Physical Function, Self-Perceived Physical Fitness, Falls, Quality of Life and Degree of Disability According to Fear and Risk of Falling in Women with Fibromyalgia
Abstract
1. Introduction
- (1)
- Women with FM with fear of falling have worse physical test performance, a higher number of previous falls, worse perceived physical condition, worse health-related quality of life, worse self-perceived health, and a greater degree of disability due to the disease than women without fear of falling.
- (2)
- Women with FM at risk of falls have worse performance on physical tests, a higher number of previous falls, worse perceived physical condition, worse health-related quality of life, worse self-perceived health, and a greater degree of disability due to the disease than women without risk of falls.
- (3)
- There are correlations between physical function, perceived physical condition, previous falls, health-related quality of life, self-perceived health, and degree of disability due to the disease with fear of falling (assessed with the FES-I) and risk of falling (assessed with the ABC Scale).
2. Materials and Methods
2.1. Design and Participants
2.2. Procedures
- Physical test
- Questionnaires
2.3. Statistical Analysis
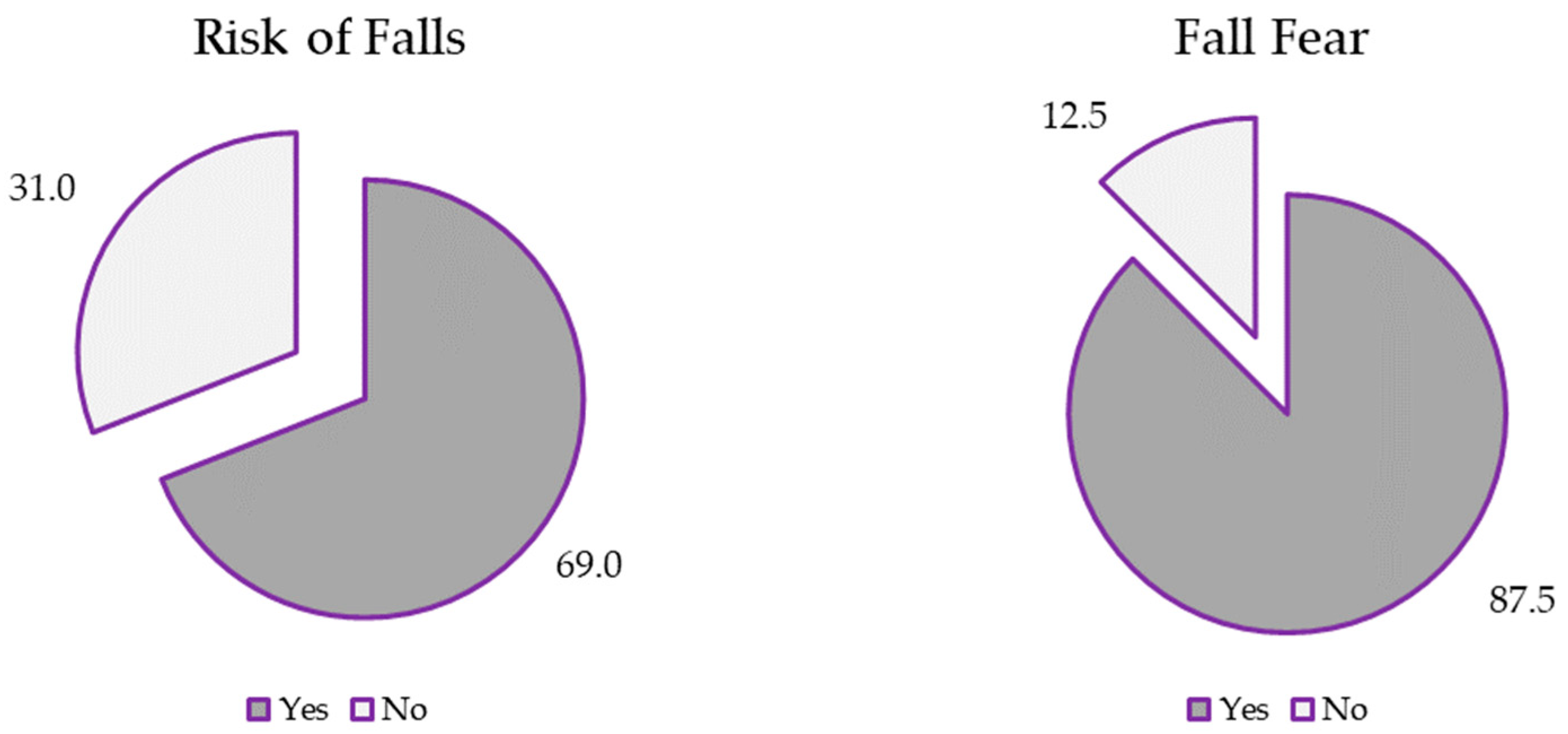
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vilarino, G.T.; Andreato, L.V.; de Souza, L.C.; Branco, J.H.L.; Andrade, A. Effects of Resistance Training on the Mental Health of Patients with Fibromyalgia: A Systematic Review. Clin. Rheumatol. 2021, 40, 4417–4425. [Google Scholar] [CrossRef] [PubMed]
- Sarzi-Puttini, P.; Giorgi, V.; Marotto, D.; Atzeni, F. Fibromyalgia: An Update on Clinical Characteristics, Aetiopathogenesis and Treatment. Nat. Rev. Rheumatol. 2020, 16, 645–660. [Google Scholar] [CrossRef] [PubMed]
- Fietta, P.; Fietta, P.; Manganelli, P. Fibromyalgia and Psychiatric Disorders. Acta Biomed.-Ateneo Parm. 2007, 78, 88. [Google Scholar]
- Işık-Ulusoy, S. Evaluation of Affective Temperament and Anxiety-Depression Levels in Fibromyalgia Patients: A Pilot Study. Braz. J. Psychiatry 2019, 41, 428–432. [Google Scholar] [CrossRef]
- Andrade, A.; Vilarino, G.T.; Sieczkowska, S.M.; Coimbra, D.R.; Steffens, R.d.A.K.; Vietta, G.G. Acute Effects of Physical Exercises on the Inflammatory Markers of Patients with Fibromyalgia Syndrome: A Systematic Review. J. Neuroimmunol. 2018, 316, 40–49. [Google Scholar] [CrossRef]
- Córdoba-Torrecilla, S.; Aparicio, V.; Soriano-Maldonado, A.; Estévez-López, F.; Segura-Jiménez, V.; Álvarez-Gallardo, I.; Femia, P.; Delgado-Fernández, M. Physical Fitness Is Associated with Anxiety Levels in Women with Fibromyalgia: The al-Ándalus Project. Qual. Life Res. 2016, 25, 1053–1058. [Google Scholar] [CrossRef]
- Mingorance, J.A.; Montoya, P.; Miranda, J.G.V.; Riquelme, I. An Observational Study Comparing Fibromyalgia and Chronic Low Back Pain in Somatosensory Sensitivity, Motor Function and Balance. Healthcare 2021, 9, 1533. [Google Scholar] [CrossRef]
- Lee, L.K.; Ebata, N.; Hlavacek, P.; DiBonaventura, M.; Cappelleri, J.C.; Sadosky, A. Humanistic and Economic Burden of Fibromyalgia in Japan. J. Pain Res. 2016, 9, 967–978. [Google Scholar] [CrossRef]
- Booth, J.; Moseley, G.L.; Schiltenwolf, M.; Cashin, A.; Davies, M.; Hübscher, M. Exercise for Chronic Musculoskeletal Pain: A Biopsychosocial Approach. Musculoskelet. Care 2017, 15, 413–421. [Google Scholar] [CrossRef]
- Singh, R.; Rai, N.K.; Pathak, A.; Rai, J.; Pakhare, A.; Kashyap, P.V.; Rozatkar, A.R.; Mishra, S.; Mudda, S. Impact of Fibromyalgia Severity on Patients Mood, Sleep Quality, and Quality of Life. J. Neurosci. Rural Pract. 2024, 15, 320. [Google Scholar] [CrossRef]
- Antunes, M.; Cruz, A.T.; Januário, P.D.O.; Marques, A.P. AB1552-HPR health perception of patients with fibromyalgia in Brazil. Ann. Rheum. Dis. 2022, 81, 1876–1877. [Google Scholar] [CrossRef]
- Jones, K.D.; Horak, F.B.; Winters-Stone, K.; Irvine, J.M.; Bennett, R.M. Fibromyalgia Is Associated with Impaired Balance and Falls. JCR J. Clin. Rheumatol. 2009, 15, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Núñez-Fuentes, D.; Obrero-Gaitán, E.; Zagalaz-Anula, N.; Ibáñez-Vera, A.J.; Achalandabaso-Ochoa, A.; López-Ruiz, M.D.; Rodríguez-Almagro, D.; Lomas-Vega, R. Alteration of Postural Balance in Patients with Fibromyalgia Syndrome—A Systematic Review and Meta-Analysis. Diagnostics 2021, 11, 127. [Google Scholar] [CrossRef] [PubMed]
- Huijnen, I.P.; Verbunt, J.A.; Meeus, M.; Smeets, R.J. Energy Expenditure during Functional Daily Life Performances in Patients with Fibromyalgia. Pain Pract. 2015, 15, 748–756. [Google Scholar] [CrossRef] [PubMed]
- Murillo-Garcia, A.; Villafaina, S.; Leon-Llamas, J.L.; Sánchez-Gómez, J.; Domínguez-Muñoz, F.J.; Collado-Mateo, D.; Gusi, N. Mobility Assessment under Dual Task Conditions in Women with Fibromyalgia: A Test-retest Reliability Study. PMR 2021, 13, 66–72. [Google Scholar] [CrossRef]
- Collado-Mateo, D.; Gallego-Diaz, J.M.; Adsuar, J.C.; Domínguez-Muñoz, F.J.; Olivares, P.; Gusi, N. Fear of Falling in Women with Fibromyalgia and Its Relation with Number of Falls and Balance Performance. BioMed Res. Int. 2015, 2015, 589014. [Google Scholar] [CrossRef][Green Version]
- Meireles, S.A.; Antero, D.C.; Kulczycki, M.M.; Skare, T.L. Prevalence of Falls in Fibromyalgia Patients. Acta Ortop. Bras. 2014, 22, 163–166. [Google Scholar] [CrossRef]
- Russek, L.; Gardner, S.; Maguire, K.; Stevens, C.; Brown, E.Z.; Jayawardana, V.; Mondal, S. A Cross-Sectional Survey Assessing Sources of Movement-Related Fear among People with Fibromyalgia Syndrome. Clin. Rheumatol. 2015, 34, 1109–1119. [Google Scholar] [CrossRef]
- Cigarán-Méndez, M.; Úbeda-D’Ocasar, E.; Arias-Buría, J.L.; Fernández-de-Las-Peñas, C.; Gallego-Sendarrubias, G.M.; Valera-Calero, J.A. The Hand Grip Force Test as a Measure of Physical Function in Women with Fibromyalgia. Sci. Rep. 2022, 12, 3414. [Google Scholar] [CrossRef]
- Sarıhan, K.; Uzkeser, H.; Erdal, A. Evaluation of Balance, Fall Risk, and Related Factors in Patients with Fibromyalgia Syndrome. Turk. J. Phys. Med. Rehabil. 2021, 67, 409. [Google Scholar] [CrossRef]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and Elaboration. Int. J. Surg. 2014, 12, 1500–1524. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, F.; Rasker, J.J.; Ten Klooster, P.; Häuser, W.; Rasker, J.J.J.; Klooster, P. Subjective Cognitive Dysfunction in Patients with and without Fibromyalgia: Prevalence, Predictors, Correlates, and Consequences. Cureus 2021, 13, e20351. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez, F.A. Cuestionario de Aptitud Para La Actividad Física (C-AAF), Versión Catalana/Castellana Del PAR-Q Revisado. Apunt. Med. De L" Esport (Castell.) 1994, 31, 301–310. [Google Scholar]
- Carbonell-Baeza, A.; Álvarez-Gallardo, I.C.; Segura-Jiménez, V.; Castro-Piñero, J.; Ruiz, J.; Delgado-Fernández, M.; Aparicio, V.A. Reliability and Feasibility of Physical Fitness Tests in Female Fibromyalgia Patients. Int. J. Sports Med. 2015, 36, 157–162. [Google Scholar] [CrossRef]
- Beauchet, O.; Fantino, B.; Allali, G.; Muir, S.W.; Montero-Odasso, M.; Annweiler, C. Timed up and Go Test and Risk of Falls in Older Adults: A Systematic Review. J. Nutr. Health Aging 2011, 15, 933–938. [Google Scholar] [CrossRef]
- Dite, W.; Temple, V.A. A Clinical Test of Stepping and Change of Direction to Identify Multiple Falling Older Adults. Arch. Phys. Med. Rehabil. 2002, 83, 1566–1571. [Google Scholar] [CrossRef]
- Carlos-Vivas, J.; Pérez-Gómez, J.; Delgado-Gil, S.; Campos-López, J.C.; Granado-Sánchez, M.; Rojo-Ramos, J.; Muñoz-Bermejo, L.; Barrios-Fernandez, S.; Mendoza-Muñoz, M.; Prado-Solano, A. Cost-Effectiveness of “Tele-Square Step Exercise” for Falls Prevention in Fibromyalgia Patients: A Study Protocol. Int. J. Environ. Res. Public Health 2020, 17, 695. [Google Scholar] [CrossRef]
- Izquierdo-Alventosa, R.; Inglés, M.; Cortés-Amador, S.; Gimeno-Mallench, L.; Chirivella-Garrido, J.; Kropotov, J.; Serra-Añó, P. Low-Intensity Physical Exercise Improves Pain Catastrophizing and Other Psychological and Physical Aspects in Women with Fibromyalgia: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2020, 17, 3634. [Google Scholar] [CrossRef]
- Andersson, M.; Moberg, L.; Svantesson, U.; Sundbom, A.; Johansson, H.; Emtner, M. Measuring Walking Speed in COPD: Test-Retest Reliability of the 30-Metre Walk Test and Comparison with the 6-Minute Walk Test. Prim. Care Respir. J. 2011, 20, 434–440. [Google Scholar] [CrossRef]
- Spagnuolo, D.L.; Jürgensen, S.P.; Iwama, Â.M.; Dourado, V.Z. Walking for the Assessment of Balance in Healthy Subjects Older than 40 Years. Gerontology 2010, 56, 467–473. [Google Scholar] [CrossRef]
- Rikli, R.E.; Jones, C.J. Development and Validation of Criterion-Referenced Clinically Relevant Fitness Standards for Maintaining Physical Independence in Later Years. Gerontol. 2013, 53, 255–267. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Ruiz, J.; Mesa, J.L.; Gutiérrez, A.; Castillo, M.J. Hand Size Influences Optimal Grip Span in Women but Not in Men. J. Hand Surg. 2002, 27, 897–901. [Google Scholar] [CrossRef] [PubMed]
- Luciano, J.V.; Aguado, J.; Serrano-Blanco, A.; Calandre, E.P.; Rodriguez-Lopez, C.M. Dimensionality, Reliability, and Validity of the Revised Fibromyalgia Impact Questionnaire in Two Spanish Samples. Arthritis Care Res. 2013, 65, 1682–1689. [Google Scholar] [CrossRef] [PubMed]
- Salgueiro, M.; García-Leiva, J.M.; Ballesteros, J.; Hidalgo, J.; Molina, R.; Calandre, E.P. Validation of a Spanish Version of the Revised Fibromyalgia Impact Questionnaire (FIQR). Health Qual. Life Outcomes 2013, 11, 132. [Google Scholar] [CrossRef]
- Ishimoto, Y.; Wada, T.; Kasahara, Y.; Kimura, Y.; Fukutomi, E.; Chen, W.; Hirosaki, M.; Nakatsuka, M.; Fujisawa, M.; Sakamoto, R. Fall Risk Index Predicts Functional Decline Regardless of Fall Experiences among Community-dwelling Elderly. Geriatr. Gerontol. Int. 2012, 12, 659–666. [Google Scholar] [CrossRef]
- Montilla-Ibáñez, A.; Martínez-Amat, A.; Lomas-Vega, R.; Cruz-Díaz, D.; Torre-Cruz, M.J.D.l.; Casuso-Pérez, R.; Hita-Contreras, F. The Activities-Specific Balance Confidence Scale: Reliability and Validity in Spanish Patients with Vestibular Disorders. Disabil. Rehabil. 2017, 39, 697–703. [Google Scholar] [CrossRef]
- Yardley, L.; Beyer, N.; Hauer, K.; Kempen, G.; Piot-Ziegler, C.; Todd, C. Development and Initial Validation of the Falls Efficacy Scale-International (FES-I). Age Ageing 2005, 34, 614–619. [Google Scholar] [CrossRef]
- Kempen, G.I.J.M.; Todd, C.J.; Van Haastregt, J.C.M.; Rixt Zijlstra, G.A.; Beyer, N.; Freiberger, E.; Hauer, K.A.; Piot-Ziegler, C.; Yardley, L. Cross-Cultural Validation of the Falls Efficacy Scale International (FES-I) in Older People: Results from Germany, the Netherlands and the UK Were Satisfactory. Disabil. Rehabil. 2007, 29, 155–162. [Google Scholar] [CrossRef]
- Lomas-Vega, R.; Hita-Contreras, F.; Mendoza, N.; Martínez-Amat, A. Cross-Cultural Adaptation and Validation of the Falls Efficacy Scale International in Spanish Postmenopausal Women. Menopause 2012, 19, 904–908. [Google Scholar] [CrossRef]
- Rutledge, D.N.; Martinez, A.; Traska, T.K.; Rose, D.J. Fall Experiences of Persons with Fibromyalgia over 6 Months. J. Adv. Nurs. 2013, 69, 435–448. [Google Scholar] [CrossRef]
- Peinado-Rubia, A.; Osuna-Pérez, M.C.; Rodríguez-Almagro, D.; Zagalaz-Anula, N.; López-Ruiz, M.C.; Lomas-Vega, R. Impaired Balance in Patients with Fibromyalgia Syndrome: Predictors of the Impact of This Disorder and Balance Confidence. Int. J. Environ. Res. Public Health 2020, 17, 3160. [Google Scholar] [CrossRef] [PubMed]
- Costa, I.d.S.; Gamundí, A.; Miranda, J.G.V.; França, L.G.S.; De Santana, C.N.; Montoya, P. Altered Functional Performance in Patients with Fibromyalgia. Front. Hum. Neurosci. 2017, 11, 14. [Google Scholar] [CrossRef] [PubMed]
- Leon-Llamas, J.L.; Murillo-Garcia, A.; Villafaina, S.; Domínguez-Muñoz, F.J.; Morenas, J.; Gusi, N. Relationship between Kinesiophobia and Mobility, Impact of the Disease, and Fear of Falling in Women with and without Fibromyalgia: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 8257. [Google Scholar] [CrossRef] [PubMed]
- SH, K. Kinesiophobia: A New View of Chronic Pain Behavior. Pain Manag. 1990, 3, 35–43. [Google Scholar]
- Luque-Suarez, A.; Martinez-Calderon, J.; Falla, D. Role of Kinesiophobia on Pain, Disability and Quality of Life in People Suffering from Chronic Musculoskeletal Pain: A Systematic Review. Br. J. Sports Med. 2019, 53, 554–559. [Google Scholar] [CrossRef]
- Varallo, G.; Scarpina, F.; Giusti, E.M.; Cattivelli, R.; Guerrini Usubini, A.; Capodaglio, P.; Castelnuovo, G. Does Kinesiophobia Mediate the Relationship between Pain Intensity and Disability in Individuals with Chronic Low-Back Pain and Obesity? Brain Sci. 2021, 11, 684. [Google Scholar] [CrossRef]
- Collado-Mateo, D.; Dominguez-Muñoz, F.J.; Adsuar, J.C.; Merellano-Navarro, E.; Gusi, N. Exergames for Women with Fibromyalgia: A Randomised Controlled Trial to Evaluate the Effects on Mobility Skills, Balance and Fear of Falling. PeerJ 2017, 5, e3211. [Google Scholar] [CrossRef]
| Variables | Fear of Falling (FES-I) | ||||||
|---|---|---|---|---|---|---|---|
| Yes (n = 70) | No (n = 10) | ||||||
| Mdn | (IQR) | Mdn | (IQR) | p | rho | p† | |
| i-Time Up and Go test (s) | 5.25 | (2.79) | 4.69 | (2.21) | 0.242 | 0.187 | 0.0.97 |
| Time Up and Go test (s) | 7.70 | (3.26) | 6.58 | (1.21) | 0.123 | 0.406 | <0.001 ** |
| Delta Time Up and Go test | 9.45 | (13.04) | 10.24 | (7.87) | 0.919 | 0.154 | 0.172 |
| Dual Time Up and Go test (s) | 9.25 | (4.77) | 7.70 | (2.07) | 0.078 | 0.419 | <0.001 ** |
| Four Step Square test (s) | 7.33 | (2.44) | 5.48 | (2.24) | 0.022 | 0.363 | 0.001 * |
| 4 m Walking test (s) | 2.70 | (0.77) | 2.26 | (0.63) | 0.156 | 0.255 | 0.024 |
| 30 m Walking test (s) | 19.15 | (7.25) | 17.35 | (5.31) | 0.250 | 0.170 | 0.142 |
| 6 min Walking test (m) | 483 | (159) | 510 | (203) | 0.381 | −0.168 | 0.147 |
| 30” Sit to Stand test (rep) | 10 | (5) | 12 | (2) | 0.045 | −0.375 | 0.001 * |
| Dual 30” Sit to Stand test (rep) | 9 | (3) | 11 | (1) | 0.035 | −0.323 | 0.003 |
| 5 reps Sit to Stand test (s) | 13.50 | (5.00) | 12.38 | (2.00) | 0.120 | 0.356 | 0.001 * |
| Max Strength Handgrip (kg) | 22.5 | (6.8) | 24.3 | (7.0) | 0.103 | −0.291 | 0.103 |
| Max Strength/Weight Ratio | 0.29 | (0.12) | 0.39 | (0.13) | 0.004 | −0.345 | 0.009 |
| 30” Biceps Curl test (rep) | 14 | (6) | 17 | (6) | 0.060 | −0.203 | 0.008 |
| Functional reach test (cm) | 34.5 | (13.5) | 35.3 | (9.9) | 0.948 | 0.014 | 0.902 |
| Sit and Reach (cm) | −2.0 | (10.5) | 4.0 | (16.8) | 0.051 | −0.320 | 0.005 |
| Back Scratch (cm) | −4.5 | (14) | −0.3 | (7.6) | 0.087 | −0.206 | 0.066 |
| Variables | Fear of Falling (FES-I) | ||||||
|---|---|---|---|---|---|---|---|
| Yes (n = 70) | No (n = 10) | ||||||
| Mdn | (IQR) | Mdn | (IQR) | p | rho | p† | |
| IFIS (Score 5–25) | 12 | (4) | 17 | (4) | 0.001 * | −0.572 | <0.001 ** |
| EQ-5D-5L Index | 0.159 | (0.291) | 0.464 | (0.226) | <0.001 ** | −0.560 | <0.001 ** |
| EQ-5D-5L VAS | 49.0 | (36.5) | 65.0 | (20.3) | 0.029 | −0.295 | 0.008 |
| FIQ-R Function (Score 0–30) | 18.7 | (10.3) | 8.0 | (10.5) | <0.001 ** | 0.689 | <0.001 ** |
| FIQ-R Impact (Score 0–20) | 13.0 | (6.0) | 3.0 | (12.0) | 0.003 * | 0.639 | <0.001 ** |
| FIQ-R Symptoms (Score 0–50) | 34.5 | (10.0) | 25.0 | (6.3) | 0.001 * | 0.676 | <0.001 ** |
| FIQ-R (Score 0–100) | 64.7 | (23.3) | 36.5 | (28.5) | <0.001 ** | 0.731 | <0.001 ** |
| Variables | Risk of Falling (ABC Scale) | ||||||
|---|---|---|---|---|---|---|---|
| Yes (n = 58) | No (n = 26) | ||||||
| Mdn | (IQR) | Mdn | (IQR) | p | rho | p† | |
| i-Time Up and Go test (s) | 5.27 | (2.68) | 5.17 | (2.94) | 0.985 | −0.074 | 0.506 |
| Time Up and Go test (s) | 7.93 | (3.34) | 6.58 | (2.06) | 0.017 | −0.269 | 0.013 |
| Delta Time Up and Go test | 10.31 | (13.70) | 7.29 | (8.60) | 0.056 | −0.133 | 0.229 |
| Dual Time Up and Go test (s) | 9.90 | (4.74) | 8.20 | (3.08) | 0.040 | −0.240 | 0.028 |
| Four Step Square test (s) | 7.44 | (2.42) | 6.52 | (2.31) | 0.077 | −0.256 | 0.019 |
| 4 m Walking test (s) | 2.78 | (0.91) | 2.47 | (0.53) | 0.025 | −0.225 | 0.042 |
| 30 m Walking test (s) | 19.59 | (6.10) | 18.47 | (5.16) | 0.302 | −0.084 | 0.460 |
| 6 min Walking test (m) | 467 | (143) | 505 | (201) | 0.227 | 0.136 | 0.228 |
| 30” Sit to Stand test (rep) | 10 | (4) | 11 | (4) | 0.097 | 0.257 | 0.018 |
| Dual 30” Sit to Stand test (rep) | 9 | (4) | 10 | (2) | 0.444 | 0.196 | 0.074 |
| 5 reps Sit to Stand test (s) | 13.63 | (6.00) | 12.39 | (4.00) | 0.026 | −0.276 | 0.012 |
| Max Strength Handgrip (kg) | 22.0 | (6.5) | 23.9 | 5.1) | 0.174 | 0.218 | 0.046 |
| Max Strength/Weight Ratio | 0.30 | (0.13) | 0.34 | (0.15) | 0.336 | 0.184 | 0.160 |
| 30” Biceps Curl test (rep) | 15 | (7) | 14 | (8) | 0.834 | −0.013 | 0.904 |
| Functional reach test (cm) | 32.8 | (13.6) | 35.5 | (11.5) | 0.117 | 0.083 | 0.451 |
| Sit and Reach (cm) | −4.0 | (12.5) | 2.0 | (12.3) | 0.002 * | 0.266 | 0.016 |
| Back Scratch (cm) | −7.5 | (15.0) | 0.5 | (7.5) | 0.003 | 0.269 | 0.013 |
| Variables | Risk of Falling (ABC Scale) | ||||||
|---|---|---|---|---|---|---|---|
| Yes (n = 58) | No (n = 26) | ||||||
| Mdn | (IQR) | Mdn | (IQR) | p | rho | p† | |
| IFIS (Score 5–25) | 12 | (4) | 15 | (5) | 0.001 * | 0.446 | <0.001 ** |
| EQ-5D-5L Index | 0.134 | (0.306) | 0.306 | (0.304) | 0.004 | 0.479 | <0.001 ** |
| EQ-5D-5L VAS | 45.5 | (30.0) | 60.0 | (25.5) | 0.001 * | 0.439 | <0.001 ** |
| FIQ Function (Score 0–30) | 18.7 | (8.2) | 11.3 | (11.6) | 0.001 * | −0.578 | <0.001 ** |
| FIQ-R Impact (Score 0–20) | 13.0 | (6.0) | 8.5 | (12.3) | 0.010 | −0.412 | <0.001 ** |
| FIQ-R Symptoms (Score 0–50) | 34.8 | (8.4) | 26.5 | (14.1) | 0.002 * | −0.531 | <0.001 ** |
| FIQ-R (Score 0–100) | 65.5 | (22.6) | 46.6 | (33.7) | 0.001 * | −0.580 | <0.001 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Denche-Zamorano, Á.; Pereira-Payo, D.; Collado-Mateo, D.; Adsuar-Sala, J.C.; Tomas-Carus, P.; Parraca, J.A. Physical Function, Self-Perceived Physical Fitness, Falls, Quality of Life and Degree of Disability According to Fear and Risk of Falling in Women with Fibromyalgia. J. Funct. Morphol. Kinesiol. 2024, 9, 174. https://doi.org/10.3390/jfmk9030174
Denche-Zamorano Á, Pereira-Payo D, Collado-Mateo D, Adsuar-Sala JC, Tomas-Carus P, Parraca JA. Physical Function, Self-Perceived Physical Fitness, Falls, Quality of Life and Degree of Disability According to Fear and Risk of Falling in Women with Fibromyalgia. Journal of Functional Morphology and Kinesiology. 2024; 9(3):174. https://doi.org/10.3390/jfmk9030174
Chicago/Turabian StyleDenche-Zamorano, Ángel, Damián Pereira-Payo, Daniel Collado-Mateo, José Carmelo Adsuar-Sala, Pablo Tomas-Carus, and Jose Alberto Parraca. 2024. "Physical Function, Self-Perceived Physical Fitness, Falls, Quality of Life and Degree of Disability According to Fear and Risk of Falling in Women with Fibromyalgia" Journal of Functional Morphology and Kinesiology 9, no. 3: 174. https://doi.org/10.3390/jfmk9030174
APA StyleDenche-Zamorano, Á., Pereira-Payo, D., Collado-Mateo, D., Adsuar-Sala, J. C., Tomas-Carus, P., & Parraca, J. A. (2024). Physical Function, Self-Perceived Physical Fitness, Falls, Quality of Life and Degree of Disability According to Fear and Risk of Falling in Women with Fibromyalgia. Journal of Functional Morphology and Kinesiology, 9(3), 174. https://doi.org/10.3390/jfmk9030174









