Photobiomodulation as Medicine: Low-Level Laser Therapy (LLLT) for Acute Tissue Injury or Sport Performance Recovery
Abstract
1. Introduction
2. Literature Search Strategy
3. Findings from the Clinical Literature
3.1. Wound Healing
3.1.1. Post Surgery
3.1.2. Pre-Conditioning of Wounds
3.2. Athletic Training and Performance
3.3. Management of Acute Musculoskeletal Injury
3.4. LLLT at a Cellular Level
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- National Library of Medicine. MeSH Descriptor Data. 2023. Available online: https://meshb.nlm.nih.gov/record/ui?ui=D028022 (accessed on 31 July 2024).
- Anders, J.J.; Lanzafame, R.J.; Arany, P.R. Low-Level Light/Laser Therapy Versus Photobiomodulation Therapy. Photomed. Laser Surg. 2015, 33, 183–184. [Google Scholar] [CrossRef] [PubMed]
- Mussttaf, R.A.; Jenkins, D.F.L.; Jha, A.N. Assessing the impact of low level laser therapy (LLLT) on biological systems: A review. Int. J. Radiat. Biol. 2019, 95, 120–143. [Google Scholar] [CrossRef]
- Hamblin, M.R. Photobiomodulation or low-level laser therapy. J. Biophotonics 2016, 9, 1122–1124. [Google Scholar] [CrossRef] [PubMed]
- Mester, E.; Mester, A.F.; Mester, A. The biomedical effects of laser application. Lasers Surg. Med. 1985, 5, 31–39. [Google Scholar] [CrossRef] [PubMed]
- U.S. Food & Drug Administration. Laser Products and Instruments. 2023. Available online: https://www.fda.gov/radiation-emitting-products/home-business-and-entertainment-products/laser-products-and-instruments (accessed on 31 July 2024).
- Regulatory Affairs Professionals Society. FDA Draft Guidance Covers Low-Level Light Therapy Devices. 2023. Available online: https://www.raps.org/News-and-Articles/News-Articles/2023/1/FDA-draft-guidance-covers-low-level-light-therapy (accessed on 31 July 2024).
- Heiskanen, V.; Hamblin, M.R. Photobiomodulation: Lasers vs. light emitting diodes? Photochem. Photobiol. Sci. 2018, 17, 1003–1017. [Google Scholar] [CrossRef]
- World Association for Photobiomodulation Therapy. WALT Recommendations—Dosage Recommendations 2022. 2022. Available online: https://waltpbm.org/documentation-links/recommendations/ (accessed on 31 July 2024).
- Gayton, J.; Monga, A. Goal setting in physiotherapy-led adult musculoskeletal care: A scoping review. Musculoskelet. Care 2023, 21, 1315–1340. [Google Scholar] [CrossRef]
- Opel, D.R.; Hagstrom, E.; Pace, A.K.; Sisto, K.; Hirano-Ali, S.A.; Desai, S.; Swan, J. Light-emitting Diodes: A Brief Review and Clinical Experience. J. Clin. Aesthet. Dermatol. 2015, 8, 36–44. [Google Scholar]
- Rola, P.; Wlodarczk, S.; Lesiak, M.; Doroszko, A.; Wlodarczk, A. Changes in Cell Biology under the Influence of Low-LevelLaser Therapy. Photonics 2022, 9, 502. [Google Scholar] [CrossRef]
- Artzi, O.; Friedman, O.; Al-niaimi, F.; Wolf, Y.; Mehrabi, J.N. Mitigation of Postsurgical Scars Using Lasers. Plast. Reconstr. Surg. Glob. Open 2020, 8, e2746. [Google Scholar] [CrossRef]
- Seago, M.; Shumaker, P.R.; Spring, L.K.; Alam, M.; Al-Niaimi, F.; Rox Anderson, R.; Artzi, O.; Bayat, A.; Cassuto, D.; Chan, H.H.; et al. Laser Treatment of Traumatic Scars and Contractures: 2020 International Consensus Recommendations. Lasers Surg. Med. 2020, 52, 96–116. [Google Scholar] [CrossRef]
- Wang, Z.; Chen, Y.; Yang, X.; Pan, B.; Xie, H.; Bi, H. Safety and Effectiveness of Laser or Intense Pulsed Light Treatment for Early Surgical Scar: A Systematic Review and Meta-analysis. Aesthetic Plast. Surg. 2023, 48, 228–235. [Google Scholar] [CrossRef] [PubMed]
- Friedman, O.; Gofstein, D.; Arad, E.; Gur, E.; Sprecher, E.; Artzi, O. Laser pretreatment for the attenuation of planned surgical scars: A randomized self-controlled hemi-scar pilot study. J. Plast. Reconstr. Aesthetic Surg. 2020, 73, 893–898. [Google Scholar] [CrossRef]
- González-Muñoz, A.; Perez-Montilla, J.J.; Cuevas-Cervera, M.; Aguilar-García, M.; Aguilar-Nuñez, D.; Hamed-Hamed, D.; Pruimboom, L.; Navarro-Ledesma, S. Effects of Photobiomodulation in Sports Performance: A Literature Review. Appl. Sci. 2023, 13, 3147. [Google Scholar] [CrossRef]
- Oliveira, A.F.S.S.D.; Silva, J.L.D.; Camillo, C.A.M.; Andraus, R.A.C.; Maia, L.P. Does Photobiomodulation Improve Muscle Performance and Recovery? A Systematic Review. Rev. Bras. Med. Esporte 2023, 29, e2021_0412. [Google Scholar] [CrossRef]
- Luo, W.T.; Lee, C.J.; Tam, K.W.; Huang, T.W. Effects of Low-Level Laser Therapy on Muscular Performance and Soreness Recovery in Athletes: A Meta-analysis of Randomized Controlled Trials. Sports Health Multidiscip. Approach 2022, 14, 687–693. [Google Scholar] [CrossRef]
- De Marchi, T.; Ferlito, J.V.; Ferlito, M.V.; Salvador, M.; Cesar, E.; Leal-Junior, P. Can Photobiomodulation Therapy (PBMT) Minimize Exercise-Induced Oxidative Stress? A Systematic Review and Meta-Analysis. Antioxidants 2022, 11, 1671. [Google Scholar] [CrossRef]
- Ailioaie, L.M.; Litscher, G.; Crovella, S. Photobiomodulation and Sports: Results of a Narrative Review. Life 2021, 11, 1339. [Google Scholar] [CrossRef]
- Alves, V.M.N.; Furlan, R.M.M.M.; Motta, A.R. Immediate effects of photobiomodulation with low-level laser therapy on muscle performance: An integrative literature review. Rev. CEFAC 2019, 21, e12019. [Google Scholar] [CrossRef]
- Vanin, A.A.; Verhagen, E.; Barboza, S.D.; Costa, L.O.P.; Leal-Junior, E.C.P. Photobiomodulation therapy for the improvement of muscular performance and reduction of muscular fatigue associated with exercise in healthy people: A systematic review and meta-analysis. Lasers Med. Sci. 2018, 33, 181–214. [Google Scholar] [CrossRef]
- Ferraresi, C.; Huang, Y.Y.; Hamblin, M.R. Photobiomodulation in human muscle tissue: An advantage in sports performance? J. Biophotonics 2016, 9, 1273–1299. [Google Scholar] [CrossRef]
- Nampo, F.K.; Cavalheri, V.; dos Santos Soares, F.; de Paula Ramos, S.; Camargo, E.A. Low-level phototherapy to improve exercise capacity and muscle performance: A systematic review and meta-analysis. Lasers Med. Sci. 2016, 31, 1957–1970. [Google Scholar] [CrossRef] [PubMed]
- Borsa, P.A.; Larkin, K.A.; True, J.M. Does Phototherapy Enhance Skeletal Muscle Contractile Function and Postexercise Recovery? A Systematic Review. J. Athl. Train. 2013, 48, 57–67. [Google Scholar] [CrossRef]
- Leal-Junior, E.C.P.; Vanin, A.A.; Miranda, E.F.; de Carvalho, P.D.T.C.; Dal Corso, S.; Bjordal, J.M. Effect of phototherapy (low-level laser therapy and light-emitting diode therapy) on exercise performance and markers of exercise recovery: A systematic review with meta-analysis. Lasers Med. Sci. 2013, 30, 925–939. [Google Scholar] [CrossRef]
- Dutra, Y.M.; Malta, E.S.; Elias, A.S.; Broatch, J.R.; Zagatto, A.M. Deconstructing the Ergogenic Effects of Photobiomodulation: A Systematic Review and Meta-analysis of its Efficacy in Improving Mode-Specific Exercise Performance in Humans. Sports Med. 2022, 52, 2733–2757. [Google Scholar] [CrossRef] [PubMed]
- Toma, R.L.; Vassão, P.G.; Assis, L.; Antunes, H.K.M.; Renno, A.C.M. Low level laser therapy associated with a strength training program on muscle performance in elderly women: A randomized double blind control study. Lasers Med. Sci. 2016, 31, 1219–1229. [Google Scholar] [CrossRef]
- Vassão, P.G.; Toma, R.L.; Antunes, H.K.M.; Tucci, H.T.; Renno, A.C.M. Effects of photobiomodulation on the fatigue level in elderly women: An isokinetic dynamometry evaluation. Lasers Med. Sci. 2016, 31, 275–282. [Google Scholar] [CrossRef]
- Toma, R.L.; Tucci, H.T.; Antunes, H.K.M.; Pedroni, C.R.; de Oliveira, A.S.; Buck, I.; Ferreira, P.D.; Vassão, P.G.; Renno, A.C.M. Effect of 808 nm low-level laser therapy in exercise-induced skeletal muscle fatigue in elderly women. Lasers Med. Sci. 2013, 28, 1375–1382. [Google Scholar] [CrossRef] [PubMed]
- Bublitz, C.; Renno, A.C.M.; Ramos, R.S.; Assis, L.; Sellera, C.A.C.; Trimer, R.; Borghi-Silva, A.; Arena, R.; Guizilini, S. Acute effects of low-level laser therapy irradiation on blood lactate and muscle fatigue perception in hospitalized patients with heart failure—A pilot study. Lasers Med. Sci. 2016, 31, 1203–1209. [Google Scholar] [CrossRef]
- Tomazoni, S.S.; Machado, C.D.S.M.; De Marchi, T.; Casalechi, H.L.; Bjordal, J.M.; de Carvalho, P.D.T.C.; Leal-Junior, E.C.P. Infrared Low-Level Laser Therapy (Photobiomodulation Therapy) before Intense Progressive Running Test of High-Level Soccer Players: Effects on Functional, Muscle Damage, Inflammatory, and Oxidative Stress Markers—A Randomized Controlled Trial. Oxidative Med. Cell. Longev. 2019, 2019, 6239058. [Google Scholar] [CrossRef]
- Miranda, E.F.; Tomazoni, S.S.; de Paiva, P.R.V.; Pinto, H.D.; Smith, D.; Santos, L.A.; de Tarso Camillo de Carvalho, P.; Leal-Junior, E.C.P. When is the best moment to apply photobiomodulation therapy (PBMT) when associated to a treadmill endurance-training program? A randomized, triple-blinded, placebo-controlled clinical trial. Lasers Med. Sci. 2018, 33, 719–727. [Google Scholar] [CrossRef]
- Follmer, B.; Dellagrana, R.A.; Rossato, M.; Sakugawa, R.L.; Diefenthaeler, F. Photobiomodulation therapy is beneficial in reducing muscle fatigue in Brazilian jiu-jitsu athletes and physically active men. Sport Sci. Health 2018, 14, 685–691. [Google Scholar] [CrossRef]
- De Marchi, T.; Leal-Junior, E.C.P.; Lando, K.C.; Cimadon, F.; Vanin, A.A.; da Rosa, D.P.; Salvador, M. Photobiomodulation therapy before futsal matches improves the staying time of athletes in the court and accelerates post-exercise recovery. Lasers Med. Sci. 2019, 34, 139–148. [Google Scholar] [CrossRef] [PubMed]
- Machado, C.D.S.M.; Casalechi, H.L.; Vanin, A.A.; de Azevedo, J.B.; de Carvalho, P.D.T.C.; Leal-Junior, E.C.P. Does photobiomodulation therapy combined to static magnetic field (PBMT-sMF) promote ergogenic effects even when the exercised muscle group is not irradiated? A randomized, triple-blind, placebo-controlled trial. BMC Sports Sci. Med. Rehabil. 2020, 12, 49. [Google Scholar] [CrossRef] [PubMed]
- Leal-Junior, E.C.P.; de Oliveira, M.F.D.; Joensen, J.; Stausholm, M.B.; Bjordal, J.M.; Tomazoni, S.S. What is the optimal time-response window for the use of photobiomodulation therapy combined with static magnetic field (PBMT-sMF) for the improvement of exercise performance and recovery, and for how long the effects last? A randomized, triple-blinded, placebo-controlled trial. BMC Sports Sci. Med. Rehabil. 2020, 12, 64. [Google Scholar] [CrossRef]
- De Paiva, P.R.V.; Casalechi, H.L.; Tomazoni, S.S.; Machado, C.D.S.M.; Ribeiro, N.F.; Pereira, A.L.; De Oliveira, M.F.D.; Alves, M.N.D.S.; Dos Santos, M.C.; Takara, I.E.T.; et al. Does the combination of photobiomodulation therapy (PBMT) and static magnetic fields (sMF) potentiate the effects of aerobic endurance training and decrease the loss of performance during detraining? A randomised, triple-blinded, placebo-controlled trial. BMC Sports Sci. Med. Rehabil. 2020, 12, 23. [Google Scholar] [CrossRef]
- Machado, A.F.; Leal-Junior, E.C.P.; Batista, N.P.; Espinoza, R.M.C.P.P.; Hidalgo, R.B.R.; Carvalho, F.A.; Micheletti, J.K.; Vanderlei, F.M.; Pastre, C.M. Photobiomodulation therapy applied during an exercise-training program does not promote additional effects in trained individuals: A randomized placebo-controlled trial. Braz. J. Phys. Ther. 2022, 26, 100388. [Google Scholar] [CrossRef]
- Orssatto, L.B.D.R.; Detanico, D.; Kons, R.L.; Sakugawa, R.L.; Silva, J.N.D., Jr.; Diefenthaeler, F. Photobiomodulation Therapy Does Not Attenuate Fatigue and Muscle Damage in Judo Athletes: A Randomized, Triple-Blind, Placebo-Controlled Trial. Front. Physiol. 2019, 10, 811. [Google Scholar] [CrossRef]
- de Oliveira, A.R.; Vanin, A.A.; Tomazoni, S.S.; Miranda, E.F.; Albuquerque-Pontes, G.M.; De Marchi, T.; dos Santos Grandinetti, V.; de Paiva, P.R.V.; Imperatori, T.B.G.; de Carvalho, P.D.T.C.; et al. Pre-Exercise Infrared Photobiomodulation Therapy (810 nm) in Skeletal Muscle Performance and Postexercise Recovery in Humans: What Is the Optimal Power Output? Photomed. Laser Surg. 2017, 35, 595–603. [Google Scholar] [CrossRef]
- Pinto, H.D.; Vanin, A.A.; Miranda, E.F.; Tomazoni, S.S.; Johnson, D.S.; Albuquerque-Pontes, G.M.; Ivo de OAleixo, J.; Grandinetti, V.D.S.; Casalechi, H.L.; Paulo de Tarso, C.; et al. Photobiomodulation Therapy Improves Performance and Accelerates Recovery of High-Level Rugby Players in Field Test: A Randomized, Crossover, Double-Blind, Placebo-Controlled Clinical Study. J. Strength Cond. Res. 2016, 30, 3329–3338. [Google Scholar] [CrossRef]
- Larkin-Kaiser, K.A.; Borsa, P.A.; Baweja, H.S.; Moore, M.A.; Tillman, M.D.; George, S.Z.; Christou, E.A. Photobiomodulation delays the onset of skeletal muscle fatigue in a dose-dependent manner. Lasers Med. Sci. 2016, 31, 1325–1332. [Google Scholar] [CrossRef]
- Aver Vanin, A.; De Marchi, T.; Silva Tomazoni, S.; Tairova, O.; Leão Casalechi, H.; de Tarso Camillo de Carvalho, P.; Bjordal, J.M.; Leal-Junior, E.C. Pre-Exercise Infrared Low-Level Laser Therapy (810 nm) in Skeletal Muscle Performance and Postexercise Recovery in Humans, What Is the Optimal Dose? A Randomized, Double-Blind, Placebo-Controlled Clinical Trial. Photomed. Laser Surg. 2016, 34, 473–482. [Google Scholar] [CrossRef] [PubMed]
- Dellagrana, R.A.; Rossato, M.; Sakugawa, R.L.; Lazzari, C.D.; Baroni, B.M.; Diefenthaeler, F. Dose-response effect of photobiomodulation therapy on neuromuscular economy during submaximal running. Lasers Med. Sci. 2018, 33, 329–336. [Google Scholar] [CrossRef]
- Ferraresi, C.; de Brito Oliveira, T.; de Oliveira Zafalon, L.; de Menezes Reiff, R.B.; Baldissera, V.; de Andrade Perez, S.E.; Júnior, E.M.; Parizotto, N.A. Effects of low level laser therapy (808 nm) on physical strength training in humans. Lasers Med. Sci. 2011, 26, 349–358. [Google Scholar] [CrossRef] [PubMed]
- Antonialli, F.C.; De Marchi, T.; Tomazoni, S.S.; Vanin, A.A.; dos Santos Grandinetti, V.; de Paiva, P.R.V.; Pinto, H.D.; Miranda, E.F.; de Tarso Camillo de Carvalho, P.; Leal-Junior, E.C.P. Phototherapy in skeletal muscle performance and recovery after exercise: Effect of combination of super-pulsed laser and light-emitting diodes. Lasers Med. Sci. 2014, 29, 1967–1976. [Google Scholar] [CrossRef] [PubMed]
- De Marchi, T.; Leal-Junior, E.C.P.; Bortoli, C.; Tomazoni, S.S.; Lopes-Martins, R.Á.B.; Salvador, M. Low-level laser therapy (LLLT) in human progressive-intensity running: Effects on exercise performance, skeletal muscle status, and oxidative stress. Lasers Med. Sci. 2012, 27, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Zagatto, A.M.; de Paula Ramos, S.; Nakamura, F.Y.; de Lira, F.S.; Lopes-Martins, R.Á.B.; de Paiva Carvalho, R.L. Effects of low-level laser therapy on performance, inflammatory markers, and muscle damage in young water polo athletes: A double-blind, randomized, placebo-controlled study. Lasers Med. Sci. 2016, 31, 511–521. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Larkin-Kaiser, K.A.; Christou, E.; Tillman, M.; George, S.; Borsa, P.A. Near-Infrared Light Therapy to Attenuate Strength Loss After Strenuous Resistance Exercise. J. Athl. Train. 2015, 50, 45–50. [Google Scholar] [CrossRef]
- de Almeida, P.; Lopes-Martins, R.Á.B.; De Marchi, T.; Tomazoni, S.S.; Albertini, R.; Corrêa, J.C.F.; Rossi, R.P.; Machado, G.P.; da Silva, D.P.; Bjordal, J.M.; et al. Red (660 nm) and infrared (830 nm) low-level laser therapy in skeletal muscle fatigue in humans: What is better? Lasers Med. Sci. 2012, 27, 453–458. [Google Scholar] [CrossRef]
- Toma, R.L.; Oliveira, M.X.; Renno, A.C.M.; Laakso, E.L. Photobiomodulation (PBM) therapy at 904 nm mitigates effects of exercise-induced skeletal muscle fatigue in young women. Lasers Med. Sci. 2018, 33, 1197–1205. [Google Scholar] [CrossRef]
- Lanferdini, F.J.; Bini, R.R.; Baroni, B.M.; Klein, K.D.; Carpes, F.P.; Vaz, M.A. Improvement of Performance and Reduction of Fatigue With Low-Level Laser Therapy in Competitive Cyclists. Int. J. Sports Physiol. Perform. 2018, 13, 14–22. [Google Scholar] [CrossRef]
- Dellagrana, R.A.; Rossato, M.; Sakugawa, R.L.; Baroni, B.M.; Diefenthaeler, F. Photobiomodulation Therapy on Physiological and Performance Parameters During Running Tests: Dose–Response Effects. J. Strength Cond. Res. 2018, 32, 2807–2815. [Google Scholar] [CrossRef]
- Teixeira, C.L.; Mezzaroba, P.V.; Machado, F.A. Effect of Photobiomodulation on Critical Swimming Velocity: A Randomized, Crossover, Double-Blind, and Placebo-Controlled Study. Int. J. Sports Physiol. Perform. 2021, 16, 1035–1042. [Google Scholar] [CrossRef] [PubMed]
- Azuma, R.H.E.; Merlo, J.K.; Jacinto, J.L.; Borim, J.M.; da Silva, R.A.; Pacagnelli, F.L.; Nunes, J.P.; Ribeiro, A.S.; Aguiar, A.F. Photobiomodulation Therapy at 808 nm Does Not Improve Biceps Brachii Performance to Exhaustion and Delayed-Onset Muscle Soreness in Young Adult Women: A Randomized, Controlled, Crossover Trial. Front. Physiol. 2021, 12, 664582. [Google Scholar] [CrossRef] [PubMed]
- Leal-Junior, E.C.P.; Lopes-Martins, R.A.B.; Baroni, B.M.; De Marchi, T.; Rossi, R.P.; Grosselli, D.; Generosi, R.A.; de Godoi, V.; Basso, M.; Mancalossi, J.L.; et al. Comparison Between Single-Diode Low-Level Laser Therapy (LLLT) and LED Multi-Diode (Cluster) Therapy (LEDT) Applications Before High-Intensity Exercise. Photomed. Laser Surg. 2009, 27, 617–623. [Google Scholar] [CrossRef] [PubMed]
- Leal-Junior, E.C.P.; Lopes-Martins, R.Á.B.; Baroni, B.M.; De Marchi, T.; Taufer, D.; Manfro, D.S.; Rech, M.; Danna, V.; Grosselli, D.; Generosi, R.A.; et al. Effect of 830 nm low-level laser therapy applied before high-intensity exercises on skeletal muscle recovery in athletes. Lasers Med. Sci. 2009, 24, 857–863. [Google Scholar] [CrossRef]
- Leal, E.C.P.; Lopes-Martins, R.Á.B.; Frigo, L.; De Marchi, T.; Rossi, R.P.; De Godoi, V.; Tomazoni, S.S.; Silva, D.P.; Basso, M.; Filho, P.L.; et al. Effects of Low-Level Laser Therapy (LLLT) in the Development of Exercise-Induced Skeletal Muscle Fatigue and Changes in Biochemical Markers Related to Postexercise Recovery. J. Orthop. Sports Phys. Ther. 2010, 40, 524–532. [Google Scholar] [CrossRef] [PubMed]
- Leal-Junior, E.C.P.; Lopes-Martins, R.Á.B.; Vanin, A.A.; Baroni, B.M.; Grosselli, D.; De Marchi, T.; Iversen, V.V.; Bjordal, J.M. Effect of 830 nm low-level laser therapy in exercise-induced skeletal muscle fatigue in humans. Lasers Med. Sci. 2009, 24, 425–431. [Google Scholar] [CrossRef]
- Rossato, M.; Dellagrana, R.A.; Sakugawa, R.L.; Baroni, B.M.; Diefenthaeler, F. Dose–Response Effect of Photobiomodulation Therapy on Muscle Performance and Fatigue During a Multiple-Set Knee Extension Exercise: A Randomized, Crossover, Double-Blind Placebo-Controlled Trial. Photobiomodul. Photomed. Laser Surg. 2020, 38, 758–765. [Google Scholar] [CrossRef]
- Rossato, M.; Dellagrana, R.A.; Sakugawa, R.L.; Lazzari, C.D.; Baroni, B.M.; Diefenthaeler, F. Time Response of Photobiomodulation Therapy on Muscular Fatigue in Humans. J. Strength Cond. Res. 2018, 32, 3285–3293. [Google Scholar] [CrossRef]
- Miranda, E.F.; Vanin, A.A.; Tomazoni, S.S.; Grandinetti, V.D.S.; de Paiva, P.R.V.; Machado, C.D.S.M.; Monteiro, K.K.D.S.; Casalechi, H.L.; de Tarso, P.; de Carvalho, C.; et al. Using Pre-Exercise Photobiomodulation Therapy Combining Super-Pulsed Lasers and Light-Emitting Diodes to Improve Performance in Progressive Cardiopulmonary Exercise Tests. J. Athl. Train. 2016, 51, 129–135. [Google Scholar] [CrossRef]
- Orssatto, L.B.R.; Rossato, M.; Vargas, M.; Diefenthaeler, F.; de la Rocha Freitas, C. Photobiomodulation Therapy Effects on Resistance Training Volume and Discomfort in Well-Trained Adults: A Randomized, Double-Blind, Placebo-Controlled Trial. Photobiomodul. Photomed. Laser Surg. 2020, 38, 720–726. [Google Scholar] [CrossRef]
- Dellagrana, R.A.; Rossato, M.; Orssatto, L.B.R.; Sakugawa, R.L.; Baroni, B.M.; Diefenthaeler, F. Effect of Photobiomodulation Therapy in the 1500 m Run: An Analysis of Performance and Individual Responsiveness. Photobiomodul. Photomed. Laser Surg. 2020, 38, 734–742. [Google Scholar] [CrossRef] [PubMed]
- Higashi, R.H.; Toma, R.L.; Tucci, H.T.; Pedroni, C.R.; Ferreira, P.D.; Baldini, G.S.; Aveiro, M.C.; Borghi-Silva, A.; de Oliveira, A.S.; Renno, A.C.M. Effects of Low-Level Laser Therapy on Biceps Braquialis Muscle Fatigue in Young Women. Photomed. Laser Surg. 2013, 31, 586–594. [Google Scholar] [CrossRef] [PubMed]
- da Silva Alves, M.A.; Pinfildi, C.E.; Neto, L.N.; Lourenço, R.P.; de Azevedo, P.H.S.M.; Dourado, V.Z. Acute effects of low-level laser therapy on physiologic and electromyographic responses to the cardiopulmonary exercise testing in healthy untrained adults. Lasers Med. Sci. 2014, 29, 1945–1951. [Google Scholar] [CrossRef] [PubMed]
- dos Santos Maciel, T.; Muñoz, I.S.S.; Nicolau, R.A.; Nogueira, D.V.; Hauck, L.A.; Osório, R.A.L.; de Paula Júnior, A.R. Phototherapy effect on the muscular activity of regular physical activity practitioners. Lasers Med. Sci. 2014, 29, 1145–1152. [Google Scholar] [CrossRef] [PubMed]
- da Cunha, R.A.; Pinfildi, C.E.; de Castro Pochini, A.; Cohen, M. Photobiomodulation therapy and NMES improve muscle strength and jumping performance in young volleyball athletes: A randomized controlled trial study in Brazil. Lasers Med. Sci. 2020, 35, 621–631. [Google Scholar] [CrossRef] [PubMed]
- Dos Reis, F.A.; da Silva, B.A.K.; Laraia, E.M.S.; de Melo, R.M.; Silva, P.H.; Leal-Junior, E.C.P.; de Carvalho, P.D.T.C. Effects of Pre- or Post-Exercise Low-Level Laser Therapy (830 nm) on Skeletal Muscle Fatigue and Biochemical Markers of Recovery in Humans: Double-Blind Placebo-Controlled Trial. Photomed. Laser Surg. 2014, 32, 106–112. [Google Scholar] [CrossRef]
- Lanferdini, F.J.; Krüger, R.L.; Baroni, B.M.; Lazzari, C.; Figueiredo, P.; Reischak-Oliveira, A.; Vaz, M.A. Low-level laser therapy improves the VO2 kinetics in competitive cyclists. Lasers Med. Sci. 2018, 33, 453–460. [Google Scholar] [CrossRef]
- Leal-Junior, E.C.P.; Lopes-Martins, R.Á.B.; Dalan, F.; Ferrari, M.; Sbabo, F.M.; Generosi, R.A.; Baroni, B.M.; Penna, S.C.; Iversen, V.V.; Bjordal, J.M. Effect of 655-nm Low-Level Laser Therapy on Exercise-Induced Skeletal Muscle Fatigue in Humans. Photomed. Laser Surg. 2008, 26, 419–424. [Google Scholar] [CrossRef]
- Liu, Y.; Yang, H. Effect of Low-Level Laser Therapy on Exercise-Induced Skeletal Muscle Fatigue and Exercise Performance. Acta Medica Mediterr. 2020, 36, 2019–2025. [Google Scholar] [CrossRef]
- Medeiros, D.M.; Aimi, M.; Vaz, M.A.; Baroni, B.M. Effects of low-level laser therapy on hamstring strain injury rehabilitation: A randomized controlled trial. Phys. Ther. Sport 2020, 42, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Pinto, H.D.; Casalechi, H.L.; de Marchi, T.; dos Santos Monteiro Machado, C.; Dias, L.B.; Lino, M.M.A.; de Azevedo, J.B.; Tomazoni, S.S.; Leal-Junior, E.C.P. Photobiomodulation Therapy Combined with a Static Magnetic Field Applied in Different Moments Enhances Performance and Accelerates Muscle Recovery in CrossFit® Athletes: A Randomized, Triple-Blind, Placebo-Controlled Crossover Trial. Oxidative Med. Cell. Longev. 2022, 2022, 9968428. [Google Scholar] [CrossRef] [PubMed]
- de Paiva, P.R.V.; Tomazoni, S.S.; Johnson, D.S.; Vanin, A.A.; Albuquerque-Pontes, G.M.; Machado, C.D.S.M.; Casalechi, H.L.; de Carvalho, P.D.T.C.; Leal-Junior, E.C.P. Photobiomodulation therapy (PBMT) and/or cryotherapy in skeletal muscle restitution, what is better? A randomized, double-blinded, placebo-controlled clinical trial. Lasers Med. Sci. 2016, 31, 1925–1933. [Google Scholar] [CrossRef] [PubMed]
- Vanin, A.A.; Miranda, E.F.; Machado, C.S.M.; de Paiva, P.R.V.; Albuquerque-Pontes, G.M.; Casalechi, H.L.; de Tarso Camillo de Carvalho, P.; Leal-Junior, E.C.P. What is the best moment to apply phototherapy when associated to a strength training program? A randomized, double-blinded, placebo-controlled trial. Lasers Med. Sci. 2016, 31, 1555–1564. [Google Scholar] [CrossRef] [PubMed]
- de Brito Vieira, W.H.; Bezerra, R.M.; Queiroz, R.A.S.; Maciel, N.F.B.; Parizotto, N.A.; Ferraresi, C. Use of Low-Level Laser Therapy (808 nm) to Muscle Fatigue Resistance: A Randomized Double-Blind Crossover Trial. Photomed. Laser Surg. 2014, 32, 678–685. [Google Scholar] [CrossRef]
- Florianovicz, V.C.; Ferraresi, C.; Kuriki, H.U.; Marcolino, A.M.; Barbosa, R.I. Effects of Photobiomodulation Therapy and Restriction of Wrist Extensor Blood Flow on Grip: Randomized Clinical Trial. Photobiomodul. Photomed. Laser Surg. 2020, 38, 743–749. [Google Scholar] [CrossRef]
- Baroni, B.M.; Leal-Junior, E.C.P.; De Marchi, T.; Lopes, A.L.; Salvador, M.; Vaz, M.A. Low level laser therapy before eccentric exercise reduces muscle damage markers in humans. Eur. J. Appl. Physiol. 2010, 110, 789–796. [Google Scholar] [CrossRef]
- de Brito Vieira, W.H.; Ferraresi, C.; de Andrade Perez, S.E.; Baldissera, V.; Parizotto, N.A. Effects of low-level laser therapy (808 nm) on isokinetic muscle performance of young women submitted to endurance training: A randomized controlled clinical trial. Lasers Med. Sci. 2012, 27, 497–504. [Google Scholar] [CrossRef]
- Baroni, B.M.; Rodrigues, R.; Freire, B.B.; Franke, R.D.A.; Geremia, J.M.; Vaz, M.A. Effect of low-level laser therapy on muscle adaptation to knee extensor eccentric training. Eur. J. Appl. Physiol. 2015, 115, 639–647. [Google Scholar] [CrossRef]
- Kakihata, C.M.M.; Malanotte, J.A.; Higa, J.Y.; Errero, T.K.; Balbo, S.L.; Bertolini, G.R.F. Influence of low-level laser therapy on vertical jump in sedentary individuals. Einstein 2015, 13, 41–46. [Google Scholar] [CrossRef]
- de Souza, C.G.; Borges, D.T.; de Brito Macedo, L.; Brasileiro, J.S. Low-level laser therapy reduces the fatigue index in the ankle plantar flexors of healthy subjects. Lasers Med. Sci. 2016, 31, 1949–1955. [Google Scholar] [CrossRef] [PubMed]
- Felismino, A.S.; Costa, E.C.; Aoki, M.S.; Ferraresi, C.; de Araújo Moura Lemos, T.M.; de Brito Vieira, W.H. Effect of low-level laser therapy (808 nm) on markers of muscle damage: A randomized double-blind placebo-controlled trial. Lasers Med. Sci. 2014, 29, 933–938. [Google Scholar] [CrossRef] [PubMed]
- Fritsch, C.G.; Dornelles, M.P.; Severo-Silveira, L.; Marques, V.B.; Rosso, I.D.A.; Baroni, B.M. Effects of low-level laser therapy applied before or after plyometric exercise on muscle damage markers: Randomized, double-blind, placebo-controlled trial. Lasers Med. Sci. 2016, 31, 1935–1942. [Google Scholar] [CrossRef] [PubMed]
- Gorgey, A.S.; Wadee, A.N.; Sobhi, N.N. The Effect of Low-Level Laser Therapy on Electrically Induced Muscle Fatigue: A Pilot Study. Photomed. Laser Surg. 2008, 26, 501–506. [Google Scholar] [CrossRef]
- Rossato, M.; Dellagrana, R.A.; Lanferdini, F.J.; Sakugawa, R.L.; Lazzari, C.D.; Baroni, B.M.; Diefenthaeler, F. Effect of pre-exercise phototherapy applied with different cluster probe sizes on elbow flexor muscle fatigue. Lasers Med. Sci. 2016, 31, 1237–1244. [Google Scholar] [CrossRef]
- Craig, J.A.; Barlas, P.; Baxter, G.D.; Walsh, D.M.; Allen, J.M. Delayed-Onset Muscle Soreness: Lack of Effect of Combined Phototherapy/Low-Intensity Laser Therapy at Low Pulse Repetition Rates. J. Clin. Laser Med. Surg. 1996, 14, 375–380. [Google Scholar] [CrossRef]
- Craig, J.A.; Barron, J.; Walsh, D.M.; Baxter, G.D. Lack of effect of combined low intensity laser therapy/phototherapy (CLILT) on delayed onset muscle soreness in humans. Lasers Surg. Med. 1999, 24, 223–230. [Google Scholar] [CrossRef]
- Hainline, B.; Derman, W.; Vernec, A.; Budgett, R.; Deie, M.; Dvořák, J.; Harle, C.; Herring, S.A.; McNamee, M.; Meeuwisse, W.; et al. International Olympic Committee consensus statement on pain management in elite athletes. Br. J. Sports Med. 2017, 51, 1245–1258. [Google Scholar] [CrossRef]
- Tripodi, N.; Feehan, J.; Husaric, M.; Sidiroglou, F.; Apostolopoulos, V. The effect of low-level red and near-infrared photobiomodulation on pain and function in tendinopathy: A systematic review and meta-analysis of randomized control trials. BMC Sports Sci. Med. Rehabil. 2021, 13, 91. [Google Scholar] [CrossRef]
- Taylor, D.N.; Winfield, T.; Wynd, S. Low-Level Laser Light Therapy Dosage Variables vs Treatment Efficacy of Neuromusculoskeletal Conditions: A Scoping Review. J. Chiropr. Med. 2020, 19, 119–127. [Google Scholar] [CrossRef]
- Awotidebe, A.W.; Inglis-Jassiem, G.; Young, T. Does Low-level Laser Therapy Provide Additional Benefits to Exercise in Patients with Shoulder Musculoskeletal Disorders? A Meta-analysis of Randomised Controlled Trials. Ortop. Traumatol. Rehabil. 2019, 21, 407–416. [Google Scholar] [CrossRef] [PubMed]
- Clijsen, R.; Brunner, A.; Barbero, M.; Clarys, P.; Taeymans, J. Effects of low-level laser therapy on pain in patients with musculoskeletal disorders: A systematic review and meta-analysis. Eur. J. Phys. Rehabil. Med. 2017, 53, 603–610. [Google Scholar] [CrossRef] [PubMed]
- Haslerud, S.; Magnussen, L.H.; Joensen, J.; Lopes-Martins, R.A.B.; Bjordal, J.M. The Efficacy of Low-Level Laser Therapy for Shoulder Tendinopathy: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Physiother. Res. Int. 2015, 20, 108–125. [Google Scholar] [CrossRef]
- Emanet, S.K.; Altan, L.İ.; Yurtkuran, M. Investigation of the Effect of GaAs Laser Therapy on Lateral Epicondylitis. Photomed. Laser Surg. 2010, 28, 397–403. [Google Scholar] [CrossRef]
- Kaydok, E. Short-Term Efficacy Comparison of High-Intensity and Low-Intensity Laser Therapy in the Treatment of Lateral Epicondylitis: A Randomized Double-Blind Clinical Study. Arch. Rheumatol. 2020, 35, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Lam, L.K.Y.; Cheing, G.L.Y. Effects of 904-nm Low-Level Laser Therapy in the Management of Lateral Epicondylitis: A Randomized Controlled Trial. Photomed. Laser Surg. 2007, 25, 65–71. [Google Scholar] [CrossRef]
- Eslamian, F.; Shakouri, S.K.; Ghojazadeh, M.; Nobari, O.E.; Eftekharsadat, B. Effects of low-level laser therapy in combination with physiotherapy in the management of rotator cuff tendinitis. Lasers Med. Sci. 2012, 27, 951–958. [Google Scholar] [CrossRef]
- Bal, A.; Eksioglu, E.; Gurcay, E.; Gulec, B.; Karaahmet, O.; Cakci, A. Low-Level Laser Therapy in Subacromial Impingement Syndrome. Photomed. Laser Surg. 2009, 27, 31–36. [Google Scholar] [CrossRef]
- World Association for Photobiomodulation Therapy. WALT Recommendations—Dosage Recommendations 2010. 2010. Available online: https://waltpbm.org/documentation-links/recommendations/ (accessed on 31 July 2024).
- Bingöl, Ü.; Altan, L.; Yurtkuran, M. Low-Power Laser Treatment for Shoulder Pain. Photomed. Laser Surg. 2005, 23, 459–464. [Google Scholar] [CrossRef]
- Yeldan, I.; Cetin, E.; Razak Ozdincler, A. The effectiveness of low-level laser therapy on shoulder function in subacromial impingement syndrome. Disabil. Rehabil. 2009, 31, 935–940. [Google Scholar] [CrossRef]
- Tascioglu, F.; Degirmenci, N.A.; Ozkan, S.; Mehmetoglu, O. Low-level laser in the treatment of carpal tunnel syndrome: Clinical, electrophysiological, and ultrasonographical evaluation. Rheumatol. Int. 2012, 32, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Sommer, A.P. Mitochondrial cytochrome c oxidase is not the primary acceptor for near infrared light—It is mitochondrial bound water: The principles of low-level light therapy. Ann. Transl. Med. 2019, 7 (Suppl. 1), S13. [Google Scholar] [CrossRef] [PubMed]
- RHamblin, M. Mechanisms and applications of the anti-inflammatory effects of photobiomodulation. AIMS Biophys. 2017, 4, 337–361. [Google Scholar] [CrossRef] [PubMed]
- da Silva, T.G.; Ribeiro, R.S.; Mencalha, A.L.; de Souza Fonseca, A. Photobiomodulation at molecular, cellular, and systemic levels. Lasers Med. Sci. 2023, 38, 136. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.M.; Darafsheh, A. Light Sources and Dosimetry Techniques for Photodynamic Therapy. Photochem. Photobiol. 2020, 96, 280–294. [Google Scholar] [CrossRef]
- Esnouf, A.; Wright, P.A.; Moore, J.C.; Ahmed, S. Depth of Penetration of an 850nm Wavelength Low Level Laser in Human Skin. Acupunct. Electro-Ther. Res. 2007, 32, 81–86. [Google Scholar] [CrossRef]
- Souza-Barros, L.; Dhaidan, G.; Maunula, M.; Solomon, V.; Gabison, S.; Lilge, L.; Nussbaum, E.L. Skin color and tissue thickness effects on transmittance, reflectance, and skin temperature when using 635 and 808 nm lasers in low intensity therapeutics. Lasers Surg. Med. 2018, 50, 291–301. [Google Scholar] [CrossRef]
- De Marchi, T.; Schmitt, V.M.; Machado, G.P.; de Sene, J.S.; de Col, C.D.; Tairova, O.; Salvador, M.; Leal-Junior, E.C.P. Does photobiomodulation therapy is better than cryotherapy in muscle recovery after a high-intensity exercise? A randomized, double-blind, placebo-controlled clinical trial. Lasers Med. Sci. 2017, 32, 429–437. [Google Scholar] [CrossRef]
- Bettleyon, J.; Kaminski, T.W. Does Low-Level Laser Therapy Decrease Muscle-Damaging Mediators After Performance in Soccer Athletes Versus Sham Laser Treatment? A Critically Appraised Topic. J. Sport Rehabil. 2020, 29, 1210–1213. [Google Scholar] [CrossRef]
- Berni, M.; Brancato, A.M.; Torriani, C.; Bina, V.; Annunziata, S.; Cornella, E.; Trucchi, M.; Jannelli, E.; Mosconi, M.; Gastaldi, G.; et al. The Role of Low-Level Laser Therapy in Bone Healing: Systematic Review. Int. J. Mol. Sci. 2023, 24, 7094. [Google Scholar] [CrossRef]



| Literature Search In-Scope Criteria | Literature Search Out-of-Scope Criteria |
|---|---|
|
|
| Review | RCTs Evaluated | Laser Parameter Ranges | Outcome | LLLT Pre-, Post-Exertion or Both | Quality of Primary Research Evidence |
|---|---|---|---|---|---|
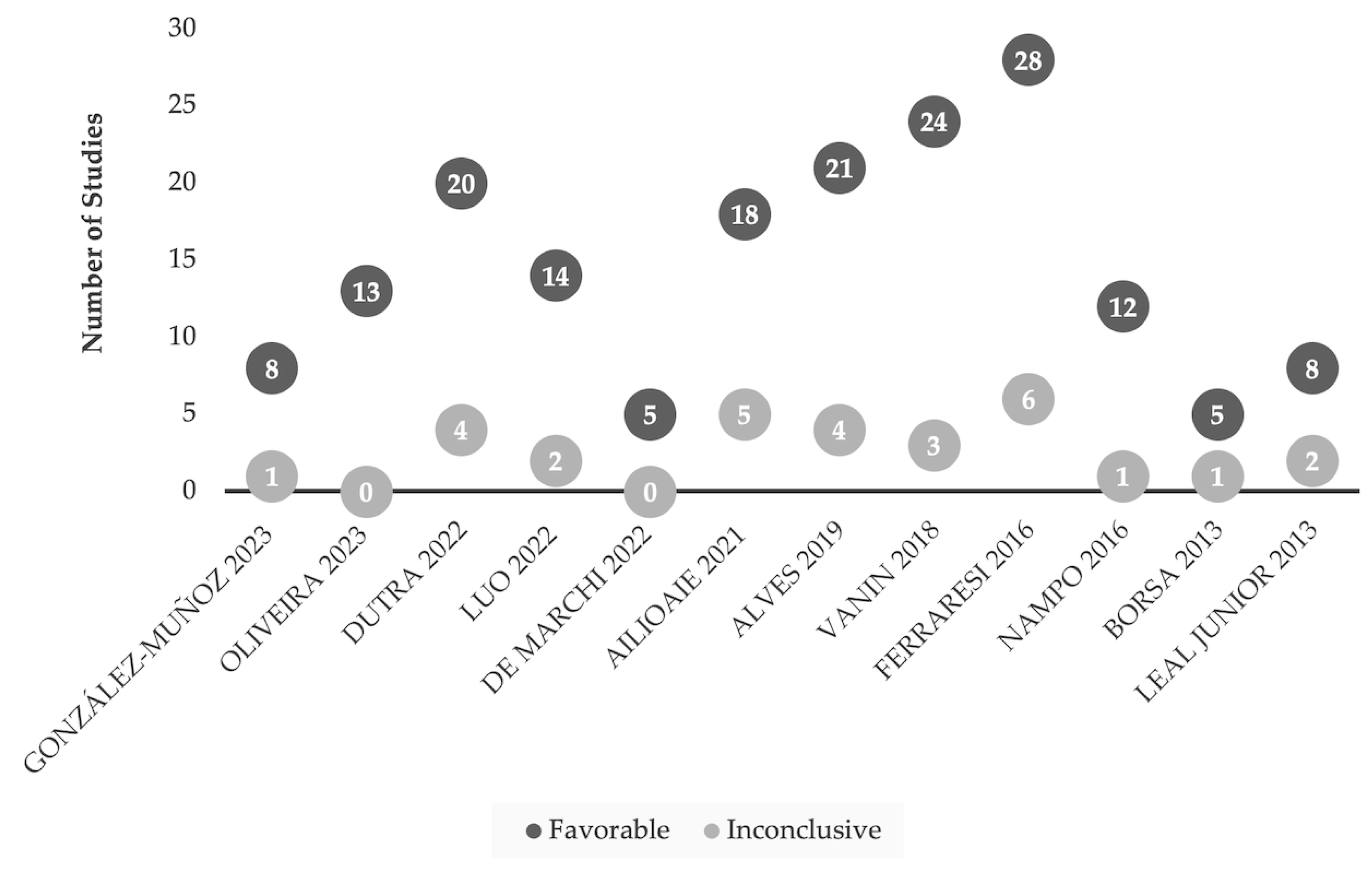
| González-Muñoz 2023 [17] |
| 810, 850, 905 nm 0.285–30 J/point; 30–60, 510, 850 J total 32–228 s 2–17, 85 exposure points | 8 of 9 favorable results | Pre-Exertion: 5 Post-Exertion: 1 Both: 2 | Low |
| Oliveira 2023 [18] |
| 660, 800–980 nm 0.095–50 J/point; 10–60, 180–480 J total 16–30 s–<6.5 min 3–17, 42 exposure points | 13 of 13 favorable results | Pre-Exertion: 9 Post-Exertion: 2 Both: 2 | Low |
| Dutra 2022 [28] |
| 660, 780–905 nm 0.81–60 J/point; 12–84, 100–540 J total 13–300 s 2–29 exposure points | 20 of 24 favorable results | Pre-Exertion: 20 | Low |
| Luo 2022 [19] |
| 632.8, 655 810–905 nm 0.285–45 J/point; 12–60, 135–405 J total 15–600 s 2–9, 17, 42, 85 exposure points | 14 of 16 favorable results | Pre-Exertion: 12 Post-Exertion: 1 Both: 1 | Low |
| De Marchi 2022 [20] |
| 810–905 nm 0.285–30 J/point; 30–68, 180, 300, 360 J total 25–228 s 6–17, 85 exposure points | 5 of 5 favorable results | Pre-Exertion: 3 Post-Exertion: 1 Both: 1 | Low |
| Ailioaie 2021 [21] |
| 640, 810–905 nm 0.095–50 J/point; 10–60, 180–540 J total 16–381 s 3–9, 17, 85 exposure points | 18 of 23 favorable results | Pre-Exertion: 12 Post-Exertion: 3 Both: 3 | Low |
| Alves 2019 [22] |
| 655–660, 808–950 nm 0.6–50 J/point; 1.92–60, 180–300 J total 8–300 s 2–12, 29, 30, 42 exposure points | 21 of 25 favorable results | Pre-Exertion: 16 Post-Exertion: 4 Both: 1 | Low |
| Vanin 2018 [23] |
| 660, 810–905 nm 0.285–50 J/point; 4–60, 180–360 J total 10–300 s 2–17, 30, 42 exposure points | 24 of 27 favorable results | Pre-Exertion: 16 Post-Exertion: 4 Both: 4 | Low |
| Ferraresi 2016 [24] |
| 660, 780, 808–950 nm 0.095–30 J/point; 4–60, 132–380 J total 10–720 s 1–7, 29, 42 exposure points | 28 of 34 favorable results | Pre-Exertion: 19 Post-Exertion: 5 Both: 4 | Low |
| Nampo 2016 [25] |
| 655, 660, 808–970 nm 0.6–30 J/point, 12–60, 180, 360 J total 20–240 s 2–12, 42 exposure points | 12 of 13 favorable results | Pre-Exertion: 11 Both: 1 | Low |
| Borsa 2013 [26] |
| 655, 810, 830 nm 3–40 J/point; 20–60 J total 30–100 s 2–5 exposure points | 5 of 6 favorable results | Pre-Exertion: 5 | Low |
| Leal Junior 2013 [27] |
| 655/660, 808/810, 830 nm 0.6–30 J/point, 12–60, 360 J total 30–600 s 2–12, 42 exposure points | 8 of 10 favorable results | Pre-Exertion: 7 Post-Exertion: 1 | Low |
| Review | RCTs Evaluated | Participant Injury | Laser Parameters | Outcome | Quality of Primary Research Evidence |
|---|---|---|---|---|---|
| Tripodi 2021 [93] |
|
| 830, 904/905 nm 1–4 J/cm2 11–30 or 120 s | 2 of 5 favorable results | Low |
| Taylor 2020 [94] |
|
| 830, 904/905 nm 2–4 J/cm2 11, 20, 90, 120 s | 1 of 4 favorable results | Low |
| Awotidebe 2020 [95] |
|
| 830, 904 nm 1.6–4 J/cm2 20, 60, 90, 120 s | 1 of 4 favorable results | Low |
| Clijsen 2017 [96] |
|
| 830, 905 nm 1 J/cm2 1 or 2 min | 0 of 2 favorable results | Low |
| Haslerud 2015 [97] |
|
| 830, 904 nm 2–4 J/cm2 20, 60, 90, 120 s | 1 of 4 favorable results | Low |
| Parameter | Low-Level Laser Therapy (LLLT) | Light Emitting Diode (LED) |
|---|---|---|
| Light Source | Light Amplification by Stimulated Emission of Radiation (LASER). Uses a gas or crystal medium to produce light; electricity passes through the medium causing electrons to emit photons that are amplified Laser diode: LASER; Class of lasers that generate laser radiation through a semiconductor; stimulated emission | LED from spontaneous emission. Use semiconductor materials and much simpler p-n junctions than laser diodes, to produce non-coherent (less directional), broad spectrum light; the process is called electroluminescence |
| Classification | Class IIIb: treatment of musculoskeletal conditions (e.g., sport performance, acute and chronic inflammatory conditions), would healing Class IV: similar to Class IIIb above but also deep tissue repair and rehabilitation | N/A |
| Emitted Light | Monochromatic | Broad spectral width (~5% of central wavelength) [110] |
| Coherency | Coherent light | Non-coherent light |
| Wavelength | 632.8–660 & 808–980 nm *,† | 630–980 nm [24,26] |
| Depth of Penetration | Both superficial and deeper structures; suggested to penetrate ≤50 mm [111] | Superficial; 2–10 mm [11] |
| Energy Density | 3–500 & 1071.43–1785 J/cm2 *,† | 1.5–8 J/cm2 [24,26] |
| Exposure Time | 8–720 s *,† | 30–360 s [24,26] |
| Power Output | Class IIIb: 5–500 mW; Class IV: >500 mW | 10–300 mW [24,26] |
| Skin Application | Direct contact or non-contact protocol for wounds | Direct contact or non-contact protocol for wounds |
| Other features | Wavelength specificity, in-clinic/professional treatments, targets treatment to damaged tissue | Lower cost device, possible at-home administration, may expose larger areas to treatment |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lawrence, J.; Sorra, K. Photobiomodulation as Medicine: Low-Level Laser Therapy (LLLT) for Acute Tissue Injury or Sport Performance Recovery. J. Funct. Morphol. Kinesiol. 2024, 9, 181. https://doi.org/10.3390/jfmk9040181
Lawrence J, Sorra K. Photobiomodulation as Medicine: Low-Level Laser Therapy (LLLT) for Acute Tissue Injury or Sport Performance Recovery. Journal of Functional Morphology and Kinesiology. 2024; 9(4):181. https://doi.org/10.3390/jfmk9040181
Chicago/Turabian StyleLawrence, Julia, and Karin Sorra. 2024. "Photobiomodulation as Medicine: Low-Level Laser Therapy (LLLT) for Acute Tissue Injury or Sport Performance Recovery" Journal of Functional Morphology and Kinesiology 9, no. 4: 181. https://doi.org/10.3390/jfmk9040181
APA StyleLawrence, J., & Sorra, K. (2024). Photobiomodulation as Medicine: Low-Level Laser Therapy (LLLT) for Acute Tissue Injury or Sport Performance Recovery. Journal of Functional Morphology and Kinesiology, 9(4), 181. https://doi.org/10.3390/jfmk9040181






