Gender Differences in the Relationship Between Fatigue, Different Types of Physical Activity, Postural Changes, and Sleep Quality in University Students—Part II Analyses from a Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
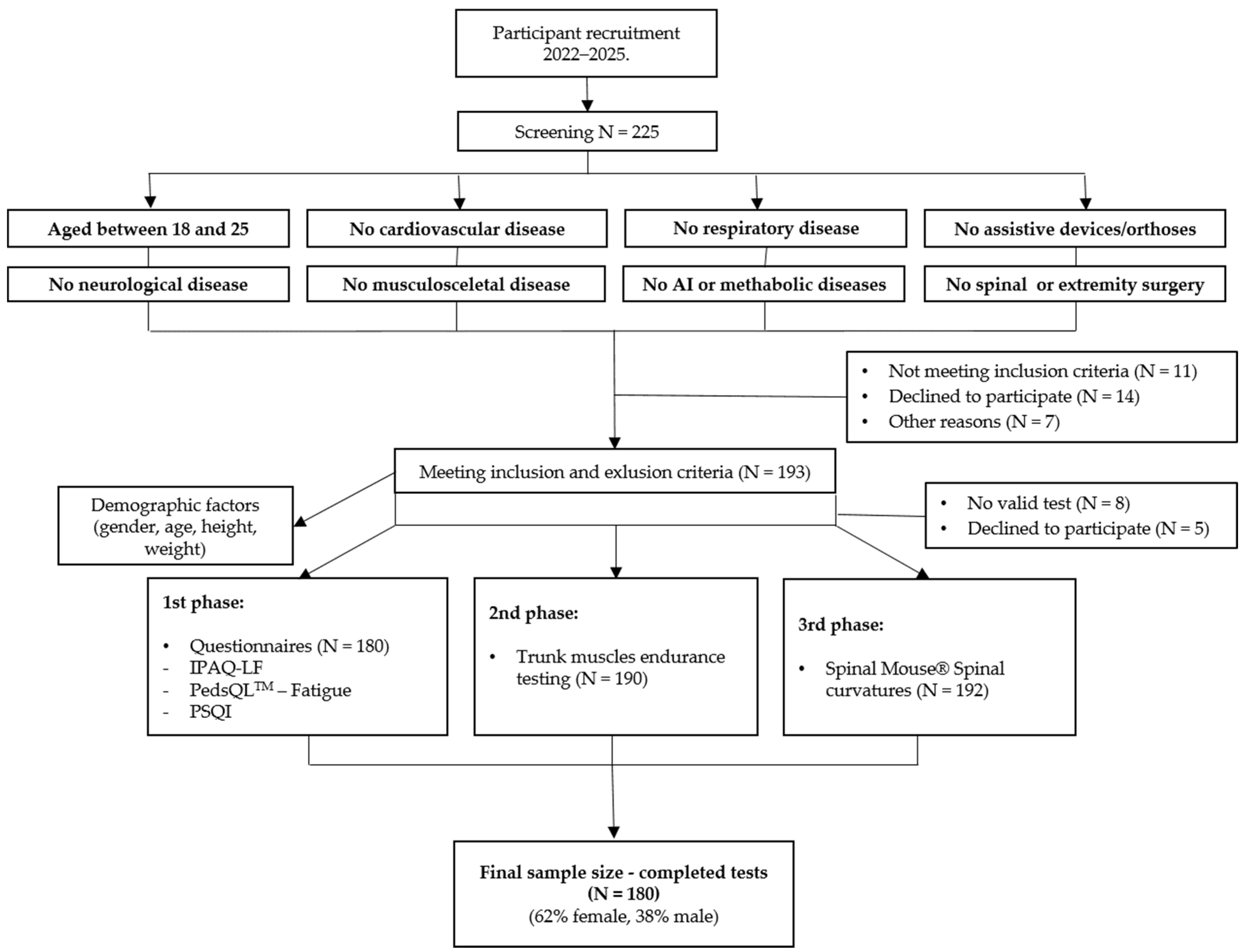
2.1. Participants
- (1)
- (2)
2.2. Study Design
2.3. Outcome Measures
2.3.1. Questionnaires
- •
- Self-Reported PA and Time Spent Sitting
- •
- Self-Reported Fatigue
- •
- Self-Reported Sleep Quality
2.3.2. Trunk Muscles Endurance Testing
- •
- Trunk Extensor Endurance Testing
- •
- Trunk Flexor Endurance Testing
- •
- Balance of Trunk Muscles
2.3.3. Visual Analogue Scale (VAS) for NS-LBP
2.3.4. Evaluation of Spinal Curvatures
2.4. Statistical Analysis
3. Results
4. Strengths and Limitations
5. Discussion
5.1. Relationship Between Fatigue, PA, Time Spent Sitting, and SQ in University Students
5.2. Relationship Between Fatigue, Posture, NS-LBP, and SQ in University Students
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PA | Physical activity |
| IPAQ-LF | International Physical Activity Questionnaire-Long Form |
| PedsQL | Pediatric Quality of Life |
| SQ | Sleep quality |
| NS-LPB | Non-specific low back pain |
| STROBE | Strengthening the Reporting of Observational Studies in Epidemiology |
| PSQI | Pittsburgh Sleep Quality |
| VAS | Visual Analogue Scale |
| SM | Spinal Mouse |
| ICC | Interclass Correlation Coefficient |
| PSIS | Posterior superior iliac spine |
| BMI | Body mass index |
| MET | Metabolic Equivalent of Tasks |
| NA | Not applicable |
| df | Degree of freedom |
| SD | Standard deviation |
| SES | Socioeconomic status |
References
- Hallal, P.C.; Andersen, L.B.; Bull, F.C.; Guthold, R.; Haskell, W.; Ekelund, U. Global physical activity levels: Surveillance progress, pitfalls, and prospects. Lancet 2012, 380, 247–257. [Google Scholar] [CrossRef] [PubMed]
- Haseler, T.; Haseler, C. Lack of physical activity is a global problem. BMJ 2022, 376, o348. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks. Available online: https://iris.who.int/handle/10665/44203 (accessed on 20 January 2025).
- Grasdalsmoen, M.; Eriksen, H.R.; Lønning, K.J.; Sivertsen, B. Physical exercise and body-mass index in young adults: A national survey of Norwegian university students. BMC Public Health 2019, 19, 1354. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World. Available online: https://iris.who.int/handle/10665/272722 (accessed on 20 January 2025).
- Park, J.H.; Moon, J.H.; Kim, H.J.; Kong, M.H.; Oh, Y.H. Sedentary Lifestyle: Overview of updated evidence of potential health risks. Korean J. Fam. Med. 2020, 41, 365–373. [Google Scholar] [CrossRef]
- Peterson, N.E.; Sirard, J.R.; Kulbok, P.A.; DeBoer, M.D.; Erickson, J.M. Sedentary behavior and physical activity of young adult university students. Res. Nurs. Health 2018, 41, 30–38. [Google Scholar] [CrossRef]
- Huang, Z.; Liu, Y.; Zhou, Y. Sedentary Behaviors and Health Outcomes among Young Adults: A Systematic Review of Longitudinal Studies. Healthcare 2022, 10, 1480. [Google Scholar] [CrossRef]
- Marijančić, V.; Peharec, S.; Starčević-Klasan, G.; Kezele, T.G. Gender Differences in the Relationship between Physical Activity, Postural Characteristics and Non-Specific Low Back Pain in Young Adults. J. Funct. Morphol. Kinesiol. 2024, 9, 189. [Google Scholar] [CrossRef]
- Jabeen, R.; Narjis Unar, N.; Khan, D.S.; Tunio, S.; Sabah, N.A. Study on the Effects of Students’ Posture, Comfort and Health in Consequences of Prolonged Sitting among Senior Cambridge Students. Available online: https://journalppw.com/index.php/jpsp/article/view/16827 (accessed on 20 January 2025).
- Bricout, V.-A.; Nguyen, D.-T.; Juvin, A.F. Physical activity or inactivity and Fatigue in Children and Adolescents: A Cross-Sectional Study. J. Clin. Med. 2025, 14, 1574. [Google Scholar] [CrossRef]
- O’Connor, P.J. Evaluation of four highly cited energy and fatigue mood measures. J. Psychosom. Res. 2004, 57, 435–441. [Google Scholar] [CrossRef]
- Maekawa, M.; Yoshizawa, E.; Hayata, G.; Ohashi, S. Physical and psychological effects of postural educational intervention for students experienced school refusal. Curr. Psychol. 2021, 42, 3510–3519. [Google Scholar] [CrossRef]
- Alias, A.N.; Karuppiah, K.; Sanmugam, K. Optimising Posture: An Experimental Study of Posture Support for Comfort among University Students. Int. J. Acad. Res. Bus. Soc. Sci. 2024, 14, 1975–1991. [Google Scholar] [CrossRef] [PubMed]
- Salmela-Aro, K.; Kiuru, N.; Pietikäinen, M.; Jokela, J. Does school matter? Eur. Psychol. 2008, 13, 12–23. [Google Scholar] [CrossRef]
- Likhon, D.N. Combining Workload and Academic Performance: Case of International Students. Master’s Thesis, Tallinn University of Technology, Tallinn, Estonia, 2021. [Google Scholar]
- Marcora, S.M.; Staiano, W.; Manning, V. Mental fatigue impairs physical performance in humans. J. Appl. Physiol. 2009, 106, 857–864. [Google Scholar] [CrossRef] [PubMed]
- Van Cutsem, J.; Marcora, S.; De Pauw, K.; Bailey, S.; Meeusen, R.; Roelands, B. The Effects of Mental Fatigue on Physical Performance: A Systematic review. Sports Med. 2017, 47, 1569–1588. [Google Scholar] [CrossRef]
- Habay, J.; Van Cutsem, J.; Verschueren, J.; De Bock, S.; Proost, M.; De Wachter, J.; Tassignon, B.; Meeusen, R.; Roelands, B. Mental Fatigue and Sport-Specific Psychomotor Performance: A Systematic review. Sports Med. 2021, 51, 1527–1548. [Google Scholar] [CrossRef]
- Wylie, G.R.; Sisto, A.J.P.; Genova, H.M.; DeLuca, J. Fatigue Across the Lifespan in Men and Women: State vs. Trait. Front. Hum. Neurosci. 2022, 16, 790006. [Google Scholar] [CrossRef]
- Li, W.; Chen, J.; Li, M.; Smith, A.P.; Fan, J. The effect of exercise on academic fatigue and sleep quality among university students. Front. Psychol. 2022, 13, 1025280. [Google Scholar] [CrossRef]
- Baran, E.; Yılmaz, A. The relationship between physical activity, fatigue, sleep quality, and anxiety levels of students during the university examination period. Northwestern Med. J. 2025, 5, 39–45. [Google Scholar] [CrossRef]
- Kezele, T.G.; Babić, M.; Štimac, D. Exploring the feasibility of a mild and short 4-week combined upper limb and breathing exercise program as a possible home base program to decrease fatigue and improve quality of life in ambulatory and non-ambulatory multiple sclerosis individuals. Neurol. Sci. 2019, 40, 733–743. [Google Scholar] [CrossRef]
- Marijančić, V.; Kezele, T.G.; Peharec, S.; Dragaš-Zubalj, N.; Žeželj, S.P.; Starčević-Klasan, G. Relationship between Physical Activity and Sedentary Behavior, Spinal Curvatures, Endurance and Balance of the Trunk Muscles-Extended Physical Health Analysis in Young Adults. Int. J. Environ. Res. Public. Health 2023, 20, 6938. [Google Scholar] [CrossRef]
- Golmohamadi, S.; Graham, B.M. Why are women more fatigued than men? The roles of stress, sleep, and repetitive negative thinking. Psychol. Health Med. 2025, 30, 1485–1506. [Google Scholar] [CrossRef]
- Amann, M.; Proctor, L.T.; Sebranek, J.J.; Pegelow, D.F.; Dempsey, J.A. Opioid-mediated muscle afferents inhibit central motor drive and limit peripheral muscle fatigue development in humans. J. Physiol. 2008, 587, 271–283. [Google Scholar] [CrossRef] [PubMed]
- Hunter, S.K. Sex differences in human fatigability: Mechanisms and insight to physiological responses. Acta Physiol. 2014, 210, 768–789. [Google Scholar] [CrossRef]
- Esbjornsson-Liljedahl, M.; Sundberg, C.J.; Norman, B.; Jansson, E. Metabolic response in type I and type II muscle fibers during a 30-s cycle sprint in men and women. J. Appl. Physiol. 1999, 87, 1326–1332. [Google Scholar] [CrossRef] [PubMed]
- Esbjornsson-Liljedahl, M.; Bodin, K.; Jansson, E. Smaller muscle ATP reduction in women than in men by repeated bouts of sprint exercise. J. Appl. Physiol. 2002, 93, 1075–1083. [Google Scholar] [CrossRef]
- Ghram, A.; Abidi, S.; Ben Abdessamie, A.; Weiss, K.; Dammak, M.; Jribi, S.; Yahia, A.; Ghroubi, S.; Habib Elleuch, M.; Knechtle, B. Impact of gender, change of base of support, and visual deprivation on postural balance control in young, healthy subjects. INTJSSH 2021, 4, e126891. [Google Scholar] [CrossRef]
- Smith, L.K.; Lelas, J.L.; Kerrigan, D.C. Gender differences in pelvic motions and center of mass displacement during walking: Stereotypes quantified. J. Womens Health Gend. Based Med. 2002, 11, 453–458. [Google Scholar] [CrossRef]
- Krasnoff, J.B.; Basaria, S.; Pencina, M.J.; Jasuja, G.K.; Vasan, R.S.; Ulloor, J.; Zhang, A.; Coviello, A.; Kelly-Hayes, M.; D’Agostino, R.B.; et al. Free testosterone levels are associated with mobility limitation and physical performance in community-dwelling men: The Framingham Offspring Study. J. Clin. Endocrinol. Metab. 2010, 95, 2790–2799. [Google Scholar] [CrossRef]
- Marijančić, V.; Starčević-Klasan, G.; Grubić Kezele, T. Gender differences in physical activity and quality of life in university students of Rijeka. In Proceedings of the 2nd International Scientific Conference 4 Healthy Academic Society, Poreč, Croatia, 30 May–1 June 2024; Available online: https://conference.unisport.hr/.
- Chaitow, L. Muscle Energy Techniques, 3rd ed.; Elsevier Health Sciences: Saintt Louis, UK, 2006. [Google Scholar] [CrossRef]
- Suzuki, N.; Endo, S. A quantitative study of trunk muscle strength and fatigability in the Low- Back-Pain Syndrome. Spine 1983, 8, 69–74. [Google Scholar] [CrossRef]
- Zorlular, A.; Aygün Polat, E.; Kafa, N.; Atalay Guzel, N. The Relationship Between Trunk Muscle Strength and Pelvic Oscillation in Asymptomatic Physically Inactive Adults. Turk. J. Physiother. Rehabil. 2022, 33, 139–145. [Google Scholar] [CrossRef]
- Liebenson, C. Rehabilitation of the Spine: A Practitioner’s Manual, 2nd ed.; Williams & Wilkins: Baltimore, MD, USA, 1996. [Google Scholar]
- Kelly, G.A.; Blake, C.; Power, C.K.; O’Keeffe, D.; Fullen, B.M. The association between chronic low back pain and sleep. Clin. J. Pain 2010, 27, 169–181. [Google Scholar] [CrossRef] [PubMed]
- Çelenay, Ş.T.; Kaya, D.Ö. An 8-week thoracic spine stabilization exercise program improves postural back pain, spine alignment, postural sway, and core endurance in university students:a randomized controlled study. Turk. J. Med. Sci. 2017, 47, 504–513. [Google Scholar] [CrossRef] [PubMed]
- Khobkhun, F.; Thanakamchokchai, J. Biological sex-related differences in whole-body coordination during standing turns in healthy young adults. Sci. Rep. 2023, 13, 22112. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences. 2013. [Google Scholar]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef]
- IPAQ—Score. Available online: https://sites.google.com/view/ipaq/score?authuser=0 (accessed on 21 January 2024).
- Booth, M. Assessment of Physical Activity: An international perspective. Res. Q. Exerc. Sport 2000, 71, 114–120. [Google Scholar] [CrossRef]
- Dinger, M.K.; Behrens, T.K.; Han, J.L. Validity and reliability of the International Physical Activity Questionnaire in College students. AJHE 2006, 37, 337–343. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.L.; Yngve, A.; Sallis, J.F.; et al. International Physical Activity Questionnaire: 12-Country Reliability and Validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Varni, J.W.; Limbers, C.A. The PedsQL™ Multidimensional Fatigue Scale in young adults: Feasibility, reliability and validity in a University student population. Qual. Life. Res. 2007, 17, 105–114. [Google Scholar] [CrossRef]
- Varni, J.W.; Limbers, C.A.; Bryant, W.P.; Wilson, D.P. The PedsQL™ Multidimensional Fatigue Scale in pediatric obesity: Feasibility, reliability and validity. Int. J. Pediatr. Obes. 2010, 5, 34–42. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef] [PubMed]
- Kezele, T.G.; Trope, Z.; Ahel, V.; Ružić, N.; Omrčen, H.; Đudarić, L.; Fužinac-Smojver, A. Upper-lower limb and breathing exercise program for improving sleep quality and psychological status in multiple sclerosis: A pilot randomized controlled trial. Brain Impair. 2021, 24, 86–102. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Wu, Y.-X.; Lin, Y.-Q.; Wang, L.; Zeng, Z.-N.; Xie, X.-L.; Chen, Q.-Y.; Wei, S.-C. Reliability and validity of the Pittsburgh Sleep Quality Index among frontline COVID-19 health care workers using classical test theory and item response theory. J. Clin. Sleep Med. 2021, 18, 541–551. [Google Scholar] [CrossRef]
- McGill, S.M.; Childs, A.; Liebenson, C. Endurance times for low back stabilization exercises: Clinical targets for testing and training from a normal database. Arch. Phys. Med. Rehabil. 1999, 80, 941–944. [Google Scholar] [CrossRef] [PubMed]
- Alaranta, H.; Hurri, H.; Heliövaara, M.; Soukka, A.; Harju, R. Non-dynamometric trunk performance tests: Reliability and normative data. J. Rehabilitation Med. 1994, 26, 211–215. [Google Scholar] [CrossRef]
- Reiman, M.P.; Krier, A.D.; Nelson, J.A.; Rogers, M.A.; Stuke, Z.O.; Smith, B.S. Comparison of Different Trunk Endurance Testing Methods in College-Aged Individuals. Available online: https://pubmed.ncbi.nlm.nih.gov/23091786/ (accessed on 20 January 2025).
- Kim, H.-J.; Chung, S.; Kim, S.; Shin, H.; Lee, J.; Kim, S.; Song, M.-Y. Influences of trunk muscles on lumbar lordosis and sacral angle. Eur. Spine J. 2005, 15, 409–414. [Google Scholar] [CrossRef]
- Chiarotto, A.; Maxwell, L.J.; Ostelo, R.W.; Boers, M.; Tugwell, P.; Terwee, C.B. Measurement properties of visual analogue scale, numeric rating scale, and pain Severity subscale of the brief pain inventory in patients with low back pain: A Systematic review. J. Pain 2018, 20, 245–263. [Google Scholar] [CrossRef]
- Kezele, T.G.; Babić, M.; Kauzlarić-Živković, T.; Gulić, T. Combined upper limb and breathing exercise programme for pain management in ambulatory and non-ambulatory multiple sclerosis individuals: Part II analyses from feasibility study. Neurol. Sci. 2019, 41, 65–74. [Google Scholar] [CrossRef]
- Mejia, E.A.; Hennrikus, W.L.; Schwend, R.M.; Emans, J.B. A Prospective Evaluation of Idiopathic Left Thoracic Scoliosis with Magnetic Resonance Imaging. J. Pediatr. Orthop. 1996, 16, 354–358. [Google Scholar] [CrossRef]
- Kellis, E.; Adamou, G.; Tzilios, G.; Emmanouilidou, M. Reliability of spinal range of motion in healthy boys using a Skin-Surface device. J. Manipulative Physiol. Ther. 2008, 31, 570–576. [Google Scholar] [CrossRef]
- Fadaee, E.; Seidi, F.; Rajabi, R. The Validity and Reliability of Spinal Mouse Device in Measuring Angle Values of Thoracic Kyphosis and Lumbar Lordosis. Available online: https://www.researchgate.net/publication/339988445_The_validity_and_reliability_of_spinal_mouse_device_in_measuring_angle_values_of_thoracic_kyphosis_and_lumbar_lordosis (accessed on 20 January 2025).
- Guermazi, M.; Ghroubi, S.; Kassis, M.; Jaziri, O.; Keskes, H.; Kessomtini, W.; Hammouda, I.B.; Elleuch, M. -H. Validité et reproductibilité du Spinal Mouse® pour l’étude de la mobilité en flexion du rachis lombaire. Ann. Réadapt. Méd. Phys. 2006, 49, 172–177. [Google Scholar] [CrossRef] [PubMed]
- Mannion, A.F.; Knecht, K.; Balaban, G.; Dvorak, J.; Grob, D. A new skin-surface device for measuring the curvature and global and segmental ranges of motion of the spine: Reliability of measurements and comparison with data reviewed from the literature. Eur. Spine J. 2004, 13, 122–136. [Google Scholar] [CrossRef]
- Post, R.B.; Leferink, V.J.M. Spinal mobility: Sagittal range of motion measured with the SpinalMouse, a new non-invasive device. Arch. Orthop. Trauma. Surg. 2004, 124, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Barrett, E.; McCreesh, K.; Lewis, J. Reliability and validity of non-radiographic methods of thoracic kyphosis measurement: A systematic review. Man. Ther. 2013, 19, 10–17. [Google Scholar] [CrossRef]
- Cepková, A.; Zemková, E.; Šooš, Ľ.; Uvaček, M.; Muyor, J.M. Spinal curvature in female and male university students with prolonged bouts of sedentary behaviour. Res. Sq. 2022. preprint. [Google Scholar] [CrossRef]
- Kim, J.H. Multicollinearity and misleading statistical results. Korean J. Anesthesiol. 2019, 72, 558–569. [Google Scholar] [CrossRef]
- O’Connor, P.J.; Puetz, T.W. Chronic physical activity and feelings of energy and fatigue. Med. Sci. Sports Exerc. 2005, 37, 299–305. [Google Scholar] [CrossRef]
- Wennberg, P.; Boraxbekk, C.-J.; Wheeler, M.; Howard, B.; Dempsey, P.C.; Lambert, G.; Eikelis, N.; Larsen, R.; Sethi, P.; Occleston, J.; et al. Acute effects of breaking up prolonged sitting on fatigue and cognition: A pilot study. BMJ Open 2016, 6, e009630. [Google Scholar] [CrossRef]
- Hu, N.-C.; Chen, J.-D.; Cheng, T.-J. The associations between long working hours, physical inactivity, and burnout. J. Occup. Environ. Med. 2016, 58, 514–518. [Google Scholar] [CrossRef]
- Bláfoss, R.; Sundstrup, E.; Jakobsen, M.D.; Brandt, M.; Bay, H.; Andersen, L.L. Physical workload and bodily fatigue after work: Cross-sectional study among 5000 workers. Eur. J. Public Health 2019, 29, 837–842. [Google Scholar] [CrossRef] [PubMed]
- Chrismas, B.C.R.; Taylor, L.; Cherif, A.; Sayegh, S.; Bailey, D.P. Breaking up prolonged sitting with moderate-intensity walking improves attention and executive function in Qatari females. PLoS ONE 2019, 14, e0219565. [Google Scholar] [CrossRef]
- Horiuchi, M.; Pomeroy, A.; Horiuchi, Y.; Stone, K.; Stoner, L. Effects of intermittent exercise during prolonged sitting on executive function, cerebrovascular, and psychological response: A randomized crossover trial. J. Appl. Physiol. 2023, 135, 1421–1430. [Google Scholar] [CrossRef]
- Alnawwar, M.A.; Alraddadi, M.I.; Algethmi, R.A.; Salem, G.A.; Salem, M.A.; Alharbi, A.A. The Effect of Physical activity on sleep quality and sleep Disorder: A Systematic review. Cureus 2023, 15, e43595. [Google Scholar] [CrossRef] [PubMed]
- Ablin, J.N.; Clauw, D.J.; Lyden, A.K.; Ambrose, K.; Williams, D.A.; Gracely, R.H.; Glass, J.M. Effects of Sleep Restriction and Exercise Deprivation on Somatic Symptoms and Mood in Healthy Adults. Available online: https://pubmed.ncbi.nlm.nih.gov/24373363/ (accessed on 20 January 2025).
- Kehler, T.; Kezele, T.G.; Fužinac-Smojver, A.; Kauzlarić-Živković, T. Association of vitamin D insufficiency and low physical activity with fatigue, headaches and psychological distress in college students, North-Mediterranean Croatia—A pilot study. Paediatr. Croat. 2021, 65. [Google Scholar] [CrossRef]
- Lupu, C.E.; Scafa-Udriște, A.; Matei, R.S.; Licu, M.; Stanciu, T.I.; Stanciu, G.; Hashemi, F.; Mihai, A.; Lupu, S.; Ene, R.; et al. Adolescent Nutritional Patterns and Health Behaviors in Romania: A Cross-Sectional Analysis. Nutrients 2025, 17, 1448. [Google Scholar] [CrossRef] [PubMed]
- Engberg, I.; Segerstedt, J.; Waller, G.; Wennberg, P.; Eliasson, M. Fatigue in the general population- associations to age, sex, socioeconomic status, physical activity, sitting time and self-rated health: The northern Sweden MONICA study 2014. BMC Public Health 2017, 17, 654. [Google Scholar] [CrossRef] [PubMed]
- Mohammadi, N.; Doosti-Irani, A.; Cheraghi, Z. Socioeconomic inequality in physical activity among adults in western Iran: A cross-sectional study. Int. J. Equity Health 2024, 23, 273. [Google Scholar] [CrossRef]
- Collinge, A.N.; Bath, P.A. Socioeconomic Background and Self-Reported Sleep Quality in Older Adults during the COVID-19 Pandemic: An Analysis of the English Longitudinal Study of Ageing (ELSA). Int. J. Environ. Res. Public Health 2023, 20, 4534. [Google Scholar] [CrossRef]
- Doerr, J.M.; Ditzen, B.; Strahler, J.; Linnemann, A.; Ziemek, J.; Skoluda, N.; Hoppmann, C.A.; Nater, U.M. Reciprocal relationship between acute stress and acute fatigue in everyday life in a sample of university students. Biol. Psychol. 2015, 110, 42–49. [Google Scholar] [CrossRef]
- Li, S.H.; Lloyd, A.R.; Graham, B.M. Physical and mental fatigue across the menstrual cycle in women with and without generalised anxiety disorder. Horm. Behav. 2020, 118, 104667. [Google Scholar] [CrossRef]
- Wojtys, E.M.; Ashton-Miller, J.A.; Huston, L.J.; Moga, P.J. The Association between Athletic Training Time and the Sagittal Curvature of the Immature Spine. Am. J. Sports Med. 2000, 28, 490–498. [Google Scholar] [CrossRef]
- Villafañe, J.H.; Bissolotti, L.; Zaina, F.; Arienti, C.; Donzelli, S.; Negrini, S. Thoracic hyperkyphosis non invasively measured by general practitioners is associated with chronic low back pain: A cross-sectional study of 1364 subjects. J. Bodyw. Mov. Ther. 2017, 22, 752–756. [Google Scholar] [CrossRef]
- Ghamkhar, L.; Kahlaee, A.H. The effect of trunk muscle fatigue on postural control of upright stance: A systematic review. Gait Posture 2019, 72, 167–174. [Google Scholar] [CrossRef]
- Snekkevik, H.; Eriksen, H.R.; Tangen, T.; Chalder, T.; Reme, S.E. Fatigue and Depression in Sick-Listed Chronic Low Back Pain patients. Pain Med. 2014, 15, 1163–1170. [Google Scholar] [CrossRef]
- Espada, M.; Romero-Parra, N.; Bores-García, D.; La Morena, J.M.D.-D. Gender differences in university students’ levels of physical activity and motivations to engage in physical activity. Educ. Sci. 2023, 13, 340. [Google Scholar] [CrossRef]
- Graves, B.S.; Hall, M.E.; Dias-Karch, C.; Haischer, M.H.; Apter, C. Gender differences in perceived stress and coping among college students. PLoS ONE 2021, 16, e0255634. [Google Scholar] [CrossRef] [PubMed]
- Why Women Feel More Stress at Work. Harvard Business Review. Available online: https://hbr.org/2016/08/why-women-feel-more-stress-at-work (accessed on 4 June 2025).
| Variable | Females | Males | Total | p Value | d |
|---|---|---|---|---|---|
| Gender, n (%) | 112 (62) | 68 (38) | 180 (100) | NA | NA |
| Age, mean ± SD | 20.7 ± 1.7 | 20.9 ± 1.8 | 20.7 ± 1.9 | 0.241 | 0.11 |
| BMI (kg/m2), mean ± SD | 24.1 ± 2.8 | 24.5 ± 3.2 | 24.8 ± 15.9 | 0.621 | 0.13 |
| General fatigue | 70.3 ± 19.4 | 67.4 ± 17.9 | 68.9 ± 17.9 | 0.350 | 0.15 |
| Sleep/rest fatigue | 64.2 ± 16.5 | 63.0 ± 16.8 | 63.4 ± 16.7 | 0.668 | 0.07 |
| Cognitive fatigue | 71.5 ± 23.1 | 73.6 ± 18.7 | 72.8 ± 20.4 | 0.548 | 0.09 |
| Total fatigue | 68.6 ± 16.4 | 67.9 ± 14.9 | 68.2 ± 15.4 | 0.809 | 0.04 |
| Variable (Per Fatigue Quartiles/MET-min/wk) | Females | Males | Total | p Value | d |
|---|---|---|---|---|---|
| Q1 (19–58) | |||||
| Q2 (59–69) | |||||
| Q3 (70–79) | |||||
| Q4 (80–99) | |||||
| a Participants, n (%) | (df = 3) 0.666 | NA | |||
| Q1 | 30/46 (65.2) | 16/46 (34.8) | 46/180 (25.6) | ||
| Q2 | 26/42 (61.9) | 16/42 (38.1) | 42/180 (23.3) | ||
| Q3 | 30/46 (65.2) | 16/46 (34.8) | 46/180 (25.6) | ||
| Q4 | 26/46 (56.5) | 20/46 (43.5) | 46/180 (25.6) | ||
| Level of PA | |||||
| b Walking (MET-min/wk), mean ± SD | 2249.4 ± 2049.0 | ||||
| Q1 | 2681.5 ± 2520.8 | 2773.5 ± 2787.7 | 0.922 | 0.03 | |
| Q2 | 1390.4 ± 1462.0 | 2334.0 ± 1705.1 | 0.108 | 0.59 | |
| Q3 | 2206.4 ± 1287.0 | 2689.5 ± 3152.9 | 0.509 | 0.2 | |
| Q4 | 2101.0 ± 1749.2 | 1979.4 ± 1553.8 | 0.827 | 0.07 | |
| Total | 2193.0 ± 1949.4 | 2378.5 ± 2274.2 | 0.577 | 0.08 | |
| b Moderate (MET-min/wk), mean ± SD | 1515.5 ± 1693.5 | ||||
| Q1 | 1967.8 ± 2511.8 | 1358.3 ± 746.4 | 0.459 | 0.33 | |
| Q2 | 1177.9 ± 1574.1 | 1799.5 ± 1276.3 | 0.265 | 0.43 | |
| Q3 | 1666.7 ± 1737.5 | 2207.9 ± 1874.5 | 0.392 | 0.2 | |
| Q4 | 875.5 ± 798.6 | 1831.3 ± 1668.8 | 0.027 * | 0.73 | |
| Total | 1430.4 ± 1809.3 | 2031.8 ± 1831.1 | 0.009 * | 0.33 | |
| b Vigorous (MET-min/wk), mean ± SD | 2159.9 ± 2699.6 | ||||
| Q1 | 2067.9 ± 2953.3 | 2431.1 ± 2198.9 | 0.739 | 0.14 | |
| Q2 | 1454.0 ± 2039.0 | 1997.8 ± 1439.2 | 0.452 | 0.3 | |
| Q3 | 2543.2 ± 3389.6 | 3867.8 ± 3876.6 | 0.339 | 0.36 | |
| Q4 | 884.8 ± 937.2 | 3669.1 ± 3113.4 | <0.001 * | 1.21 | |
| Total | 1791.4 ± 2591.3 | 3061.3 ± 2800.5 | 0.008 * | 0.47 | |
| b Total PA (MET-min/wk), mean ± SD | 5839.1 ± 4559.7 | ||||
| Q1 | 6562.1 ± 6039.1 | 5537.6 ± 3852.1 | 0.594 | 0.2 | |
| Q2 | 4088.4 ± 3713.9 | 5454.4 ± 3366.7 | 0.298 | 0.38 | |
| Q3 | 6416.3 ± 4570.1 | 7865.8 ± 6065.3 | 0.422 | 0.27 | |
| Q4 | 3861.3 ± 2331.8 | 7532.8 ± 4569.6 | 0.003 * | 1.01 | |
| Total | 4900.4 ± 4027.2 | 6913.3 ± 4378.1 | 0.005 * | 0.48 | |
| Type of PA | |||||
| b Job-related PA (MET-min/wk), mean ± SD | 1044.4 ± 2037.9 | ||||
| Q1 | 1910.5 ± 4524.2 | 450.0 ± 1064.2 | 0.28 | 0.44 | |
| Q2 | 496.4 ± 1752.8 | 526.3 ± 1038.9 | 0.957 | 0.02 | |
| Q3 | 460.3 ± 1474.3 | 2177.2 ± 3773.9 | 0.053 | 0.59 | |
| Q4 | 1208.1 ± 2739.9 | 2246.2 ± 3663.1 | 0.293 | 0.32 | |
| Total | 921.7 ± 2785.6 | 1252.6 ± 2647.3 | 0.473 | 0.12 | |
| b Transportation (MET-min/wk), mean ± SD | 986.5 ± 985.1 | ||||
| Q1 | 1128.6 ± 880.1 | 1406.0 ± 1817.7 | 0.532 | 0.19 | |
| Q2 | 664.5 ± 766.9 | 1042.1 ± 923.8 | 0.222 | 0.44 | |
| Q3 | 1092.9 ± 760.9 | 1078.0 ± 1526.7 | 0.968 | 0.01 | |
| Q4 | 785.5 ± 683.6 | 887.0 ± 829.6 | 0.669 | 0.13 | |
| Total | 924.9 ± 788.5 | 1082.7 ± 1249.4 | 0.341 | 0.15 | |
| b Housework (MET-min/wk), mean ± SD | 913.4 ± 1218.4 | ||||
| Q1 | 946.3 ± 1115.6 | 866.4 ± 1219.1 | 0.836 | 0.06 | |
| Q2 | 783.3 ± 1115.9 | 1390.2 ± 1455.9 | 0.188 | 0.46 | |
| Q3 | 1451.4 ± 1895.9 | 628.2 ± 1895.9 | 0.148 | 0.43 | |
| Q4 | 426.9 ± 453.7 | 803.2 ± 871.0 | 0.09 | 0.54 | |
| Total | 907.4 ± 1312.4 | 909.7 ± 1035.2 | 0.991 | 0 | |
| b Recreation, sport, and leisure -time (MET-min/wk), mean ± SD | 2872.3 ± 2548.6 | ||||
| Q1 | 2555.1 ± 2542.1 | 3193.6 ± 1539.2 | 0.461 | 0.3 | |
| Q2 | 2086.8 ± 2219.2 | 2948.7 ± 1972.6 | 0.295 | 0.41 | |
| Q3 | 3456.4 ± 3041.3 | 3347.8 ± 2348.9 | 0.914 | 0.03 | |
| Q4 | 1792.9 ± 1446.2 | 4432.8 ± 3494.6 | 0.003 * | 0.98 | |
| Total | 2578.7 ± 2500.6 | 3543.9 ± 2623.4 | 0.029 * | 0.37 | |
| b Sitting time (MET-min/wk), mean ± SD | 5.7 ± 2.0 | ||||
| Q1 | 6.3 ± 1.8 | 5.8 ± 3.3 | 0.601 | 0.18 | |
| Q2 | 6.1 ± 1.9 | 5.4 ± 2.2 | 0.371 | 0.34 | |
| Q3 | 5.7 ± 1.3 | 4.6 ± 2.3 | 0.092 | 0.58 | |
| Q4 | 5.9 ± 1.4 | 5.1 ± 1.2 | 0.089 | 0.61 | |
| Total | 6.2 ± 1.9 | 5.0 ± 1.6 | 0.013 * | 0.68 | |
| Variable | Total Fatigue (PedsQL™ Multidimensional Fatigue Scale) | |||
|---|---|---|---|---|
| Female | Male | |||
| r | p | r | p | |
| Type of PA (IPAQ-LF, MET-min/wk) | ||||
| Job-related PA (MET-min/wk) | −0.104 | 0.312 | 0.192 | 0.159 |
| Transportation (MET-min/wk) | −0.152 | 0.140 | 0.167 | 0.223 |
| Housework (MET-min/wk) | −0.081 | 0.435 | −0.043 | 0.751 |
| Recreation, sport, and leisure time (MET-min/wk) | −0.104 | 0.311 | 0.187 | 0.181 |
| Sitting time (h/day) | 0.027 | 0.800 | −0.097 | 0.692 |
| Level of PA (IPAQ-LF, MET-min/wk) | ||||
| Walking (MET-min/wk) | −0.153 | 0.136 | −0.005 | 0.689 |
| Moderate (MET-min/wk) | −0.153 | 0.136 | 0.158 | 0.248 |
| Vigorous (MET-min/wk) | −0.090 | 0.385 | 0.184 | 0.215 |
| Total (MET-min/wk) | −0.230 | 0.028 * | 0.158 | 0.257 |
| Variable | Total PA (IPAQ-LF, MET-min/wk) | |||
|---|---|---|---|---|
| Female | Male | |||
| PedsQL™ Multidimensional Fatigue Scale Domains | r | p | r | p |
| General fatigue | −0.161 | 0.127 | 0.187 | 0.178 |
| Sleep/rest fatigue | −0.236 | 0.024 * | 0.151 | 0.279 |
| Cognitive fatigue | −0.186 | 0.077 | 0.071 | 0.609 |
| Variable (Per Fatigue Quartiles/MET-min/wk) | Females | Males | Total | p Value | d |
|---|---|---|---|---|---|
| Q1 (19–58) | |||||
| Q2 (59–69) | |||||
| Q3 (70–79) | |||||
| Q4 (80–99) | |||||
| a Sleep quality, median (range) | 6 (0–17) | NA | |||
| Q1 | 7 (3–10) | 6 (2–17) | 0.379 | ||
| Q2 | 5 (2–7) | 6 (2–12) | 0.728 | ||
| Q3 | 5 (2–9) | 4 (2–11) | 0.618 | ||
| Q4 | 5 (2–11) | 6.5 (2–12) | 0.303 | ||
| Total | 6 (2–11) | 6 (2–17) | 0.723 | ||
| a NS-LBP, median (range) | 2 (0–8) | NA | |||
| Q1 | 2 (0–8) | 2 (0–8) | 0.346 | ||
| Q2 | 2 (0–7) | 1 (0–6) | 0.248 | ||
| Q3 | 1 (0- ) | 2 (0–6) | 0.733 | ||
| Q4 | 1 (0–6) | 2 (0–4) | 0.557 | ||
| Total | 2 (0–8) | 2 (0–8) | 0.21 | ||
| b Kyphosis straight standing (°), mean ± SD | 44.2 ± 9.7 | ||||
| Q1 | 40.3 ± 8.0 | 49.0 ± 10.8 | 0.034 * | 0.91 | |
| Q2 | 41.8 ± 9.4 | 46.8 ± 7.3 | 0.143 | 0.59 | |
| Q3 | 43.9 ± 8.0 | 46.5 ± 9.8 | 0.443 | 0.29 | |
| Q4 | 44.3 ± 12.9 | 45.0 ± 10.0 | 0.861 | 0.06 | |
| Total | 42.7 ± 9.6 | 46.4 ± 9.4 | 0.037 * | 0.38 | |
| b Lordosis straight standing (°), mean ± SD | −30.9 ± 9.4 | ||||
| Q1 | −35.3 ± 7.0 | −26.3 ± 8.1 | 0.009 * | 1.18 | |
| Q2 | −36.4 ± 9.3 | −28.1 ± 8.3 | 0.020 * | 1.65 | |
| Q3 | −36.4 ± 10.7 | −24.7 ± 7.7 | 0.007 * | 1.25 | |
| Q4 | −31.4 ± 8.5 | −27.1 ± 8.5 | 0.188 | 0.5 | |
| Total | −34.2 ± 8.9 | −26.3 ± 7.9 | <0.001 * | 0.93 | |
| b Trunk flexor endurance, mean ± SD | 167.9 ± 32.2 | ||||
| Q1 | 166.9 ± 32.1 | 178.7 ± 4.6 | 0.222 | 0.51 | |
| Q2 | 177.2 ± 10.8 | 176.0 ± 12.0 | 0.803 | 0.1 | |
| Q3 | 166.2 ± 29.9 | 160.8 ± 35.4 | 0.43 | 0.16 | |
| Q4 | 170.8 ± 25.3 | 159.5 ± 48.6 | 0.43 | 0.29 | |
| Total | 170.0 ± 26.1 | 164.8 ± 39.4 | 0.645 | 0.15 | |
| b Trunk extensor endurance, mean ± SD | 147.9 ± 36.8 | ||||
| Q1 | 170.6 ± 21.9 | 145.4 ± 32.7 | 0.022 * | 0.9 | |
| Q2 | 153.0 ± 33.2 | 113.7 ± 40.0 | 0.016 * | 1.06 | |
| Q3 | 149.4 ± 35.3 | 136.2 ± 42.9 | 0.35 | 0.33 | |
| Q4 | 145.0 ± 41.1 | 153.4 ± 33.5 | 0.571 | 0.22 | |
| Total | 154.3 ± 34.6 | 138.4 ± 38.1 | 0.019 * | 0.43 | |
| b Extensors/flexors ratio (balance), mean ± SD | 0.92 ± 0.5 | ||||
| Q1 | 1.01 ± 0.2 | 0.88 ± 0.2 | 0.075 | 0.65 | |
| Q2 | 0.87 ± 0.3 | 0.64 ± 0.3 | 0.017 * | 0.76 | |
| Q3 | 0.93 ± 0.3 | 0.86 ± 0.3 | 0.555 | 0.23 | |
| Q4 | 0.88 ± 0.2 | 0.78 ± 0.3 | 0.297 | 0.39 | |
| Total | 0.92 ± 0.3 | 0.80 ± 0.3 | 0.015 * | 0.4 |
| Variable | Sleep/Rest Fatigue (PedsQL™ Multidimensional Fatigue Scale) | PSQI (SQ) | ||||||
|---|---|---|---|---|---|---|---|---|
| Female | Male | Female | Male | |||||
| r | p | r | p | r | p | r | p | |
| PSQI (SQ) | −0.237 | 0.021 * | −0.311 | 0.023 * | / | / | / | / |
| VAS (NS-LBP) | −0.042 | 0.689 | −0.107 | 0.437 | 0.314 | 0.002 ** | 0.316 | 0.021 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marijančić, V.; Šegulja, S.; Vučković, M.; Sović, I.; Peharec, S.; Grubić Kezele, T.; Starčević-Klasan, G. Gender Differences in the Relationship Between Fatigue, Different Types of Physical Activity, Postural Changes, and Sleep Quality in University Students—Part II Analyses from a Cross-Sectional Study. J. Funct. Morphol. Kinesiol. 2025, 10, 307. https://doi.org/10.3390/jfmk10030307
Marijančić V, Šegulja S, Vučković M, Sović I, Peharec S, Grubić Kezele T, Starčević-Klasan G. Gender Differences in the Relationship Between Fatigue, Different Types of Physical Activity, Postural Changes, and Sleep Quality in University Students—Part II Analyses from a Cross-Sectional Study. Journal of Functional Morphology and Kinesiology. 2025; 10(3):307. https://doi.org/10.3390/jfmk10030307
Chicago/Turabian StyleMarijančić, Verner, Silvije Šegulja, Mirela Vučković, Ivana Sović, Stanislav Peharec, Tanja Grubić Kezele, and Gordana Starčević-Klasan. 2025. "Gender Differences in the Relationship Between Fatigue, Different Types of Physical Activity, Postural Changes, and Sleep Quality in University Students—Part II Analyses from a Cross-Sectional Study" Journal of Functional Morphology and Kinesiology 10, no. 3: 307. https://doi.org/10.3390/jfmk10030307
APA StyleMarijančić, V., Šegulja, S., Vučković, M., Sović, I., Peharec, S., Grubić Kezele, T., & Starčević-Klasan, G. (2025). Gender Differences in the Relationship Between Fatigue, Different Types of Physical Activity, Postural Changes, and Sleep Quality in University Students—Part II Analyses from a Cross-Sectional Study. Journal of Functional Morphology and Kinesiology, 10(3), 307. https://doi.org/10.3390/jfmk10030307









