Brachial Plexus Injuries in Sport Medicine: Clinical Evaluation, Diagnostic Approaches, Treatment Options, and Rehabilitative Interventions
Abstract
1. Introduction
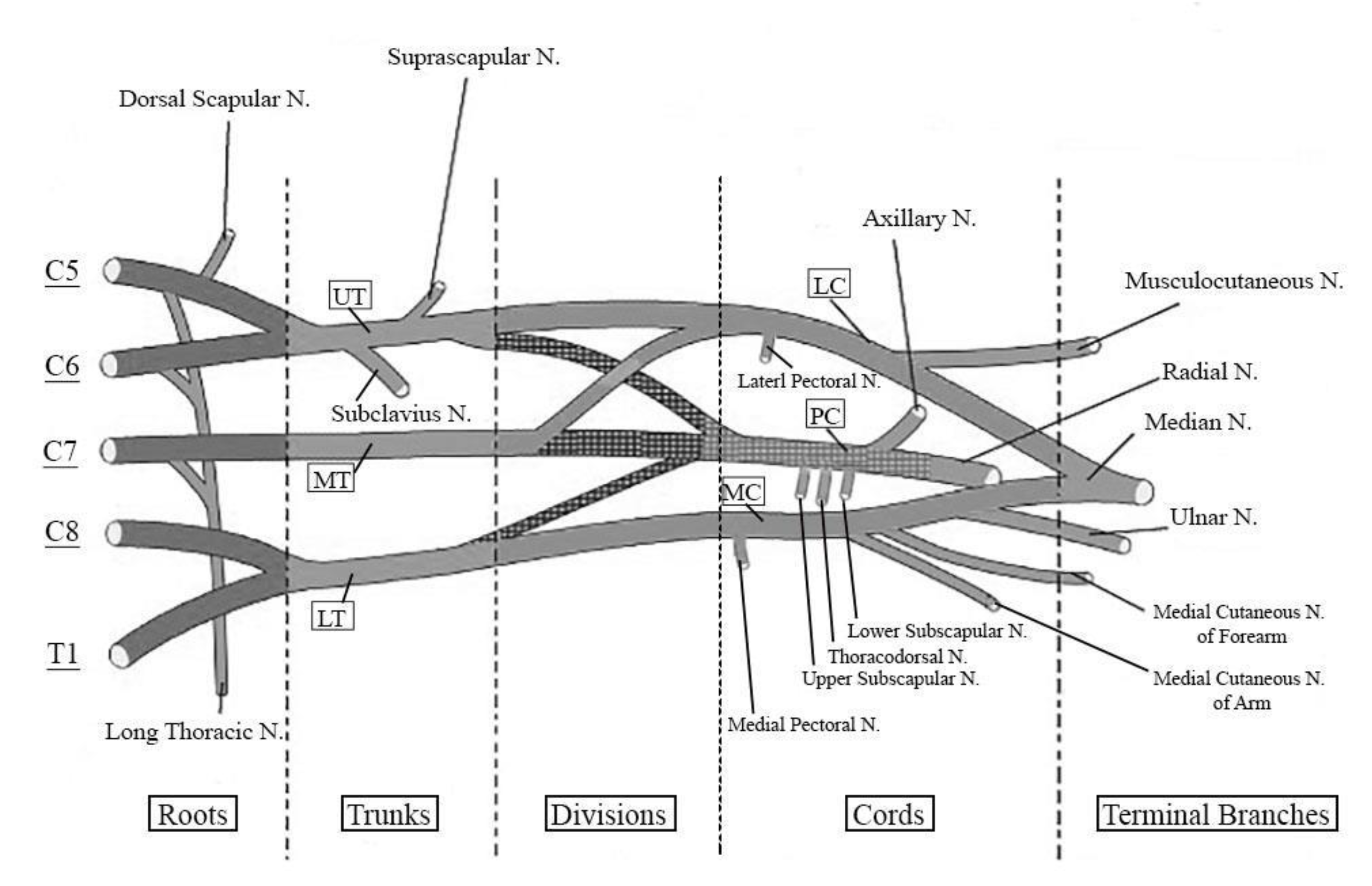
2. The Spinal Nerves
3. Anatomy of the Brachial Plexus
4. Nerve Injuries: Pathophysiology and Impact on Prognosis
5. Epidemiology of BPIs and Their Relevance in Sport Medicine
6. Clinical Evaluation
6.1. Clinical Findings
6.2. Electrodiagnostic Studies
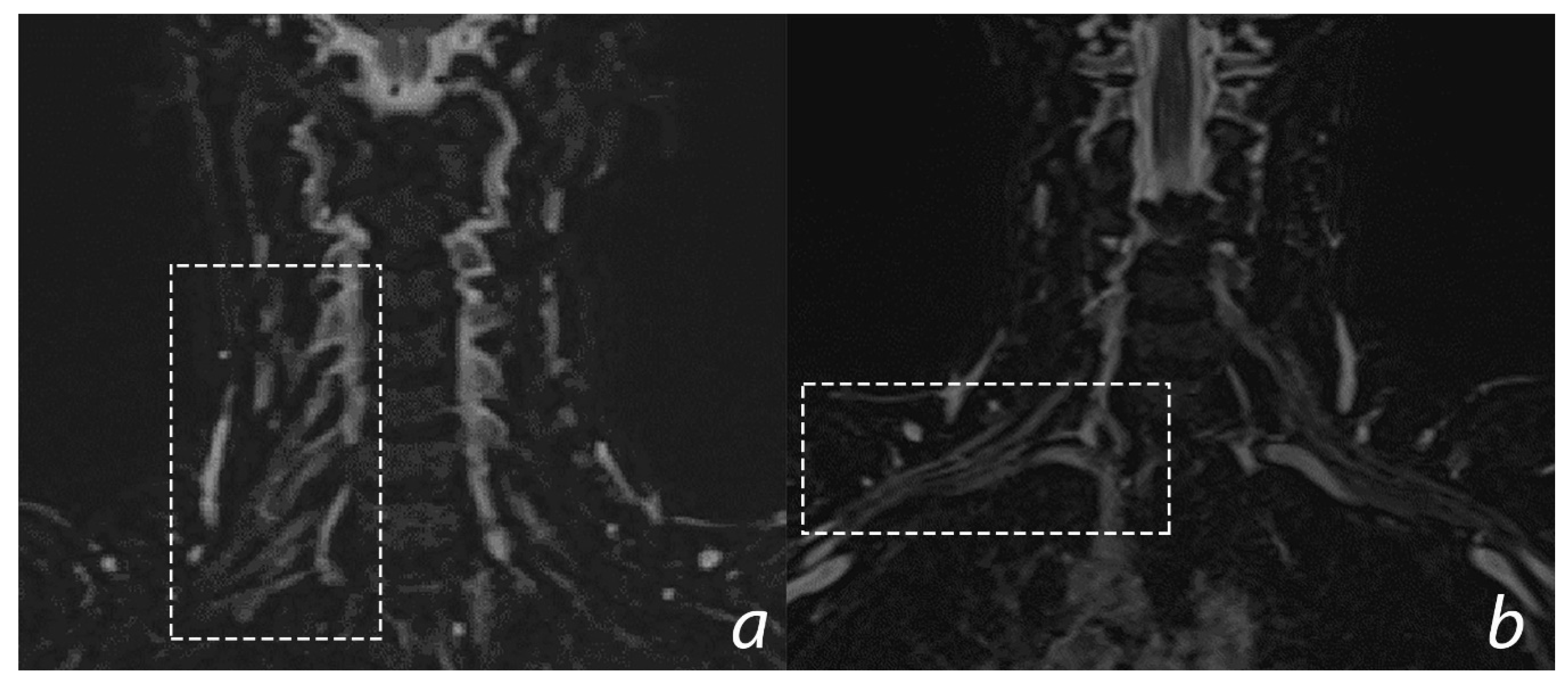
6.3. Imaging
7. Therapeutic Options
7.1. Rehabilitation
7.2. Surgery
8. The Sport Doctor and the Management of the Athlete with BPIs: From the Side-Line to the Return to Play
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Faglioni, W.; Siqueira, M.G.; Martins, R.S.; Heise, C.O.; Foroni, L. The epidemiology of adult traumatic brachial plexus lesions in a large metropolis. Acta Neurochir. (Wien) 2014, 156, 1025–1028. [Google Scholar] [CrossRef] [PubMed]
- Midha, R. Epidemiology of brachial plexus injuries in a multitrauma population. Neurosurgery 1997, 40, 1182–1189. [Google Scholar] [CrossRef] [PubMed]
- Smania, N.; Berto, G.; La Marchina, E.; Melotti, C.; Midiri, A.; Roncari, L.; Zenorini, A.; Ianes, P.; Picelli, A.; Waldner, A.; et al. Rehabilitation of brachial plexus injuries in adults and children. Eur. J. Phys. Rehabil. Med. 2012, 48, 483–506. [Google Scholar]
- Hems, T. Brachial Plexus Injuries. In Nerves and Nerve Injuries, Vol 2: Pain, Treatment, Injury, Disease and Future Directions; Academic Press Elsevier: Cambridge, MA, USA, 2015; pp. 681–706. [Google Scholar]
- Kaiser, R.; Waldauf, P.; Ullas, G.; Krajcová, A. Epidemiology, etiology, and types of severe adult brachial plexus injuries requiring surgical repair: Systematic review and meta-analysis. Neurosurg. Rev. 2018, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Krivickas, L.S.; Wilbourn, A.J. Peripheral nerve injuries in athletes: A case series of over 200 injuries. Semin. Neurol. 2000, 20, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Saliba, S.; Saliba, E.N.; Pugh, K.F.; Chhabra, A.; Diduch, D. Rehabilitation considerations of a brachial plexus injury with complete avulsion of C5 and C6 nerve roots in a college football player: A case study. Sports Health 2009, 1, 370–375. [Google Scholar] [CrossRef]
- Johnson, E.O.; Vekris, M.; Demesticha, T.; Soucacos, P.N. Neuroanatomy of the brachial plexus: Normal and variant anatomy of its formation. Surg. Radiol. Anat. 2010, 32, 291–297. [Google Scholar] [CrossRef]
- Higuchi, K.; Sato, T. Anatomical study of lumbar spine innervation. Folia Morphol. (Warsz) 2002, 61, 71–79. [Google Scholar]
- Stifani, N. Motor neurons and the generation of spinal motor neuron diversity. Front. Cell Neurosci. 2014, 8, 293. [Google Scholar] [CrossRef]
- Light, A.R.; Metz, C.B. The morphology of the spinal cord efferent and afferent neurons contributing to the ventral roots of the cat. J. Comp. Neurol. 1978, 179, 501–515. [Google Scholar] [CrossRef]
- Liu, Y.T.; Zhou, X.J.; Ma, J.; Ge, Y.; Bin, C.X. The diameters and number of nerve fibers in spinal nerve roots. J. Spinal. Cord Med. 2015, 38, 532–537. [Google Scholar] [CrossRef]
- Glenesk, N.L.; Lopez, P.P. Anatomy, Head and Neck, Posterior Cervical Nerve Plexus; StatPearls Publishing: Treasure Island, FL, USA, 2019. [Google Scholar]
- Usui, Y.; Kobayashi, T.; Kakinuma, H.; Watanabe, K.; Kitajima, T.; Matsuno, K. An anatomical basis for blocking of the deep cervical plexus and cervical sympathetic tract using an ultrasound-guided technique. Anesth. Analg. 2010, 110, 964–968. [Google Scholar] [CrossRef] [PubMed]
- Leinberry, C.F.; Wehbé, M.A. Brachial plexus anatomy. Hand Clin. 2004, 20, 1–5. [Google Scholar] [CrossRef]
- Orebaugh, S.L.; Williams, B.A. Brachial plexus anatomy: Normal and variant. Sci. World J. 2009, 9, 300–312. [Google Scholar] [CrossRef] [PubMed]
- Kattan, A.E.; Borschel, G.H. Anatomy of the brachial plexus. J. Pediatr. Rehabil. Med. 2011, 4, 107–111. [Google Scholar] [CrossRef]
- Polcaro, L.; Daly, D.T. Anatomy, Head and Neck, Brachial Plexus; StatPearls Publishing: Treasure Island, FL, USA, 2018. [Google Scholar]
- Gu, Y. Functional motor innervation of brachial plexus roots. An intraoperative electrophysiological study. Chin. Med. J. Engl. 1996, 109, 749–751. [Google Scholar]
- Bertelli, J.A.; Ghizoni, M.F. Long thoracic nerve: Anatomy and functional assessment. J. Bone Jt. Surg. Ser. A 2005, 87, 993–998. [Google Scholar]
- Tubbs, R.S.; Tyler-Kabara, E.C.; Aikens, A.C.; Martin, J.P.; Weed, L.L.; Salter, E.G.; Oakes, W.J. Surgical anatomy of the dorsal scapular nerve. J. Neurosurg. 2005, 102, 910–911. [Google Scholar] [CrossRef]
- Okwumabua, E.; Thompson, J.H. Anatomy, Shoulder and Upper Limb, Nerves; StatPearls Publishing: Treasure Island, FL, USA, 2018. [Google Scholar]
- Greiner, A.; Golser, K.; Wambacher, M.; Kralinger, F.; Sperner, G. The course of the suprascapular nerve in the supraspinatus fossa and its vulnerability in muscle advancement. J. Shoulder Elb Surg. 2003, 12, 256–259. [Google Scholar] [CrossRef]
- Hoffman, G.W.; Elliott, L.F. The anatomy of the pectoral nerves and its significance to the general and plastic surgeon. Ann. Surg. 1987, 205, 504–507. [Google Scholar] [CrossRef]
- Benedikt, S.; Parvizi, D.; Feigl, G.; Koch, H. Anatomy of the medial antebrachial cutaneous nerve and its significance in ulnar nerve surgery: An anatomical study. J. Plast. Reconstr. Aesthetic Surg. 2017, 70, 1582–1588. [Google Scholar] [CrossRef] [PubMed]
- Tubbs, R.S.; Loukas, M.; Shahid, K.; Judge, T.; Pinyard, J.; Shoia, M.M.; Slappey, J.B.; McEvoy, W.C.; Oakes, W.J. Anatomy and quantitation of the subscapular nerves. Clin. Anat. 2007, 20, 656–659. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.B.J.; Robinson, T.; Kingery, W.S.; Date, E.S. Thoracodorsal nerve conduction study. Am. J. Phys. Med. Rehabil. 1998, 77, 296–298. [Google Scholar] [CrossRef] [PubMed]
- Prakash, K.G.; Saniya, K. Anatomy of axillary nerve and its clinical importance: A cadaveric study. J. Clin. Diagn. Res. 2015, 9, AC13–AC17. [Google Scholar]
- Osborne, A.W.; Birch, R.M.; Munshi, P.; Bonney, G. The musculocutaneous nerve. J. Bone Joint. Surg. Br. 2000, 82, 1140–1142. [Google Scholar] [CrossRef]
- Abrams, R.A.; Ziets, R.J.; Lieber, R.L.; Botte, M.J. Anatomy of the radial nerve motor branches in the forearm. J. Hand. Surg. Am. 1997, 22, 232–237. [Google Scholar] [CrossRef]
- Murphy, K.A.; Morrisonponce, D. Anatomy, Shoulder and Upper Limb, Median Nerve; StatPearls Publishing: Treasure Island, FL, USA, 2019. [Google Scholar]
- Polatsch, D.B.; Melone, C.P.; Beldner, S.; Incorvaia, A. Ulnar Nerve Anatomy. Hand Clin. 2007, 23, 283–289. [Google Scholar] [CrossRef]
- Battista, A.F.; Lusskin, R. The anatomy and physiology of the peripheral nerve. Foot Ankle. 1986, 7, 65–70. [Google Scholar] [CrossRef]
- Sunderland, S. A classification of peripheral nerve injuries producing loss of function. Brain 1951, 74, 491–516. [Google Scholar] [CrossRef]
- Seddon, H.J. A classification of nerve injuries. Br. Med. J. 1942, 2, 237. [Google Scholar] [CrossRef]
- Dahlin, L.B.; Wiberg, M. Nerve injuries of the upper extremity and hand. EFORT Open Rev. 2017, 2, 158–170. [Google Scholar] [CrossRef] [PubMed]
- Feinberg, J.H. Burners and stingers. Phys. Med. Rehabil. Clin. N. Am. 2000, 11, 771–784. [Google Scholar] [CrossRef]
- Bridge, P.M.; Ball, D.J.; Mackinnon, S.E.; Nakao, Y.; Brandt, K.; Hunter, D.A.; Hertl, C. Nerve crush injuries-a model for axonotmesis. Exp. Neurol. 1994, 127, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Kang, H.; Lichtman, J.W. Motor axon regeneration and muscle reinnervation in young adult and aged animals. J. Neurosci. 2013, 33, 19480–19491. [Google Scholar] [CrossRef]
- Menorca, R.M.G.; Fussell, T.S.; Elfar, J.C. Nerve physiology. Mechanisms of injury and recovery. Hand Clin. 2013, 29, 317–330. [Google Scholar] [CrossRef]
- Eggermann, K.G.; Häusler, H.W. Hereditary neuropathies: Clinical presentation and genetic panel diagnosis. Dtsch. Arztebl. Int. 2018, 115, 91–97. [Google Scholar]
- Callaghan, B.; Feldman, E. The metabolic syndrome and neuropathy: Therapeutic challenges and opportunities. Ann. Neurol. 2013, 74, 397–403. [Google Scholar] [CrossRef]
- Manji, H. Toxic neuropathy. Curr. Opin. Neurol. 2011, 24, 484–490. [Google Scholar] [CrossRef]
- Hammond, N.; Wang, Y.; Dimachkie, M.M.; Barohn, R.J. Nutritional neuropathies. Neurol. Clin. 2013, 31, 477–489. [Google Scholar] [CrossRef]
- De Freitas, M.R.G. Infectious neuropathy. Curr. Opin. Neurol. 2007, 20, 548–552. [Google Scholar] [CrossRef]
- Ho, T.W.; McKhann, G.M.; Griffin, J.W. Human Autoimmune Neuropathies. Annu. Rev. Neurosci. 1998, 21, 187–226. [Google Scholar] [CrossRef] [PubMed]
- Toyooka, K.; Fujimura, H. Iatrogenic neuropathies. Curr. Opin. Neurol. 2009, 22, 475–479. [Google Scholar] [CrossRef] [PubMed]
- Koike, H.; Sobue, G. Paraneoplastic neuropathy. Handb Clin. Neurol. 2013, 115, 713–726. [Google Scholar] [PubMed]
- Clancy, W.G.; Brand, R.L.; Bergfield, J.A. Upper trunk brachial plexus injuries in contact sports. Am. J. Sports Med. 1977, 5, 209–216. [Google Scholar] [CrossRef]
- Sakellariou, V.I.; Badilas, N.K.; Mazis, G.A.; Stavropoulos, N.A.; Kotoulas, H.K.; Kyriakopoulos, S.; Tagkalegkas, I.; Sofianos, I.P. Brachial Plexus Injuries in Adults: Evaluation and Diagnostic Approach. ISRN Orthop. 2014, 2014, 1–9. [Google Scholar] [CrossRef]
- Kaiser, R.; Mencl, L.; Haninec, P. Injuries associated with serious brachial plexus involvement in polytrauma among patients requiring surgical repair. Injury 2014, 45, 223–226. [Google Scholar] [CrossRef]
- Gorden, J.A.; Straub, S.J.; Swanik, C.B.; Swanik, K.A. Effects of Football Collars on Cervical Hyperextension and Lateral Flexion. J. Athl. Train. 2003, 38, 209–215. [Google Scholar]
- Ferraresi, S.; Garozzo, D.; Griffini, C.; Resmini, B.; Manara, O.; Foresti, C.; Ubiali, E.; Bistoni, A.; Ghislandi, I. Brachial plexus injuries Guidelines for management: Our experience. Ital. J. Neurol. Sci. 1994, 15, 273–284. [Google Scholar] [CrossRef]
- Arzillo, S.; Gishen, K.; Askari, M. Brachial plexus injury: Treatment options and outcomes. J. Craniofac. Surg. 2014, 25, 1200–1206. [Google Scholar] [CrossRef]
- Kawasaki, T.; Maki, N.; Shimizu, K.; Ota, C.; Urayama, S.; Moriya, S.; Kaketa, T.; Kobayashi, H.; Kaneko, K. Do stingers affect scapular kinematics in rugby players? J. Shoulder Elb. Surg. 2014, 23, e293–e299. [Google Scholar] [CrossRef]
- Charbonneau, R.M.E.; McVeigh, S.A.; Thompson, K. Brachial neuropraxia in Canadian Atlantic University sport football players: What is the incidence of “stingers”? Clin. J. Sport Med. 2012, 22, 472–477. [Google Scholar] [CrossRef] [PubMed]
- Starr, H.M.; Anderson, B.; Courson, R.; Seiler, J.G. Brachial plexus injury: A descriptive study of American football. J. Surg. Orthop. Adv. 2014, 23, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Thatte, M.R.; Babhulkar, S.; Hiremath, A. Brachial plexus injury in adults: Diagnosis and surgical treatment strategies. Ann. Indian Acad. Neurol. 2013, 16, 26–33. [Google Scholar] [CrossRef] [PubMed]
- Amato, A.A.; Russell, J.A.; James, A. Neuromuscular Disorders; McGraw-Hill Medical: New York, NY, USA, 2008. [Google Scholar]
- Sirico, F.; Castaldo, C.; Baioccato, V.; Marino, N.; Zappia, M.; Montagnani, S.; Di Meglio, F.; Nurzynska, D. Prevalence of musculocutaneous nerve variations: Systematic review and meta-analysis. Clin. Anat. 2019, 32, 183–195. [Google Scholar] [CrossRef]
- Sakellariou, V.I.; Badilas, N.K.; Stavropoulos, N.A.; Mazis, G.; Kotoulas, H.K.; Kyriakopoulos, S.; Tagkalegkas, I.; Sofianos, I.P. Treatment Options for Brachial Plexus Injuries. ISRN Orthop. 2014, 2014, 1–10. [Google Scholar] [CrossRef]
- Martin, R.M.; Fish, D.E. Scapular winging: Anatomical review, diagnosis and treatments. Curr. Rev. Musculoskelet Med. 2008, 1, 1–11. [Google Scholar] [CrossRef]
- Gooding, B.W.T.; Geoghegan, J.M.; Wallace, W.A.; Manning, P.A. Scapular Winging. Shoulder Elb. 2014, 6, 4–11. [Google Scholar] [CrossRef]
- Kanagalingam, S.; Miller, N.R. Horner syndrome: Clinical perspectives. Eye Brain 2015, 7, 35–46. [Google Scholar]
- Chater, M.; Camfield, P.; Camfield, C. Erb’s palsy—Who is to blame and what will happen? Paediatr. Child Health (Oxford) 2004, 9, 556–560. [Google Scholar] [CrossRef]
- Merryman, J.; Varacallo, M. Klumpke’s Palsy; StatPearls Publishing: Treasure Island, FL, USA, 2019. [Google Scholar]
- Emamhadi, M.; Andalib, S. Successful recovery of sensation loss in upper brachial plexus injuries. Acta Neurochir. (Wien) 2018, 160, 2019–2023. [Google Scholar] [CrossRef] [PubMed]
- Mansukhani, K.A. Electrodiagnosis in traumatic brachial plexus injury. Ann. Indian Acad. Neurol. 2013, 16, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Varacallo, M.; Mair, S.D. Proximal Biceps Tendinitis and Tendinopathy; StatPearls Publishing: Treasure Island, FL, USA, 2019. [Google Scholar]
- Kimura, J. Electrodiagnosis in Diseases of Nerve and Muscle; Oxford University Press: Oxford, UK, 2014. [Google Scholar]
- Taverner, D. Electrodiagnosis in Facial Palsy. Arch. Otolaryngol. 1965, 81, 470–477. [Google Scholar] [CrossRef]
- Daube, J.R.; Rubin, D.I. Needle electromyography. Muscle Nerve 2009, 39, 244–270. [Google Scholar] [CrossRef] [PubMed]
- Preston, D.C.; Shapiro, B.E. Needle electromyography. Fundamentals, normal and abnormal patterns. Neurol. Clin. 2002, 20, 361–396. [Google Scholar] [CrossRef]
- Benecke, R.; Berthold, A.; Conrad, B. Denervation activity in the EMG of patients with upper motor neuron lesions: Time course, local distribution and pathogenetic aspects. J. Neurol. 1983, 230, 143–151. [Google Scholar] [CrossRef]
- Presciutti, S.M.; DeLuca, P.; Marchetto, P.; Wilsey, J.T.; Shaffrey, C.; Vaccaro, A.R. Mean subaxial space available for the cord index as a novel method of measuring cervical spine geometry to predict the chronic stinger syndrome in American football players. J. Neurosurg. Spine 2009, 11, 264–271. [Google Scholar] [CrossRef]
- Gasparotti, R. New techniques in spinal imaging. Neuroradiology. 2011, 53 (Suppl. 1), S195–S197. [Google Scholar] [CrossRef]
- Bianchi, S.; Martinoli, C. Ultrasound of the Musculoskeletal System; Springer: Heidelberg, Germany, 2007. [Google Scholar]
- Hartley, R.A.; Kordecki, M.E. Rehabilitation of chronic brachial plexus neuropraxia and loss of cervical extension in a high school football player: A case report. Int. J. Sports Phys Ther. 2018, 13, 1061–1072. [Google Scholar] [CrossRef]
- Cui, J.; Blaha, C.; Moradkhan, R.; Gray, K.S.; Sinoway, L.I. Muscle sympathetic nerve activity responses to dynamic passive muscle stretch in humans. J. Physiol. 2006, 576, 625–634. [Google Scholar] [CrossRef]
- Limthongthang, R.; Muennoi, P.; Phoojaroenchanachai, R.; Vathana, T.; Wongtrakul, S.; Songcharoen, P. Effectiveness and safety of home-based muscle electrical stimulator in brachial plexus injury patients. J. Med. Assoc. Thai. 2014, 97 (Suppl. 9), S56–S61. [Google Scholar]
- Lovaglio, A.; Socolovsky, M.; Di Masi, G.; Bonilla, G. Treatment of neuropathic pain after peripheral nerve and brachial plexus traumatic injury. Neurol. India. 2019, 67, 32. [Google Scholar] [CrossRef] [PubMed]
- Sharman, M.J.; Cresswell, A.G.; Riek, S. Proprioceptive neuromuscular facilitation stretching: Mechanisms and clinical implications. Sport Med. 2006, 36, 929–939. [Google Scholar] [CrossRef] [PubMed]
- Maroto-Izquierdo, S.; García-López, D.; De Paz, J.A. Functional and Muscle-Size Effects of Flywheel Resistance Training with Eccentric-Overload in Professional Handball Players. J. Hum. Kinet. 2017, 60, 133–143. [Google Scholar] [CrossRef] [PubMed]
- Shipton, E.A. Skin matters: Identifying pain mechanisms and predicting treatment outcomes. Neurol. Res. Int. 2013, 2013. [Google Scholar] [CrossRef] [PubMed]
- Derry, S.; Bell, R.F.; Straube, S.; Wiffen, P.J.; Aldington, D.; Moore, R.A. Pregabalin for neuropathic pain in adults. Cochrane Database Syst. Rev. 2019. [Google Scholar] [CrossRef] [PubMed]
- Loiacono, C.; Palermi, S.; Massa, B.; Belviso, I.; Romano, V.; Di Gregorio, A.; Sirico, F.; Sacco, A.M. Tendinopathy: Pathophysiology, therapeutic options, and role of nutraceutics. A narrative literature review. Medicine 2019, 55, 447. [Google Scholar] [CrossRef]
- Sirico, F.; Miressi, S.; Castaldo, C.; Spera, R.; Montagnani, S.; Di Meglio, F.; Nurzynska, D. Habits and beliefs related to food supplements: Results of a survey among Italian students of different education fields and levels. PLoS ONE 2018, 13. [Google Scholar] [CrossRef]
- Sirico, F.; Ricca, F.; Di Meglio, F.; Nurzynska, D.; Castaldo, C.; Spera, R.; Montagnani, S. Local corticosteroid versus autologous blood injections in lateral epicondylitis: Meta-analysis of randomized controlled trials. Eur. J. Phys. Rehabil. Med. 2017, 53, 483–491. [Google Scholar]
- Eker, H.E.; Cok, O.Y.; Aribogan, A.; Arslan, G. Management of Neuropathic Pain with Methylprednisolone at the Site of Nerve Injury. Pain Med. 2012, 13, 443–451. [Google Scholar] [CrossRef]
- Nagano, A. Treatment of brachial plexus injury. J. Orthop. Sci. 1998, 3, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Ferraresi, S.; Garozzo, D.; Basso, E.; Maistrello, L.; Lucchin, F.; Di Pasquale, P. The medial cord to musculocutaneous (MCMc) nerve transfer: A new method to reanimate elbow flexion after C5-C6-C7-(C8) avulsive injuries of the brachial plexus - Technique and results. Neurosurg. Rev. 2014, 37, 321–329. [Google Scholar] [CrossRef] [PubMed]
- Narakas, A.O.; Hentz, V.R. Neurotization in brachial plexus injuries: Indication and results. Clin. Orthop. Relat Res. 1988, 237, 43–56. [Google Scholar] [CrossRef]
- Moiyadi, A.V.; Devi, B.I.; Nair, K.P.S. Brachial plexus injuries: Outcome following neurotization with intercostal nerve. J. Neurosurg. 2007, 107, 308–313. [Google Scholar] [CrossRef]
- Oberlin, C.; Béal, D.; Leechavengvongs, S.; Salon, A.; Dauge, M.C.; Sarcy, J.J. Nerve transfer to biceps muscle using a part of ulnar nerve for C5-C6 avulsion of the brachial plexus: Anatomical study and report of four cases. J. Hand Surg. Am. 1994, 19, 232–237. [Google Scholar] [CrossRef]
- Coulet, B. Principles of tendon transfers. Hand Surg. Rehabil. 2016, 35, 68–80. [Google Scholar] [CrossRef]
- Tamai, S.; Komatsu, S.; Sakamoto, H.; Sano, S.; Sasauchi, N. Free muscle transplants in dogs, with micro surgical neurovascular anastomoses. Plast. Reconstr. Surg. 1970, 46, 219–225. [Google Scholar] [CrossRef]
- Aszmann, O.C.; Roche, A.D.; Salminger, S.; Paternosto-Sluga, T.; Herceg, M.; Sturma, A.; Hofer, C.; Farina, D. Bionic reconstruction to restore hand function after brachial plexus injury: A case series of three patients. Lancet 2015, 385, 2183–2189. [Google Scholar] [CrossRef]
- Hruby, L.A.; Gstoettner, C.; Sturma, A.; Sturma, A.; Salminger, S.; Mayer, J.A.; Aszmann, O.C. Bionic Upper Limb Reconstruction: A Valuable Alternative in Global Brachial Plexus Avulsion Injuries—A Case Series. J. Clin. Med. 2020, 9, 23. [Google Scholar] [CrossRef]
- Ahearn, B.M.; Starr, H.M.; Seiler, J.G. Traumatic Brachial Plexopathy in Athletes: Current Concepts for Diagnosis and Management of Stingers. J. Am. Acad. Orthop. Surg. 2019, 27, 677–684. [Google Scholar] [CrossRef]
- Kawasaki, T.; Ota, C.; Yoneda, T.; Maki, N.; Urayama, S.; Nagao, M.; Nagayama, M.; Kaketa, T.; Takazawa, Y.; Kaneko, K. Incidence of stingers in young rugby players. Am. J. Sports Med. 2015, 43, 2809–2815. [Google Scholar] [CrossRef] [PubMed]
- Thomas, B.E.; McCullen, G.M.; Yuan, H.A. Cervical spine injuries in football players. J. Am. Acad. Orthop. Surg. 1999, 7, 338–347. [Google Scholar] [CrossRef] [PubMed]
- Markey, K.L.; Di Benedetto, M.; Curl, W.W. Upper trunk brachial plexopathy: The stinger syndrome. Am. J. Sports Med. 1993, 21, 650–655. [Google Scholar] [CrossRef] [PubMed]
- Knapik, D.M.; Abola, M.V.; Gordon, Z.L.; Seiler, J.G.; Marcus, R.E.; Liu, R.W. Differences in cross-sectional intervertebral foraminal area from C3 to C7. Glob. Spine J. 2018, 8, 600–606. [Google Scholar] [CrossRef] [PubMed]
- Bergfeld, J.A.; Hershman, E.; Wilbourn, A. Brachial plexus injury in sports: A five-year follow-up. Am. J. Sports Med. 1988, 12, 743–744. [Google Scholar]


© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Belviso, I.; Palermi, S.; Sacco, A.M.; Romano, V.; Corrado, B.; Zappia, M.; Sirico, F. Brachial Plexus Injuries in Sport Medicine: Clinical Evaluation, Diagnostic Approaches, Treatment Options, and Rehabilitative Interventions. J. Funct. Morphol. Kinesiol. 2020, 5, 22. https://doi.org/10.3390/jfmk5020022
Belviso I, Palermi S, Sacco AM, Romano V, Corrado B, Zappia M, Sirico F. Brachial Plexus Injuries in Sport Medicine: Clinical Evaluation, Diagnostic Approaches, Treatment Options, and Rehabilitative Interventions. Journal of Functional Morphology and Kinesiology. 2020; 5(2):22. https://doi.org/10.3390/jfmk5020022
Chicago/Turabian StyleBelviso, Immacolata, Stefano Palermi, Anna Maria Sacco, Veronica Romano, Bruno Corrado, Marcello Zappia, and Felice Sirico. 2020. "Brachial Plexus Injuries in Sport Medicine: Clinical Evaluation, Diagnostic Approaches, Treatment Options, and Rehabilitative Interventions" Journal of Functional Morphology and Kinesiology 5, no. 2: 22. https://doi.org/10.3390/jfmk5020022
APA StyleBelviso, I., Palermi, S., Sacco, A. M., Romano, V., Corrado, B., Zappia, M., & Sirico, F. (2020). Brachial Plexus Injuries in Sport Medicine: Clinical Evaluation, Diagnostic Approaches, Treatment Options, and Rehabilitative Interventions. Journal of Functional Morphology and Kinesiology, 5(2), 22. https://doi.org/10.3390/jfmk5020022










