Predicting Adaptations to Resistance Training Plus Overfeeding Using Bayesian Regression: A Preliminary Investigation
Abstract
1. Introduction
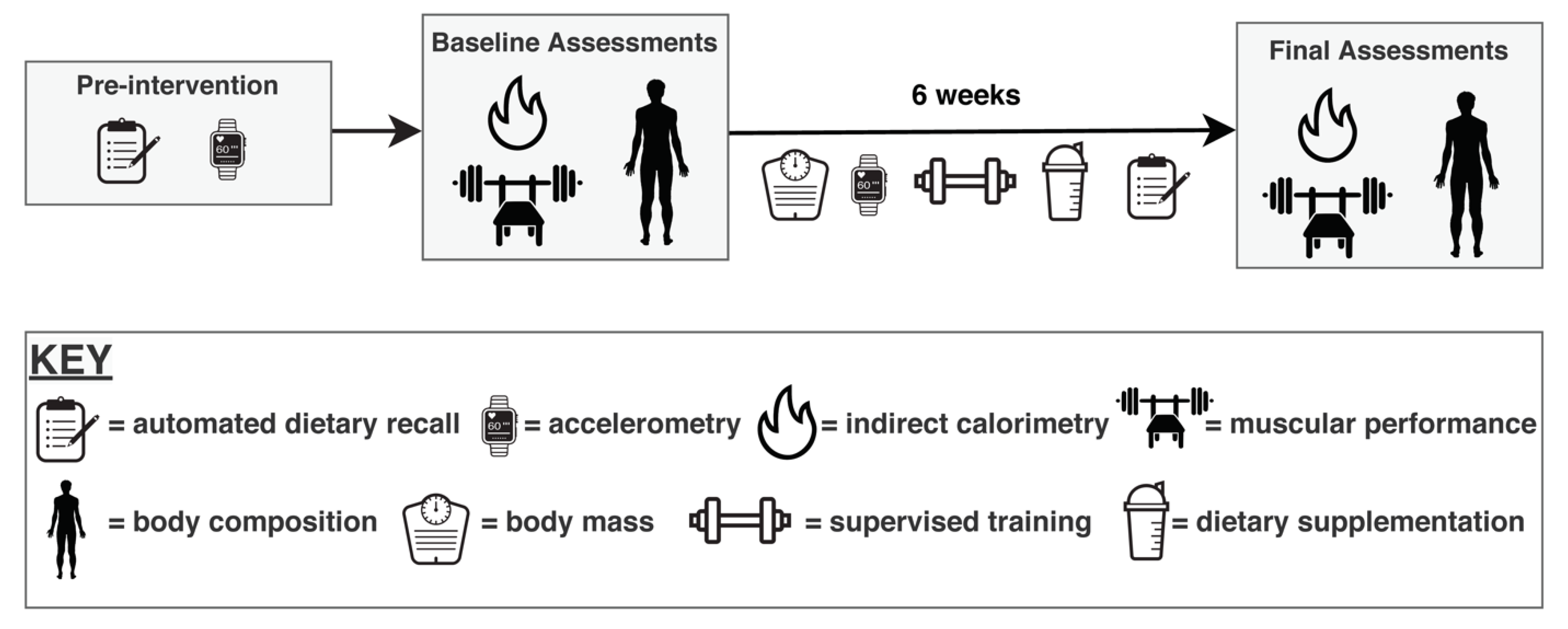
2. Materials and Methods
2.1. Participants and Study Design
2.2. Intervention
2.2.1. Dietary Program
2.2.2. Resistance Training Program
2.3. Muscular Performance Assessments
2.4. Laboratory Assessments
2.4.1. Initial Procedures
2.4.2. 4-Component Model Body Composition Analysis
2.4.3. Ultrasound Assessment
2.4.4. Indirect Calorimetry
2.5. Nutrition Intake and Physical Activity Monitoring
2.5.1. Nutritional Intake
2.5.2. Accelerometry
2.6. Statistical Analysis
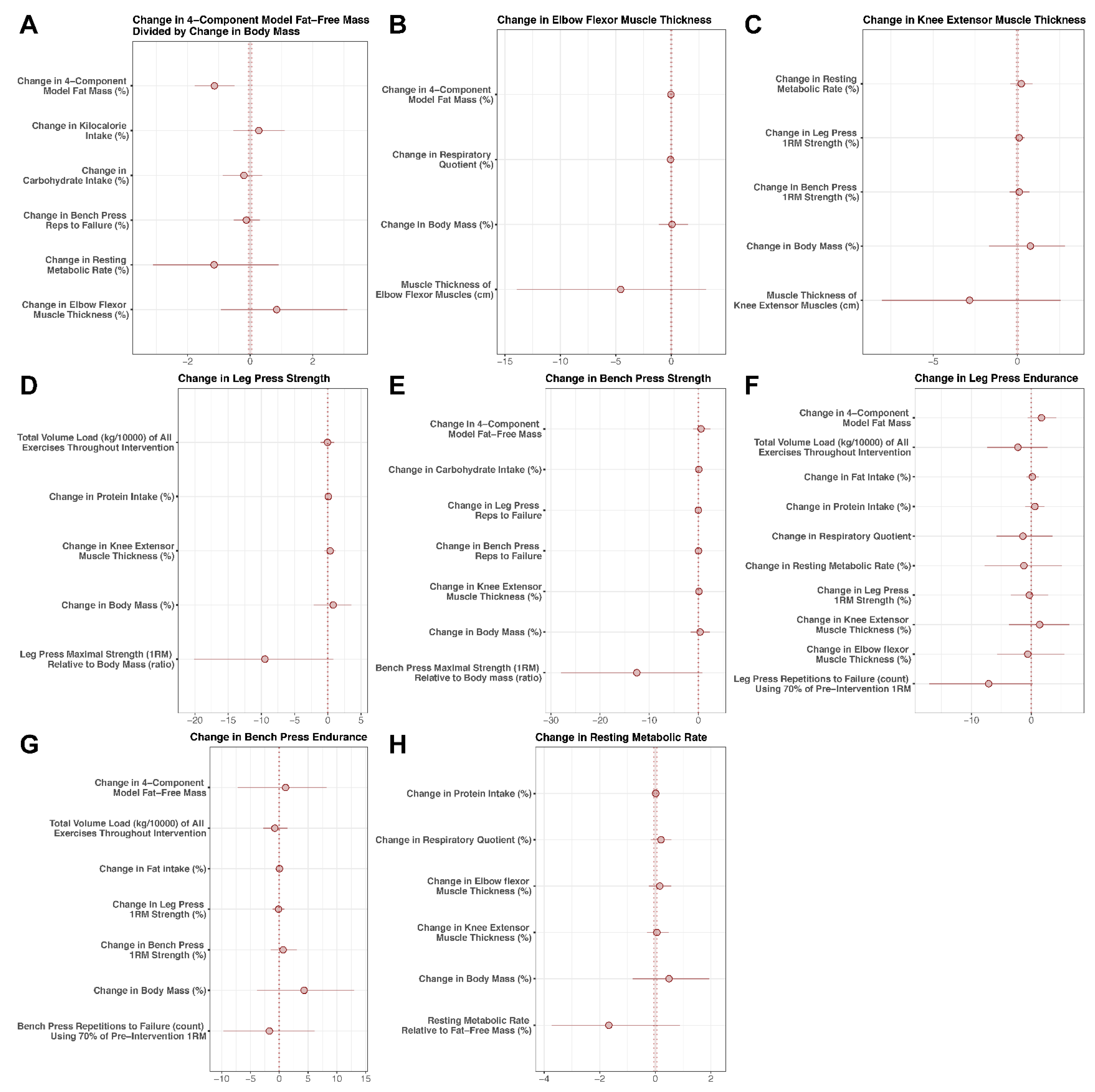
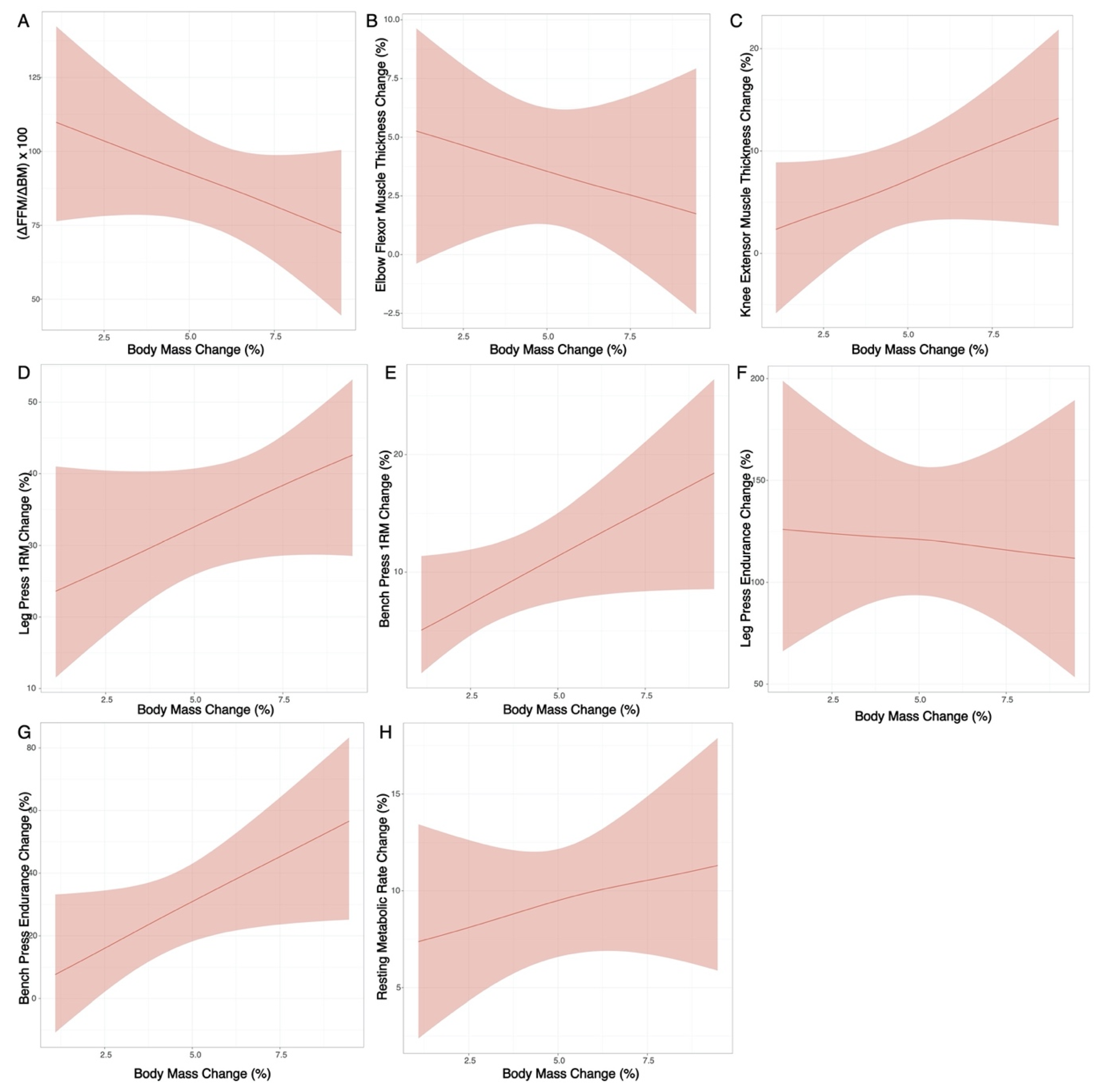
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Forbes, G.B.; Brown, M.R.; Welle, S.L.; Lipinski, B.A. Deliberate Overfeeding in Women and Men: Energy Cost and Composi-tion of the Weight Gain. Br. J. Nutr. 1986, 56, 1–9. [Google Scholar] [CrossRef]
- Campbell, B.I.; Aguilar, D.; Conlin, L.; Vargas, A.; Schoenfeld, B.J.; Corson, A.; Gai, C.; Best, S.; Galvan, E.; Couvillion, K. Effects of High Versus Low Protein Intake on Body Composition and Maximal Strength in Aspiring Female Physique Athletes Engaging in an 8-Week Resistance Training Program. Int. J. Sport Nutr. Exerc. Metab. 2018, 28, 580–585. [Google Scholar] [CrossRef] [PubMed]
- Leaf, A.; Antonio, J. The Effects of Overfeeding on Body Composition: The Role of Macronutrient Composition–a Narrative Re-view. Int. J. Exerc. Sci. 2017, 10, 1275. [Google Scholar] [PubMed]
- Rozenek, R.; Ward, P.; Long, S.; Garhammer, J. Effects of High-Calorie Supplements on Body Composition and Muscular Strength Following Resistance Training. J. Sports Med. Phys. Fit. 2002, 42, 340–347. [Google Scholar]
- Spillane, M.; Willoughby, D.S. Daily Overfeeding from Protein and/or Carbohydrate Supplementation for Eight Weeks in Conjunction with Resistance Training Does not Improve Body Composition and Muscle Strength or Increase Markers Indicative of Muscle Protein Synthesis and Myogenesis in Resistance-Trained Males. J. Sports Sci. Med. 2016, 15, 17–25. [Google Scholar] [PubMed]
- Garthe, I.; Raastad, T.; Refsnes, P.E.; Sundgot-Borgen, J. Effect of Nutritional Intervention on Body Composition and Perfor-mance in Elite Athletes. Eur. J. Sport Sci. 2013, 13, 295–303. [Google Scholar] [CrossRef] [PubMed]
- Antonio, J.; Peacock, A.C.; Ellerbroek, A.; Fromhoff, B.; Silver, T. The Effects of Consuming a High Protein Diet (4.4 g/kg/d) on Body Composition in Resistance-Trained Individuals. J. Int. Soc. Sports Nutr. 2014, 11, 19. [Google Scholar] [CrossRef]
- Antonio, J.; Ellerbroek, A.; Silver, T.; Orris, S.; Scheiner, M.; Gonzalez, A.; Peacock, A.C. A high protein diet (3.4 g/kg/d) Combined with a Heavy Resistance Training Program Improves Body Composition in Healthy Trained Men and Women-a Follow-Up Investigation. J. Int. Soc. Sports Nutr. 2015, 12, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Antonio, J.; Ellerbroek, A.; Silver, T.; Vargas, L.; Peacock, C. The Effects of a High Protein Diet on Indices of Health and Body Composition—A Crossover Trial in Resistance-Trained Men. J. Int. Soc. Sports Nutr. 2016, 13, 3. [Google Scholar] [CrossRef]
- Moon, J.R.; Eckerson, J.M.; Tobkin, S.E.; Smith, A.E.; Lockwood, C.M.; Walter, A.A.; Cramer, J.T.; Beck, T.W.; Stout, J.R. Estimating Body Fat in NCAA Division I Female Athletes: A Five-Compartment Model Validation of Laboratory Methods. Graefe’s Arch. Clin. Exp. Ophthalmol. 2009, 105, 119–130. [Google Scholar] [CrossRef]
- Toombs, R.J.; Ducher, G.; Shepherd, J.A.; De Souza, M.J. The Impact of Recent Technological Advances on the Trueness and Precision of DXA to Assess Body Composition. Obesity 2012, 20, 30–39. [Google Scholar] [CrossRef]
- Tinsley, G.M. Five-Component Model Validation of Reference, Laboratory and Field Methods of Body Composition Assessment. Br. J. Nutr. 2020, 10, 1–14. [Google Scholar] [CrossRef]
- Wang, Z.; Heshka, S.; Wang, J.; Wielopolski, L.; Heymsfield, S.B. Magnitude and Variation of Fat-Free Mass Density: A Cellular-Level Body Composition Modeling Study. Am. J. Physiol. Metab. 2003, 284, E267–E273. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wang, Z.; Deurenberg, P.; Wang, W.; Pietrobelli, A.; Baumgartner, R.N.; Heymsfield, S.B. Hydration of Fat-Free Body Mass: Review and Critique of a Classic Body-Composition Constant. Am. J. Clin. Nutr. 1999, 69, 833–841. [Google Scholar] [CrossRef] [PubMed]
- Graybeal, A.J.; Moore, M.L.; Cruz, M.R.; Tinsley, G.M. Body Composition Assessment in Male and Female Bodybuilders: A 4-Compartment Model Comparison of Dual-Energy X-Ray Absorptiometry and Impedance-Based Devices. J. Strength Cond. Res. 2020, 34, 1676–1689. [Google Scholar] [CrossRef] [PubMed]
- Tinsley, G.M.; Graybeal, A.J.; Moore, M.L.; Nickerson, B.S. Fat-free Mass Characteristics of Muscular Physique Athletes. Med. Sci. Sports Exerc. 2019, 51, 193–201. [Google Scholar] [CrossRef]
- Zourdos, M.C.; Klemp, A.; Dolan, C.; Quiles, J.M.; Schau, K.A.; Jo, E.; Helms, E.; Esgro, B.; Duncan, S.; Merino, S.G.; et al. Novel Resistance Training–Specific Rating of Perceived Exertion Scale Measuring Repetitions in Reserve. J. Strength Cond. Res. 2016, 30, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Haff, G.G.; Triplett, N.T. Essentials of Strength Training and Conditioning, 4th ed.; Human Kinetics: Champaign, IL, USA, 2015. [Google Scholar]
- Grgic, J.; Lazinica, B.; Schoenfeld, B.J.; Pedisic, Z. Test–Retest Reliability of the One-Repetition Maximum (1RM) Strength Assessment: A Systematic Review. Sports Med. Open 2020, 6, 1–16. [Google Scholar] [CrossRef]
- Nana, A.; Slater, G.J.; Hopkins, W.G.; Burke, L.M. Effects of Daily Activities on Dual-Energy X-Ray Absorptiometry Measure-ments of Body Composition in Active People. Med. Sci. Sports Exerc. 2012, 44, 180–189. [Google Scholar] [CrossRef]
- Wang, Z.; Deurenberg, P.; Guo, S.S.; Pietrobelli, A.; Wang, J.; Pierson Jr, R.; Heymsfield, S.B. Six-Compartment Body Compo-sition Model: Inter-Method Comparisons of Total Body Fat Measurement. Int. J. Obes. 1998, 22, 329–337. [Google Scholar] [CrossRef]
- Cole, K.S. Permeability and Impermeability of Cell Membranes for Ions. Cold Spring Harb. Symp. Quant. Biol. 1940, 8, 110–122. [Google Scholar] [CrossRef]
- Hanai, T. Electrical Properties of Emulsions in Emulsion Science; Sherman PH: New York, NY, USA, 1968. [Google Scholar]
- Kyle, U.G.; Bosaeus, I.; De Lorenzo, A.D.; Deurenberg, P.; Elia, M.; Gómez, J.M.; Heitmann, B.L.; Kent-Smith, L.; Melchior, J.-C.; Pirlich, M. Bioelectrical Impedance Analysis—Part I: Review of Principles and Methods. Clin. Nutr. 2004, 23, 1226–1243. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Pi-Sunyer, F.X.; Kotler, D.P.; Wielopolski, L.; Withers, R.T.; Pierson Jr, R.N.; Heymsfield, S.B. Multicomponent Methods: Evaluation of New and Traditional Soft Tissue Mineral Models by In Vivo Neutron Activation Analysis. Am. J. Clin. Nutr. 2002, 76, 968–974. [Google Scholar] [CrossRef] [PubMed]
- Thomaes, T.; Thomis, M.; Onkelinx, S.; Coudyzer, W.; Cornelissen, V.; Vanhees, L. Reliability and Validity of the Ultrasound Technique to Measure the Rectus Femoris Muscle Diameter in Older CAD-Patients. BMC Med Imaging 2012, 12, 7. [Google Scholar] [CrossRef]
- Jenkins, N.D.; Miller, J.M.; Buckner, S.L.; Cochrane, K.C.; Bergstrom, H.C.; Hill, E.C.; Smith, C.M.; Housh, T.J.; Cramer, J.T. Test–Retest Reliability of Single Transverse versus Panoramic Ultrasound Imaging for Muscle Size and Echo Intensity of the Biceps Brachii. Ultrasound Med. Biol. 2015, 41, 1584–1591. [Google Scholar] [CrossRef] [PubMed]
- Fullmer, S.; Benson-Davies, S.; Earthman, C.P.; Frankenfield, D.C.; Gradwell, E.; Lee, P.S.; Piemonte, T.; Trabulsi, J. Evidence Analysis Library Review of Best Practices for Performing Indirect Calorimetry in Healthy and Non–Critically Ill Individuals. J. Acad. Nutr. Diet. 2015, 115, 1417–1446.e2. [Google Scholar] [CrossRef] [PubMed]
- Migueles, J.H.; Rowlands, A.V.; Huber, F.; Sabia, S.; Van Hees, V.T. GGIR: A Research Community–Driven Open Source R Package for Generating Physical Activity and Sleep Outcomes From Multi-Day Raw Accelerometer Data. J. Meas. Phys. Behav. 2019, 2, 188–196. [Google Scholar] [CrossRef]
- Harrell, F.E. Regression Modeling Strategies: With Applications to Linear Models, Logistic Regression, and Survival Analysis; Springer: Cham, Switzerland, 2015. [Google Scholar]
- Newcombe, P.J.; Connolly, S.; Seaman, S.; Richardson, S.; Sharp, S.J. A Two-Step Method for Variable Selection in the Analysis of a Case-Cohort Study. Int. J. Epidemiol. 2017, 47, 597–604. [Google Scholar] [CrossRef] [PubMed]
- Juho, P.; Aki, V. On the Hyperprior Choice for the Global Shrinkage Parameter in the Horseshoe Prior. In Proceedings of the 20th International Conference on Artificial Intelligence and Statistics, Ft. Lauderdale, FL, USA, 20–22 April 2017; Volume 54, pp. 905–913. Available online: http://proceedings.mlr.press (accessed on 21 April 2021).
- Piironen, J.; Vehtari, A. Sparsity Information and Regularization in the Horseshoe and Other Shrinkage Priors. Electron. J. Stat. 2017, 11, 5018–5051. [Google Scholar] [CrossRef]
- McShane, B.B.; Gal, D.; Gelman, A.; Robert, C.; Tackett, J.L. Abandon Statistical Significance. Am. Stat. 2019, 73, 235–245. [Google Scholar] [CrossRef]
- Amrhein, V.; Greenland, S.; McShane, B. Scientists Rise up against Statistical Significance. Nat. Cell Biol. 2019, 567, 305–307. [Google Scholar] [CrossRef] [PubMed]
- Buuren, S.V. Flexible Imputation of Missing Data; CRC Press: Florida, FL, USA, 2018. [Google Scholar]
- Rubin, D.B. Multiple Imputation for Nonresponse in Surveys; Wiley: Hoboken, NJ, USA, 2004. [Google Scholar]
- Morris, T.P.; Kahan, B.C.; White, I.R. Choosing Sensitivity Analyses for Randomised Trials: Principles. BMC Med Res. Methodol. 2014, 14, 11. [Google Scholar] [CrossRef]
- Gabry, J.; Simpson, D.; Vehtari, A.; Betancourt, M.; Gelman, A. Visualization in Bayesian workflow. J. R. Stat. Soc. Ser. A Stat. Soc. 2019, 182, 389–402. [Google Scholar] [CrossRef]
- Vehtari, A.; Gelman, A.; Gabry, J. Practical Bayesian Model Evaluation using Leave-One-Out Cross-Validation and WAIC. Sta-t. Comput. 2017, 27, 1413–1432. [Google Scholar] [CrossRef]
- Carpenter, B.; Gelman, A.; Hoffman, M.D.; Lee, D.; Goodrich, B.; Betancourt, M.; Brubaker, M.; Guo, J.; Li, P.; Riddell, A. Stan: A Probabilistic Programming Language. J. Stat. Softw. 2017, 76, 1–32. [Google Scholar] [CrossRef]
- Bürkner, P.-C. brms: An R Package for Bayesian Multilevel Models Using Stan. J. Stat. Softw. 2017, 80, 1–28. [Google Scholar] [CrossRef]
- van Buuren, S.; Groothuis-Oudshoorn, K. mice: Multivariate Imputation by Chained Equations in R. J. Stat. Softw. 2011, 2010, 1–68. [Google Scholar] [CrossRef]
- Harrell, F.E. rms: Regression Modeling Strategies. BIOS 2018, 330, 14. [Google Scholar]
- Canty, A.; Ripley, B.D. Boot: Bootstrap R (S-Plus) Functions. 2020. Available online: https://rdrr.io/cran/boot/ (accessed on 11 April 2020).
- Vehtari, A.; Gabry, J.; Magnusson, M.; Yao, Y.; Gelman, A. loo: Efficient Leave-One-Out Cross-Validation and WAIC for Bayesian Models. 2019. Available online: https://mc-stan.org/loo/ (accessed on 11 April 2020).
- Schoenfeld, B.J.; Ratamess, N.A.; Peterson, M.D.; Contreras, B.; Tiryaki-Sonmez, G. Influence of Resistance Training Frequen-cy on Muscular Adaptations in Well-Trained Men. J. Strength Cond. Res. 2015, 29, 1821–1829. [Google Scholar] [CrossRef]
- Jäger, R.; Kerksick, C.M.; Campbell, B.I.; Cribb, P.J.; Wells, S.D.; Skwiat, T.M.; Purpura, M.; Ziegenfuss, T.N.; Ferrando, A.A.; Arent, S.M.; et al. International Society of Sports Nutrition Position Stand: Protein and Exercise. J. Int. Soc. Sports Nutr. 2017, 14, 20. [Google Scholar] [CrossRef]
- Witard, O.C.; Jackman, S.R.; Breen, L.; Smith, K.; Selby, A.; Tipton, K.D. Myofibrillar Muscle Protein Synthesis Rates Subse-quent to a Meal in Response to Increasing Doses of Whey Protein at Rest and after Resistance Exercise. Am. J. Clin. Nutr. 2014, 99, 86–95. [Google Scholar] [CrossRef] [PubMed]
- Slater, G.J.; Dieter, B.P.; Marsh, D.J.; Helms, E.R.; Shaw, G.; Iraki, J. Is an Energy Surplus Required to Maximize Skeletal Muscle Hypertrophy Associated With Resistance Training. Front. Nutr. 2019, 6, 131. [Google Scholar] [CrossRef] [PubMed]
- Bray, G.A.; Smith, S.R.; de Jonge, L.; Xie, H.; Rood, J.; Martin, C.K.; Most, M.; Brock, C.; Mancuso, S.; Redman, L.M. Effect of Dietary Protein Content on Weight Gain, Energy Expenditure, and Body Composition during Overeating: A Randomized Controlled Trial. JAMA 2012, 307, 47–55. [Google Scholar] [CrossRef]
- Dhurandhar, N.V.; The Energy Balance Measurement Working Group; Schoeller, D.; Brown, A.W.; Heymsfield, S.B.; Thomas, D.; Sørensen, I.A.T.; Speakman, J.R.; Jeansonne, M.; Allison, D.B. Energy Balance Measurement: When Something is Not Better than Nothing. Int. J. Obes. 2015, 39, 1109–1113. [Google Scholar] [CrossRef]
- Thomas, D.T.; Erdman, K.A.; Burke, L.M. Nutrition and Athletic Performance. Med. Sci. Sports Exerc. 2016, 48, 543–568. [Google Scholar] [CrossRef] [PubMed]
- Moore, D.R.; Tang, J.E.; Burd, N.A.; Rerecich, T.; Tarnopolsky, M.A.; Phillips, S.M. Differential Stimulation of Myofibrillar and Sarcoplasmic Protein Synthesis with Protein Ingestion at Rest and after Resistance Exercise. J. Physiol. 2009, 587, 897–904. [Google Scholar] [CrossRef]
- Schoenfeld, B.J.; Ogborn, D.; Krieger, J.W. Dose-Response Relationship between Weekly Resistance Training Volume and In-creases in Muscle Mass: A Systematic Review and Meta-Analysis. J. Sports Sci. 2017, 35, 1073–1082. [Google Scholar] [CrossRef]
- Ashtary-Larky, D.; Bagheri, R.; Abbasnezhad, A.; Tinsley, G.M.; Alipour, M.; Wong, A. Effects of Gradual Weight Loss v. Rapid Weight Loss on Body Composition and RMR: A Systematic Review and Meta-Analysis. Br. J. Nutr. 2020, 124, 1121–1132. [Google Scholar] [CrossRef]

| Weeks 1–3 | Weeks 4–6 | ||||
|---|---|---|---|---|---|
| Week 1 | Week 2 | Week 3 | Week 4 | Week 5 | Week 6 |
| 2 RIR | 1 RIR | 0 RIR | 2 RIR | 1 RIR | 0 RIR |
| Training Sessions | Exercises | (Sets) × (Reps) | Training Sessions | Exercises | (Sets) × (Reps) |
| Lower Body | Hip Sled | 3 × 6-8 | Lower Body | Hip Sled | 3 × 4-6 |
| Romanian Deadlift | 3 × 10-12 | Romanian Deadlift | 3 × 8-10 | ||
| DB Walking Lunges | 3 × 10-12 | DB Walking Lunges | 3 × 8-10 | ||
| Lying Leg Curl | 2 × 10-12 | Lying Leg Curl | 2 × 8-10 | ||
| Leg Extension | 2 × 10-12 | Leg Extension | 2 × 8-10 | ||
| Single Leg DB Calf Raise | 2 × 10-12 | Single Leg DB Calf Raise | 2 × 8-10 | ||
| Upper Body | Bench Press | 4 × 6-8 | Upper Body | Bench Press | 4 × 4-6 |
| Supinated BB Row | 3 × 6-8 | Supinated BB Row | 3 × 4-6 | ||
| Close Grip Bench Press | 3 × 10-12 | Close Grip Bench Press | 3 × 8-10 | ||
| Neutral Grip Pull up | 2 × 10-12 | Neutral Grip Pull up | 2 × 8-10 | ||
| DB Side Laterals | 2 × 10-12 | DB Side Laterals | 2 × 8-10 | ||
| EZ Bar Bicep Curl | 2 × 10-12 | EZ Bar Bicep Curl | 2 × 8-10 | ||
| Full Body | BB Conventional Deadlift | 3 × 6-8 | Full Body | BB Conventional Deadlift | 3 × 4-6 |
| Hip Sled | 2 × 10-12 | Hip Sled | 2 × 8-10 | ||
| Seated Leg Curl | 2 × 10-12 | Seated Leg Curl | 2 × 8-10 | ||
| Feet up Bench Press | 3 × 10-12 | Feet up Bench Press | 3 × 8-10 | ||
| Pendlay Row | 2 × 10-12 | Pendlay Row | 2 × 8-10 | ||
| DB Kickbacks | 2 × 10-12 | DB Kickbacks | 2 × 8-10 | ||
| DB Curl | 2 × 10-12 | DB Curl | 2 × 8-10 | ||
| Variable | Time Point | Mean | SD | Min | Max |
|---|---|---|---|---|---|
| Body Mass (kg) | Pre | 73.8 | 12.4 | 55.5 | 109.9 |
| Post | 79.6 | 13.2 | 57.3 | 118.3 | |
| Individual Δ (%) | 4.8 | 2.5 | 1.1 | 9.5 | |
| Fat Mass Index (kg/m2) | Pre | 3.2 | 1.3 | 0.6 | 5.8 |
| Post | 3.4 | 1.6 | 0.4 | 5.9 | |
| Fat-Free Mass Index (kg/m2) | Pre | 19.7 | 2.0 | 16.6 | 25.5 |
| Post | 20.5 | 2.1 | 17.8 | 27.1 | |
| Muscle Thickness—Elbow Flexors (cm) | Pre | 3.9 | 0.5 | 2.9 | 5.0 |
| Post | 4.0 | 0.4 | 3.4 | 5.2 | |
| Individual Δ (%) | 4.5 | 5.9 | −8.6 | 16.7 | |
| Muscle Thickness—Knee Extensors (cm) | Pre | 5.2 | 0.8 | 3.8 | 6.9 |
| Post | 5.4 | 0.8 | 4.4 | 7.5 | |
| Individual Δ (%) | 7.4 | 8.4 | −5.4 | 26.4 | |
| Bench Press 1RM (kg/kg BM) | Pre | 1.3 | 0.2 | 1.0 | 1.8 |
| Post | 1.4 | 0.2 | 1.1 | 1.9 | |
| Individual Δ (%) | 12.5 | 8.0 | 4.3 | 35.5 | |
| Leg Press 1RM (kg/kg BM) | Pre | 3.3 | 0.8 | 2.0 | 5.0 |
| Post | 4.2 | 0.8 | 3.0 | 6.3 | |
| Individual Δ (%) | 37.2 | 15.7 | 16.5 | 66.7 | |
| Bench Press Endurance (reps) | Pre | 14.0 | 2.0 | 9.0 | 19.0 |
| Post | 19.0 | 5.1 | 13.0 | 31.0 | |
| Individual Δ (%) | 35.8 | 37.5 | −13.3 | 106.7 | |
| Leg Press Endurance (reps) | Pre | 15.4 | 4.7 | 4.0 | 24.0 |
| Post | 34.9 | 6.8 | 23.0 | 53.0 | |
| Individual Δ (%) | 161.3 | 146.5 | 55.0 | 650.0 | |
| Resting Metabolic Rate (kcal/kg) | Pre | 27.7 | 1.5 | 25.1 | 31.6 |
| Post | 29.0 | 1.4 | 26.2 | 32.1 | |
| Individual Δ (%) | 10.9 | 6.4 | −2.0 | 21.5 | |
| Respiratory Exchange Ratio (au) | Pre | 0.8 | 0.1 | 0.7 | 1.1 |
| Post | 0.8 | 0.0 | 0.8 | 1.0 | |
| Individual Δ (%) | −0.6 | 9.2 | −18.5 | 18.8 | |
| Energy Intake (kcal/kg) | Baseline | 46.8 | 16.8 | 33.3 | 124.0 |
| Intervention | 52.3 | 17.2 | 24.8 | 119.9 | |
| Individual Δ (%) | 15.9 | 30.4 | −27.0 | 93.5 | |
| Protein Intake (g/kg) | Baseline | 2.3 | 0.9 | 1.4 | 5.8 |
| Intervention | 2.2 | 0.6 | 1.6 | 4.8 | |
| Individual Δ (%) | 11.6 | 30.2 | −37.8 | 73.3 | |
| Fat Intake (g/kg) | Baseline | 1.7 | 0.9 | 0.9 | 6.2 |
| Intervention | 1.9 | 0.9 | 0.5 | 4.6 | |
| Individual Δ (%) | 16.5 | 36.3 | −50.7 | 91.5 | |
| Carbohydrate Intake (g/kg) | Baseline | 5.6 | 1.5 | 3.6 | 11.5 |
| Intervention | 6.0 | 2.0 | 3.1 | 13.7 | |
| Individual Δ (%) | 11.3 | 34.3 | −30.6 | 157.2 | |
| Total Volume Load (kg/10,000) | Intervention | 37.1 | 7.4 | 27.4 | 48.8 |
| Total Upper Body Volume Load (kg/10,000) | Intervention | 16.5 | 3.9 | 11.4 | 25.0 |
| Total Lower Body Volume Load (kg/10,000) | Intervention | 18.4 | 3.5 | 14.4 | 25.1 |
| Time in Sedentary Activity (min/day) | Baseline | 635.4 | 66.7 | 481.5 | 740.4 |
| Intervention | 603.5 | 72.9 | 406.6 | 719.1 | |
| Time in Light-intensity Activity (min/day) | Baseline | 222.4 | 47.1 | 107.5 | 300.2 |
| Intervention | 170.8 | 74.2 | 78.0 | 400.6 | |
| Time in Moderate- or Vigorous-Intensity Activity (min/day) | Baseline | 113.0 | 43.0 | 0.0 | 198.9 |
| Intervention | 89.1 | 32.3 | 32.8 | 152.3 | |
| Composition score ([∆Fat-free mass/∆Body Mass]*100) | -- | 90.3 | 36.7 | 8.0 | 145.7 |
| Fat Mass | Individual Δ (%) | 12.1 | 28.1 | −40.4 | 99.4 |
| Fat-Free Mass | Individual Δ (%) | 4.8 | 2.6 | 0.5 | 8.8 |
| ELPD | IC | |||||
|---|---|---|---|---|---|---|
| Outcome | Est. | SE | Est. | SE | R2 | RMSE |
| Composition † | −146.13 | 5.42 | 292.25 | 10.84 | 0.36 | 45.84 |
| ∆RMR | −96.28 | 2.68 | 192.57 | 5.36 | 0.24 | 6.75 |
| ∆MTKE | −107.37 | 3.18 | 214.74 | 6.35 | 0.25 | 10.07 |
| ∆MTEF | −94.63 | 4.25 | 189.25 | 8.51 | 0.18 | 6.89 |
| ∆1RMLP | −121.07 | 3.89 | 242.14 | 7.78 | 0.34 | 16.30 |
| ∆1RMBP | −94.12 | 3.12 | 188.24 | 6.24 | 0.40 | 6.64 |
| ∆RTFLP | −179.03 | 11.83 | 358.05 | 23.66 | 0.33 | 147.50 |
| ∆RTFBP | −146.36 | 4.52 | 292.72 | 9.04 | 0.19 | 42.83 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Smith, R.W.; Harty, P.S.; Stratton, M.T.; Rafi, Z.; Rodriguez, C.; Dellinger, J.R.; Benavides, M.L.; Johnson, B.A.; White, S.J.; Williams, A.D.; et al. Predicting Adaptations to Resistance Training Plus Overfeeding Using Bayesian Regression: A Preliminary Investigation. J. Funct. Morphol. Kinesiol. 2021, 6, 36. https://doi.org/10.3390/jfmk6020036
Smith RW, Harty PS, Stratton MT, Rafi Z, Rodriguez C, Dellinger JR, Benavides ML, Johnson BA, White SJ, Williams AD, et al. Predicting Adaptations to Resistance Training Plus Overfeeding Using Bayesian Regression: A Preliminary Investigation. Journal of Functional Morphology and Kinesiology. 2021; 6(2):36. https://doi.org/10.3390/jfmk6020036
Chicago/Turabian StyleSmith, Robert W., Patrick S. Harty, Matthew T. Stratton, Zad Rafi, Christian Rodriguez, Jacob R. Dellinger, Marqui L. Benavides, Baylor A. Johnson, Sarah J. White, Abegale D. Williams, and et al. 2021. "Predicting Adaptations to Resistance Training Plus Overfeeding Using Bayesian Regression: A Preliminary Investigation" Journal of Functional Morphology and Kinesiology 6, no. 2: 36. https://doi.org/10.3390/jfmk6020036
APA StyleSmith, R. W., Harty, P. S., Stratton, M. T., Rafi, Z., Rodriguez, C., Dellinger, J. R., Benavides, M. L., Johnson, B. A., White, S. J., Williams, A. D., & Tinsley, G. M. (2021). Predicting Adaptations to Resistance Training Plus Overfeeding Using Bayesian Regression: A Preliminary Investigation. Journal of Functional Morphology and Kinesiology, 6(2), 36. https://doi.org/10.3390/jfmk6020036





