The Influence of Sonographer Experience on Skeletal Muscle Image Acquisition and Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Sonographers
2.4. B-Mode Ultrasonography Image Acquisition
2.5. Image Analysts
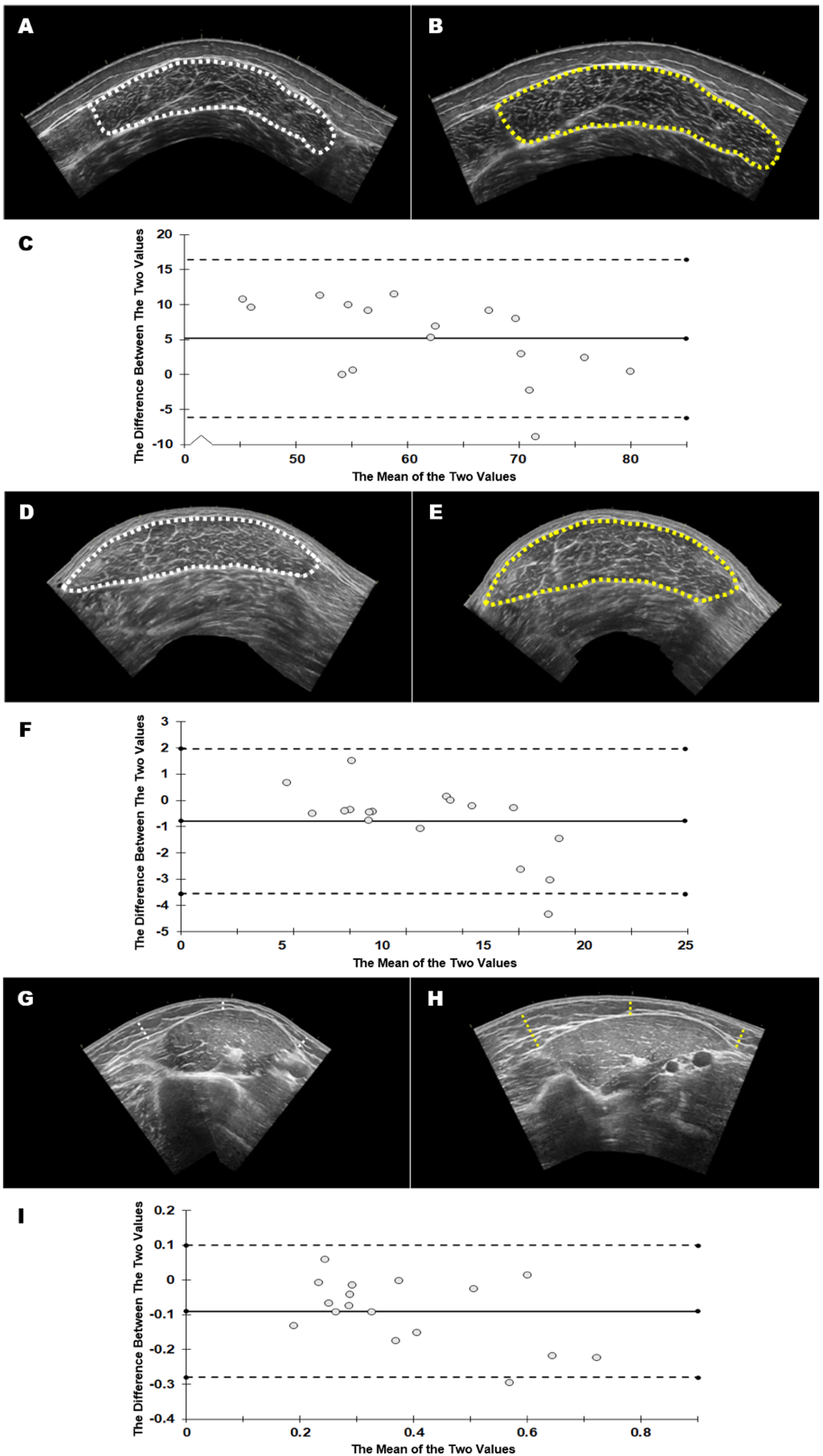
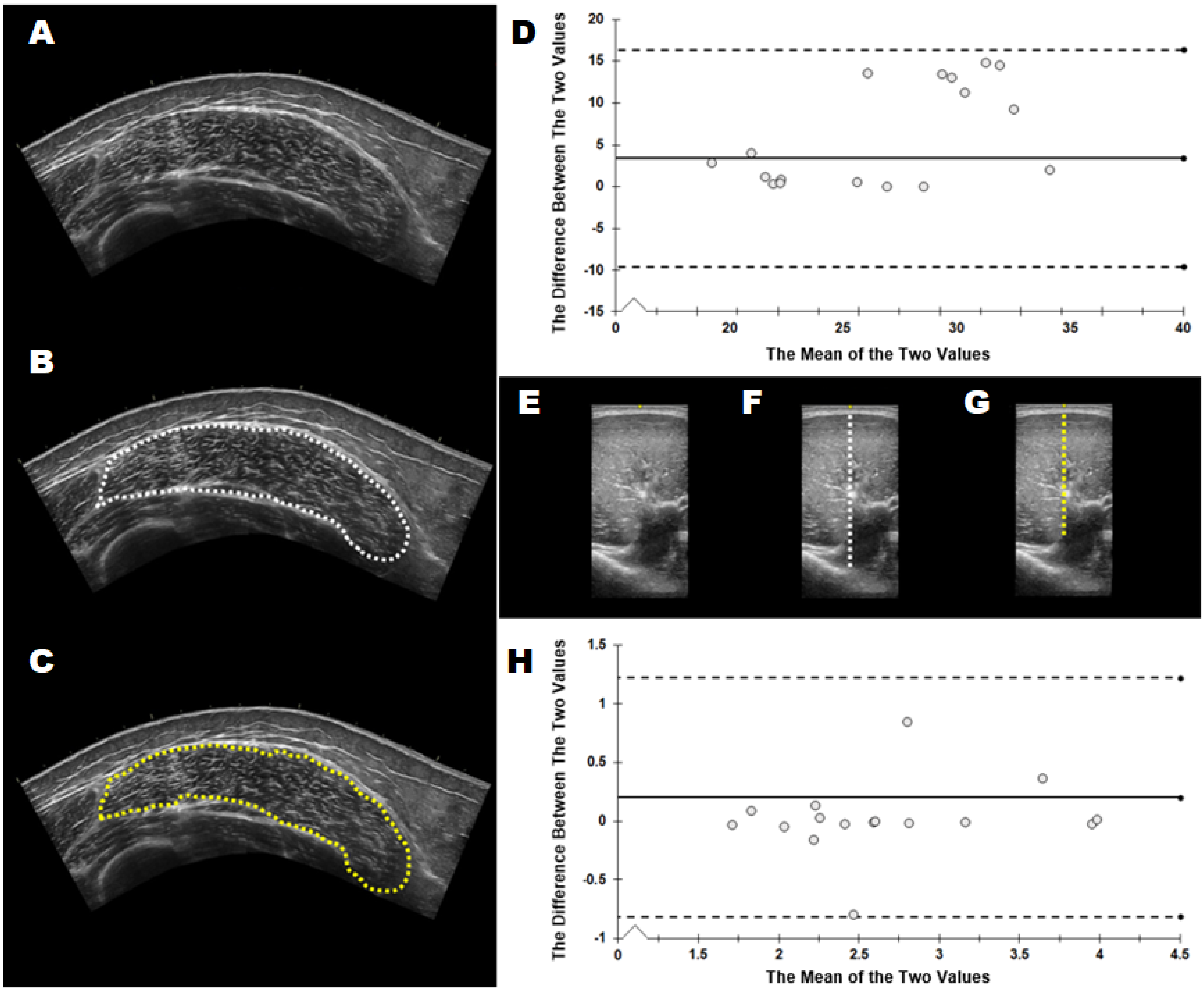
2.6. B-Mode Ultrasonography Image Analysis
2.7. Statistical Analysis
3. Results
3.1. Image Acquisition
3.2. Image Analysis
4. Discussion
4.1. Muscle Cross-Sectional Area
4.2. Echo Intensity and Subcutaneous Adipose Tissue Thickness
4.3. Muscle Thickness
4.4. Ultrasound Considerations for Novice Onboarding
4.5. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Stokes, T.; Tripp, T.R.; Murphy, K.; Morton, R.W.; Oikawa, S.Y.; Choi, H.L.; McGrath, J.; McGlory, C.; MacDonald, M.J.; Phillips, S.M. Methodological Considerations for and Validation of the Ultrasonographic Determination of Human Skeletal Muscle Hypertrophy and Atrophy. Physiol. Rep. 2021, 9, e14683. [Google Scholar] [CrossRef]
- Noorkoiv, M.; Nosaka, K.; Blazevich, A.J. Assessment of Quadriceps Muscle Cross-Sectional Area by Ultrasound Extended-Field-of-View Imaging. Eur. J. Appl. Physiol. 2010, 109, 631–639. [Google Scholar] [CrossRef] [PubMed]
- Scott, J.M.; Martin, D.S.; Ploutz-Snyder, R.; Caine, T.; Matz, T.; Arzeno, N.M.; Buxton, R.; Ploutz-Snyder, L. Reliability and Validity of Panoramic Ultrasound for Muscle Quantification. Ultrasound Med. Biol. 2012, 38, 1656–1661. [Google Scholar] [CrossRef]
- Ahtiainen, J.P.; Hoffren, M.; Hulmi, J.J.; Pietikäinen, M.; Mero, A.A.; Avela, J.; Häkkinen, K. Panoramic Ultrasonography Is a Valid Method to Measure Changes in Skeletal Muscle Cross-Sectional Area. Eur. J. Appl. Physiol. 2009, 108, 273. [Google Scholar] [CrossRef]
- Abe, T.; DeHoyos, D.V.; Pollock, M.L.; Garzarella, L. Time Course for Strength and Muscle Thickness Changes Following Upper and Lower Body Resistance Training in Men and Women. Eur. J. Appl. Physiol. 2000, 81, 174–180. [Google Scholar] [CrossRef]
- MacLennan, R.J.; Sahebi, M.; Becker, N.; Davis, E.; Garcia, J.M.; Stock, M.S. Declines in Skeletal Muscle Quality vs. Size Following Two Weeks of Knee Joint Immobilization. PeerJ 2020, 8, e8224. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stock, M.S.; Whitson, M.; Burton, A.M.; Dawson, N.T.; Sobolewski, E.J.; Thompson, B.J. Echo Intensity Versus Muscle Function Correlations in Older Adults Are Influenced by Subcutaneous Fat Thickness. Ultrasound Med. Biol. 2018, 44, 1597–1605. [Google Scholar] [CrossRef] [PubMed]
- Stock, M.S.; Mota, J.A.; Hernandez, J.M.; Thompson, B.J. Echo Intensity and Muscle Thickness as Predictors of Athleticism and Isometric Strength in Middle-School Boys. Muscle Nerve 2017, 55, 685–692. [Google Scholar] [CrossRef]
- Gerstner, G.; Thompson, B.; Rosenberg, J.; Sobolewski, E.; Scharville, M.; Ryan, E. Neural and Muscular Contributions to the Age-Related Reductions in Rapid Strength. Med. Sci. Sports Exerc. 2017, 49, 1331–1339. [Google Scholar] [CrossRef]
- Gerstner, G.R.; Giuliani, H.K.; Mota, J.A.; Ryan, E.D. Age-Related Reductions in Muscle Quality Influence the Relative Differences in Strength and Power. Exp. Gerontol. 2017, 99, 27–34. [Google Scholar] [CrossRef]
- Mayer, K.P.; Dhar, S.; Cassity, E.; Denham, A.; England, J.; Morris, P.E.; Dupont-Versteegden, E.E. Interrater Reliability of Muscle Ultrasonography Image Acquisition by Physical Therapists in Patients Who Have or Who Survived Critical Illness. Phys. Ther. 2020, 100, 1701–1711. [Google Scholar] [CrossRef]
- Zaidman, C.M.; Wu, J.S.; Wilder, S.; Darras, B.T.; Rutkove, S.B. Minimal Training Is Required to Reliably Perform Quantitative Ultrasound of Muscle. Muscle Nerve 2014, 50, 124–128. [Google Scholar] [CrossRef]
- Rosenberg, J.G.; Ryan, E.D.; Sobolewski, E.J.; Scharville, M.J.; Thompson, B.J.; King, G.E. Reliability of Panoramic Ultrasound Imaging to Simultaneously Examine Muscle Size and Quality of the Medial Gastrocnemius. Muscle Nerve 2014, 49, 736–740. [Google Scholar] [CrossRef]
- Jenkins, N.D.M.; Miller, J.M.; Buckner, S.L.; Cochrane, K.C.; Bergstrom, H.C.; Hill, E.C.; Smith, C.M.; Housh, T.J.; Cramer, J.T. Test–Retest Reliability of Single Transverse versus Panoramic Ultrasound Imaging for Muscle Size and Echo Intensity of the Biceps Brachii. Ultrasound Med. Biol. 2015, 41, 1584–1591. [Google Scholar] [CrossRef]
- Tomko, P.M.; Muddle, T.W.; Magrini, M.A.; Colquhoun, R.J.; Luera, M.J.; Jenkins, N.D. Reliability and Differences in Quadriceps Femoris Muscle Morphology Using Ultrasonography: The Effects of Body Position and Rest Time. Ultrasound 2018, 26, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Sobolewski, E.J.; Wein, L.D.; Crow, J.M.; Carpenter, K.M. Intra-Rater and Inter-Rater Reliability of the Process of Obtaining Cross-Sectional Area and Echo Intensity Measurements of Muscles from Ultrasound Images. J. Ultrason. 2021, 21, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Dankel, S.J.; Abe, T.; Bell, Z.W.; Jessee, M.B.; Buckner, S.L.; Mattocks, K.T.; Mouser, J.G.; Loenneke, J.P. The Impact of Ultrasound Probe Tilt on Muscle Thickness and Echo-Intensity: A Cross-Sectional Study. J. Clin. Densitom. 2020, 23, 630–638. [Google Scholar] [CrossRef]
- Treece, G.M.; Prager, R.W.; Gee, A.H.; Berman, L. Correction of Probe Pressure Artifacts in Freehand 3D Ultrasound. Med. Image Anal. 2002, 6, 199–214. [Google Scholar] [CrossRef]
- Cleary, C.; Nabavizadeh, O.; Young, K.; Herda, A. Inter- and Intra-Rater Reliability of Ultrasound-Derived Muscle Quantification, 2021.
- Wang, J.; Hu, Y.; Tian, G. Ultrasound Measurements of Gastrocnemius Muscle Thickness in Older People with Sarcopenia. Clin. Interv. Aging 2018, 13, 2193–2199. [Google Scholar] [CrossRef] [Green Version]
- Barber, L.; Barrett, R.; Lichtwark, G. Validity and Reliability of a Simple Ultrasound Approach to Measure Medial Gastrocnemius Muscle Length. J. Anat. 2011, 218, 637–642. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; L. Erlbaum Associates: Hillsdale, MI, USA, 1988; ISBN 978-0-8058-0283-2. [Google Scholar]
- Bland, J.M.; Altman, D.G. Statistical Methods for Assessing Agreement between Two Methods of Clinical Measurement. Lancet Lond. Engl. 1986, 1, 307–310. [Google Scholar] [CrossRef]
- Shrout, P.E.; Fleiss, J.L. Intraclass Correlations: Uses in Assessing Rater Reliability. Psychol. Bull. 1979, 86, 420–428. [Google Scholar] [CrossRef] [PubMed]
- Weir, J.P. Quantifying Test-Retest Reliability Using the Intraclass Correlation Coefficient and the SEM. J. Strength Cond. Res. 2005, 19, 231. [Google Scholar] [CrossRef] [PubMed]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schoenfeld, B.J.; Ratamess, N.A.; Peterson, M.D.; Contreras, B.; Tiryaki-Sonmez, G. Influence of Resistance Training Frequency on Muscular Adaptations in Well-Trained Men. J. Strength Cond. Res. 2015, 29, 1821–1829. [Google Scholar] [CrossRef] [Green Version]
- Nunes, J.P.; Costa, B.D.V.; Kassiano, W.; Kunevaliki, G.; Castro-e-Souza, P.; Rodacki, A.L.F.; Fortes, L.S.; Cyrino, E.S. Different Foot Positioning During Calf Training to Induce Portion-Specific Gastrocnemius Muscle Hypertrophy. J. Strength Cond. Res. 2020, 34, 2347–2351. [Google Scholar] [CrossRef]
- Stock, M.S.; Mota, J.A.; DeFranco, R.N.; Grue, K.A.; Jacobo, A.U.; Chung, E.; Moon, J.R.; DeFreitas, J.M.; Beck, T.W. The Time Course of Short-Term Hypertrophy in the Absence of Eccentric Muscle Damage. Eur. J. Appl. Physiol. 2017, 117, 989–1004. [Google Scholar] [CrossRef]
- Abe, T.; Loenneke, J.P.; Thiebaud, R.S.; Loftin, M. Morphological and Functional Relationships with Ultrasound Measured Muscle Thickness of the Upper Extremity and Trunk. Ultrasound J. Br. Med. Ultrasound Soc. 2014, 22, 229–235. [Google Scholar] [CrossRef] [Green Version]
- Cronin, N.J.; Finni, T.; Seynnes, O. Fully Automated Analysis of Muscle Architecture from B-Mode Ultrasound Images with Deep Learning. arXiv 2020, arXiv:2009.04790. [Google Scholar]
| Transverse Thickness (cm) | Sagittal Thickness (cm) | CSA (cm2) | EI (A.U.) | Subcutaneous Thickness (cm) | |
|---|---|---|---|---|---|
| Vastus Lateralis | |||||
| Experienced | 2.39 ± 0.52 | 2.38 ± 0.54 | 27.04 ± 9.23 | 64.48 ± 8.96 | 1.17 ± 0.65 |
| Novice | 2.49 ± 0.41 | 2.46 ± 0.45 | 26.74 ± 8.65 | 59.32 ± 12.09 | 1.22 ± 0.62 |
| % Mean Difference | 4.18 | 3.36 | 1.11 | 8.00 | 4.27 |
| Medial Gastrocnemius | |||||
| Experienced | 1.86 ± 0.41 | 1.84 ± 0.36 | 11.74 ± 3.98 | 110.56 ± 9.84 | 0.585 ± 0.240 |
| Novice | 1.90 ± 0.38 | 1.90 ± 0.42 | 12.53 ± 4.93 | 110.14 ± 9.49 | 0.587 ± 0.248 |
| % Mean Difference | 2.15 | 3.26 | 6.73 | 0.38 | 1.72 |
| Biceps Brachii | |||||
| Experienced | 2.61 ± 0.77 | 2.44 ± 0.77 | 9.65 ± 5.54 | 120.87 ± 8.93 | 0.341 ± 0.144 |
| Novice | 2.79 ± 0.78 | 2.64 ± 0.92 | 10.00 ± 6.19 | 123.53 ± 11.87 | 0.431 ± 0.192 |
| % Mean Difference | 6.90 | 8.20 | 3.63 | 2.20 | 26.47 |
| Transverse Thickness (cm) | Sagittal Thickness (cm) | CSA (cm2) | EI (A.U.) | Subcutaneous Thickness (cm) | |
|---|---|---|---|---|---|
| Vastus Lateralis | |||||
| p | 0.136 | 0.288 | 0.417 | 0.002 * | 0.334 |
| d | 0.381 | 0.267 | 0.202 | 0.898 | 0.241 |
| 95% CI | −0.237–0.035 | −0.203–0.066 | −0.468–1.074 | 2.208–8.123 | −0.158–0.057 |
| Limits of Agreement | −0.621–0.419 | −0.594–0.452 | −2.637–3.243 | −6.110–16.440 | −0.461–0.360 |
| Upper–Lower Limit | |||||
| ICC2,1 | 0.826 | 0.854 | 0.986 | 0.77 | 0.945 |
| SEM (raw units) | 0.19 | 0.19 | 1.06 | 4.07 | 0.15 |
| SEM (%) | 7.69 | 7.79 | 3.95 | 6.57 | 12.38 |
| MD | 0.52 | 0.52 | 2.94 | 11.27 | 0.41 |
| Medial Gastrocnemius | |||||
| p | 0.226 | 0.105 | 0.035 * | 0.838 | 0.92 |
| d | 0.305 | 0.416 | 0.559 | 0.05 | 0.025 |
| 95% CI | −0.118–0.030 | −0.137–0.014 | −1.512–−0.063 | −3.859–4.697 | −0.039–0.035 |
| Limits of Agreement | −0.325–0.238 | −0.351–0.228 | −3.551–1.976 | −15.888–16.727 | −0.143–0.149 |
| Upper–Lower Limit | |||||
| ICC2,1 | 0.932 | 0.92 | 0.939 | 0.643 | 0.959 |
| SEM (raw units) | 0.10 | 0.10 | 1.00 | 5.88 | 0.05 |
| SEM (%) | 5.41 | 5.58 | 8.22 | 5.33 | 8.71 |
| MD | 0.28 | 0.29 | 2.76 | 16.31 | 0.14 |
| Biceps Brachii | |||||
| p | 0.082 | 0.078 | 0.28 | 0.341 | 0.002 * |
| d | 0.45 | 0.456 | 0.271 | 0.238 | 0.926 |
| 95% CI | −0.365–0.024 | −0.418–0.025 | −1.019–0.315 | −8.394–3.078 | −0.139–0.040 |
| Limits of Agreement | −0.913–0.571 | −1.040–0.647 | −2.894–2.190 | −24.524–19.207 | −0.279–0.100 |
| Upper–Lower Limit | |||||
| ICC2,1 | 0.867 | 0.856 | 0.975 | 0.437 | 0.74 |
| SEM (raw units) | 0.27 | 0.30 | 0.92 | 7.89 | 0.07 |
| SEM (%) | 9.91 | 11.97 | 9.34 | 6.46 | 17.74 |
| MD | 0.74 | 0.84 | 2.54 | 21.87 | 0.19 |
| Transverse Thickness (cm) | Sagittal Thickness (cm) | CSA (cm2) | EI (A.U.) | Subcutaneous Thickness (cm) | |
|---|---|---|---|---|---|
| Vastus Lateralis | |||||
| Experienced | 2.44 ± 0.46 | 2.42 ± 0.49 | 26.89 ± 8.81 | 61.90 ± 10.80 | 1.20 ± 0.62 |
| Novice | 2.58 ± 0.54 | 2.58 ± 0.54 | 23.49 ± 8.12 | 61.98 ± 11.52 | 1.12 ± 0.52 |
| % Mean Difference | 5.95 | 6.78 | 12.64 | 0.13 | 6.40 |
| Medial Gastrocnemius | |||||
| Experienced | 1.87 ± 0.39 | 1.87 ± 0.38 | 12.13 ± 4.43 | 110.35 ± 9.52 | 0.586 ± 0.241 |
| Novice | 1.91 ± 0.43 | 1.92 ± 0.45 | 11.67 ± 4.36 | 110.84 ± 9.46 | 0.568 ± 0.254 |
| % Mean Difference | 1.47 | 2.47 | 3.84 | 0.44 | 3.10 |
| Biceps Brachii | |||||
| Experienced | 2.70 ± 0.77 | 2.54 ± 0.84 | 9.82 ± 5.78 | 122.20 ± 10.43 | 0.386 ± 0.173 |
| Novice | 2.50 ± 0.64 | 2.55 ± 0.75 | 8.44 ± 3.94 | 122.25 ± 10.84 | 0.399 ± 0.210 |
| % Mean Difference | 7.55 | 0.20 | 14.11 | 0.04 | 3.45 |
| Transverse Thickness (cm) | Sagittal Thickness (cm) | CSA (cm2) | EI (A.U.) | Subcutaneous Thickness (cm) | |
|---|---|---|---|---|---|
| Vastus Lateralis | |||||
| p | 0.087 | 0.07 | 0.005 * | 0.827 | 0.222 |
| d | 0.303 | 0.321 | 0.514 | 0.038 | 0.214 |
| 95% CI | −0.312 to 0.022 | −0.342 to 0.014 | 1.090 to 5.709 | −0.807 to 0.650 | −0.049 to 0.202 |
| Limits of Agreement | −1.084 to 0.794 | −1.165 to 0.837 | −9.572 to 16.371 | −4.171 to 4.014 | −0.626 to 0.780 |
| Upper–Lower Limit | |||||
| ICC2,1 | 0.527 | 0.489 | 0.648 | 0.983 | 0.801 |
| SEM (raw units) | 0.34 | 0.36 | 4.68 | 1.48 | 0.25 |
| SEM (%) | 13.5 | 14.4 | 18.6 | 2.4 | 21.9 |
| MD | 0.94 | 1.00 | 12.97 | 4.09 | 0.7 |
| Medial Gastrocnemius | |||||
| p | 0.313 | 0.178 | 0.093 | 0.307 | 0.158 |
| d | 0.176 | 0.236 | 0.296 | 0.178 | 0.248 |
| 95% CI | −0.083 to 0.027 | −0.115 to 0.022 | −0.082 to 1.015 | −1.452 to 0.471 | −0.007 to 0.044 |
| Limits of Agreement | −0.337 to 0.281 | −0.430 to 0.338 | −2.615 to 3.547 | −5.890 to 4.910 | −0.125 to 0.162 |
| Upper–Lower Limit | |||||
| ICC2,1 | 0.927 | 0.887 | 0.933 | 0.958 | 0.955 |
| SEM (raw units) | 0.11 | 0.14 | 1.11 | 1.95 | 0.05 |
| SEM (%) | 5.9 | 7.3 | 9.3 | 1.8 | 9.0 |
| MD | 0.31 | 0.38 | 3.08 | 5.4 | 0.14 |
| Biceps Brachii | |||||
| p | 0.029 * | 0.952 | 0.052 | 0.953 | 0.486 |
| d | 0.393 | 0.01 | 0.346 | 0.01 | 0.121 |
| 95% CI | 0.023 to 0.385 | −0.175 to 0.165 | −0.012 to 2.783 | −1.675 to 1.579 | −0.052 to 0.025 |
| Limits of Agreement | −0.815 to 1.223 | −0.960 to 0.950 | −6.465 to 9.236 | −9.190 to 9.094 | −0.229 to 0.202 |
| Upper–Lower Limit | |||||
| ICC2,1 | 0.709 | 0.818 | 0.653 | 0.906 | 0.839 |
| SEM (raw units) | 0.37 | 0.35 | 2.83 | 3.3 | 0.08 |
| SEM (%) | 14.1 | 13.5 | 31 | 2.7 | 19.8 |
| MD | 1.02 | 0.96 | 7.85 | 9.14 | 0.22 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carr, J.C.; Gerstner, G.R.; Voskuil, C.C.; Harden, J.E.; Dunnick, D.; Badillo, K.M.; Pagan, J.I.; Harmon, K.K.; Girts, R.M.; Beausejour, J.P.; et al. The Influence of Sonographer Experience on Skeletal Muscle Image Acquisition and Analysis. J. Funct. Morphol. Kinesiol. 2021, 6, 91. https://doi.org/10.3390/jfmk6040091
Carr JC, Gerstner GR, Voskuil CC, Harden JE, Dunnick D, Badillo KM, Pagan JI, Harmon KK, Girts RM, Beausejour JP, et al. The Influence of Sonographer Experience on Skeletal Muscle Image Acquisition and Analysis. Journal of Functional Morphology and Kinesiology. 2021; 6(4):91. https://doi.org/10.3390/jfmk6040091
Chicago/Turabian StyleCarr, Joshua C., Gena R. Gerstner, Caleb C. Voskuil, Joel E. Harden, Dustin Dunnick, Kristin M. Badillo, Jason I. Pagan, Kylie K. Harmon, Ryan M. Girts, Jonathan P. Beausejour, and et al. 2021. "The Influence of Sonographer Experience on Skeletal Muscle Image Acquisition and Analysis" Journal of Functional Morphology and Kinesiology 6, no. 4: 91. https://doi.org/10.3390/jfmk6040091
APA StyleCarr, J. C., Gerstner, G. R., Voskuil, C. C., Harden, J. E., Dunnick, D., Badillo, K. M., Pagan, J. I., Harmon, K. K., Girts, R. M., Beausejour, J. P., & Stock, M. S. (2021). The Influence of Sonographer Experience on Skeletal Muscle Image Acquisition and Analysis. Journal of Functional Morphology and Kinesiology, 6(4), 91. https://doi.org/10.3390/jfmk6040091







