 3.5 | 3.5 | 3.0 | 3.25 | 4.7 | 17 | Industry |
| 4 | Axis Toric Calculator | Android | 0.00 | 2.5 | 4.0 | 2.5 | 3.5 | 3.0 | 3.13 | 4.6 | 8 | Industry |
| 5 | EyeToric | iOS | 0.00 | 3.0 | 3.5 | 2.5 | 3.5 | 3.0 | 3.13 | 3.2 | 5 | Ophthalmologist |
| 6 | Excellent Toric Calculator | Android | 0.00 | 2.0 | 3.0 | 2.5 | 2.5 | 2.0 | 2.50 | - | 0 | App Developers and Industry |
| B. Summary of Axis Marking Apps (n = 4). | ||||||||||||
| Rank | App Name | Operating System (OS) | Cost (GBP) | Engagement | Functionality | Aesthetics | Information Quality | Subjective Quality | Mean App Quality Score (MAQ) | App Rating 1 (1–5) | Reviews 2 (n) | Developer(s) |
| 1 | iToric Patwardhan | Android | 0.00 | 4.0 | 4.5 | 3.5 | 4.5 | 4.5 | 4.13 | 4.7 | 19 | Ophthalmologist |
| 2 | Axis Assistant | iOS | 1.99 | 3.5 | 4.0 | 3.5 | 2.5 | 2.5 | 3.38 | 3.0 | 6 | Ophthalmologist |
| 3 | toriCAM | iOS | 0.00 | 3.0 | 3.5 | 3.0 | 3.0 | 3.0 | 3.13 | 4.3 | 7 | Ophthalmologist |
| 4 | Toric IOL Axis Marker | Android | 0.00 | 2.5 | 3.5 | 3.0 | 3.0 | 2.5 | 3.00 | 3.4 | 14 | App Developers and Clinician |
| # | Authors (Year) | Country | Type of Study | Study Setting | Sample Size (No. of Patients) | Smartphone App | Purpose of App | Control(s) | Primary Outcome |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Pallas et al. (2018) | Australia | Prospective randomised | Tertiary teaching hospital | 22 | toriCAM | Axis marking for the true reference meridian | Freehand marking vs. slit-lamp-assisted marking | Preoperative reference marking for toric IOL surgery |
| 2 | Lipsky et al. (2019) | Australia | Retrospective case series | Tertiary teaching and community hospital | 56 | toriCAM | Axis marking for the true reference meridian | Barrett dual-axis toric marker vs. Mendez gauge | Postoperative alignment error in toric IOL at 1 month |
| 3 | Khatib et al. (2020) | India | Prospective observational | Tertiary Eye Hospital | 36 | iToric Patwardhan | Axis marking | Manual marking vs. smartphone-assisted marking | Preoperative reference marking for toric IOL surgery |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scantling-Birch, Y.; Naveed, H.; Mukhija, R.; Nanavaty, M.A. A Review of Smartphone Apps Used for Toric Intraocular Lens Calculation and Alignment. Vision 2022, 6, 13. https://doi.org/10.3390/vision6010013
Scantling-Birch Y, Naveed H, Mukhija R, Nanavaty MA. A Review of Smartphone Apps Used for Toric Intraocular Lens Calculation and Alignment. Vision. 2022; 6(1):13. https://doi.org/10.3390/vision6010013
Chicago/Turabian StyleScantling-Birch, Yarrow, Hasan Naveed, Ritika Mukhija, and Mayank A. Nanavaty. 2022. "A Review of Smartphone Apps Used for Toric Intraocular Lens Calculation and Alignment" Vision 6, no. 1: 13. https://doi.org/10.3390/vision6010013
APA StyleScantling-Birch, Y., Naveed, H., Mukhija, R., & Nanavaty, M. A. (2022). A Review of Smartphone Apps Used for Toric Intraocular Lens Calculation and Alignment. Vision, 6(1), 13. https://doi.org/10.3390/vision6010013






