Pattern of the Heart Rate Performance Curve in Subjects with Beta-Blocker Treatment and Healthy Controls
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Assessment of Heart Rate and Performance Data
2.3. Statistical Analysis
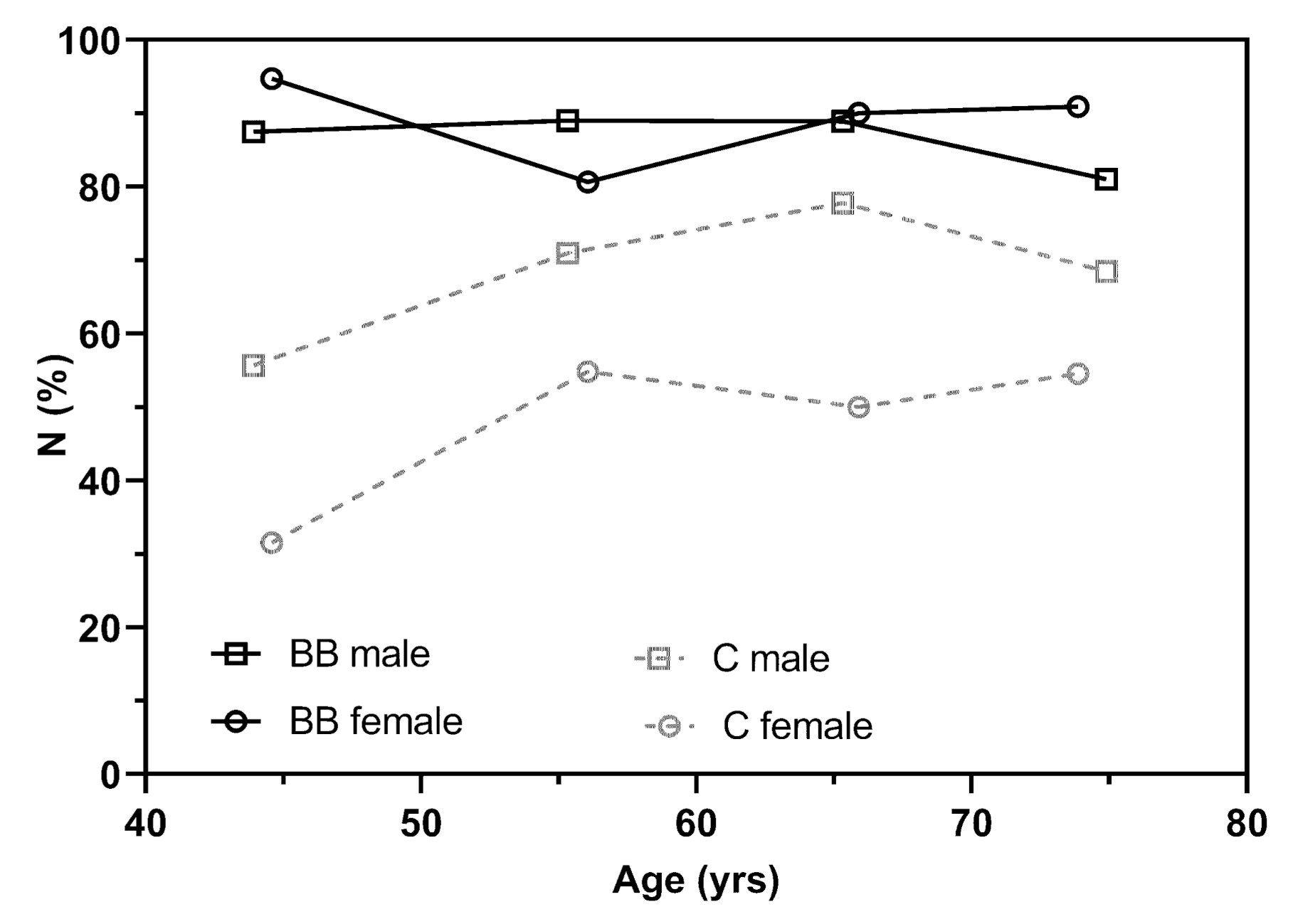
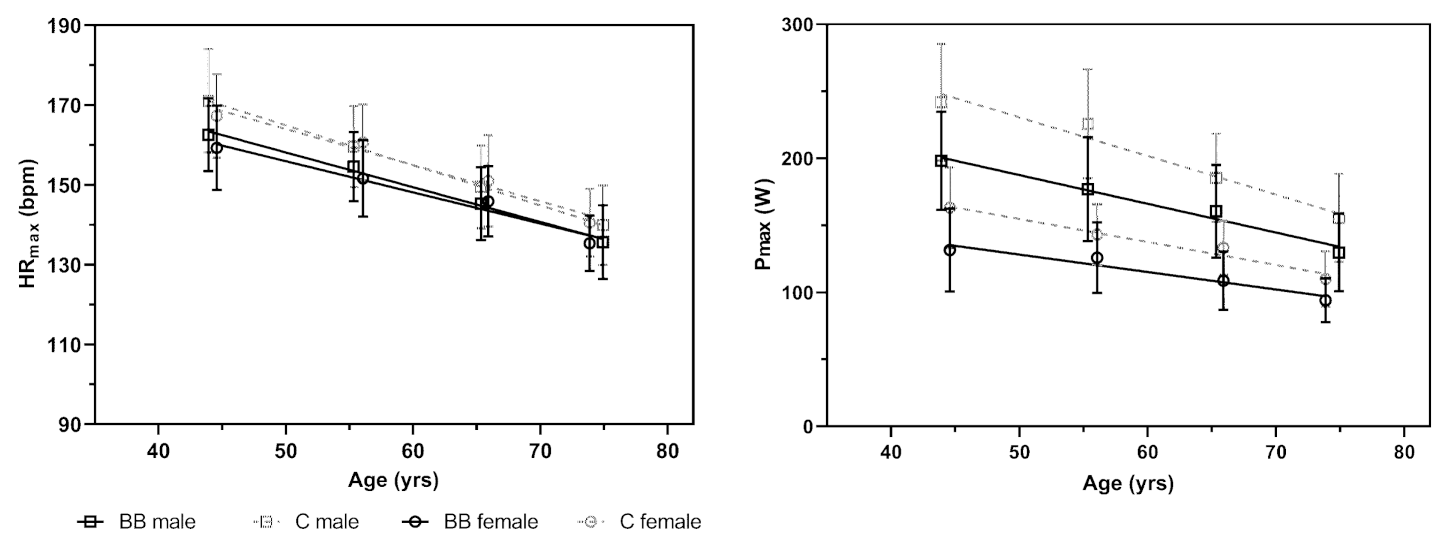
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| B (SE) | OR (95% CI) | p | |
|---|---|---|---|
| β-blocker | 1.015 (0.221) | 2.761 (1.788, 4.261) | <0.001 |
| Age | 0.022 (0.009) | 1.022 (1.005, 1.040) | 0.01 |
| Age2 | −0.002 (0.001) | 0.998 (0.997, 0.999) | 0.001 |
| Female | −0.914 (0.228) | 0.401 (0.256, 0.628) | <0.001 |
| Female × β-blocker | 1.019 (0.410) | 2.771 (1.239, 6.194) | 0.013 |
| Age × β-blocker | −0.34 (0.014) | 0.966 (0.940, 0.993) | 0.015 |
| Age2 × β-blocker | 0.001 (0.001) | 1.001 (0.999, 1.003) | 0.331 |
| Model | B (95% CI) | p |
|---|---|---|
| Constant | 156.070 (155.206, 156.933) | <0.001 |
| β-blocker | −5.457 (−6.678, −4.236) | <0.001 |
| Age | −1.017 (−1.088, −0.945) | <0.001 |
| Female | 0.448 (−1.533, 2.429) | 0.657 |
| Female × β-blocker | −1.690 (−4.492, 1.111) | 0.237 |
| Age × β-blocker | 0.165 (0.064, 0.266) | 0.001 |
| B (95% CI) | p | |
|---|---|---|
| Constant | 206.659 (203.407, 209.912) | <0.001 |
| β-blocker | −37.528 (−42.128, −32.929) | <0.001 |
| Age | −2.717 (−2.988, −2.447) | <0.001 |
| Female | −64.954 (−72.416, −57.493) | <0.001 |
| Female × β-blocker | 14.189 (3.637, 24.742) | 0.008 |
| Age × β-blocker | 0.829 (0.447, 1.210) | <0.001 |
References
- Lavie, C.J.; Thomas, R.J.; Squires, R.W.; Allison, T.G.; Milani, R.V. Exercise Training and Cardiac Rehabilitation in Primary and Secondary Prevention of Coronary Heart Disease. Mayo Clin. Proc. 2009, 84, 373–383. [Google Scholar] [CrossRef] [Green Version]
- Iannetta, D.; Inglis, E.C.; Mattu, A.T.; Fontana, F.Y.; Pogliaghi, S.; Keir, D.A.; Murias, J.M. A Critical Evaluation of Current Methods for Exercise Prescription in Women and Men. Med. Sci. Sports Exerc. 2019, 1, 466–473. [Google Scholar] [CrossRef]
- Hansen, D.; Bonné, K.; Alders, T.; Hermans, A.; Copermans, K.; Swinnen, H.; Maris, V.; Jansegers, T.; Mathijs, W.; Haenen, L.; et al. Exercise Training Intensity Determination in Cardiovascular Rehabilitation: Should the Guidelines Be Reconsidered? Eur. J. Prev. Cardiol. 2019, 26, 1921–1928. [Google Scholar] [CrossRef] [PubMed]
- Scharhag-Rosenberger, F.; Meyer, T.; Gässler, N.; Faude, O.; Kindermann, W. Exercise at given Percentages of VO2max: Heterogeneous Metabolic Responses between Individuals. J. Sci. Med. Sport 2010, 13, 74–79. [Google Scholar] [CrossRef]
- Ambrosetti, M.; Abreu, A.; Corrà, U.; Davos, C.H.; Hansen, D.; Frederix, I.; Iliou, M.C.; Pedretti, R.F.; Schmid, J.-P.; Vigorito, C.; et al. Secondary Prevention through Comprehensive Cardiovascular Rehabilitation: From Knowledge to Implementation. 2020 Update. A Position Paper from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology. Eur. J. Prev. Cardiol. 2020, 28, 460–495. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- ACSM. ACSM’s Guidelines for Exercise Testing and Prescription, 10th ed.; Lippincot Williams & Wilkins: Philadelphia, PA, USA, 2016. [Google Scholar]
- Li, W.G.; Huang, Z.; Zhang, X.A. Exercise Prescription in Cardiac Rehabilitation Needs to Be More Accurate. Eur. J. Prev. Cardiol. 2020, 30, 2047487320936021. [Google Scholar]
- Hofmann, P.; Tschakert, G. Special Needs to Prescribe Exercise Intensity for Scientific Studies. Cardiol. Res. Pract. 2010, 2011, 209302. [Google Scholar] [CrossRef] [Green Version]
- Hofmann, P.; Pokan, R.; von Duvillard, S.P.; Seibert, F.J.; Zweiker, R.; Schmid, P. Heart Rate Performance Curve during Incremental Cycle Ergometer Exercise in Healthy Young Male Subjects. Med. Sci. Sports Exerc. 1997, 29, 762–768. [Google Scholar] [CrossRef]
- Brooke, J.D.; Hamley, E.J. The Heart-Rate--Physical Work Curve Analysis for the Prediction of Exhausting Work Ability. Med. Sci. Sports 1972, 4, 23–26. [Google Scholar]
- Pokan, R.; Hofmann, P.; Preidler, K.; Leitner, H.; Dusleag, J.; Eber, B.; Schwaberger, G.; Füger, G.F.; Klein, W. Correlation between Inflection of Heart Rate/Work Performance Curve and Myocardial Function in Exhausting Cycle Ergometer Exercise. Eur. J. Appl. Physiol. Occup. Physiol. 1993, 67, 385–388. [Google Scholar] [CrossRef] [PubMed]
- Birnbaumer, P.; Traninger, H.; Borenich, A.; Falgenhauer, M.; Modre-Osprian, R.; Harpf, H.; Hofmann, P. Heart Rate Performance Curve Is Dependent on Age, Sex, and Performance. Front. Public Health 2020, 8, 98. [Google Scholar] [CrossRef] [PubMed]
- Conconi, F.; Ferrari, M.; Ziglio, P.G.; Droghetti, P.; Codeca, L. Determination of the Anaerobic Threshold by a Noninvasive Field Test in Runners. J. Appl. Physiol. 1982, 52, 869–873. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bodner, M.E.; Rhodes, E.C. A Review of the Concept of the Heart Rate Deflection Point. Sports Med. 2000, 30, 31–46. [Google Scholar] [CrossRef]
- Binder, R.K.; Wonisch, M.; Corra, U.; Cohen-Solal, A.; Vanhees, L.; Saner, H.; Schmid, J.-P. Methodological Approach to the First and Second Lactate Threshold in Incremental Cardiopulmonary Exercise Testing. Eur. J. Cardiovasc. Prev. Rehabil. 2008, 15, 726–734. [Google Scholar] [CrossRef]
- Zouhal, H.; Jacob, C.; Delamarche, P.; Gratas-Delamarche, A. Catecholamines and the Effects of Exercise, Training and Gender. Sports Med. Sports Med. 2008, 38, 401–423. [Google Scholar] [CrossRef] [PubMed]
- Pokan, R.; Hofmann, P.; Lehmann, M.; Leitner, H.; Eber, B.; Gasser, R.; Schwaberger, G.; Schmid, P.; Keul, J.; Klein, W. Heart Rate Deflection Related to Lactate Performance Curve and Plasma Catecholamine Response during Incremental Cycle Ergometer Exercise. Eur. J. Appl. Physiol. Occup. Physiol. 1995, 70, 175–179. [Google Scholar] [CrossRef]
- Hofmann, P.; Wonisch, M.; Pokan, R.; Schwaberger, G.; Smekal, G.; von Duvillard, S. Beta1-Adrenoceptor Mediated Origin of the Heart Rate Performance Curve Deflection. Med. Sci. Sports Exerc. 2005, 37, 1704–1709. [Google Scholar] [CrossRef]
- Brodde, O.E.; Bruck, H.; Leineweber, K. Cardiac Adrenoceptors: Physiological and Pathophysiological Relevance. J. Pharmacol. Sci. 2006, 100, 323–337. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chwalbińska-Moneta, J. Threshold Increases in Plasma Growth Hormone in Relation to Plasma Catecholamine and Blood Lactate Concentrations during Progressive Exercise in Endurance-Trained Athletes. Eur. J. Appl. Physiol. Occup. Physiol. 1996, 73, 117–120. [Google Scholar] [CrossRef]
- Christou, D.D.; Seals, D.R. Decreased Maximal Heart Rate with Aging Is Related to Reduced β-Adrenergic Responsiveness but Is Largely Explained by a Reduction in Intrinsic Heart Rate. J. Appl. Physiol. 2008, 105, 24–29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stratton, J.R.; Cerqueira, M.D.; Schwartz, R.S.; Levy, W.C.; Veith, R.C.; Kahn, S.E.; Abrass, I.B. Differences in Cardiovascular Responses to Isoproterenol in Relation to Age and Exercise Training in Healthy Men. Circulation 1992, 86, 504–512. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fleg, J.L.; Schulman, S.; O’Connor, F.; Becker, L.C.; Gerstenblith, G.; Clulow, J.F.; Renlund, D.G.; Lakatta, E.G. Effects of Acute Beta-Adrenergic Receptor Blockade on Age-Associated Changes in Cardiovascular Performance during Dynamic Exercise. Circulation 1994, 90, 2333–2341. [Google Scholar] [CrossRef] [Green Version]
- Zeitouni, M.; Kerneis, M.; Lattuca, B.; Guedeney, P.; Cayla, G.; Collet, J.P.; Montalescot, G.; Silvain, J. Do Patients Need Lifelong β-Blockers after an Uncomplicated Myocardial Infarction? Am. J. Cardiovasc. Drugs 2019, 19, 431–438. [Google Scholar] [CrossRef]
- Ladage, D.; Schwinger, R.H.G.; Brixius, K. Cardio-Selective Beta-Blocker: Pharmacological Evidence and Their Influence on Exercise Capacity. Cardiovasc. Ther. 2013, 31, 76–83. [Google Scholar] [CrossRef] [Green Version]
- Wonisch, M.; Hofmann, P.; Fruhwald, F.; Kraxner, W.; Hödl, R.; Pokan, R.; Klein, W. Influence of beta-blocker use on percentage of target heart rate exercise prescription. Eur. J. Cardiovasc. Prev. Rehabil. 2003, 10, 296–301. [Google Scholar] [CrossRef]
- Díaz-Buschmann, I.; Jaureguizar, K.V.; Calero, M.J.; Aquino, R.S. Programming Exercise Intensity in Patients on Beta-Blocker Treatment: The Importance of Choosing an Appropriate Method. Eur. J. Prev. Cardiol. 2014, 21, 1474–1480. [Google Scholar] [CrossRef]
- Sauer, G. β-Blocker in Der Sekundärprävention von Herz-Kreislauf-Erkrankungen. Z. Kardiol. 2003, 92, 24–30. [Google Scholar] [CrossRef]
- Hofmann, P.; Von Duvillard, S.P.; Seibert, F.J.; Pokan, R.; Wonisch, M.; Lemura, L.M.; Schwaberger, G. %HRmax Target Heart Rate Is Dependent on Heart Rate Performance Curve Deflection. Med. Sci. Sports Exerc. 2001, 33, 1726–1731. [Google Scholar] [CrossRef] [PubMed]
- Turner, M.J.; Mier, C.M.; Spina, R.J.; Schechtman, K.B.; Ehsani, A.A. Effects of Age and Gender on the Cardiovascular Responses to Isoproterenol. J. Gerontol. A Biol. Sci. Med. Sci. 1999, 54, 393–400. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mitchell, B.L.; Kade, D.; Gaynor, P.; Simon, S.; Roger, G.E. Physiological and Perceived Exertion Responses during Exercise: Effect of β-Blockade. Med. Sci. Sports Exerc. 2019, 51, 782–791. [Google Scholar] [CrossRef]
- Brawner, C.A.; Ehrman, J.K.; Schairer, J.R.; Cao, J.J.; Keteyian, S.J. Predicting Maximum Heart Rate among Patients with Coronary Heart Disease Receiving Beta-Adrenergic Blockade Therapy. Am. Heart J. 2004, 148, 910–914. [Google Scholar] [CrossRef]
- Zhu, N.; Suarez-Lopez, J.R.; Sidney, S.; Sternfeld, B.; Schreiner, P.J.; Carnethon, M.R.; Lewis, C.E.; Crow, R.S.; Bouchard, C.; Haskell, W.L.; et al. Longitudinal Examination of Age-Predicted Symptom-Limited Exercise Maximum HR. Med. Sci. Sports Exerc. 2010, 42, 1519–1527. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Higa, M.N.; Silva, E.; Neves, V.F.C.; Catai, A.M.; Gallo, L.; Silva de Sá, M.F. Comparison of Anaerobic Threshold Determined by Visual and Mathematical Methods in Healthy Women. Braz. J. Med. Biol. Res. 2007, 40, 501–508. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zamunér, A.R.; Catai, A.M.; Martins, L.E.B.; Sakabe, D.I.; Da Silva, E. Identification and Agreement of First Turn Point by Mathematical Analysis Applied to Heart Rate, Carbon Dioxide Output and Electromyography. Braz. J. Phys. Ther. 2013, 17, 614–622. [Google Scholar] [CrossRef] [Green Version]
- Pokan, R.; Hofmann, P.; Von Duvillard, S.P.; Schumacher, M.; Gasser, R.; Zweiker, R.; Fruhwald, F.M.; Eber, B.; Smekal, G.; Bachl, N.; et al. Parasympathetic Receptor Blockade and the Heart Rate Performance Curve. Med. Sci. Sports Exerc. 1998, 30, 229–233. [Google Scholar] [CrossRef]

| MALES | FEMALES | |||||||
|---|---|---|---|---|---|---|---|---|
| Variables | C n = 433 | BB n = 433 | p | d/r | C n = 102 | BB n = 102 | p | d/r |
| Age (yrs) | 59.0 ±10.9 | 59.0 ±10.9 | 1.0 a | 0.00 | 60.7 ±10.7 | 60.7 ±10.7 | 1.0 a | 0.00 |
| BMI (kg/m2) | 26.2 (4.0; 20.8) | 26.8 (4.8; 25.1) | 0.003 b | 0.10 | 24.6 (5.3; 18.8) | 25.7 (5.6; 26.9) | 0.116 b | 0.11 |
| BM (kg) | 83 (15; 117) | 84 (18; 92) | 0.121 b | 0.05 | 65 (12; 54) | 69 (17; 83) | 0.05 b | 0.14 |
| Pmax (W) | 200 (60; 280) | 170 (60; 210) | <0.001 b | 0.37 | 140 (40; 160) | 110 (40; 130) | <0.001 b | 0.37 |
| HRmax (bpm) | 155 (20; 80) | 150 (18; 67) | <0.001 b | 0.18 | 154.7 ±13.8 | 148 (16; 61) | <0.001 b | 0.27 |
| P (W) | ||||||||
| Th1 | 76.4 (21.8; 105.5) | 64.5 (19.1; 79.1) | <0.001 b | 0.33 | 50.9 (12.7; 56.4) | 46.4 (12.7; 47.3) | <0.001 b | 0.29 |
| Th2 | 145.5 (41.8; 210.9) | 119.1 ±30.0 | <0.001 b | 0.35 | 96.9 ±20.3 | 77.7 (28.4; 95.5) | <0.001 b | 0.40 |
| HR (bpm) | ||||||||
| Th1 | 98.1 (15.2; 61.9) | 93.4 (14.7; 67.7) | <0.001 b | 0.24 | 106.4 ±10.9 | 97.6 (12.6; 55.3) | <0.001 b | 0.37 |
| Th2 | 124.1 (19.3; 78.1) | 115.1 (14.6; 77.0) | <0.001 b | 0.33 | 129.9 ±14.1 | 116.9 ±10.2 | <0.001 a | 0.93 |
| P as % Pmax | ||||||||
| Th1 | 37.3 (5.0; 9.9) | 39.5 (4.2; 14.2) | <0.001 b | 0.30 | 39.4 (3.9; 8.3) | 42.1 ±2.8 | <0.001 b | 0.47 |
| Th2 | 69.31 (5.1; 7.6) | 71.7 (5.1; 7.1) | 0.009 b | 0.9 | 72.7 (4.5; 8.3) | 68.2 (5.2; 7.1) | 0.006 b | 0.19 * |
| HR as % HRmax | ||||||||
| Th1 | 63.4 (8.5; 37.6) | 62.1 (9.2; 41.5) | 0.001 b | 0.11 | 68.9 ±5.0 | 66.8 ±7.0 | 0.016 a | 0.34 |
| Th2 | 80.8 ±5.0 | 77.2 ±7.3 | <0.001 b | 0.55 | 84.2 (6.5; 19.7) | 79.2 ±5.1 | <0.001 b | 0.45 |
| kHR | −0.4 (1.3; 10.8) | −1.2 (1.32; 10.3) | <0.001 b | 0.36 | 0.1 ±1.0 | −1.0 ±1.0 | <0.001 a | −1.00 |
| MALES n = 433 | ≤50 yrs | 51–60 yrs | 61–70 yrs | >70 yrs | |
| n | 176 | 155 | 117 | 73 | |
| P Th1 (W) | C | 87.8 ± 15.6 | 83.1 ± 15.0 | 69.9 ± 11.1 | 60.7 ± 11.9 |
| BB | 75.21 ± 14.0 * | 68.5 ± 13.7 * | 62.5 ± 11.4 * | 52.3 ± 9.3 * | |
| P Th2 (W) | C | 169.7 ± 31.6 | 158.0 ± 30.2 | 129.2 ± 22.8 | 109.7 ± 22.5 |
| BB | 139.9 ± 26.9 * | 125.0 ±2 7.4 * | 113.3 ± 25.1 * | 90.7 ± 20.2 * | |
| %Pmax Th1 (%) | C | 36.4 ± 2.5 | 36.9 ± 2.4 | 37.9 ± 2.5 | 39.2 ± 2.3 |
| BB | 38.0 ± 2.4 | 39.0 ± 2.9 | 39.3 ± 2.9 | 40.9 ± 3.2 | |
| %Pmax Th2 (%) | C | 70.2 ± 2.6 | 69.9 ± 2.5 | 69.7 ± 2.5 | 70.7 ± 2.5 |
| BB | 70.5 ± 2.5 | 70.7 ± 2.5 * | 70.6 ± 2.6 * | 70.0 ± 2.5 | |
| HR Th1 (bpm) | C | 106.5 ± 11.2 | 100.2 ± 11.1 | 96.3 ± 10.6 | 94.2 ± 11.3 |
| BB | 99.0 ± 11.4 | 94.8 ± 10.5 | 90.3 ± 9.3 | 90.7 ± 10.2 | |
| HR Th2 (bpm) | C | 139.1 ± 13.8 | 128.6 ± 11.4 | 119.4 ± 10.2 | 114.6 ± 10.0 |
| BB | 126.1 ± 11.2 * | 118.9 ± 8.9 * | 111.6 ± 8.8 * | 107.7 ± 9.6 * | |
| %HRmax Th1 (%) | C | 62.3 ± 5.4 | 62.8 ± 6.2 | 64.5 ± 6.9 | 67.5 ± 7.8 |
| BB | 60.9 ± 6.2 | 61.4 ± 6.6 | 61.2 ± 10.2 | 67 ± 7.4 | |
| %HRmax Th2 (%) | C | 81.3 ± 4.8 | 80.5 ± 4.6 | 79.9 ± 5.3 | 82.0 ± 5.4 |
| BB | 77.6 ± 5.2 | 77.0 ± 5.0 | 75.7 ± 11.1 | 79.5 ± 7.4 | |
| kHR | C | −0.1 ± 1.1 | −0.3 ± 1.0 | −0.5 ± 1.2 | −0.3 ± 1.4 |
| BB | −1.0 ± 1.0 | −1.1 ± 1.1 | −1.2 ± 1.0 | −0.9 ± 1.5 | |
| FEMALES n= 102 | ≤50 yrs | 51–60 yrs | 61–70 yrs | >70 yrs | |
| n | 19 | 31 | 30 | 22 | |
| P Th1 (W) | C | 62.6 ± 9.6 | 56.1 ± 9.4 | 52.7 ± 7.2 | 44.7 ± 8.7 |
| BB | 53.3 ± 11.4 | 51.3 ± 8.9 | 45.7 ± 7.8 | 41.5 ± 6.2 | |
| P Th2 (W) | C | 115.5 ± 19.5 | 101.0 ± 16.2 | 94.7 ± 14.3 | 78.1 ± 15.9 |
| BB | 90.8 ± 20.6 | 89.0 ± 19.4 | 75.4 ± 15.3 | 65.7 ± 11.3 | |
| %Pmax Th1 (%) | C | 38.6 ± 2.3 | 39.2 ± 2.1 | 39.7 ± 2.2 | 40.6 ± 1.2 |
| BB | 40.9 ± 2.8 | 41.1 ± 2.6 | 42.3 ± 2.3 | 44.4 ± 2.0 | |
| %Pmax Th2 (%) | C | 71.0 ± 2.5 | 70.5 ± 2.4 | 71.0 ± 2.3 | 70.8 ± 2.3 |
| BB | 69.1 ± 2.3 | 70.7 ± 2.6 | 69.4 ± 2.4 | 69.9 ± 2.4 | |
| HR Th1 (bpm) | C | 112.8 ± 11.2 | 109.6 ± 10.4 | 103.5 ± 9.9 | 100.1 ± 7.4 |
| BB | 101.2 ± 10.2 | 101.5 ± 13.5 | 94.7 ± 6.9 | 96.7 ± 8.2 | |
| HR Th2 (bpm) | C | 142.0 ± 13.5 | 134.1 ± 11.9 | 126.4 ± 11.1 | 118.1 ± 9.2 |
| BB | 123.7 ±8.1 | 121.3 ± 10.6 | 113.1 ± 7.2 | 110.2 ± 8.3 | |
| %HRmax Th1 (%) | C | 67.5 ± 5.2 | 68.2 ± 4.7 | 68.6 ± 5.1 | 71.3 ± 4.5 |
| BB | 67.5 ± 5.2 | 68.2 ± 4.7 | 68.6 ± 5.1 | 71.3 ± 4.5 | |
| %HRmax Th2 (%) | C | 84.8 ± 4.4 | 83.4 ± 4.1 | 83.8 ± 4.4 | 84.0 ± 4.4 |
| BB | 77.9 ± 6.5 | 80.0 ± 4.5 | 77.6 ± 4.3 | 81.4 ± 4.5 | |
| kHR | C | 0.41 ± 1.12 | −0.07 ± 0.86 | 0.12 ± 1.06 | 0.05 ± 1.07 |
| BB | −0.98 ± 0.90 | −1.06 ± 0.98 | −1.05 ± 0.99 | −1.02 ± 0.97 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Birnbaumer, P.; Traninger, H.; Sattler, M.C.; Borenich, A.; Hofmann, P. Pattern of the Heart Rate Performance Curve in Subjects with Beta-Blocker Treatment and Healthy Controls. J. Funct. Morphol. Kinesiol. 2021, 6, 61. https://doi.org/10.3390/jfmk6030061
Birnbaumer P, Traninger H, Sattler MC, Borenich A, Hofmann P. Pattern of the Heart Rate Performance Curve in Subjects with Beta-Blocker Treatment and Healthy Controls. Journal of Functional Morphology and Kinesiology. 2021; 6(3):61. https://doi.org/10.3390/jfmk6030061
Chicago/Turabian StyleBirnbaumer, Philipp, Heimo Traninger, Matteo C. Sattler, Andrea Borenich, and Peter Hofmann. 2021. "Pattern of the Heart Rate Performance Curve in Subjects with Beta-Blocker Treatment and Healthy Controls" Journal of Functional Morphology and Kinesiology 6, no. 3: 61. https://doi.org/10.3390/jfmk6030061
APA StyleBirnbaumer, P., Traninger, H., Sattler, M. C., Borenich, A., & Hofmann, P. (2021). Pattern of the Heart Rate Performance Curve in Subjects with Beta-Blocker Treatment and Healthy Controls. Journal of Functional Morphology and Kinesiology, 6(3), 61. https://doi.org/10.3390/jfmk6030061







