Concussion in Sports
Abstract
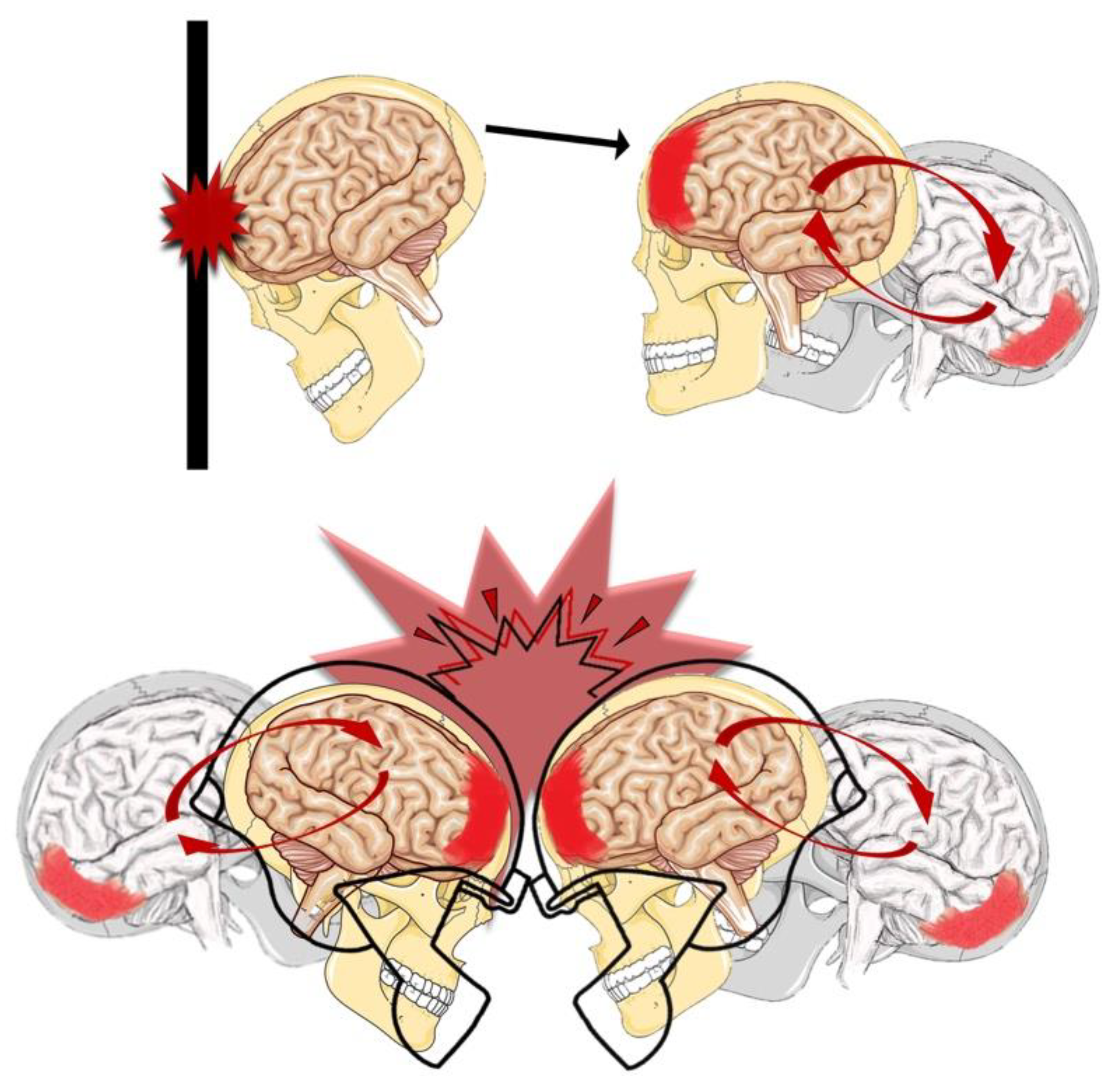
1. Introduction
2. Neurobiological Considerations
3. Postconcussive Symptomatology
4. Clinical Evaluation and Treatment
4.1. Neuropsychological Tests
4.2. Neuroimaging Techniques
4.3. Medical Community Programs
5. Future Insights
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- McCrory, P.; Feddermann-Demont, N.; Dvořák, J.; Cassidy, J.D.; McIntosh, A.; Vos, P.E.; Echemendia, R.J.; Meeuwisse, W.; Tarnutzer, A.A. What is the definition of sports-related concussion: A systematic review. Br. J. Sports Med. 2017, 51, 877–887. [Google Scholar] [CrossRef]
- McCrory, P.; Meeuwisse, W.; Dvořák, J.; Aubry, M.; Bailes, J.; Broglio, S.; Cantu, R.C.; Cassidy, D.; Echemendia, R.J.; Castellani, R.J.; et al. Consensus statement on concussion in sport-the 5(th) international conference on concussion in sport held in Berlin, October 2016. Br. J. Sports Med. 2017, 51, 838–847. [Google Scholar] [CrossRef]
- Signoretti, S.; Tavazzi, B.; Lazzarino, G.; Vagnozzi, R. The pathophysiology of concussive brain injury. In Concussion and Traumatic Encephalopathy; Victoroff, J., Bigler, E.D., Eds.; Cambridge University Press: Cambridge, UK, 2019; pp. 138–152. [Google Scholar]
- Harmon, K.G.; Clugston, J.R.; Dec, K.; Hainline, B.; Herring, S.A.; Kane, S.; Kontos, A.P.; Leddy, J.J.; McCrea, M.A.; Poddar, S.K.; et al. American Medical Society for Sports Medicine Position Statement on Concussion in Sport. Clin. J. Sport Med. 2019, 29, 87–100. [Google Scholar] [CrossRef]
- Dimou, S.; Lagopoulos, J. Toward objective markers of concussion in sport: A review of white matter and neurometabolic changes in the brain after sports-related concussion. J. Neurotraum. 2014, 31, 413–424. [Google Scholar] [CrossRef]
- Vagnozzi, R.; Signoretti, S.; Cristofori, L.; Alessandrini, F.; Floris, R.; Isgrò, E.; Ria, A.; Marziali, S.; Zoccatelli, G.; Tavazzi, B.; et al. Assessment of metabolic brain damage and recovery following mild traumatic brain injury: A multicentre, proton magnetic resonance spectroscopic study in concussed patients. Brain 2010, 133, 3232–3242. [Google Scholar] [CrossRef]
- Pearce, A.J.; Young, J.A. Hard knocks: Concussion injuries in tennis. ITF Coach. Sport Sci. Rev. 2016, 70, 5–7. [Google Scholar]
- Rueda, M.A.; Halley, W.L.; Gilchrist, M.D. Fall and injury incidence rates of jockeys while racing in Ireland, France and Britain. Injury 2010, 41, 533–539. [Google Scholar] [CrossRef]
- Connor, T.A.; Clark, J.M.; Jayamohan, J.; Stewart, M.; McGoldrick, A.; Williams, C.; Seemungal, B.M.; Smith, R.; Burek, R.; Gilchrist, M.D. Do equestrian helmets prevent concussion? A retrospective analysis of head injuries and helmet damage from real-world equestrian accidents. Sports Med. Open 2019, 5, 19. [Google Scholar] [CrossRef]
- Meehan, W.P., 3rd; Bachur, R.G. Sport-related concussion. Pediatrics 2009, 123, 114–123. [Google Scholar] [CrossRef]
- Barth, J.T.; Freeman, J.R.; Broshek, D.K.; Varney, R.N. Acceleration-Deceleration Sport-Related Concussion: The Gravity of It All. J. Athl. Train. 2001, 36, 253–256. [Google Scholar]
- Tator, C.; Starkes, J.; Dolansky, G.; Quet, J.; Michaud, J.; Vassilyadi, M. Fatal Second Impact Syndrome in Rowan Stringer, A 17-Year-Old Rugby Player. Can. J. Neurol. Sci. 2019, 4, 1–4. [Google Scholar] [CrossRef]
- Giza, C.C.; Hovda, D.A. The neurometabolic cascade of concussion. J. Athl. Train. 2001, 36, 228–235. [Google Scholar] [CrossRef]
- Giza, C.C.; Hovda, D.A. The new neurometabolic cascade of concussion. Neurosurgery 2014, 4, S24–S33. [Google Scholar] [CrossRef]
- Vagnozzi, R.; Tavazzi, B.; Signoretti, S.; Amorini, A.M.; Belli, A.; Cimatti, M.; Delfini, R.; Di Pietro, V.; Finocchiaro, A.; Lazzarino, G. Temporal window of metabolic brain vulnerability to concussions: Mitochondrial-related impairment--part I. Neurosurgery 2007, 61, 379–388. [Google Scholar] [CrossRef]
- Omalu, B. Chronic traumatic encephalopathy. Prog. Neurol. Surg. 2014, 28, 38–49. [Google Scholar]
- Mez, J.; Daneshvar, D.H.; Kiernan, P.T.; Abdolmohammadi, B.; Alvarez, V.E.; Huber, B.R.; Alosco, M.L.; Solomon, T.M.; Nowinski, C.J.; McHale, L.; et al. Clinicopathological Evaluation of Chronic Traumatic Encephalopathy in Players of American Football. JAMA 2017, 318, 360–370. [Google Scholar] [CrossRef]
- Kazemi, M.; Bogumil, M.E.; Vora, K. Concussion knowledge among Sport Chiropractic Fellows from the Royal College of Chiropractic Sports Sciences (Canada). J. Can. Chiropr. Assoc. 2017, 61, 239–252. [Google Scholar]
- Broglio, S.P.; Vagnozzi, R.; Sabin, M.; Signoretti, S.; Tavazzi, B.; Lazzarino, G. Concussion occurrence and knowledge in Italian football (soccer). J. Sports Sci. Med. 2010, 9, 418–430. [Google Scholar]
- Pearce, A.J.; Hoy, K.; Rogers, M.A.; Corp, D.T.; Davies, C.B.; Maller, J.J.; Fitzgerald, P.B. Acute motor, neurocognitive and neurophysiological change following concussion injury in Australian amateur football. A prospective multimodal investigation. J. Sci. Med. Sport 2015, 18, 500–506. [Google Scholar] [CrossRef]
- Di Pietro, V.; Lazzarino, G.; Amorini, A.M.; Signoretti, S.; Hill, L.J.; Porto, E.; Tavazzi, B.; Lazzarino, G.; Belli, A. Fusion or Fission: The Destiny of Mitochondria in Traumatic Brain Injury of Different Severities. Sci. Rep. 2017, 7, 9189. [Google Scholar] [CrossRef]
- Amorini, A.M.; Lazzarino, G.; Di Pietro, V.; Signoretti, S.; Lazzarino, G.; Belli, A.; Tavazzi, B. Metabolic, enzymatic and gene involvement in cerebral glucose dysmetabolism after traumatic brain injury. Biochim. Biophys. Acta 2016, 1862, 679–687. [Google Scholar] [CrossRef]
- Vagnozzi, R.; Signoretti, S.; Floris, R.; Marziali, S.; Manara, M.; Amorini, A.M.; Belli, A.; Di Pietro, V.; Dʼurso, S.; Pastore, F.S.; et al. Decrease in N-acetylaspartate following concussion may be coupled to decrease in creatine. J. Head Trauma Rehabil. 2013, 28, 284–292. [Google Scholar] [CrossRef]
- Vagnozzi, R.; Signoretti, S.; Tavazzi, B.; Floris, R.; Ludovici, A.; Marziali, S.; Tarascio, G.; Amorini, A.M.; Di Pietro, V.; Delfini, R.; et al. Temporal window of metabolic brain vulnerability to concussion: A pilot 1H-magnetic resonance spectroscopic study in concussed athletes—Part III. Neurosurgery 2008, 62, 1286–1295. [Google Scholar] [CrossRef]
- Hunt, T.; Asplund, C. Concussion assessment and management. Clin. Sports Med. 2010, 29, 5–17. [Google Scholar] [CrossRef]
- Finch, C.F.; Clapperton, A.J.; McCrory, P. Increasing incidence of hospitalisation for sport-related concussion in Victoria, Australia. Med. J. Aust. 2013, 198, 427–430. [Google Scholar] [CrossRef]
- Tavazzi, B.; Vagnozzi, R.; Signoretti, S.; Amorini, A.M.; Belli, A.; Cimatti, M.; Delfini, R.; Di Pietro, V.; Finocchiaro, A.; Lazzarino, G. Temporal window of metabolic brain vulnerability to concussions: Oxidative and nitrosative stresses—Part II. Neurosurgery 2007, 61, 390–395, discussion 395–396. [Google Scholar] [CrossRef]
- Childs, C.; Barker, L.A.; Gage, A.M.; Loosemore, M. Investigating possible retinal biomarkers of head trauma in Olympic boxers using optical coherence tomography. Eye Brain 2018, 10, 101–110. [Google Scholar] [CrossRef]
- Lazzarino, G.; Vagnozzi, R.; Signoretti, S.; Manara, M.; Floris, R.; Amorini, A.M.; Ludovici, A.; Marziali, S.; McIntosh, T.K.; Tavazzi, B. The Importance of Restriction from Physical Activity in the Metabolic Recovery of Concussed Brain. In Brain Injury—Pathogenesis, Monitoring, Recovery and Management; Agrawal, A., Ed.; InTech Open Access Company: Rijeka, Croatia, 2012; pp. 501–522. [Google Scholar]
- Waltzman, D.; Daugherty, J. Concussion knowledge and experience among a sample of American adults. J. Concussion 2018, 2, 1–11. [Google Scholar] [CrossRef]
- Echemendia, R.J.; Gioia, G.A. The role of neuropsychologists in concussion evaluation and management. Handb. Clin. Neurol. 2018, 158, 179–191. [Google Scholar] [CrossRef]
- Teel, E.; Gay, M.; Johnson, B.; Slobounov, S. Determining sensitivity/specificity of virtual reality-based neuropsychological tool for detecting residual abnormalities following sport-related concussion. Neuropsychology 2016, 30, 474–483. [Google Scholar] [CrossRef]
- Churchill, N.W.; Hutchison, M.G.; Graham, S.J.; Schweizer, T.A. Evaluating Cerebrovascular Reactivity during the Early Symptomatic Phase of Sport Concussion. J. Neurotrauma 2019. [Google Scholar] [CrossRef]
- Cubon, V.A.; Murugavel, M.; Holmes, K.W.; Dettwiler, A. Preliminary evidence from a prospective DTI study suggests a posterior-to-anterior pattern of recovery in college athletes with sports-related concussion. Brain Behav. 2018, 8, e01165. [Google Scholar] [CrossRef]
- Major, B.P.; Rogers, M.A.; Pearce, A.J. Using transcranial magnetic stimulation to quantify electrophysiological changes following concussive brain injury: A systematic review. Clin. Exp. Pharmacol. Physiol. 2015, 42, 394–405. [Google Scholar] [CrossRef]
- Asken, B.M.; Hack, D.C.; McCrea, M.A. The modern landscape of sport-related concussion research: Key achievements and future directions. Handb. Clin. Neurol. 2018, 158, 269–278. [Google Scholar]
- Powell, J.W. Cerebral Concussion: Causes, Effects, and Risks in Sports. J. Athl. Train. 2001, 36, 307–311. [Google Scholar]
- Howell, D.R.; Potter, M.N.; Kirkwood, M.W.; Wilson, P.E.; Provance, A.J.; Wilson, J.C. Clinical predictors of symptom resolution for children and adolescents with sport-related concussion. J. Neurosurg. Pediatr. 2019, 16, 1–8. [Google Scholar] [CrossRef]
- Haider, M.N.; Leddy, J.J.; Du, W.J.; Macfarlane, A.; Viera, K.B.; Willer, B.S. Practical Management: Brief Physical Examination for Sport-Related Concussion in the Outpatient Setting. Clin. J. Sport Med. 2018. [Google Scholar] [CrossRef]
- Ncsl National Conference of State Legislatures. Available online: http://www.ncsl.org/research/health/traumatic-brain-injury-legislation.aspx (accessed on 27 May 2019).
- Sherry, N.S.; Fazio-Sumrok, V.; Sufrinko, A.; Collins, M.W.; Kontos, A.P. Multimodal Assessment of Sport-Related Concussion. Clin. J. Sport Med. 2019. [Google Scholar] [CrossRef]
- Wallace, J.; Covassin, T.; Lafevor, M. Use of the stepwise progression return-to-play protocol following concussion among practicing athletic trainers. J. Sport Health Sci. 2018, 7, 204–209. [Google Scholar] [CrossRef]
- Slobounov, S.; Bazarian, J.; Bigler, E.; Cantu, R.; Hallett, M.; Harbaugh, R.; Hovda, D.; Mayer, A.R.; Nuwer, M.R.; Kou, Z.; et al. Sports-related concussion: Ongoing debate. Br. J. Sports Med. 2014, 48, 75–76. [Google Scholar] [CrossRef]
- Kurca, E.; Sivák, S.; Kucera, P. Impaired cognitive functions in mild traumatic brain injury patients with normal and pathologic magnetic resonance imaging. Neuroradiology 2006, 48, 661–669. [Google Scholar] [CrossRef]
- Shahim, P.; Tegner, Y.; Marklund, N.; Blennow, K.; Zetterberg, H. Neurofilament light and tau as blood biomarkers for sports-related concussion. Neurology 2018, 90, e1780–e1788. [Google Scholar] [CrossRef]
- Di Pietro, V.; Ragusa, M.; Davies, D.; Su, Z.; Hazeldine, J.; Lazzarino, G.; Hill, L.J.; Crombie, N.; Foster, M.; Purrello, M.; et al. MicroRNAs as Novel Biomarkers for the Diagnosis and Prognosis of Mild and Severe Traumatic Brain Injury. J. Neurotrauma 2017, 34, 1948–1956. [Google Scholar] [CrossRef]
- Leddy, J.J.; Willer, B. Use of graded exercise testing in concussion and return-to-activity management. Curr. Sports Med. Rep. 2013, 12, 370–376. [Google Scholar] [CrossRef]
- Leddy, J.J.; Haider, M.N.; Ellis, M.J.; Mannix, R.; Darling, S.R.; Freitas, M.S.; Suffoletto, H.N.; Leiter, J.; Cordingley, D.M.; Willer, B. Early Subthreshold Aerobic Exercise for Sport-Related Concussion: A Randomized Clinical Trial. JAMA Pediatr. 2019. [Google Scholar] [CrossRef]
- Musumeci, G.; Loreto, C.; Imbesi, R.; Trovato, F.M.; Di Giunta, A.; Lombardo, C.; Castorina, S.; Castrogiovanni, P. Advantages of exercise in rehabilitation, treatment and prevention of altered morphological features in knee osteoarthritis. A narrative review. Histol. Histopathol. 2014, 29, 707–719. [Google Scholar]
- Castorina, S.; Guglielmino, C.; Castrogiovanni, P.; Szychlinska, M.A.; Ioppolo, F.; Massimino, P.; Leonardi, P.; Maci, C.; Iannuzzi, M.; Di Giunta, A.; et al. Clinical evidence of traditional vs fast track recovery methodologies after total arthroplasty for osteoarthritic knee treatment. A retrospective observational study. Muscles Ligaments Tendons J. 2018, 7, 504–513. [Google Scholar] [CrossRef]
- Musumeci, G.; Castrogiovanni, P.; Coleman, R.; Szychlinska, M.A.; Salvatorelli, L.; Parenti, R.; Magro, G.; Imbesi, R. Somitogenesis: From somite to skeletal muscle. Acta Histochem. 2015, 117, 313–328. [Google Scholar] [CrossRef]
- Gardner, O.F.W.; Musumeci, G.; Neumann, A.J.; Eglin, D.; Archer, C.W.; Alini, M.; Stoddart, M.J. Asymmetrical seeding of MSCs into fibrin-poly(ester-urethane) scaffolds and its effect on mechanically induced chondrogenesis. J Tissue Eng Regen Med. 2017, 11, 2912–2921. [Google Scholar] [CrossRef]
- Haarbauer-Krupa, J.K.; Comstock, R.D.; Lionbarger, M.; Hirsch, S.; Kavee, A.; Lowe, B. Healthcare professional involvement and RTP compliance in high school athletes with concussion. Brain Inj. 2018, 32, 1337–1344. [Google Scholar] [CrossRef]
- Chase, D.; Schatz, P.; Smyk, N.; Franks, R.R. The stability of engagement over comprehensive neuropsychological assessment in student athletes diagnosed with sports related concussion. Dev. Neuropsychol. 2018, 43, 345–355. [Google Scholar] [CrossRef]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Musumeci, G.; Ravalli, S.; Amorini, A.M.; Lazzarino, G. Concussion in Sports. J. Funct. Morphol. Kinesiol. 2019, 4, 37. https://doi.org/10.3390/jfmk4020037
Musumeci G, Ravalli S, Amorini AM, Lazzarino G. Concussion in Sports. Journal of Functional Morphology and Kinesiology. 2019; 4(2):37. https://doi.org/10.3390/jfmk4020037
Chicago/Turabian StyleMusumeci, Giuseppe, Silvia Ravalli, Angela Maria Amorini, and Giuseppe Lazzarino. 2019. "Concussion in Sports" Journal of Functional Morphology and Kinesiology 4, no. 2: 37. https://doi.org/10.3390/jfmk4020037
APA StyleMusumeci, G., Ravalli, S., Amorini, A. M., & Lazzarino, G. (2019). Concussion in Sports. Journal of Functional Morphology and Kinesiology, 4(2), 37. https://doi.org/10.3390/jfmk4020037







