Comparison of Measurements for Recording Postural Control in Standing and Seated Position in Healthy Individuals
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
- Have you ever been told by a doctor that you have a cardiac condition and that you should only engage in exercise or sports under medical supervision?
- Have you experienced chest pain in the past month, either at rest or during physical exertion? Do you have difficulty breathing at rest or during physical activity? Have you ever fallen due to dizziness or lost consciousness? Do you have any bone or joint problems that could be exacerbated by physical activity? Have you ever been prescribed medication by a doctor for high blood pressure, or for a heart or respiratory condition?
- Are you aware of any other reason why you should not engage in physical activity?
2.2. Equipment
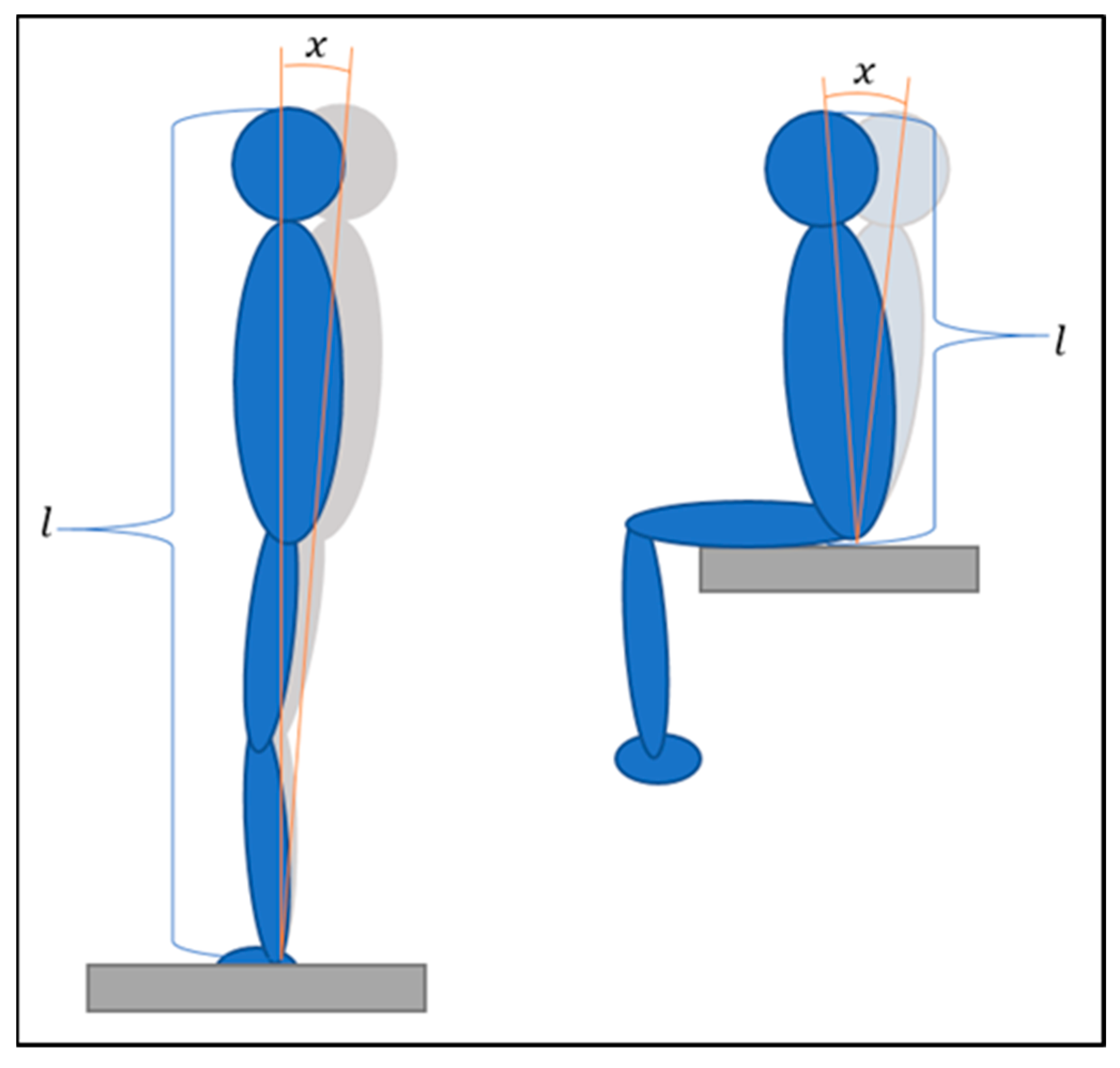
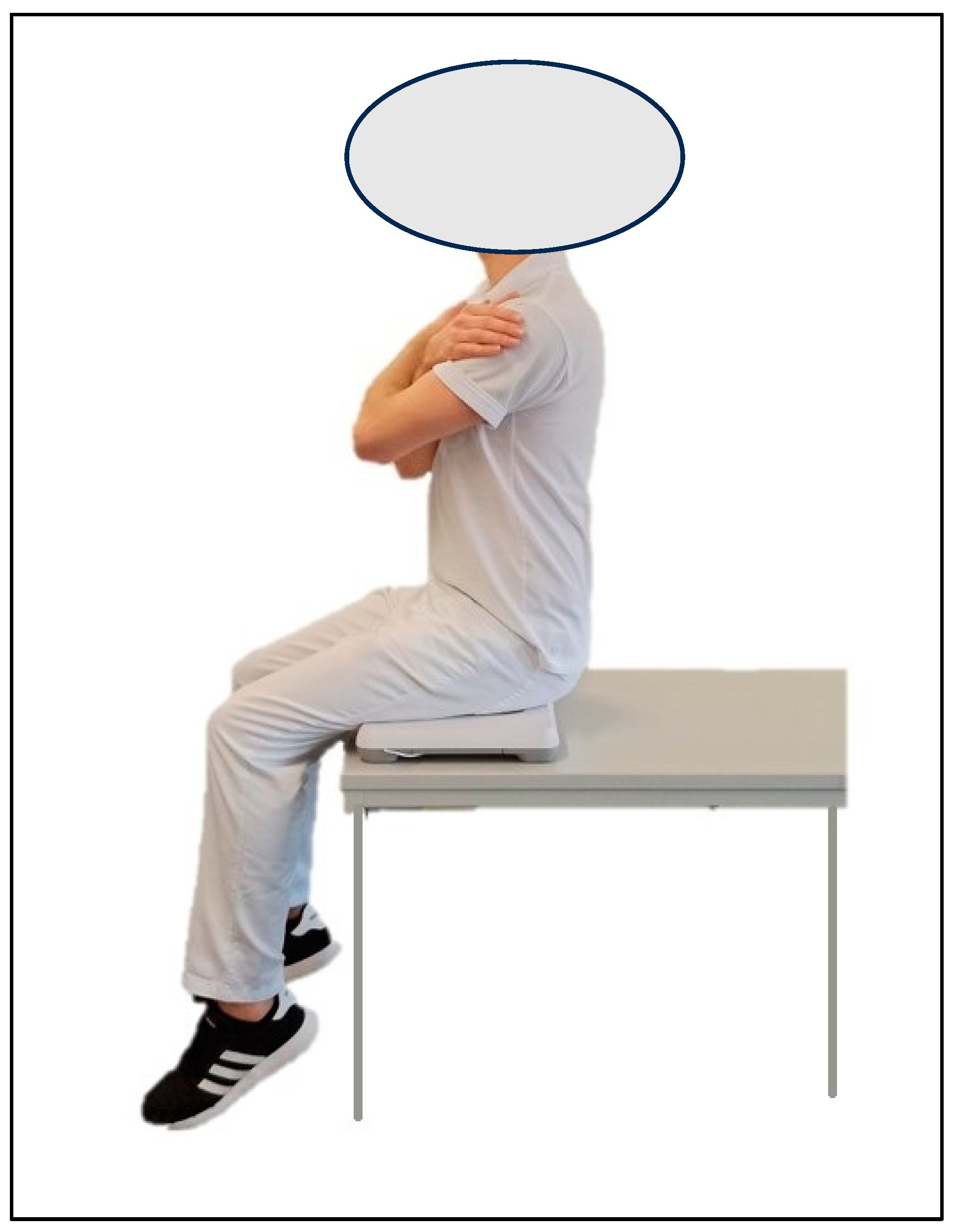
2.3. Procedures
2.4. Statistical Analysis
3. Results
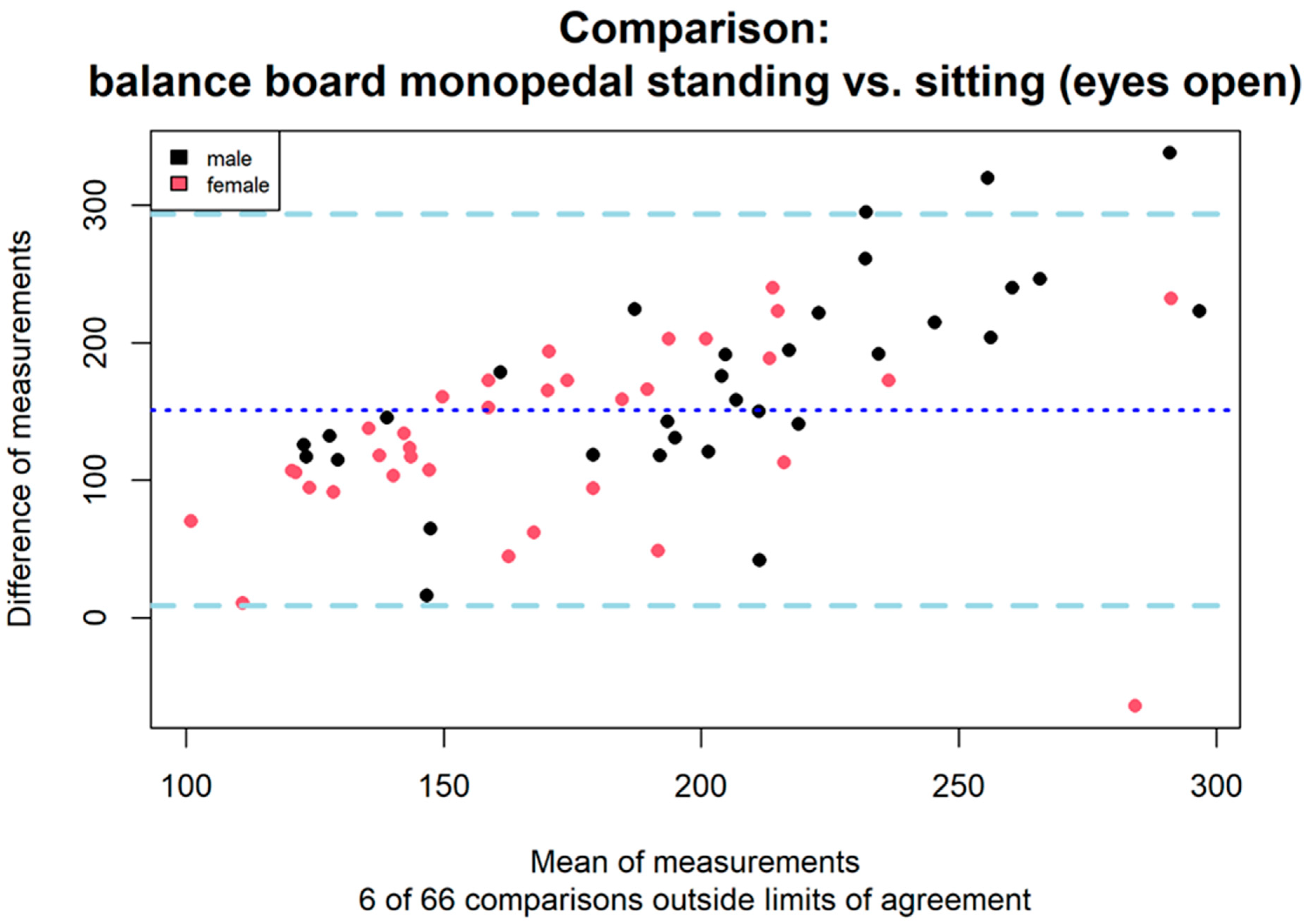
3.1. Comparison of Standing and Seated Position on the Balance Board
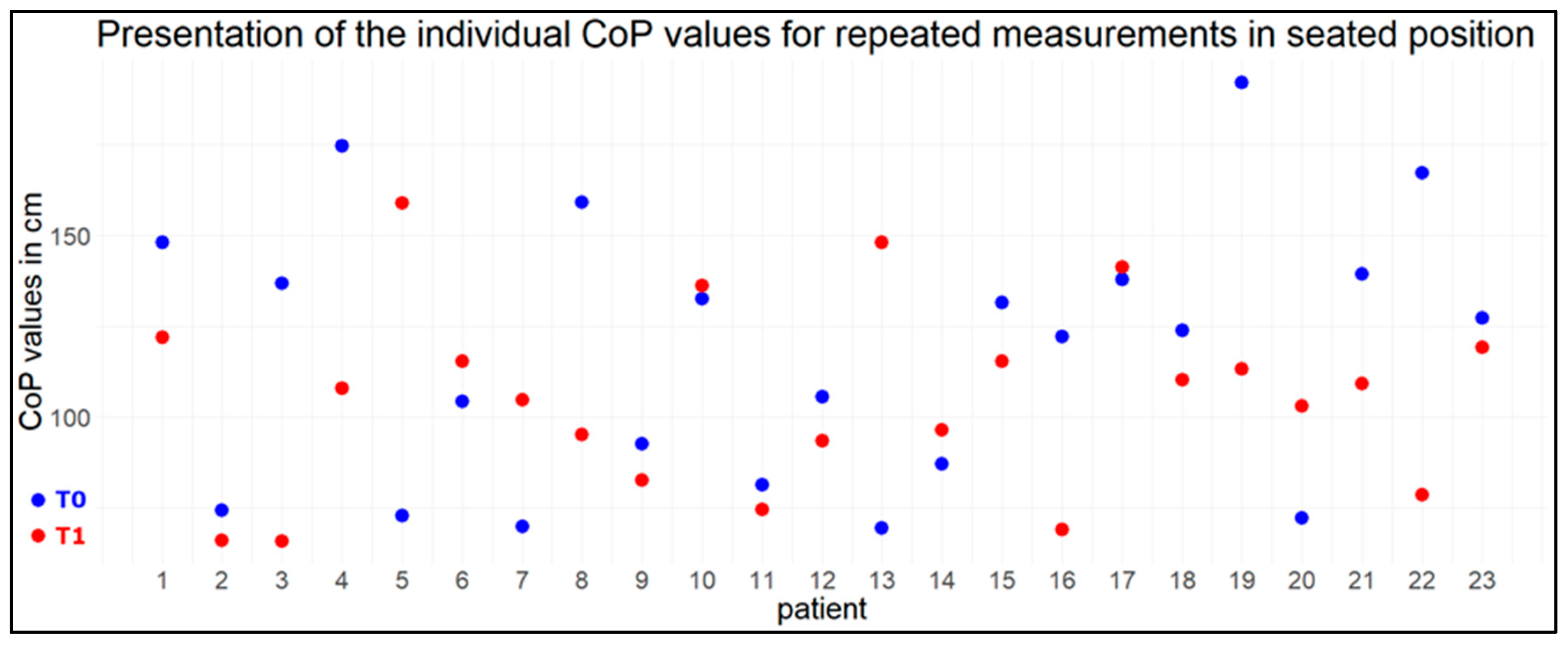
3.2. Reliability of the Measurements with the Balance Board
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ivanenko, Y.; Gurfinkel, V.S. Human postural control. Front. Neurosci. 2018, 12, 171. [Google Scholar] [CrossRef] [PubMed]
- Abelin-Genevois, K. Sagittal balance of the spine. Orthop. Traumatol. Surg. Res. 2021, 107, 102769. [Google Scholar] [CrossRef] [PubMed]
- Henry, M.; Baudry, S. Age-related changes in leg proprioception: Implications for postural control. J. Neurophysiol. 2019, 122, 525–538. [Google Scholar] [CrossRef] [PubMed]
- Comber, L.; Sosnoff, J.J.; Galvin, R.; Coote, S. Postural control deficits in people with Multiple Sclerosis: A systematic review and meta-analysis. Gait Posture 2018, 61, 445–452. [Google Scholar] [CrossRef]
- Moretto, G.F.; Santinelli, F.B.; Penedo, T.; Mochizuki, L.; Rinaldi, N.M.; Barbieri, F.A. Prolonged Standing Task Affects Adaptability of Postural Control in People with Parkinson’s Disease. Neurorehabil. Neural Repair. 2020, 35, 58–67. [Google Scholar] [CrossRef]
- Cameron, M.H.; Lord, S. Postural control in multiple sclerosis: Implications for fall prevention. Curr. Neurol. Neurosci. Rep. 2010, 10, 407–412. [Google Scholar] [CrossRef]
- Mokhtarinia, H.R.; Sanjari, M.A.; Chehrehrazi, M.; Kahrizi, S.; Parnianpour, M. Trunk coordination in healthy and chronic nonspecific low back pain subjects during repetitive flexion--extension tasks: Effects of movement asymmetry, velocity and load. Hum. Mov. Sci. 2016, 45, 182–192. [Google Scholar] [CrossRef]
- Demoulin, C.; Crielaard, J.-M.; Vanderthommen, M. Spinal muscle evaluation in healthy individuals and low-back-pain patients: A literature review. Jt. Bone Spine 2007, 74, 9–13. [Google Scholar] [CrossRef]
- Sung, W.; Abraham, M.; Plastaras, C.; Silfies, S.P. Trunk motor control deficits in acute and subacute low back pain are not associated with pain or fear of movement. Spine J. 2015, 15, 1772–1782. [Google Scholar] [CrossRef]
- Hartvigsen, J.; Hancock, M.J.; Kongsted, A.; Louw, Q.; Ferreira, M.L.; Genevay, S.; Hoy, D.; Karppinen, J.; Pransky, G.; Sieper, J.; et al. What low back pain is and why we need to pay attention. Lancet 2018, 391, 2356–2367. [Google Scholar] [CrossRef]
- Brumitt, J.; Matheson, J.W.; Meira, E.P. Core stabilization exercise prescription, part I: Current concepts in assessment and intervention. Sports Health 2013, 5, 504–509. [Google Scholar] [CrossRef] [PubMed]
- Lemos, L.F.C.; Teixeira, C.S.; Mota, C.B. Low back pain and corporal balance of female brazilian selection canoeing flatwater athletes. Brazilian J. Kinanthropometry Hum. Perform. 2010, 12, 457–463. [Google Scholar] [CrossRef]
- Ruhe, A.; Fejer, R.; Walker, B. Center of pressure excursion as a measure of balance performance in patients with non-specific low back pain compared to healthy controls: A systematic review of the literature. Eur. Spine J. 2011, 20, 358–368. [Google Scholar] [CrossRef]
- Doná, F.; Aquino, C.; Gazzola, J.; Borges, V.; Silva, S.; Ganança, F.; Caovilla, H.; Ferraz, H. Changes in postural control in patients with Parkinson’s disease: A posturographic study. Physiotherapy 2016, 102, 272–279. [Google Scholar] [CrossRef] [PubMed]
- Barbado, D.; Barbado, L.C.; Elvira, J.L.L.; van Dieën, J.H.; Vera-Garcia, F.J. Sports-related testing protocols are required to reveal trunk stability adaptations in high-level athletes. Gait Posture 2016, 49, 90–96. [Google Scholar] [CrossRef]
- Roerdink, M.; Hlavackova, P.; Vuillerme, N. Center-of-pressure regularity as a marker for attentional investment in postural control: A comparison between sitting and standing postures. Hum. Mov. Sci. 2011, 30, 203–212. [Google Scholar] [CrossRef]
- Winter, D.A.; Patla, A.E.; Ishac, M.; Gage, W.H. Motor mechanisms of balance during quiet standing. J. Electromyogr. Kinesiol. 2003, 13, 49–56. [Google Scholar] [CrossRef]
- Gage, W.H.; Winter, D.A.; Frank, J.S.; Adkin, A.L. Kinematic and kinetic validity of the inverted pendulum model in quiet standing. Gait Posture 2004, 19, 124–132. [Google Scholar] [CrossRef]
- Reinhardt, L.; Heilmann, F.; Teicher, M.; Lauenroth, A.; Delank, K.-S.; Schwesig, R.; Wollny, R.; Kurz, E. Comparison of posturographic outcomes between two different devices. J. Biomech. 2019, 86, 218–224. [Google Scholar] [CrossRef]
- Donath, L.; Roth, R.; Zahner, L.; Faude, O. Testing single and double limb standing balance performance: Comparison of COP path length evaluation between two devices. Gait Posture 2012, 36, 439–443. [Google Scholar] [CrossRef]
- Koltermann, J.J.; Gerber, M.; Beck, H.; Beck, M. Validation of the HUMAC balance system in comparison with conventional force plates. Technologies 2017, 5, 44. [Google Scholar] [CrossRef]
- Leach, J.M.; Mancini, M.; Peterka, R.J.; Hayes, T.L.; Horak, F.B. Validating and calibrating the Nintendo Wii balance board to derive reliable center of pressure measures. Sensors 2014, 14, 18244–18267. [Google Scholar] [CrossRef] [PubMed]
- Lu, M.-J.; Zhong, W.-H.; Liu, Y.-X.; Miao, H.-Z.; Li, Y.-C.; Ji, M.-H. Sample size for assessing agreement between two methods of measurement by Bland-Altman method. Int. J. Biostat. 2016, 12. [Google Scholar] [CrossRef] [PubMed]
- Schoonjans, F. MedCalc Statistical Software—Free Trial. MedCalc. 2023. Available online: https://www.medcalc.org (accessed on 24 June 2024).
- PAR-Q-Fragebogen. Available online: http://www.hwrun.de/par-q-fragebogen.pdf (accessed on 4 January 2021).
- Klasen, B.W.; Hallner, D.; Schaub, C.; Willburger, R.; Hasenbring, M. Validation and reliability of the German version of the Chronic Pain Grade questionnaire in primary care back pain patients. Psychosoc. Med. 2004, 1, Doc07. [Google Scholar]
- Koltermann, J.J.; Gerber, M. Quantification of the Dependence of the Measurement Error on the Quantization of the A/D Converter for Center of Pressure Measurements. Biomechanics 2022, 2, 309–318. [Google Scholar] [CrossRef]
- Koltermann, J.J.; Gerber, M.; Beck, H.; Beck, M. Validation of Different Filters for Center of Pressure Measurements by a Cross-Section Study. Technologies 2019, 7, 68. [Google Scholar] [CrossRef]
- Hwang, S.; Huang, C.-T.; Cherng, R.-J.; Huang, C.-C. Postural fluctuations during pointing from a unilateral or bilateral stance. Hum. Mov. Sci. 2006, 25, 275–291. [Google Scholar] [CrossRef]
- Donath, L.; Kurz, E.; Roth, R.; Zahner, L.; Faude, O. Different ankle muscle coordination patterns and co-activation during quiet stance between young adults and seniors do not change after a bout of high intensity training. BMC Geriatr. 2015, 15, 19. [Google Scholar] [CrossRef] [PubMed]
- Genthon, N.; Vuillerme, N.; Monnet, J.P.; Petit, C.; Rougier, P. Biomechanical assessment of the sitting posture maintenance in patients with stroke. Clin. Biomech. 2007, 22, 1024–1029. [Google Scholar] [CrossRef]
- Grangeon, M.; Gauthier, C.; Duclos, C.; Lemay, J.-F.; Gagnon, D. Unsupported eyes closed sitting and quiet standing share postural control strategies in healthy individuals. Motor Control 2015, 19, 10–24. [Google Scholar] [CrossRef]
- de Oliveira, M.R.; Fabrin, L.F.; de Oliveira Gil, A.W.; Benassi, G.H.; Camargo, M.Z.; da Silva, R.A.; de Lima, R.R. Acute effect of core stability and sensory-motor exercises on postural control during sitting and standing positions in young adults. J. Bodyw. Mov. Ther. 2021, 28, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Bland, J.M.; Altman, D.G. Measuring agreement in method comparison studies. Stat. Methods Med. Res. 1999, 8, 135–160. [Google Scholar] [CrossRef]
- Lakens, D. Equivalence tests: A practical primer for t tests, correlations, and meta-analyses. Soc. Psychol. Personal. Sci. 2017, 8, 355–362. [Google Scholar] [CrossRef]
- Wellek, S. On powerful exact nonrandomized tests for the Poisson two-sample setting. Stat. Methods Med. Res. 2020, 29, 2538–2553. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; Foundation for Statistical Computing: Vienna, Austria, 2013. [Google Scholar]
- Vuillerme, N.; Nougier, V. Attentional demand for regulating postural sway: The effect of expertise in gymnastics. Brain Res. Bull. 2004, 63, 161–165. [Google Scholar] [CrossRef]
- Smith, C.E.; Nyland, J.; Caudill, P.; Brosky, J.; Caborn, D.N.M. Dynamic trunk stabilization: A conceptual back injury prevention program for volleyball athletes. J. Orthop. Sport. Phys. Ther. 2008, 38, 703–720. [Google Scholar] [CrossRef]
- Mann, R.; Herman, J. Kinematic analysis of Olympic sprint performance: Men’s 200 meters. J. Appl. Biomech. 1985, 1, 151–162. [Google Scholar] [CrossRef]
- Avrillon, S.; Guilhem, G.; Barthelemy, A.; Hug, F. Coordination of hamstrings is individual specific and is related to motor performance. J. Appl. Physiol. 2018, 125, 1069–1079. [Google Scholar] [CrossRef]
- Zemková, E.; Zapletalová, L. The role of neuromuscular control of postural and core stability in functional movement and athlete performance. Front. Physiol. 2022, 13, 796097. [Google Scholar] [CrossRef]
- Glofcheskie, G.O.; Brown, S.H.M. Athletic background is related to superior trunk proprioceptive ability, postural control, and neuromuscular responses to sudden perturbations. Hum. Mov. Sci. 2017, 52, 74–83. [Google Scholar] [CrossRef]
- Imai, A.; Kaneoka, K.; Okubo, Y.; Shiraki, H. Effects of two types of trunk exercises on balance and athletic performance in youth soccer players. Int. J. Sports Phys. Ther. 2014, 9, 47. [Google Scholar] [PubMed]
| Mean | ±SD | |
|---|---|---|
| CoP balance board monopedal standing (average value of the two limbs) in cm | 256.71 | 5.14 |
| CoP balance board sitting (average value) in cm | 124.06 | 20.12 |
| Extension force in Nm/kg | 3.32 | 0.798 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Floessel, P.; Hammerschmidt, F.; Koltermann, J.J.; Foerster, J.; Beck, H.; Disch, A.C.; Datzmann, T. Comparison of Measurements for Recording Postural Control in Standing and Seated Position in Healthy Individuals. J. Funct. Morphol. Kinesiol. 2024, 9, 178. https://doi.org/10.3390/jfmk9040178
Floessel P, Hammerschmidt F, Koltermann JJ, Foerster J, Beck H, Disch AC, Datzmann T. Comparison of Measurements for Recording Postural Control in Standing and Seated Position in Healthy Individuals. Journal of Functional Morphology and Kinesiology. 2024; 9(4):178. https://doi.org/10.3390/jfmk9040178
Chicago/Turabian StyleFloessel, Philipp, Franziska Hammerschmidt, Jan Jens Koltermann, Justin Foerster, Heidrun Beck, Alexander Carl Disch, and Thomas Datzmann. 2024. "Comparison of Measurements for Recording Postural Control in Standing and Seated Position in Healthy Individuals" Journal of Functional Morphology and Kinesiology 9, no. 4: 178. https://doi.org/10.3390/jfmk9040178
APA StyleFloessel, P., Hammerschmidt, F., Koltermann, J. J., Foerster, J., Beck, H., Disch, A. C., & Datzmann, T. (2024). Comparison of Measurements for Recording Postural Control in Standing and Seated Position in Healthy Individuals. Journal of Functional Morphology and Kinesiology, 9(4), 178. https://doi.org/10.3390/jfmk9040178








