Morphological and Motor Ability Adaptations Following a Short-Term Moderate-Intensity Strength Training Intervention in a Sedentary Adult Male with Asymmetrical Bilateral Spastic Cerebral Palsy: A Case Study
Abstract
1. Introduction
2. Case Description
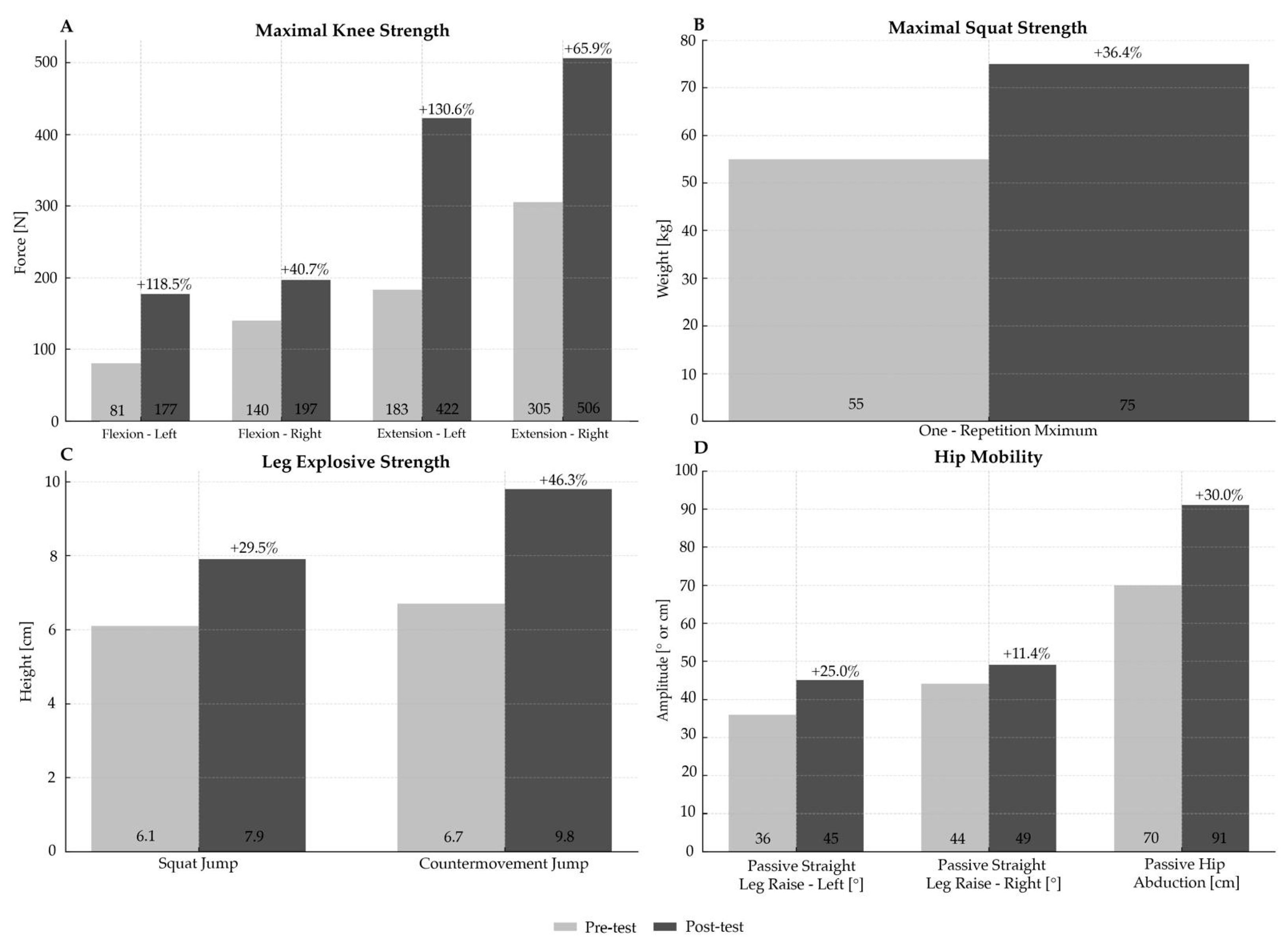
Results
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CP | Cerebral palsy |
| ST | Strength training |
| MC | Morphological characteristics |
| MA | Motor abilities |
References
- Centers for Disease Control and Prevention. Cerebral Palsy. Available online: https://www.cdc.gov/cerebral-palsy/about/?CDC_AAref_Val=https://www.cdc.gov/ncbddd/cp/facts.html (accessed on 23 July 2025).
- Rosenbaum, P.; Paneth, N.; Leviton, A.; Goldstein, M.; Bax, M.; Damiano, D.; Dan, B.; Jacobsson, B. A report: The definition and classification of cerebral palsy April 2006. Dev. Med. Child. Neurol. Suppl. 2007, 109, 8–14. [Google Scholar] [PubMed]
- Krigger, K.W. Cerebral palsy: An overview. Am. Fam. Physician 2006, 73, 91–100. [Google Scholar] [PubMed]
- Johnson, A. Prevalence and characteristics of children with cerebral palsy in Europe. Dev. Med. Child. Neurol. 2002, 44, 633–640. [Google Scholar] [CrossRef]
- Whitney, D.G.; Warschausky, S.A.; Ng, S.; Hurvitz, E.A.; Kamdar, N.S.; Peterson, M.D. Prevalence of mental health disorders among adults with cerebral palsy: A cross-sectional analysis. Ann. Intern. Med. 2019, 171, 328–333. [Google Scholar] [CrossRef] [PubMed]
- Ryan, J.M.; Peterson, M.D.; Matthews, A.; Ryan, N.; Smith, K.J.; O’Connell, N.E.; Liverani, S.; Anokye, N.; Victor, C.; Allen, E. Noncommunicable disease among adults with cerebral palsy: A matched cohort study. Neurology 2019, 93, e1385–e1396. [Google Scholar] [CrossRef] [PubMed]
- Wiley, M.E.; Damiano, D.L. Lower-extremity strength profiles in spastic cerebral palsy. Dev. Med. Child. Neurol. 1998, 40, 100–107. [Google Scholar] [CrossRef]
- Hombergen, S.P.; Huisstede, B.M.; Streur, M.F.; Stam, H.J.; Slaman, J.; Bussmann, J.B.; van den Berg-Emons, R.J. Impact of cerebral palsy on health-related physical fitness in adults: Systematic review. Arch. Phys. Med. Rehabil. 2012, 93, 871–881. [Google Scholar] [CrossRef] [PubMed]
- Verschuren, O.; Peterson, M.D.; Balemans, A.C.; Hurvitz, E.A. Exercise and physical activity recommendations for people with cerebral palsy. Dev. Med. Child. Neurol. 2016, 58, 798–808. [Google Scholar] [CrossRef]
- Scholtes, V.A.; Becher, J.G.; Comuth, A.; Dekkers, H.; Van Dijk, L.; Dallmeijer, A.J. Effectiveness of functional progressive resistance exercise strength training on muscle strength and mobility in children with cerebral palsy: A randomized controlled trial. Dev. Med. Child. Neurol. 2010, 52, e107–e113. [Google Scholar] [CrossRef] [PubMed]
- Aagaard, P. Training-induced changes in neural function. Exerc. Sport. Sci. Rev. 2003, 31, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, C.; Williams, G.N. Effect of knee joint angle on side-to-side strength ratios. J. Strength. Cond. Res. 2014, 28, 2981–2987. [Google Scholar] [CrossRef] [PubMed]
- Puig-Diví, A.; Escalona-Marfil, C.; Padullés-Riu, J.M.; Busquets, A.; Padullés-Chando, X.; Marcos-Ruiz, D. Validity and reliability of the Kinovea program in obtaining angles and distances using coordinates in four perspectives. PLoS ONE 2019, 14, e0216448. [Google Scholar] [CrossRef] [PubMed]
- Day, M.L.; McGuigan, M.R.; Brice, G.; Foster, C. Monitoring exercise intensity during resistance training using the session RPE scale. J. Strength. Cond. Res. 2004, 18, 353–358. [Google Scholar] [CrossRef] [PubMed]
- McManus, A.; Bembridge, M.; Scales, J.; Wiles, J.; Coleman, D.; O’Driscoll, J. A 4-week resistance training intervention improves stability, strength and neuromuscular activity in the lower limb: A case study of a cerebral palsy adult. Int. J. Sports Sci. Med. 2018, 2, 50–55. [Google Scholar] [CrossRef]
- Wittenberg, G.F. Neural plasticity and treatment across the lifespan for motor deficits in cerebral palsy. Dev. Med. Child. Neurol. 2009, 51, 130–133. [Google Scholar] [CrossRef] [PubMed]
- Taylor, N.F.; Dodd, K.J.; Larkin, H. Adults with cerebral palsy benefit from participating in a strength training programme at a community gymnasium. Disabil. Rehabil. 2004, 26, 1128–1134. [Google Scholar] [CrossRef] [PubMed]

| Exercise Name | Exercise Description |
|---|---|
| Leg press | While sitting, push the resistance platform with both legs to full knee extension, then slowly lower the resistance platform down till comfortable hip and knee flexion. |
| Knee extension | In seated position with adjusted resistance bar over anterior shin, extend both knees till full extension, then slowly lower the resistance bar. |
| Knee flexion | In prone position with adjusted resistance bar over posterior shin, flex both knees till full flexion, then slowly lower the resistance bar. |
| Hip abduction | While sitting, push thigh pads laterally till full hip abduction, then slowly return to the starting position. |
| Hip adduction | While sitting, pull thigh pads medially till full hip adduction, then slowly return to the starting position. |
| Chest press | In supine position, push the resistance handles forward to full elbow extension, then slowly return to the starting position. |
| Shoulder press | While sitting, push the resistance handles overhead, to full elbow extension, then slowly return to the starting position. |
| Lat pull down | While sitting, pull the resistance handles as close to the chest as possible (pronated grip), then slowly release to the starting position. |
| Seated row | While sitting, pull the resistance handles as close to the torso as possible (parallel grip), then slowly release to the starting position. |
| Abdominals | While in supine position with knees bent and stabilized, perform trunk flexion till the scapulas are above the floor, then slowly return to the floor. |
| Triceps pull down | While standing, extend the elbows downward against cable resistance till full extension, then slowly return to the starting position. |
| Biceps curl | While sitting on Scott bench, flex the elbows upward against resistance bar till full flexion, then slowly return to the starting position. |
| Tests | Variables | Pre-Test | Post-Test | % |
|---|---|---|---|---|
| Body composition | Body Mass [kg] | 65.4 | 66.3 | +1.4 |
| Total Body Water [L] | 35.9 | 37.0 | +3.1 | |
| Skeletal Muscle Mass [kg] | 27.3 | 28.0 | +2.6 | |
| Body Fat Mass [kg] | 16.5 | 16.1 | −2.4 | |
| Body Fat Percentage [%] | 25.3 | 24.2 | −4.3 | |
| Visceral Fat Area [cm2] | 88.8 | 83.1 | −6.4 | |
| Protein [kg] | 9.7 | 9.9 | +2.1 | |
| Mineral [kg] | 3.28 | 3.30 | +0.6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Popović, A.; Kapeleti, M.; Zlatović, I.; Jankucić, M.; Kocić, A.; Mrdaković, V.; Macura, M. Morphological and Motor Ability Adaptations Following a Short-Term Moderate-Intensity Strength Training Intervention in a Sedentary Adult Male with Asymmetrical Bilateral Spastic Cerebral Palsy: A Case Study. J. Funct. Morphol. Kinesiol. 2025, 10, 442. https://doi.org/10.3390/jfmk10040442
Popović A, Kapeleti M, Zlatović I, Jankucić M, Kocić A, Mrdaković V, Macura M. Morphological and Motor Ability Adaptations Following a Short-Term Moderate-Intensity Strength Training Intervention in a Sedentary Adult Male with Asymmetrical Bilateral Spastic Cerebral Palsy: A Case Study. Journal of Functional Morphology and Kinesiology. 2025; 10(4):442. https://doi.org/10.3390/jfmk10040442
Chicago/Turabian StylePopović, Aleksandra, Marko Kapeleti, Igor Zlatović, Milica Jankucić, Anastasija Kocić, Vladimir Mrdaković, and Marija Macura. 2025. "Morphological and Motor Ability Adaptations Following a Short-Term Moderate-Intensity Strength Training Intervention in a Sedentary Adult Male with Asymmetrical Bilateral Spastic Cerebral Palsy: A Case Study" Journal of Functional Morphology and Kinesiology 10, no. 4: 442. https://doi.org/10.3390/jfmk10040442
APA StylePopović, A., Kapeleti, M., Zlatović, I., Jankucić, M., Kocić, A., Mrdaković, V., & Macura, M. (2025). Morphological and Motor Ability Adaptations Following a Short-Term Moderate-Intensity Strength Training Intervention in a Sedentary Adult Male with Asymmetrical Bilateral Spastic Cerebral Palsy: A Case Study. Journal of Functional Morphology and Kinesiology, 10(4), 442. https://doi.org/10.3390/jfmk10040442







