Peripapillary Retinal Nerve Fiber Measurement with Spectral-Domain Optical Coherence Tomography in Age-Related Macular Degeneration
Abstract
:1. Introduction
2. Methods
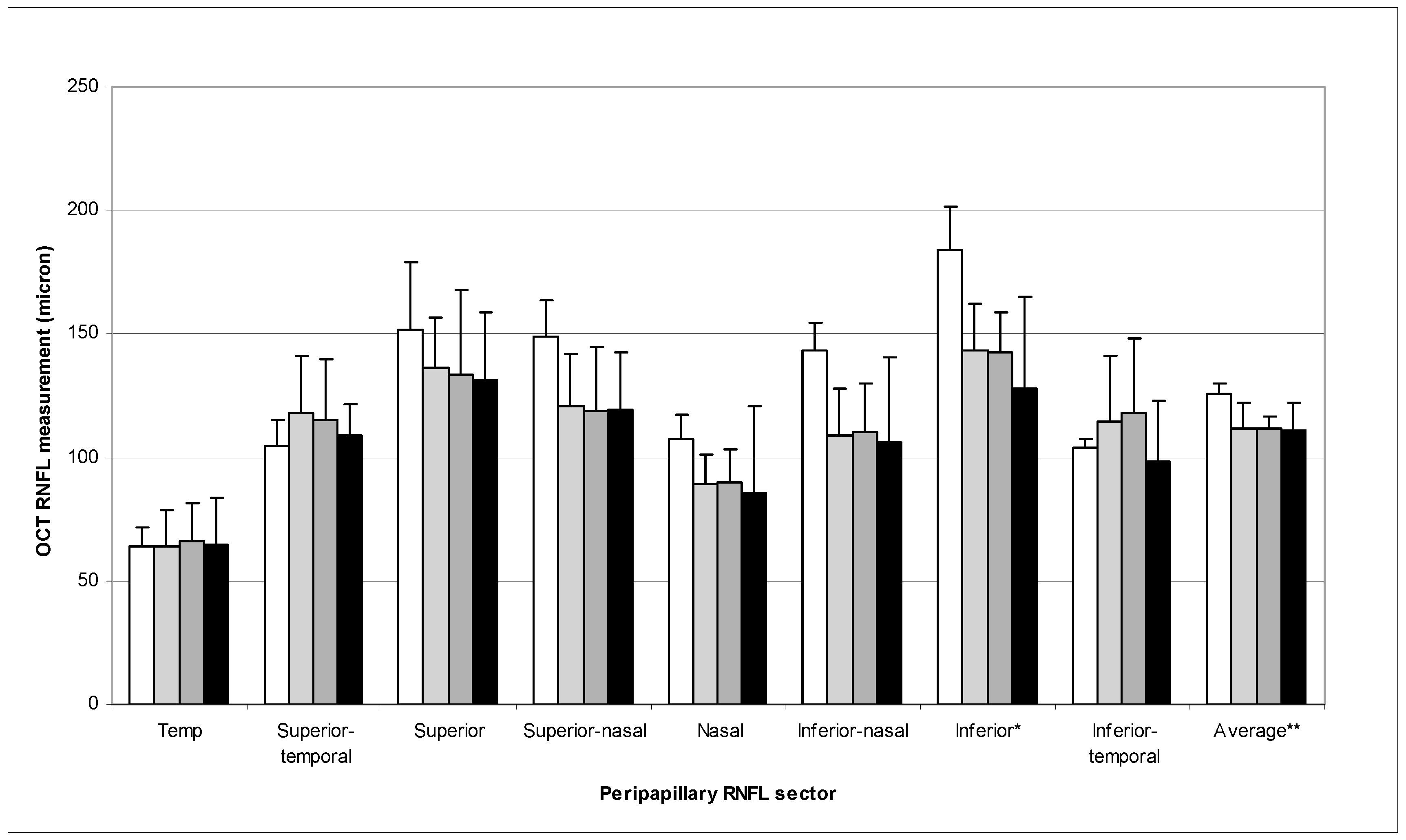
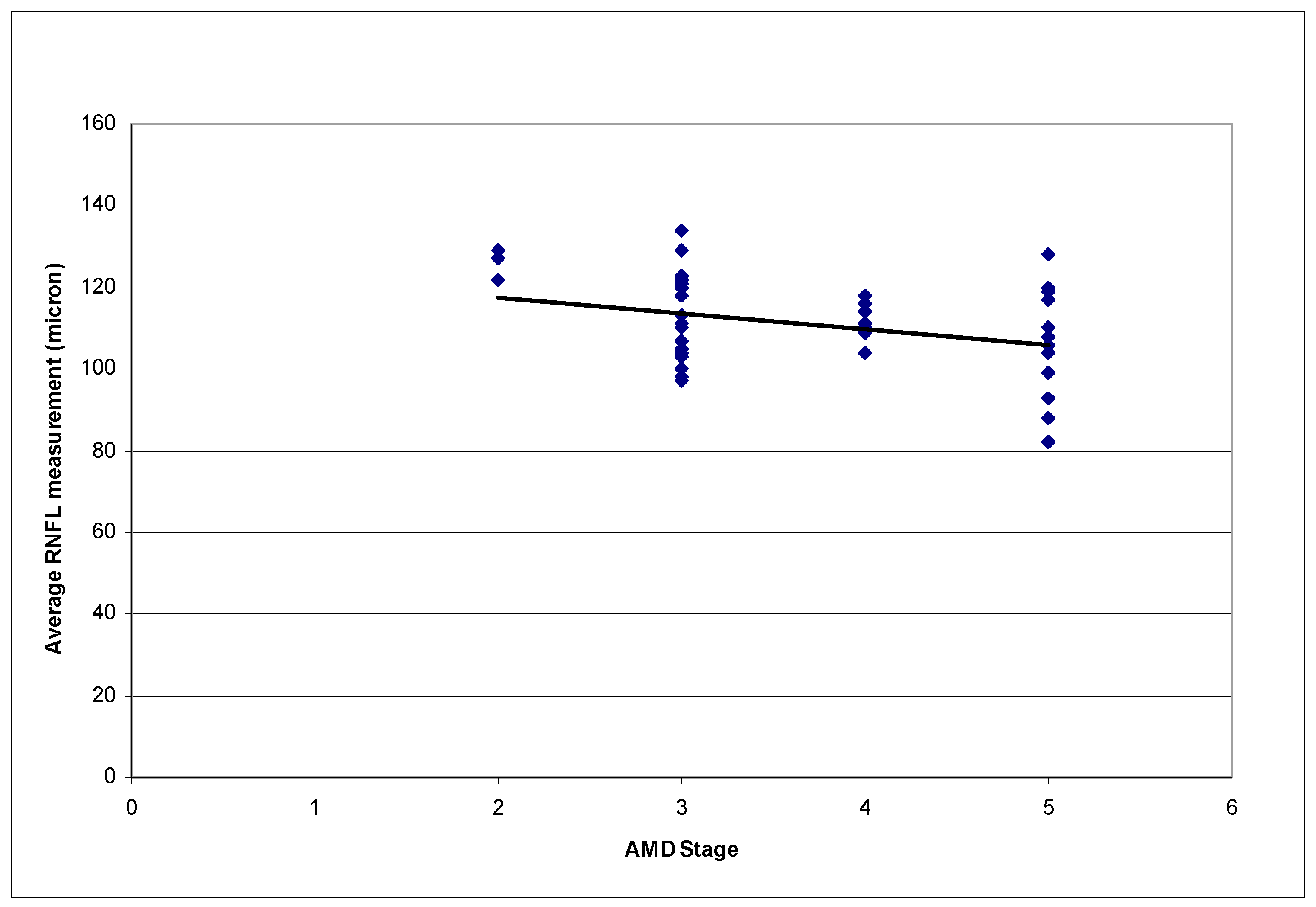
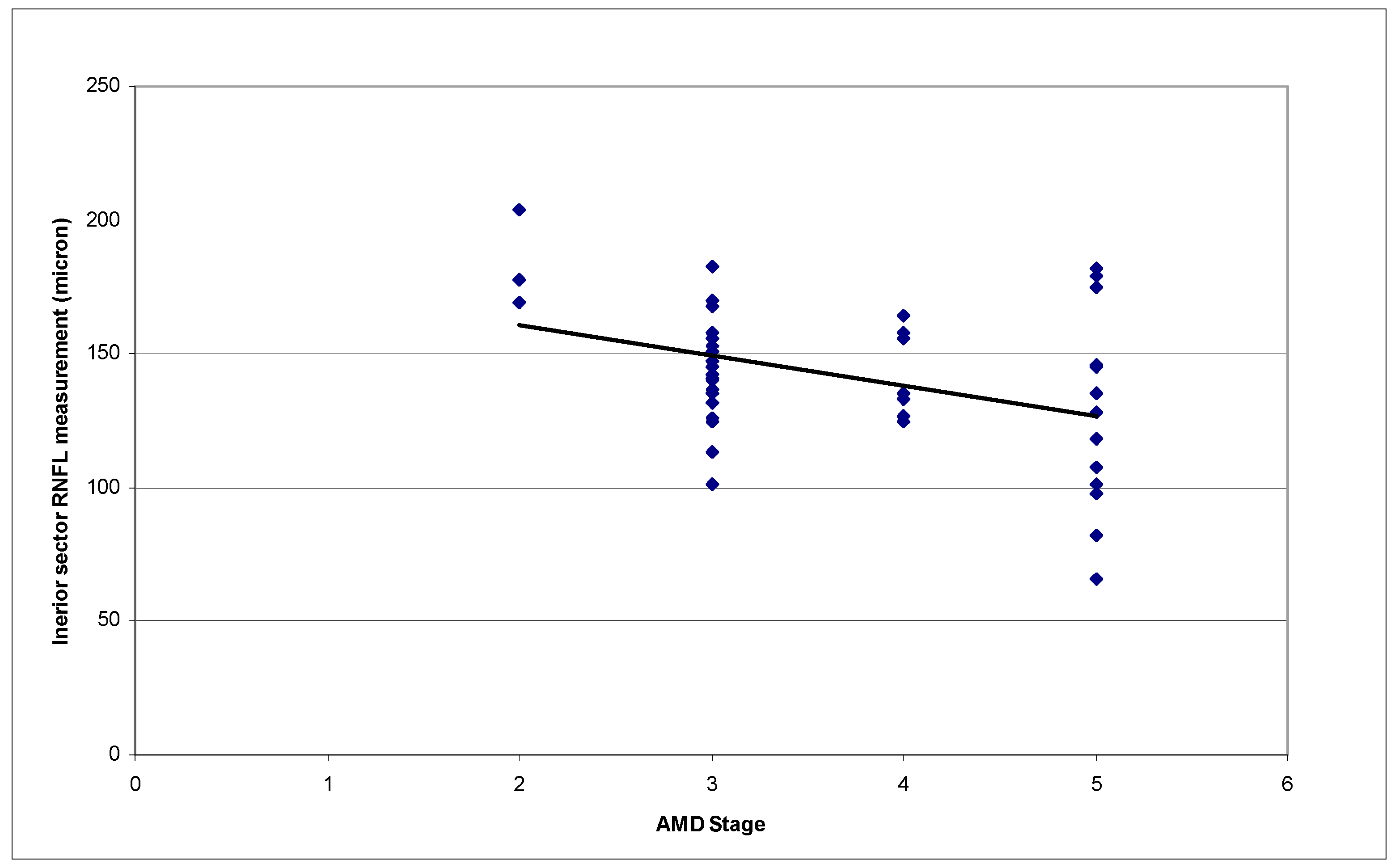
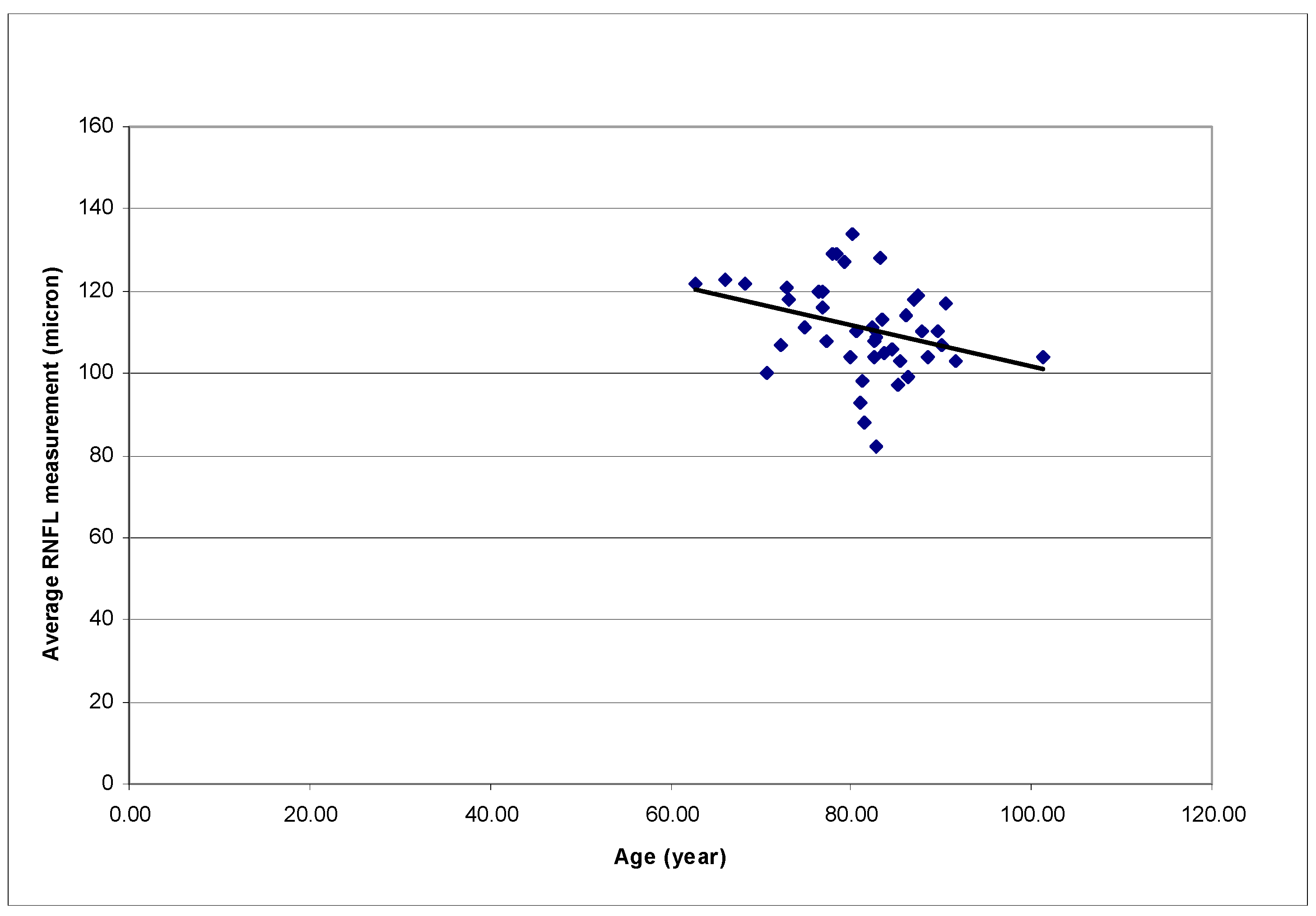
3. Results
4. Discussions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- The Eye Disease Prevalence Research Group. Prevalence of age-related macular degeneration in the United States. Arch. Ophthlamol. 2004, 122, 564–572. [Google Scholar]
- The Eye Disease Prevalence Research Group. Prevalence of open-angle glaucoma among adults in the United States. Arch. Ophthlamol. 2004, 122, 532–538. [Google Scholar]
- Alward, W.L. Macular degeneration and glaucoma-like optic nerve head cupping. Am. J. Ophthalmol. 2004, 138, 135–136. [Google Scholar] [PubMed]
- Zlateva, G.P.; Javitt, J.C.; Shah, S.N.; Zhou, Z.; Murphy, J.G. Comparison of comorbid conditions between neovascular age-related macular degeneration patients and a control cohort in the medicare population. Retina 2007, 27, 1292–1299. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.P.; Feldman, Z.W.; Ostermann, J.; Brown, D.S.; Sloan, F.A. Longitudinal prevalence of major eye diseases. Arch. Ophthalmol. 2003, 121, 1303–1310. [Google Scholar] [CrossRef] [PubMed]
- Law, S.K.; Sohn, Y.H.; Hoffman, D.; Small, K.; Coleman, A.L.; Caprioli, J. Optic disk appearance in advanced age-related macular degeneration. Am. J. Ophthalmol. 2004, 138, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Hall, E.R.; Klein, B.E.; Knudtson, M.D.; Meuer, S.M.; Klein, R. Age-related macular degeneration and optic disk cupping: The Beaver Dam Eye Study. Am. J. Ophthalmol. 2006, 141, 494–497. [Google Scholar] [CrossRef] [PubMed]
- Paunescu, L.A.; Schuman, J.S.; Price, L.L.; Stark, P.C.; Beaton, S.; Ishikawa, H.; Wollstein, G.; Fujimoto, J.G. Reproducibility of nerve fiber thickness, macular thickness and optic nerve head measurements using StratusOCT. Investig. Ophthalmol. Vis. Sci. 2004, 45, 1716–1724. [Google Scholar] [CrossRef]
- Mansoori, T.; Viswanath, K.; Balakrishna, N. Reproducibility of peripapillary retinal nerve fibre layer thickness measurements with spectral domain optical coherence tomography in normal and glaucomatous eyes. Br. J. Ophthalmol. 2011, 95, 685–688. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; de Boer, J.F.; Chen, T.C. Reproducibility of retinal nerve fiber layer thickness measurements using spectral domain optical coherence tomography. J. Glaucoma 2011, 20, 470–476. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.W.; Sung, K.R.; Hong, J.T.; Um, T.W.; Kang, S.Y.; Kook, M.S. Detection of glaucoma by spectral domain-scanning laser ophthalmoscopy/optical coherence tomography (SD-SLO/OCT) and time domain optical coherence tomography. J. Glaucoma 2011, 20, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Sehi, M.; Grewal, D.S.; Sheets, C.W.; Greenfield, D.S. Diagnostic ability of Fourier-domain vs. time-domain optical coherence tomography for glaucoma detection. Am. J. Ophthalmol. 2009, 148, 597–605. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.R.; Jeoung, J.W.; Choi, J.; Choi, J.Y.; Park, K.H.; Kim, Y.D. Structure-function relationships in normal and glaucomatous eyes determined by time- and spectral-domain optical coherence tomography. Investig. Ophthalmol. Vis. Sci. 2010, 51, 6424–6430. [Google Scholar] [CrossRef] [PubMed]
- Chang, R.T.; Knight, O.J.; Feuer, W.J.; Budenz, D.L. Sensitivity and specificity of time-domain versus spectral-domain optical coherence tomography in diagnosing early to moderate glaucoma. Ophthalmology 2009, 116, 2294–2299. [Google Scholar] [CrossRef] [PubMed]
- Yuda, K.; Inoue, Y.; Tomidokoro, A.; Tamaki, Y.; Yanagi, Y. Nerve fiber layer thickness in exudative age-related macular degeneration in Japanese patients. Graefes Arch. Clin. Exp. Ophthalmol. 2010, 248, 353–359. [Google Scholar] [CrossRef] [PubMed]
- Seddon, J.M.; Sharma, S.; Adelman, R.A. Evaluation of the clinical age-related maculopathy staging system. Ophthalmology 2006, 113, 260–266. [Google Scholar] [CrossRef] [PubMed]
- Schuman, J.S.; Hee, M.R.; Puliafito, C.A.; Wong, C.; Pedut-Kloizman, T.; Lin, C.P.; Hertzemark, E.; Izatt, J.A.; Swanson, E.A.; Fujimoto, J.G. Quantification of nerve fiber layer thickness in normal and glaucomatous eyes using optical coherence tomography. Arch. Ophthalmol. 1995, 113, 586–596. [Google Scholar] [CrossRef] [PubMed]
- Macular Photocoagulation Study Group. Subfoveal neovascular lesions in age-related macular degeneration, guidelines for evaluation and treatment in the Macular Photocoagulation Study. Arch. Ophthalmol. 1991, 109, 1242–1257. [Google Scholar]
- Quigley, H.A.; Addicks, E.M. Regional differences in the structure of the lamina cribrosa and their relation to glaucomatous optic nerve damage. Arch. Ophthalmol. 1981, 99, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Jonas, J.B.; Nguyen, N.X.; Naumann, G.O. The retinal nerve fiber layer in normal eyes. Ophthalmology 1989, 96, 627–632. [Google Scholar] [CrossRef]
- Solomon, S.D.; Lindsley, K.; Vedula, S.S.; Krzystolik, M.G.; Hawkins, B.S. Anti-vascular therapy with anti-vascular endothelial growth factor modalities for neovascular age-related macular degeneration. Cochraone Database Syst. Rev. 2014, 8, CD005139. [Google Scholar] [CrossRef]
- Tolentino, M. Systemic and Ocular Safety of Intravitreal anti-VEGF therapies for ocular neovascular disease. Surv. Ophthalmol. 2011, 56, 95–113. [Google Scholar] [CrossRef] [PubMed]
- Good, T.J.; Kimura, A.E.; Mandava, N.; Kahook, M.Y. Sustained elevation of intraocular pressure after intravitreal injections of anti-VEGF agents. Br. J. Ophthalmol. 2011, 95, 1111–1114. [Google Scholar] [CrossRef] [PubMed]
- Adelman, R.A.; Zheng, Q.; Mayer, H.R. Persistent ocular hypertension following intravitreal bevacizumab and ranibizumab injections. J. Ocul. Pharmacol. Ther. 2010, 26, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Horsley, M.B.; Mandava, N.; Maycotte, M.A.; Kahook, M.Y. Retinal nerve fiber layer thickness in patients receiving chronic anti-vascular endothelial growth factor therapy. Am. J. Ophthalmol. 2010, 150, 558–561. [Google Scholar] [CrossRef] [PubMed]
- Seth, R.K.; Salim, S.; Shields, M.B.; Adelman, R.A. Assessment of optic nerve cup-to-disk ratio changes in patients receiving multiple intravitreal injections of antivascular endothelial growth factor agents. Retina 2009, 29, 956–959. [Google Scholar] [CrossRef] [PubMed]
| Grade of Maculopathy | Clinical Features |
|---|---|
| 1 | No drusen or <10 small drusen without pigment abnormalities |
| 2 | Approximately ≥10 small drusen or <15 intermediate drusen, or pigment abnormalities associated with ARM |
| a. Drusen | |
| b. RPE changes (hyperpigmentation and hypopigmentation) | |
| c. Both drusen and RPE changes | |
| 3 | Approximately ≥15 intermediate drusen or any large drusen |
| a. No drusenoid RPED | |
| b. Drusenoid RPED | |
| 4 | Geographic atrophy with involvement of the macular center, or non-central geographic atrophy at least 350 μm in size |
| 5 | Exudative AMD, including non-drusenoid pigment epithelial detachments, serous or hemorrhagic retinal detachments, CNVM with sub retinal or sub-RPE hemorrhages or fibrosis, or scars consistent with treatment of AMD |
| a. Serous RPED, without CNVM | |
| b. CNVM or disciform scar |
| Peripapillary Sector | RNFL Measurement (Mean ± S.D. in Micron) |
|---|---|
| Temporal | 64.53 ± 15.28 |
| Superior Temporal | 113.81 ± 22.72 |
| Superior | 135.40 ± 25.08 |
| Superior Nasal | 122.12 ± 22.76 |
| Nasal | 89.37 ± 21.78 |
| Inferior Nasal | 110.77 ± 25.41 |
| Inferior | 141.28 ± 28.27 |
| Inferior Temporal | 109.40 ± 26.61 |
| Average | 110.95 ± 11.31 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Law, S.K.; Small, K.W.; Caprioli, J. Peripapillary Retinal Nerve Fiber Measurement with Spectral-Domain Optical Coherence Tomography in Age-Related Macular Degeneration. Vision 2017, 1, 26. https://doi.org/10.3390/vision1040026
Law SK, Small KW, Caprioli J. Peripapillary Retinal Nerve Fiber Measurement with Spectral-Domain Optical Coherence Tomography in Age-Related Macular Degeneration. Vision. 2017; 1(4):26. https://doi.org/10.3390/vision1040026
Chicago/Turabian StyleLaw, Simon K., Kent W. Small, and Joseph Caprioli. 2017. "Peripapillary Retinal Nerve Fiber Measurement with Spectral-Domain Optical Coherence Tomography in Age-Related Macular Degeneration" Vision 1, no. 4: 26. https://doi.org/10.3390/vision1040026
APA StyleLaw, S. K., Small, K. W., & Caprioli, J. (2017). Peripapillary Retinal Nerve Fiber Measurement with Spectral-Domain Optical Coherence Tomography in Age-Related Macular Degeneration. Vision, 1(4), 26. https://doi.org/10.3390/vision1040026





