Abstract
The goal of cancer treatment is to arrest or eradicate the tumor while minimizing the often toxic effects of treatment. While oncologic diagnostics and treatments are improving and survival rates are increasing, it is critical to provide additional patient management that appears to affect long-term survival. Epidemiologic evidence suggests patients diagnosed with cancer tend to fair better after treatment when following a comprehensive rehabilitation program aimed at achieving an ideal body weight through dietary and exercise interventions while also increasing cardiorespiratory fitness, strength, mobility, neuromuscular integrity and psycho-social wellbeing. Additionally, it is now being tested whether exercise during cancer treatment and possibly prior to the start of treatment may increase post treatment outcomes by altering body weight, having direct effects on tumorigenesis, reducing oxidative stress and inflammation, and perhaps increasing chemotherapy delivery efficacy. The purpose of this review is to outline an evidence based model to evaluate cancer patients and provide guidelines for post-cancer treatment rehabilitation programs. Additionally, strategies aimed at changing lifestyle habits such as smoking and poor dietary habits will be addressed.
1. Introduction
Cancer is among the leading causes of morbidity and mortality worldwide, with approximately 14 million new cases and 8.2 million cancer related deaths in 2012 and an incidence rate expected to rise by 70% over the next two decades [1]. It is well documented that tumorgenesis and cancer treatment is associated with adverse physical and physiological changes leading to metabolic and functional modifications, inducing pathologies of the cardiac, pulmonary, neural, bone and skeletomuscular systems [2]. These alterations effect cardiorespiratory capacity (fitness), strength, body composition, and physical function including immune system integrity, peripheral neuropathy, and quality of life [3,4,5,6,7,8]. However, it is increasingly clear that prescribing exercise during and post-cancer treatment may mitigate many of these adverse changes (Table 1) by decreasing tissue inflammation contributing to tumorgenesis [9,10,11,12,13,14].

Table 1.
Late and long-term effects of cancer treatment where physical activity can have a positive impact.
Given the high prevalence, incidence and the complexity of the management of the disease, interest from Internal Medicine and specifically Sports Medicine professionals has increased proportionally especially as it relates to prescribing physical activity to offset the adverse effects of treatment. The modification of lifestyle factors post-cancer treatment has surfaced as an emerging need. Currently in Italy, the Sports and Exercise Medicine specialization is dedicated to lifestyle management specifically addressing changing behavior patterns in individuals who were previously sedentary [9]. Therefore, the purpose of this concept manuscript is to review clinical issues related to cancer treatment and to outline a model of exercise prescription for cancer patients under the Italian health care model. This system allows for an integrated approach between sports medicine specialists, oncologists, physical therapists, nutritionists, mental health professionals and personal trainers.
2. Medical Treatment Considerations and Contraindications
Here we provide a brief review of medical treatments for cancer including surgery, chemotherapy, radiotherapy and selected associated complications which include lymphedema, cardiotoxicity, chemotherapy induced peripheral neuropathy, cancer-related fatigue and general metabolic disturbances. While it is important to consider each of these factors in a comprehensive cancer rehabilitation program, it is relevant to note that cancer survivors are at elevated risk of recurrence, development of secondary cancers, cardiovascular disease and premature death since the incidence and prevalence of cancer is higher in subjects aged >55 years [15]. Normal age-related changes in physical function in addition to a sedentary lifestyle increase the risk of co-morbidities that are often seen in the cancer patient [16]. Therefore, the correct clinical approach for the cancer patient should be rooted in thorough clinical patient evaluation which ultimately will be used to determine the optimal time to begin a patient specific exercise/rehabilitation program. In the Italian model, the Sports Medicine professional should prescribe exercise and dietary guidelines in order to reduce the risk of co-morbidities, clinical complications and premature mortality. Literature supports the importance of the exercise prescription across the many types of cancer, however the majority of data in this field has been obtained mainly in breast and colon cancer survivors [17,18].
2.1. Surgery
Surgery is considered a foundation of cancer treatment and includes removal of the entire tumor/tumor bed, debulking and in some cases is used to ease cancer symptoms. Surgery is associated with pain, limited range of motion, and potentially other acute complications like infection, bleeding or thrombosis. Moreover, after surgical treatment, patients often become more sedentary due to post surgical complications. Reconstructive surgery creates additional medical complications (e.g., abdominal or latissimus tram-flap reconstruction) that should be considered by the rehabilitation specialist. As surgical treatment can be indicated at any time during the cancer continuum, long term management of the cancer patient should start with an initial period of acute rehabilitation followed by an extended period of body reconditioning following any surgical procedure.
2.2. Surgical Complications: Lymphedema
Secondary lymphedema as a result of axillary node dissection is a common complication in subjects undergoing surgical treatment for breast cancer. Complications due to lymphedema are important because they contribute to self-reported alterations of body image, decreased arm function and increase the risk to secondary infections. A recent meta-analysis suggest surgical lymphedema occurs in approximately one out of five breast cancer survivors and that women who have axillary node dissection vs. sentinel node dissection are at a fourfold increased risk of developing the condition [19].
In addition to axillary-lymph-node dissection, the greater number of lymph nodes dissected, mastectomy (partial and radical), obesity and physical inactivity are associated with increased risk of developing lymphedema. As such, strategies to increase general physical activity, increase movement in the effected-side arm, and improve body composition have been considered. Recent studies suggest that resistance exercise in women with breast cancer is both safe (when monitored appropriately), may decrease the risk of lymphedema development and clearly decreases the signs and symptoms of the condition [19,20]. In a recently published Cochrane review, the effects of manual lymphatic drainage independently and/or combined with exercise therapy have provided inconclusive results however, it was reported that shoulder mobility such as lateral movements and forward flexion were better when starting shoulder exercises earlier rather than later (after surgery) and that progressive resistance exercise therapy does not increase the risk of developing lymphedema [21]. Schmitz reported in 2010, that resistance training in breast cancer patients not only was indicated in rehabilitation programs, but also reported less lymphedema in her cohort [22]. It therefore seems reasonable, that increased movement in areas susceptible to lymphedema may actually improve clinical outcomes by increasing muscle pump and therefore effectively removing lymph from the extremities. If lymphedema is a concern, pre- and post-exercise measures of limb circumference should be taken and reported. Serious lymphedema should be immediately referred to the oncology team for further evaluation. Use of compression garments is encouraged if risk of swelling is high. Guidelines for lymphedema mitigation may be found at www.lymphedema.org medical advisory committee for the National Lymphedema Network [20].
Another complication of surgery (particularly partial mastectomy, radical mastectomy, and reconstructive surgeries for breast cancer) includes scarring and restricted mobility in the effected side of the body. This is similar to and highly related to radiotherapy scarring (see section on radiation). As a result of surgical trauma and/or radiotherapy and conservative physical therapy, it is not uncommon for breast cancer survivors to experience adhesive capsulitis or “frozen shoulder syndrome” as a result of compensatory protective mechanisms post-surgery [23]. Current strategies aimed at reducing the risk of “frozen shoulder syndrome” include progressive mobility exercises, stretching and a progressive resistance training program (see section on resistance training for cancer patients).
2.3. Radiotherapy (RT) Induced Pathology
Radiotherapy generally improves patient survival among differing cancer diagnoses, however, it can induce cardiomyopathy, mainly pericardial involvement when used in certain cancers such as, lung, breast, thyroid and Hodgkin lymphoma. This cardiomyopathy is termed radiation induced heart disease (RIHD) and is characterized by several abnormalities in the coronary vessels, pericardium, valves and may induce conduction defects [24]. Histopathological studies have demonstrated that radiation induces fibrosis of the myocardium which ultimately leads to a decrease in elasticity and distensibility of the muscle, and therefore leads to reduced diastolic function which progresses to significantly smaller ejection fractions [25,26]. This mechanism can increase the incidence of arrhythmias and potentially depress cardiac function for extended time periods. Additionally, there appears to be an acceleration of the atherosclerotic process due to sub-endothelial fibrosis, fibrosis of lymphatic channels, microvascular damage, all which can lead to a progressive deterioration of the conducting tracts or nodes in the myocardial tissue. These symptoms are often specific for the site of involvement and therefore exclusion of diseases like hypertension, coronary artery disease (CAD) or others is mandatory during the clinical assessment.
Survivors of breast cancer and Hodgkin Disease (HD) are at the greatest risk of RIHD. The mechanisms by which these abnormalities are caused in the heart are described in detail by Madan et al. [26], and are linked to increased inflammation, mediation of tumor necrosis factor (TNF), interleukins (IL), IL-1, 6, and 8 which increase further coronary artery neutrophil infiltration. It is important to note that RIHD generally occurs after a latent period of 10–15 years and is of special concern for younger cancer survivors. Because of the latent effects of RIHD, it is essential that long term follow-up and preventive clinical management of high risk patients be considered.
2.4. Chemotherapy (CT) Induced Pathology
CT is used to cure, control, or in palliation and is recognized as a main reason for increased survival rates of cancer patients. CT includes cytotoxic agents, hormonal blockers, and receptor specific targeted therapy. Depending on the drug and administration cycle, these drugs effect normal cell reproduction and often lead to myelosuppression, immunosuppression, mucositis, and alopecia and in some cases the adverse effect may be fatal [8]. In the rehabilitation setting, detailed documentation including complete blood counts of these conditions is considered essential in the development of the exercise prescription.
CT induced cardiotoxicity can be a subtle event in the cancer continuum as adverse effects are often asymptomatic for prolonged periods of time. Accordingly, CT induced pathology is diagnosed as an expression of left ventricular dysfunction and is defined as a ≥5% reduction in left ventricular ejection fraction (EF) in symptomatic patients or a ≥10% reduction in asymptomatic patients when measured from baseline with an upper limit of <55%. As the incidence of cardiotoxicity is potentially high in cancer patients, it is critical that myocardial function be assessed regularly in the clinical cardiology/sports medicine practice and that that information is conveyed to the entire rehabilitation team.
In addition to decreased EF, adverse effects of CT include heart failure, thromboembolism, severe hypertension and lethal arrhythmias which may interrupt cancer treatment and decreases in a patient’s quality of life. Among the principal CT drugs, doxorubicin, tamoxifene and trastuzumab are the most common cause of heart failure. Trastuzumab is a Her2/neu receptor inhibitor approved by the United States Federal Drug Administration but has been shown to induce myocardial dysfunction in 7%–18% of cancer patients [27]. Overexpression of Her2/neu receptor is associated with progression of malignancy in breast cancer [27]. The abnormal changes in heart’s function can escape the traditional diagnosis based on ejection fractions (i.e., volume dependent parameters), while “strain” and particularly Global Longitudinal Strain (GLS), a measure of contractility by deformation, and can be helpful in this detection in the early phase [28]. It is therefore, essential that cardiac function be evaluated as soon as is feasible after potentially cardiotoxic treatment has ended and prior to the start of the rehabilitation program.
CT induced cardiotoxicity prevention is one of the most important aspects of cardio-oncology. Considering that cardiac damage may limit optimal anticancer treatment and that several pathological myocardial changes can be irreversible, an appropriate management should include better detection of those patients at risk, the development of preventive strategies and the early treatment of cardiotoxicity when it does appear [29]. Despite the fact that there are some cardioprotective drugs (i.e., statins, beta-blockers, nitrates; angiotension converting enzyme (ACE) inhibitors) in order to reduce oxidative stress (reactive oxygen species), improve lipid profiles, decrease blood pressure and improve vascular blood flow and potentially decrease incidence of mortality and morbidity, it has been shown that physical exercise can be considered a better “polypill” for its multiple effects in protecting the heart with less adverse side effects [30]. The mechanism of action of exercise as a powerful therapeutic in reducing cardiovascular disease is linked to improved endothelial function via decreased fibrosis, increased vasodilatation effect better heart rate variability (via improved neural sensitivity in the heart), lower level of reactive oxygen species (ROS’s) and improved lipid-clot forming profiles.
2.5. Cancer Related Fatigue (CRF)
CRF is one of the most common symptoms of cancer treatments and has been reported to effect up to 80%–90% of cancer patients [6]. CRF is characterized by tiredness, weakness, and lack of energy as a result of a complex sequence of events effecting metabolism, immune function and mental wellbeing. CRF fatigue is differentiated by its general fatigue by its severity and the fact that it is often not alleviated by rest or sleep [6,31]. As a result, cancer patients with CRF also present with depression and lower quality of life (QoL) measures. The early symptoms may be undiagnosed or inadequately interpreted. Potential mechanism in the development of CRF may be related to altered metabolism due to decrease peripheral circulation, altered substrate utilization and increased inflammation. Additionally, tumor-related factors including electrolyte abnormalities, dehydration, cachexia, thrombosis/pulmonary embolism, renal failure, liver failure, hypoxia, adrenalin sufficiency, neurological deficit have been suggested as causes [6].
CRF has deleterious effects on many aspects of a patient quality of life, and for this reason a screening for fatigue at their initial clinical visit and then regularly during and after their cancer treatment is important. Among the most common and important factors related to CRF and where potential pharmacological interventions are aimed include adjusting CT dosage and/or treating anemia. For long term support, regular physical exercise has been shown to decrease both depression and fatigue [31]. Several clinical studies and meta-analyses have shown the benefits of increased physical activity/exercise on CRF, physical/emotional functioning, insomnia and overall quality of life [6,13,32].
2.6. Cancer Induced Peripheral Neuropathy (CIPN)
CIPN is a common toxicity associated with cancer treatment that is progressive, often debilitating and occasionally irreversible and has been shown to affect 30%–40% of cancer patients undergoing chemotherapy. CIPN is associated with thalidomide, vincristine, vinblastine, paclitaxel and docetaxel, protease inhibitors platinum based drugs including cisplatin, oxaliplatin and carboplatin. The condition is characterized by pain, tingling, numbness and temperature sensitivity. Axonal degeneration by any of these agents leads to akinesia, dyskinesia, allodynia, peripheral skeletal muscle weakness and indirectly effects balance and increases the risk of falling. Suspected CIPN should be evaluated clinically and site specific rehabilitation should be incorporated post treatment. Further drug therapy is often prescribed for pain relief and should be considered as part of the program.
CIPN risk factors, fall risk and prevalence in long-time cancer survivors has been well studied and mainly in breast cancer patients [33,34]. The positive effect of exercise appears to be related to reducing pain and improving physical function [14]. Mechanistically, there is emerging evidence to suggest that exercise and peripheral muscle stimulation may decreases axonal degeneration and maintain peripheral neuronal function (presumably via better blood flow in the region) [35]. Therefore, strategies for increasing overall physical activity and limb/region specific rehabilitation in cancer patients reporting CIPN should be incorporated in order to increase strength, improve balance, and quality of life presumably by decreasing the severity of pain [14].
2.7. Metabolic Disturbances
Altered whole body metabolism as a result tumor metabolism may necessitate increased caloric intake to offset cachexia (muscle wasting). Additionally, mitochondrial destruction and loss of peripheral capillary density, may shift substrate utilization as seen by increased whole body glucose production, increase glutamine, increased glycolysis and changes in the use of metabolic enzyme isoforms and increased secretion of lactate [36]. As a result of peripheral anatomical changes and/or change in metabolic substrate sources, cardiorespiratory fitness (CRF)/aerobic capacity may be affected. Other factors affecting CRF are related to physical inactivity associated with treatment, cancer related fatigue and depression. As a result, the ability to transport and effectively use oxygen in the skeletal muscle is compromised to such an extent that substrate utilization may be altered (a shift from aerobic respiration to anaerobic glycolysis) [3]. While this area of research is incomplete, it is important to consider that metabolic disturbance may affect exercise abilities of cancer patients.
3. Contraindications for Participating in Exercise Programs among Cancer Patients
Despite the fact that physical activity is suitable for most cancer survivors in stable condition, a regular medical checkup is important in order for early detection of any potential acute complications contraindicating physical activity. In the Italian health care model, standard of care is a follow up with a sports medicine professional to administer and review cardiovascular performance evaluations with electrocardiography which include 6-min walking tests (6MWT), exercise/stress tests and, if necessary, stress echocardiography. The different assessments are dependent on the clinical conditions of the presenting cancer patients. In the Italian model, the Sports Medicine professional has the expertise and training to evaluate these conditions and then direct the rehabilitation and exercise prescription plan.
It is important to monitor hematologic abnormalities (e.g., low platelets, hematocrit and hemoglobin levels, and neutrophil counts), musculoskeletal disorders (e.g., recent bone, back or neck pain; unusual muscular weakness; extreme fatigue; severe cachexia), gastrointestinal disorders (e.g., severe nausea, vomiting and diarrhea, dehydration, poor nutrition), cardiovascular disorders (e.g., chest pain, elevated resting heart rates, elevated blood pressure (both systolic and diastolic), irregular heartbeats, lymphedema), pulmonary disorders (e.g., severe difficulty breathing, coughing/wheezing), and neurological disorders (e.g., decline in cognitive status, dizziness/lightheadedness, disorientation, blurred vision, increased postural instability) [37]. A comprehensive list of contraindications to exercise testing and training is included in Table 2. One specific contraindication not listed below is associated with radiotherapy treatment whereby pool swimming is contraindicated because of the increased risk of potential infections and burn site irritation.

Table 2.
Contraindications and precautions to the exercise prescription for cancer.
3.1. Medical Assessment
The Italian model for cancer rehabilitation for complete lifestyle restoration is a multidisciplinary model incorporating the Sports Medicine physician first that interacts with oncology, eventually cardiology, internal medicine or primary care, and rehabilitation medicine, and is supported by ancillary health care professionals including physical therapists, occupational therapists, nutritionists and exercise trainers.
Entry of a patients for an “exercise is medicine program” is initiated by oncologists, while the evaluation and the assessment of the program needs a specific competence in Sports Medicine where the culture of exercise and an understanding of the acute and chronic impact of sports training in patients is well known. Following referral from the oncology team, regular follow- up by the Sports Medicine physician is mandatory especially for the potential long term damage as a result of chemo- and radio-therapy.
Post cancer treatment, standard of care for the cancer patient includes standard echocardiography and more recently by the use of sophisticated software packages such as speckle tracking which is used to investigate heart deformation parameters in order to classify the extent of cardiac toxicity. Additional stress echocardiography may be necessary in order to evaluate myocardial response to exercise and possibly aid in the exercise prescription for the patients. These symptom limited graded exercise tests includes blood pressure monitoring and termination at 85% age-predicted maximal heart rate. Based on results of the stress echocardiogram, intensity of the exercise can be established at lower heart rate values especially if the rating of perceived exertion during testing is not proportional to the actual work output. Should ECG (Electrocardiogram) or wall abnormalities be found to the extent that exercise is contraindicated, the patient is evaluated by the Sports Medicine team (because of their clinical understanding of the cardiac-exercise connection) and re-scheduled for follow up.
3.2. Other Assessments
Body composition should be assessed to estimate percentage of fat and used to calculate fat free and fat mass. In the hospital setting dual-X-ray absorptiometry is considered a gold standard while body composition can be estimated in the out-patient clinical setting through skinfold measures, bio-electrical impedance, near-infra-red spectrometry, or plethysmography. It is beyond the scope of this review to review the strength and weaknesses of each of these body composition tests. It is however, an important measure as reaching an ideal body size and composition is critical for long term survival [38].
Strength evaluation: In the clinical setting, strength is often assessed using hand grip dynamometry. Standards have been published by the American College of Sports Medicine [39].
Flexibility evaluation: In the clinical setting flexibility is often assessed using the sit and reach test. Standards have been published by the American College of Sports Medicine [39].
It should be noted that post-surgical treatment, physical therapists may determine strength, flexibility and range of motion using practice specific assessments and normative data which are better representative of their condition compared to normative data compiled on healthy individuals.
Quality of Life evauation: In the clinical setting, there are a number of validated quality of life assessment tools. The 36-item short form health survey (SF-36) and the functional assessment of cancer therapy-general (FACT-G) are commonly used [40,41].
3.3. Exercise Guidelines
Exercise guidelines for cancer survivors have been previously published [13] and are the basis of our recommendations post-cancer treatment. The efficacy and safety of exercise testing and exercise training post-cancer treatment has been previously published [42] and testing and training appear relatively safe. In Europe and also in Italy, where the characteristics of the general population are different from the American counterparts, the management of cancer survivors is relatively new. The approach presented here has not been validated but it is closely related to the ACSM guidelines. Recently exercise during cancer treatment has been suggested to slow the overall rate of physiologic decline and maintain better quality of life [43]. Currently, there are no validated guidelines for exercise during cancer treatment and practitioners are encouraged to proceed cautiously until further data has been scrutinized.
There is clear relationship between cardiorespiratory fitness (CRF) and mortality which suggests that those with the highest CRF have a significantly lower risk of premature death to the cancer itself or other age-related co-morbidities [44]. Therefore, if the health of the given patient is relatively good, they should be encouraged to do more than the current exercise minimums. Given the importance of the oxygen cascade and the relationship of CRF and cancer related death, one primary goal of cancer rehabilitation is to arrest the decline in aerobic fitness during treatment and then restore aerobic fitness to pre-diagnosis levels with an ultimate goal of improving aerobic capacity above pre-diagnosis levels.
Cancer survivors of all cancer-types and at all stages of cancer have been shown to increase aerobic capacity when given the appropriate overload [13]. From a scientific perspective, the aim is to achieve 500–1000 Metabolic Equivalent of Task (MET) minutes of activity per week where a MET is the metabolic equivalent of energy use. For example, 1 MET is considered the energy used while resting and is equivalent to an oxygen consumption of ~3.5 mL·O2·kg−1·min−1. A MET per minute is defined as the level of intensity x time (minute) doing the activity. For example: The MET/minutes for walking at 4 km·h−1 (MET level = 2.9) × 30 min = 87 MET/minutes [45].
In order to achieve the 500–1000 MET/minute per week the following guidelines have been validated. Cancer patients should set as a goal of at least 150 min (2.5 h) a week of moderate-intensity or 75 min (1.25 h) a week of vigorous-intensity aerobic physical activity, or an equivalent combination of moderate- and vigorous-intensity aerobic activity. Aerobic activity should be performed in episodes of at least 10 min, and preferably, it should be spread throughout the week. When older adults cannot do 150 min of moderate-intensity aerobic activity a week because of chronic conditions, they should be as physically active as their abilities and conditions allow. For additional and more extensive health benefits, cancer patients (if able) should increase their aerobic physical activity to 300 min (5 h) a week of moderate-intensity, or 150 min a week of vigorous-intensity aerobic physical activity, or an equivalent combination of moderate- and vigorous-intensity activity. Additional health benefits are gained by engaging in physical activity beyond this amount [45].
3.4. Exercise Intensity
Exercise intensity levels should be established based on clinical evaluation to ensure overall patient safety which should include physician assessment via graded exercise testing with electrocardiography or echocardiography. Heart rate is currently the preferred method to establish exercise intensity while many researchers have had success using the CR10 or Borg rating of perceived exertion scale (1–10).
The current exercise guidelines for cancer patients suggest an intensity level of moderate-to-vigorous, which is defined as 40%–60% of maximal oxygen uptake reserve (VO2 reserve) or heart rate reserve (HRR) [13]. We will only consider heart rate reserve for this discussion. However, it is important to emphasize that in Italy, the current model includes both the calculated HR intensities and CR10 scale.
HRR is determined as the heart rate maximum (HRmax) − heart rate rest (HRrest). HRmax can be estimated from the equation 208 bpm − 70% × age or ideally measured in a clinical setting [46]. Many times when completing a symptom limited cardiopulmonary exercise test, HRmax is not achieved and therefore peak heart rate (HRpeak) is used as an upper limit for HRR calculations. It should be noted that establishing exercise intensity based on HRpeak may result in underestimate of exercise intensity needed for improvements in fitness and the clinician will have to use best judgement to establish an upper HR limit for each cancer patient. It has also been reported in breast cancer survivors that prescribing exercise intensity based on HRR may result in higher exercise intensity than intended and therefore should be used conservatively [47]. Vigorous exercise is defined as ≥60% HRR or VO2 reserve or and it is suggested for safety concerns not to exceed 85% of HRR. In the current Italian model, maximal exercise testing is terminated at 85% of an age-predicted HRmax. HRR reserve and exercise intensities are subsequently determined from these results.
3.5. Practical Application
At the initiation of an exercise program for a cancer patient who has been previously sedentary, it may be necessary to begin with light activity and then proceed to moderate-to-vigorous exercise. In general, light activity is defined as 1.1 up to 3.0 MET, Moderate activity is defined as 3.0 up to 6.0 MET and Vigorous activity is defined as more than 6.0 MET. (Table 3).

Table 3.
Intensity the aerobic exercise based on MET level, Heart Rate Reserve, Rating of Perceived Exertion (RPE) with examples.
From a relative intensity level, use of the CR10 or Modified Borg scale works well. Moderate intensity activity is a level of effort of 6 or below on a 1–10 scale while vigorous intensity is a 7–8 on the 1–10 scale.
Currently, effective aerobic conditioning programs appear to incorporate some type low level activity followed by intermittent high intensity exercise in significantly shorter durations. These aerobic training sessions are typically prescribed on alternating days throughout the week. This alternating level of high intensity/low intensity allows for significant overload and stimulus for adaptation while proving very safe and effective [48,49,50]. Note that in the initial phase of conditioning at low intensity levels, it is not necessary to supervise the exercise sessions but higher intensity exercise sessions may need supervision by a health professional.
3.5.1. Modality
Walking is typically the preferred modality of aerobic activity but any and all modalities should be considered for the cancer patient with thought given to surgical limitations, radiation complications, and perhaps anatomic limitations (i.e., cycling for prostate patients).
3.5.2. Anaerobic-Resistance Training
Cancer treatments affect bone mineral density, muscle mass integrity and possible neuromuscular function. It is generally agreed upon that some type of resistance training program be prescribed for the cancer population. The independent effects of strength training in cancer survivors are generally such that strength and to a lesser degree functionality may be increased. In general, maximal strength gains in cancer patients have been on average 20%–50% [5]. It is, therefore, recommended that adult cancer patients should do muscle-strengthening activities that are moderate or high intensity and involve all major muscle groups on two or more days a week, as these activities provide additional health benefits.
There are a number of strategies to prescribe gym and home based exercise for cancer patients and usually a combination utilizing minimal equipment is preferred. It is recommended, however, that cancer patients be taught (through physical therapy or certified cancer exercise specialists) the importance of posture, mobility, segment stability and whole body stability. Many individuals both healthy and those with cancer have poor biomechanics or movement patterns in the weight room. While single joint exercises are safe and effective for increasing strength, often the movement patterns are not similar to normal activities of daily living. Therefore, a program that emphasizes basic movement and proper alignment appears to be a better strategy for increasing performance on activities of daily living. For instance, a woman who has undergone chemotherapy, radiation treatment, and surgery for breast cancer, requires strength training to improve posture (i.e., neutral spine position), upper body range of motion/flexibility (or mobility) on both sides, stability in the shoulder girdle (segment stability), and muscular strength and endurance (in order to participate in normal activities of daily living).
Because most cancer clients are 50+ years [16], promoting improved posture, greater mobility of the hips and upper body musculature, and spinal stability along with neuromuscular “re-education”, movement patterns are enhanced (and perhaps corrected) and increases in general strength have been recorded. Improved movement patterns allow the older adult to exercise and move/walk safely while avoiding falls and potential future orthopedic complications (lordosis, cervical spine, limited range of motion). It also allows patients to engage safely in other aerobic activities and progress toward greater resistance workloads [51]. Increases in load may be achieved by simply increasing the weight lifted for a particular muscle group or the individual can increase load by engaging in more proprioceptive type training (single leg squats rather than two-footed squats with a barbell).
As the cancer patient is typically older, it is recommended that adults do exercises that maintain or improve balance if they are at risk of falling [49]. This type of resistance training includes specific balance training, agility and neuromuscular activation. For example, single leg balance on an unstable platform (with safety precautions in place) is an ideal method to increase strength, balance, and facilitate neuromuscular feedback and integration. In general, a simple approach to starting a cancer patient on a resistance training program involves these 10 warm up exercises followed by progressions determined by trained exercise professionals.
3.5.3. Intensity
Engaging cancer patients in resistance training exercises based on 1-repetition maximum testing is problematic as safety is often compromised and assessment procedures are not uniformly followed. The experienced therapist should start cancer patients with body weight movements practiced until form is lost. The goal is to progress to two sets of a specific exercise at perfect form for 10 repetitions emphasizing correct movement patterns. The load can then be increased either by increasing number of sets, number of repetitions, and/or increasing load according to this standard. Once basic movement patterns have been learned, advancement to resistance machines and whole body exercise should be encouraged.
Note: For frail, very old and those with co-morbidities such as Alzheimer’s, Parkinson’s, or other CNS pathologies, single joint weight machines (cable, Nautilus, Cybex, etc.) are ideal.
3.5.4. Flexibility
It is recommended that cancer patients participate in active stretching routines as part of a pre-exercise warm up. In the physical therapy setting, assisted stretching and modalities aimed at decreasing rigidity are standard of care. Surgical complications and fibrosis from radiotherapy should be considered for all resistance exercises. Sufficient mobility must be obtained before heavy lifting should occur. Rather than simply prescribing a linear aerobic warm up (like treadmill walking or cycle ergometry) prior to resistance training, dynamic movements emphasizing muscle activation are preferred. This type of active stretching is preferably to traditional static stretching.
Finally, strength training workouts should incorporate agility work (rapid foot movements, dance, single leg balance exercises, ladder exercises, foot work agility exercises) following the strength training component. Below (Table 4) is a simplified weekly training plan incorporating resistance and aerobic training.

Table 4.
Sample weekly exercise program for cancer patients.
3.5.5. Nutrition
Overweight and obesity are very common after CT treatment and increased fat mass has been associated with inflammation and higher rates of cancer recurrence. As body weight management is critical for long-term survival after cancer treatment, practitioners should address changes in dietary patterns to ensure adequate nutrition and to initiate lifestyle changes in order to lose and maintain body weight [38,52,53]. As part of a comprehensive cancer rehabilitation program, at minimum a three day dietary should be administered and reviewed by a nutritionist. In Italy, nutrition advice is offered after completion of the dietary recall and prior to the entry into the rehabilitation program. Failure to adopt healthy dietary practices after the initial consultation is followed by more specific recommendation when needed.
Depending on specific cancer type and associated treatment plan (surgery, chemotherapy, radiation), there are a number of adverse physical complications that may be corrected to some degree by sound eating patterns or a better nutritional strategy. These complications can range from vitamin deficiencies due to malabsorption, sarcopenia, osteopenia/osteoporosis, anemia and immunosuppression. Additionally, cancer treatment may cause an inability to eat because of
- Loss of appetite
- Sore mouth or throat
- Dry mouth
- Dental and gum problems
- Changes in taste or smell
- Nausea
- Vomiting
- Diarrhea
- Constipation
- Cancer related fatigue
- Depression
It should be noted that a recent Cochrane review has indicated that increased dietary anti-oxidant supplements may increase mortality risk [54]. It is, therefore, suggested that cancer patients receive their vitamins and anti-oxidants from whole foods rather than dietary supplements.
As a result of an inability to eat well during and after cancer treatment, energy levels may be decreased. Along with a decrease in physical activity and loss of muscle mass, changes in body composition may result (increased percentage of fat, increased body weight, increased body mass index). The “cancer treatment—poor nutrition—decreased physical activity” triad causes a downward spiral in general health and may complicate and/or prolong recovery during the cancer rehabilitation process.
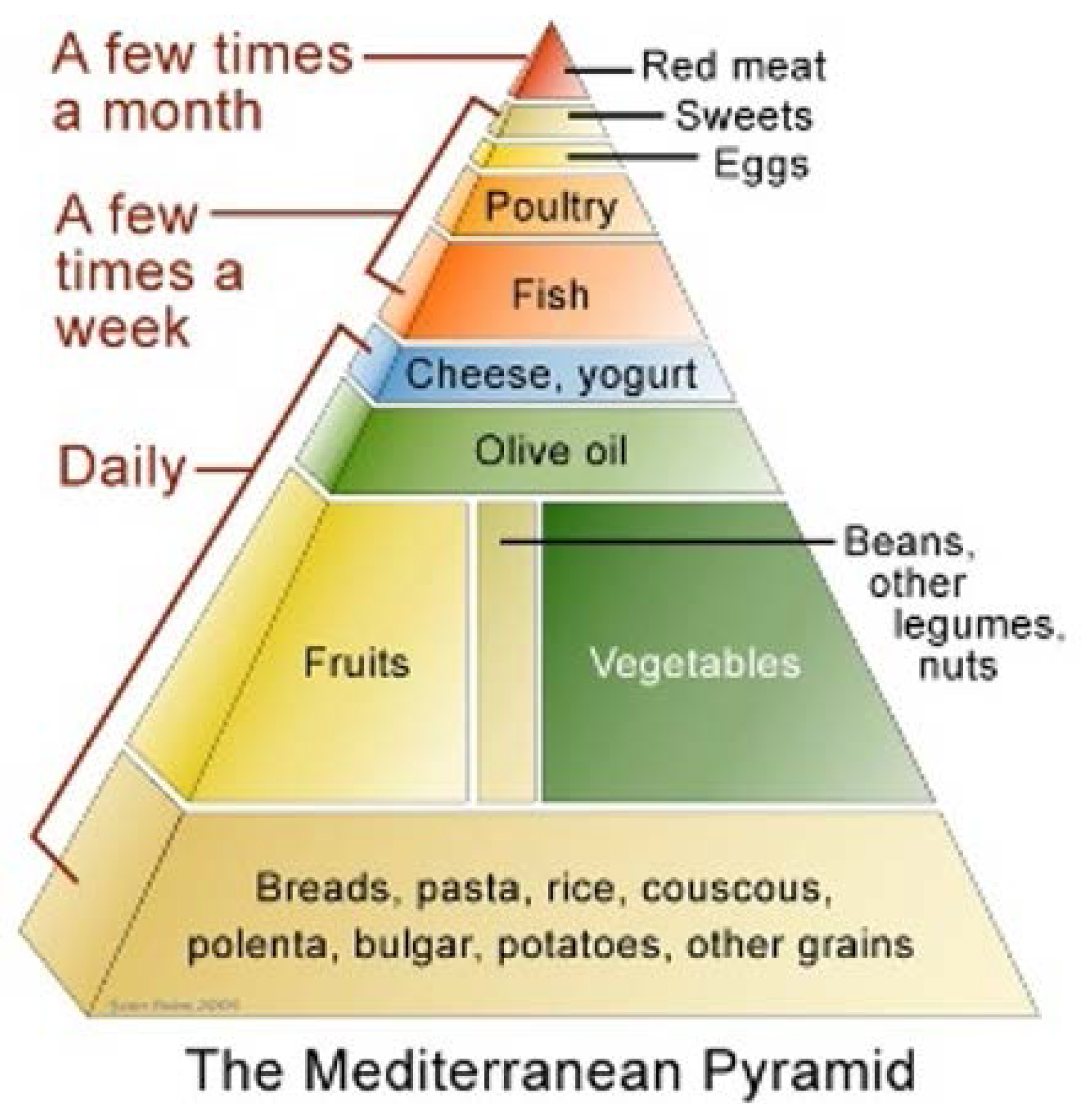
Current research indicates that a Mediterranean diet promotes weight loss in obese subjects which was maintained for over two years and significantly reduces the risk for cardiovascular disease [53]. The traditional Mediterranean diet (Figure 1) includes an abundance of plants including fruits and vegetables, whole grains, breads, legumes, potatoes, nuts and seeds [52]. Additional olive oil use is encouraged, along with moderate amounts of fish, poultry, dairy and eggs. Red meat is eaten rarely.
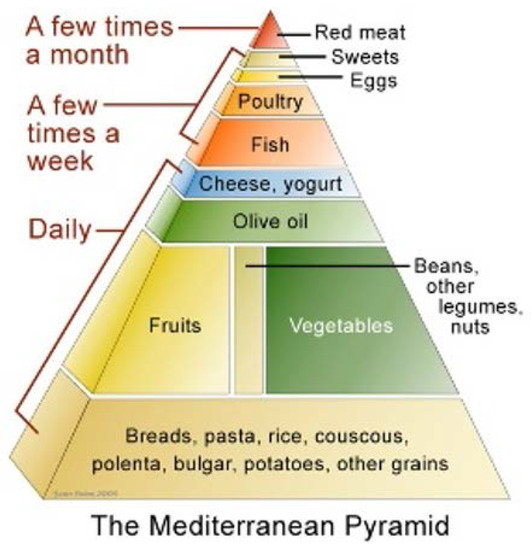
Figure 1.
Pyramid of Mediterranean diet.
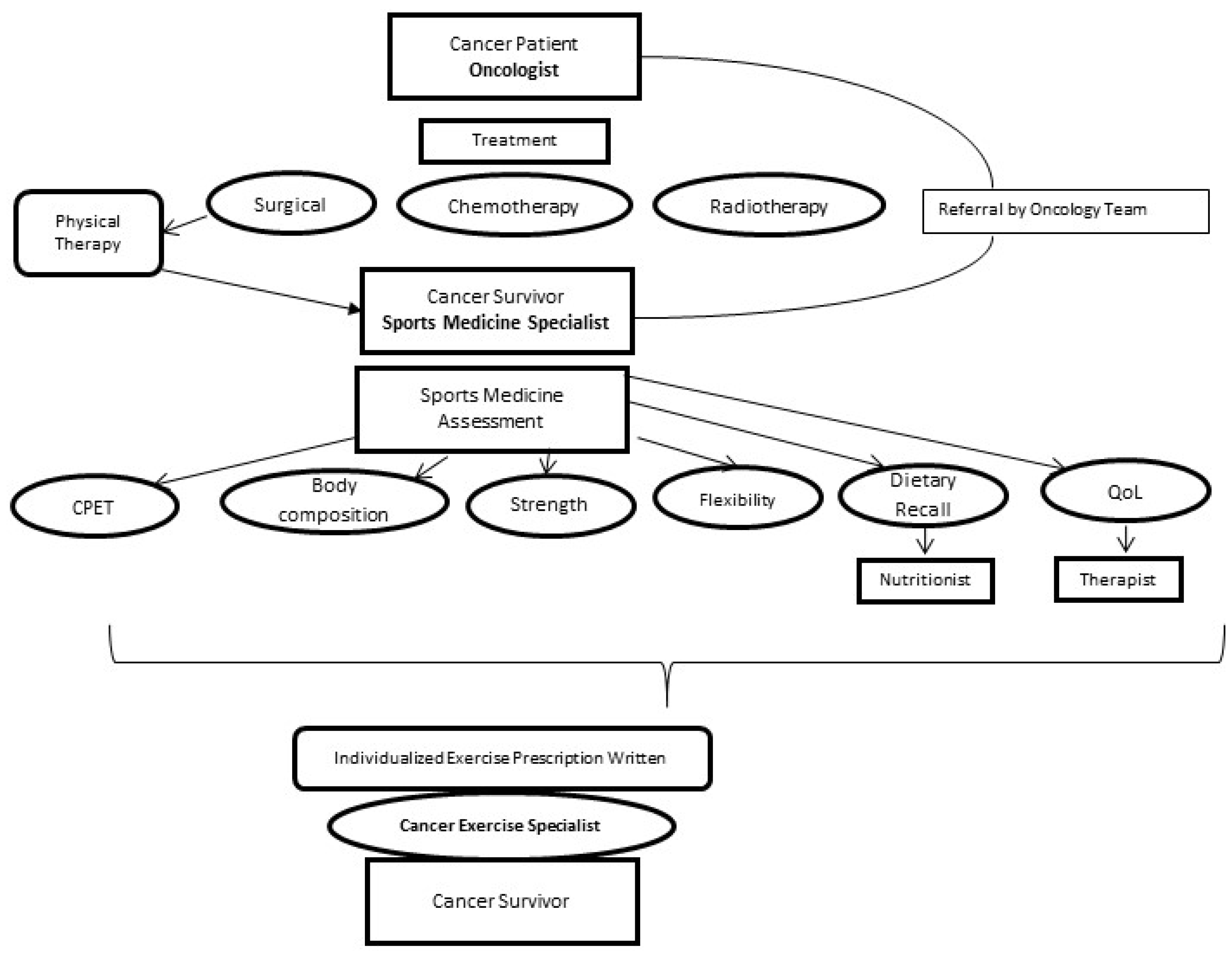
3.6. How to Approach the Patient Flow Chart, Italian Model
Below is a suggested flow chart (Figure 2) for the cancer patient transitioning to cancer survivor in the Italian model. Feedback from all team members should be coordinated through the Sports Medicine Specialist. Exercise prescription including frequency, intensity, type, duration (time) (FITT) and progression is dependent on pre-diagnosis physical activity level, treatment complications, and motivation. The main goal is to achieve 150 min of accumulated activity per week at a moderate to vigorous intensity. Additionally, resistance training emphasizing strength, endurance, balance and coordination should be prescribed twice weekly.
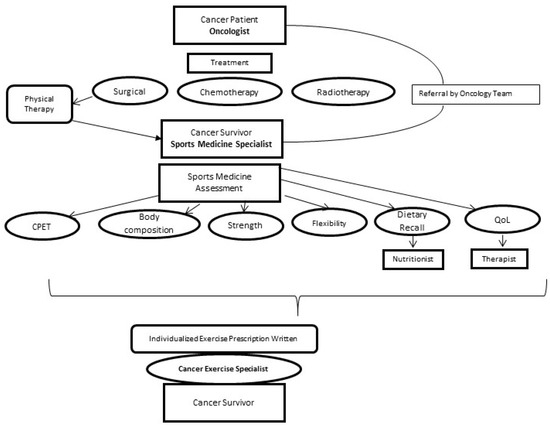
Figure 2.
Flow chart for transition from cancer patient to cancer survivor and rehabilitation considerations. CPET: cardiopulmonary exercise test with Electrocardiogram or Echocardiography; Body: Body composition analysis (BIK or skinfolds); Flexibility: Sit and Reach; Strength: Hand Grip Dynamometry; Dietary: Three day dietary recall and analysis; QoL: Quality of life questionnaire.
4. Conclusions
The goal of this article is to present evidence based medicine indicating the exercise and dietary intervention for cancer survivors should be part of a comprehensive cancer treatment and rehabilitation plan. Physical inactivity, obesity, cigarette smoking, alcohol consumption, and illicit drug use and altered sleep habits are modifiable risk factors for the prevention of cancer and should considered in a comprehensive cancer survivor plan. This review focuses on physical activity and dietary changes. Practitioners should be aware of the adverse health effects of surgery, chemotherapy, radiotherapy including altered immune system responses, anemia, CIPN, cancer related fatigue, and loss of cardiorespiratory fitness.
The Sports Medicine Medical Doctor with the support of other professionals should make the determination when to start an exercise program, the progression, and intensity of the exercise and a plan designed to avoid the complications as a result of treatment. Receiving feedback from the entire team, will ultimately contribute to the correct management of the patient.
The primary goal of the rehabilitation program should be to achieve ideal weight managements, with a correct body composition in terms of fatty mass and fat free mass, increase cardiorespiratory fitness, muscular strength and endurance and preserve neuromuscular integrity. Dietary strategies that include mild caloric restriction and a traditional Mediterranean diet should be encouraged. Prior to starting an exercise program post treatment, all cancer patients should have a medical evaluation including cardiopulmonary testing to ensure there are no latent cardiotoxic abnormalities due to treatment itself.
Author Contributions
Laura Stefani, Giorgio Galanti and Riggs Klika have conceived the manuscript; Laura Stefani and Riggs Klika have elaborated and written the manuscript; Giorgio Galanti has approved the final version of the study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Stewart, B.W.; Wild, C.P. (Eds.) World Cancer Report 2014; International Agency for Research on Cancer: Lyon, France, 2014.
- Hewitt, M.; Greenfield, S.; Stovall, E. (Eds.) From Cancer Patient to Cancer Survivor: Lost in Transition; National Academies Press: Washington, DC, USA, 2006.
- Jones, L.W.; Eves, N.D.; Haykowsky, S.; Freeland, S.J.; Mackey, J.R. Exercise intolerance in cancer and the role of exercise therapy to reverse dysfunction. Lancet Oncol. 2009, 10, 598–605. [Google Scholar] [CrossRef]
- Gould, D.W.; Lahart, I.; Carmichael, A.R.; Koutedakis, Y.; Metsios, G.S. Cancer cachexia prevention via physical exercise: Molecular mechanisms. J. Cachexia Sarcopenia Muscle 2012, 4, 111–124. [Google Scholar] [CrossRef] [PubMed]
- Hanson, E.D.; Wagoner, C.W.; Anderson, T.; Battaglini, C.L. The independent effects of strength training in cancer survivors: A systematic review. Curr. Oncol. Rep. 2016, 18, 31–49. [Google Scholar] [CrossRef] [PubMed]
- Hofman, M.; Ryan, J.L.; Figueroa-Moseley, C.D.; Jean-Pierre, P.; Morrow, G.R. Cancer related fatigue: The scale of the problem. Oncologist 2007, 12, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Bao, T.; Basal, C.; Seluzicki, C.; Li, S.Q.; Seidman, A.D.; Mao, J.J. Long-term chemotherapy-induced peripheral neuropathy among breast cancer survivors: Prevalence, risk factors, and fall risk. Breast Cancer Res. Treat. 2016, 159, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Minami, M.; Matsumoto, S.; Horiuchi, H. Cardiovascular side-effects of modern cancer therapy. Circ. J. 2010, 74, 1779–1786. [Google Scholar] [CrossRef] [PubMed]
- Stefani, L.; Petri, C.; Mascherini, G.; Galanti, G. Lifestyle intervention in surviving cancer patients. J. Func. Morphol. Kinesiol. 2016, 1, 48–53. [Google Scholar] [CrossRef]
- Albrecht, T.A.; Taylor, A.G. Physical activity in patients with advanced-stage cancer: A systematic review of the literature. Clin. J. Oncol. Nurs. 2012, 16, 293–300. [Google Scholar] [CrossRef] [PubMed]
- Conn, V.S.; Hafdahl, A.R.; Porock, D.C.; McDaniel, R.; Nielsen, P.J. A meta-analysis of exercise interventions among people treated for cancer. Support. Care Cancer 2006, 14, 699–712. [Google Scholar] [CrossRef] [PubMed]
- Speck, R.M.; Courneya, K.S.; Masse, L.C.; Duval, S.; Schmitz, K.H. An update of controlled physical activity trials in cancer survivors: A systematic review and meta-analysis. J. Cancer Surviv. 2010, 4, 87–100. [Google Scholar] [CrossRef] [PubMed]
- Schmitz, K.H.; Courneya, K.S.; Matthews, C.; Demark-Wahnefried, W.; Galvão, D.A.; Pinto, B.M.; Irwin, M.L.; Wolin, K.Y.; Segal, R.J.; Lucia, A.; et al. American College of Sports Medicine roundtable on exercise guidelines for cancer survivors. Med. Sci. Sports Exerc. 2010, 42, 1409–1426. [Google Scholar] [CrossRef] [PubMed]
- Wonders, K.Y.; Reigle, B.S.; Drury, D.G. Treatment strategies for chemotherapy-induced peripheral neuropathy: Potential role of exercise. Oncol. Rev. 2010, 4, 117–125. [Google Scholar] [CrossRef]
- Yancik, R. Population aging and cancer: A cross-national concern. Cancer J. 2005, 11, 437–441. [Google Scholar] [CrossRef] [PubMed]
- Liberman, K.; Forti, L.N.; Beyer, I.; Bautmans, I. The effects of exercise on muscle strength, body composition, physical functioning and the inflammatory profile of older adults: A systematic review. Curr. Opin. Clin. Nutr. Metab. Care 2016, 20, 30–53. [Google Scholar] [CrossRef] [PubMed]
- Meneses-Echavez, J.F.; Correa-Bautista, J.E.; Gonzalez-Jimenez, E.; Schmidt Rio-Valle, J.; Elkins, M.R.; Lobelo, F.; Ramirez-Velez, R. The effect of exercise training on mediators of inflammation in breast cancer survivors: A systematic review with meta-analysis. Cancer Epidemiol. Biomark. Prev. 2016, 25, 1009–1017. [Google Scholar] [CrossRef] [PubMed]
- Van Blarigan, E.L.; Meyerhardt, J.A. Role of physical activity and diet after colorectal cancer diagnosis. J. Clin. Oncol. 2015, 33, 1825–1834. [Google Scholar] [CrossRef] [PubMed]
- DiSipio, T.; Rye, S.; Newman, B.; Hayes, S. Incidence of unilateral arm lymphedema after breast cancer: A systematic review and meta-analysis. Lancet Oncol. 2013, 14, 500–515. [Google Scholar] [CrossRef]
- NLN Medical Advisory Committee, National Lymphedema Network. Position Statement on the Diagnosis and Treatment of Lymphedema. Available online: www.lymphnet.org (accessed on 1 January 2017).
- Ezzo, J.; Manheimer, E.; McNeely, M.L.; Howell, D.M.; Weiss, R.; Johansson, K.I.; Bao, T.; Bily, L.; Tuppo, C.M.; Williams, A.F.; et al. Manual lymphatic drainage for lymphedema following breast cancer treatment. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef]
- Schmitz, K.H.; Ahmed, R.L.; Troxel, A.B.; Cheville, A.; Lewis-Grant, L.; Smith, R.; Bryan, C.J.; Williams-Smith, C.T.; Chittams, J. Weight lifting for women at risk for breast cancer-related lymphedema: A randomized trial. JAMA 2010, 304, 2699–2705. [Google Scholar] [CrossRef] [PubMed]
- Getz, C.L.; Phillips, J.; Skirven, T.M.; Osterman, A.L.; Fedorczyk, J.M.; Adadio, P.C. Adhesive capsulitis. In Rehabilitation of the Hand and Upper Extremity, 6th ed.; Elsevier Mosby: Philadelphia, PA, USA, 2011; Chapter 89. [Google Scholar]
- Taunk, N.K.; Haffty, B.G.; Kostis, J.B.; Goyal, S. Radiation-induced heart disease: Pathologic abnormalities and putative mechanisms. Front. Oncol. 2015, 5, 39. [Google Scholar] [CrossRef] [PubMed]
- Zinzani, P.L.; Gherlinzoni, F.; Piovaccari, G.; Frezza, G.; Bendandi, M.; Ferretti, R.M.; Barbieri, E.; Fiacchini, M.; Babini, L.; Magnani, B.; et al. Cardiac injury as late toxicity of mediastinal radiation therapy for Hodgkin’s disease patients. Haematologica 1996, 81, 132–137. [Google Scholar] [PubMed]
- Madan, R.; Benson, R.; Sharma, D.N.; Julka, P.K.; Rath, G.K. Radiation induced heart disease: Pathogenesis, management and review literature. J. Egypt. Natl. Cancer Inst. 2015, 4, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Slamon, D.J.; Clark, G.M.; Wong, S.G.; Levin, W.J.; Ullrich, A.; McGuire, W.L. Human breast cancer: Correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science 1987, 235, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Stefani, L.; Pedrizzetti, G.; Galanti, G. Clinical application of 2D speckle tracking strain for assessing cardio-toxicity in oncology. J. Func. Morphol. Kinesiol. 2016, 1, 343–354. [Google Scholar] [CrossRef]
- Altena, R.; Perik, P.J.; van Veldhuisen, D.J.; de Vries, E.G.; Gietema, J.A. Cardiovascular toxicity caused by cancer treatment: Strategies for early detection. Lancet Oncol. 2009, 10, 391–399. [Google Scholar] [CrossRef]
- Fiuza-Luces, C.; Garatachea, N.; Berger, N.A.; Lucia, A. Exercise is the real polypill. Physiology 2013, 28, 330–358. [Google Scholar] [CrossRef] [PubMed]
- Mustian, K.M.; Morrow, G.R.; Carroll, J.K.; Figueroa-Moseley, C.D.; Jean-Pierre, P.; Williams, G.C. Integrative nonpharmacologic behavioral interventions for the management of cancer-related fatigue. Oncologist 2007, 12, 52–67. [Google Scholar] [CrossRef] [PubMed]
- Morten, Q.; Lis Adamsen, L.; Rorth, M.; Laursen, J.H.; Christensen, K.B.; Langer, S.W. The impact of a multidimensional exercise intervention on physical and functional capacity, anxiety, and depression in patients with advanced-stage lung cancer undergoing chemotherapy integrative cancer therapy. Integr. Cancer Ther. 2015, 14, 341–349. [Google Scholar]
- Balducci, S.; Iacobellis, G.; Parisi, L.; di Biase, N.; Calandriello, E.; Leonetti, F.; Fallucca, F. Exercise training can modify the natural history of diabetic peripheral neuropathy. J. Diabetes Complicat. 2006, 20, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Stubblefield, M.D.; Burstein, H.J.; Burton, A.W.; Custodio, C.M.; Deng, G.E.; Ho, M.; Junck, L.; Morris, G.S.; Paice, J.A.; Tummala, S.; et al. NCCN task force report: Management of neuropathy in cancer. J. Natl. Compr. Cancer Netw. 2009, 7, 1–26. [Google Scholar]
- Park, J.S.; Kim, S.; Hoke, A. An exercise regimen prevents development paclitaxel induced peripheral neuropathy in a mouse model. J. Peripher. Nerv. Syst. 2015, 20, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Coller, H.A. Is cancer a metabolic disease? Am. J. Pathol. 2014, 184, 4–17. [Google Scholar] [CrossRef] [PubMed]
- McNeely, M.L.; Peddle, C.J.; Parilment, M.; Courneya, K.S. Cancer rehabilitation: Recommendations for integrating exercise programming in a clinical setting. Curr. Cancer Ther. Rev. 2006, 2, 251–260. [Google Scholar] [CrossRef]
- McTiernan, A. (Ed.) Cancer Prevention and Management through Exercise and Weight Control; Taylor and Francis: Boca Raton, FL, USA, 2006.
- Schmitz, K.; Courneya, K.; Matthews, C.; Demark-Wahnefried, W.; Galvao, D.A.; Pinto, B.M.; Irwin, M.L.; Wolin, K.Y.; Segal, R.J.; Lucia, A.; et al. ACSM’s Guidelines for Exercise Testing and Prescription, 9th ed.; Wolters Kluwer: Baltimore, MD, USA, 2014. [Google Scholar]
- Ware, J.E., Jr.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Cella, D.F.; Tulsky, D.S.; Gray, G.; Sarafian, B.; Linn, E.; Bonomi, A.; Silberman, M.; Yellen, S.B.; Winicour, P.; Brannon, J.; et al. The functional assessment of cancer therapy scale: Development and validation of the general measure. J. Clin. Oncol. 1993, 11, 570–579. [Google Scholar] [PubMed]
- Jones, L.W.; Eves, N.D.; Mackey, J.R.; Peddle, C.J.; Haykowsky, M.; Joy, A.A.; Courenya, K.S.; Tankel, K.; Spratlin, J.; Reiman, T. Safety and feasibility of cardiopulmonary exercise testing in patients with advance cancer. Lung Cancer 2007, 55, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Van Waart, H.; Stuiverm, M.M.; van Harten, W.H.; Geleijn, E.; Kieffer, J.M.; Buffart, L.M.; de Maaker-Berkof, M.; Boven, E. Effect of low-intensity physical activity and moderate—To high-intensity physical exercise during adjuvant chemotherapy on physical fitness, fatigue, and chemotherapy completion rates: Results of the PACES randomized clinical trial. JCO 2014, 59, 1081–1091. [Google Scholar] [CrossRef] [PubMed]
- Lakoski, S.G.; Willis, B.L.; Barlow, C.E.; Leonard, D.; Gao, A.; Radford, N.B.; Farrell, S.W.; Douglas, P.S.; Berry, J.D.; DeFina, L.F.; et al. Midlife cardiorespiratory fitness, incident cancer, and survival after cancer in men: The cooper center longitudinal study. JAMA Oncol. 2015, 1, 231–237. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans; Department of Health and Human Services: Washington, DC, USA, 2008.
- Tanaka, H.; Monahan, K.G.; Seals, D.S. Age—Predicted maximal heart rate revisited. J. Am. Coll. Cardiol. 2001, 37, 153–156. [Google Scholar] [CrossRef]
- Scharhaq-Rosenberger, F.; Kuehl, R.; Klassen, O.; Schommer, K.; Schmidt, M.E.; Ulrich, C.M.; Wiskemann, J.; Steindorf, K. Exercise training intensity prescription in breast cancer survivors: Validity of current practice and specific recommendations. J. Cancer Survivorship 2015, 9, 612–619. [Google Scholar] [CrossRef] [PubMed]
- Klika, R.J.; Callahan, K.E.; Drum, S.N. Effects of individualized 12 weeks exercise training enhance aerobic capacity of cancer survivors. Phys. Sportsmed. 2009, 37, 68–77. [Google Scholar] [CrossRef] [PubMed]
- Nelson, M.E.; Rejeski, W.J.; Blair, S.N.; Duncan, P.W.; Judge, J.O.; King, A.C.; Macera, C.A.; Castaneda-Sceppa, C. Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Med. Sci. Sports Exerc. 2007, 8, 1435–1445. [Google Scholar] [CrossRef] [PubMed]
- Holmes, M.D.; Chen, Y.; Feskanich, D.; Kroenke, C.H.; Colditz, G.A. Physical activity and survival after breast cancer diagnosis. JAMA 2005, 293, 2479–2486. [Google Scholar] [CrossRef] [PubMed]
- McGill, S. Core training: Evidence translating to better performance and injury prevention. Strength Cond. J. 2010, 32, 33–46. [Google Scholar] [CrossRef]
- Eustruch, R.; Ros, E.; Salas-Salvado, J.; Covas, M.I.; Corella, D.; Aros, F.; Gomez-Gracia, E.; Ruiz-Gutierrez, V.; Fiol, M.; Lapetra, J.; et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N. Engl. J. Med. 2013, 368, 1279–1290. [Google Scholar] [CrossRef] [PubMed]
- Shai, I.; Schwarzfuchs, D.; Henkin, Y.; Shahar, D.R.; Witkow, S.; Greenberg, I.; Golan, R.; Fraser, D.; Bolotin, A.; Vardi, H.; et al. Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. NEJM 2008, 359, 229–241. [Google Scholar] [CrossRef] [PubMed]
- Bjelakovic, G.; Nikolova, D.; Gluud, L.L.; Simonetti, R.G.; Gluud, C. Antioxidant supplements for prevention of mortality in healthy participants and patients with various diseases. Cochrane Database Syst. Rev. 2012. [Google Scholar] [CrossRef]
© 2017 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).