A Preliminary Investigation of the Efficacy of Far-Infrared-Emitting Garments in Enhancing Objective and Subjective Recovery Following Resistance Exercise
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Study Design
2.3. Anthropometrics and Initial Survey
2.4. Resistance Exercise Protocol
2.5. Subjective Questionnaires
2.6. Countermovement Jump
2.7. Fatigue Biomarkers
2.8. Statistical Analyses
3. Results
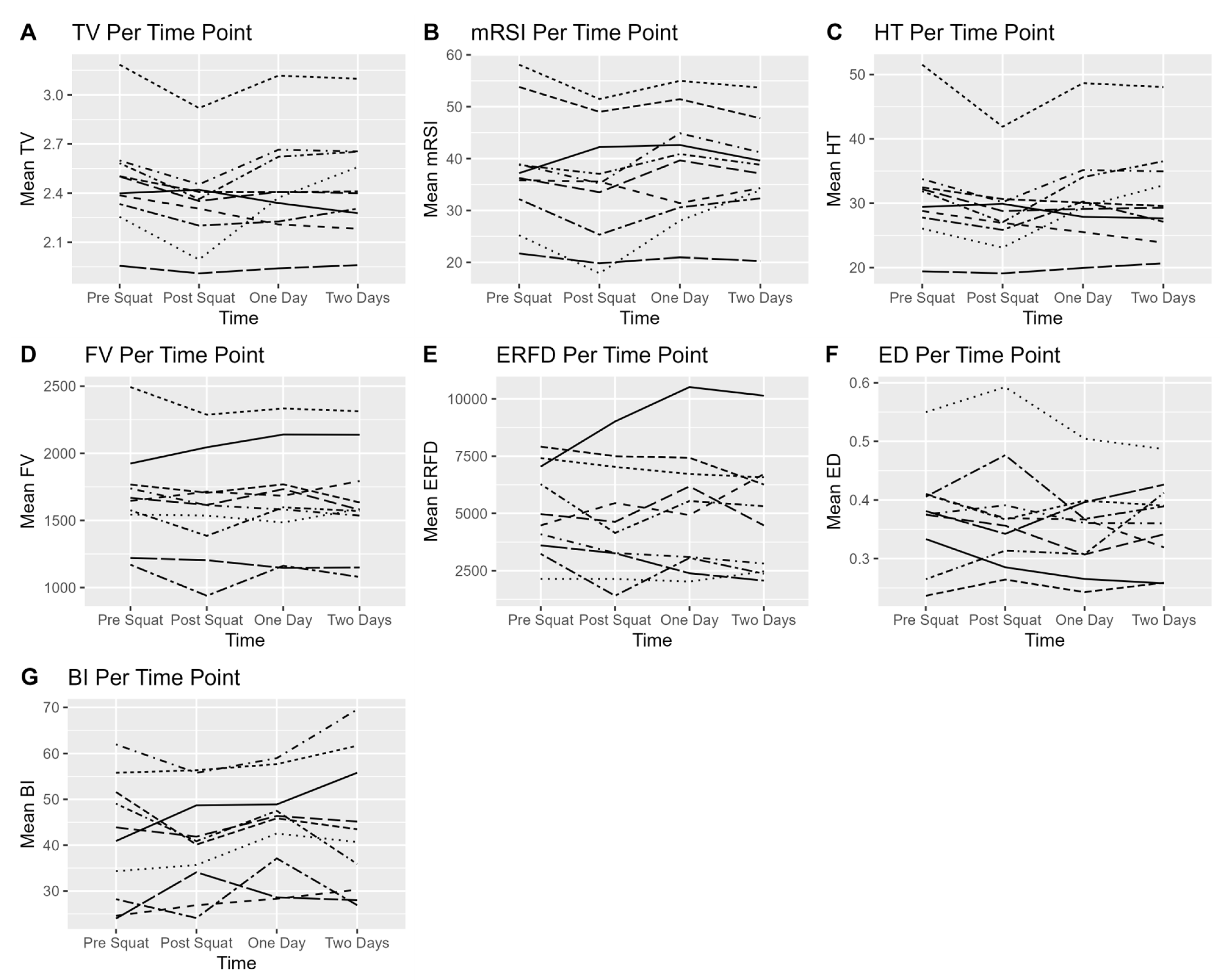
3.1. Countermovement Jump
3.2. Fatigue Biomarkers
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Andersson, H.M.; Raastad, T.; Nilsson, J.; Paulsen, G.; Garthe, I.; Kadi, F. Neuromuscular fatigue and recovery in elite female soccer: Effects of active recovery. Med. Sci. Sports Exerc. 2008, 40, 372–380. [Google Scholar] [CrossRef] [PubMed]
- Hausswirth, C.; Louis, J.; Bieuzen, F.; Pournot, H.; Fournier, J.; Filliard, J.; Brisswalter, J. Effects of whole-body cryotherapy vs. far-infrared vs. passive modalities on recovery from exercise-induced muscle damage in highly-trained runners. PLoS ONE 2011, 6, e27749. [Google Scholar] [CrossRef] [PubMed]
- Nédélec, M.; McCall, A.; Carling, C.; Legall, F.; Berthoin, S.; Dupont, G. Recovery in soccer: Part II—Recovery strategies. Sports Med. 2013, 43, 9–22. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.C.; Huang, Y.; Chou, T.; Hsu, S.; Chen, M.; Nosaka, K. Effects of far-infrared radiation lamp therapy on recovery from muscle damage induced by eccentric exercise. Eur. J. Sport Sci. 2023, 23, 1638–1646. [Google Scholar] [CrossRef]
- Leung, T.; Lee, C.; Tsai, S.; Chen, Y.; Chao, J. A pilot study of ceramic powder far-infrared ray irradiation (cFIR) on physiology: Observation of cell cultures and amphibian skeletal muscle. Chin. J. Physiol. 2011, 54, 247–254. [Google Scholar] [CrossRef]
- Vatansever, F.; Hamblin, M.R. Far infrared radiation (FIR): Its biological effects and medical applications: Ferne infrarotstrahlung: Biologische effekte und medizinische anwendungen. Photonics Lasers Med. 2012, 1, 255–266. [Google Scholar] [CrossRef]
- Tsai, S.; Hamblin, M.R. Biological effects and medical applications of infrared radiation. J. Photochem. Photobiol. B Biol. 2017, 170, 197–207. [Google Scholar] [CrossRef]
- Loturco, I.; Abad, C.C.C.; Nakamura, F.Y.; Ramos, S.d.P.; Kobal, R.; Gil, S.; Pereira, L.A.; Burini, F.H.P.; Roschel, H.; Ugrinowitsch, C. Effects of far infrared rays emitting clothing on recovery after an intense plyometric exercise bout applied to elite soccer players: A randomized double-blind placebo-controlled trial. Biol. Sport 2016, 33, 277–283. [Google Scholar] [CrossRef]
- Bontemps, B.; Gruet, M.; Vercruyssen, F.; Louis, J. Utilisation of far infrared-emitting garments for optimising performance and recovery in sport: Real potential or new fad? A systematic review. PLoS ONE 2021, 16, e0251282. [Google Scholar] [CrossRef]
- Mero, A.; Tornberg, J.; Mäntykoski, M.; Puurtinen, R. Effects of far-infrared sauna bathing on recovery from strength and endurance training sessions in men. Springerplus 2015, 4, 321. [Google Scholar] [CrossRef][Green Version]
- Wiriawan, O.; Setijono, H.; Putera, S.H.P.; Yosika, G.F.; Kaharina, A.; Sholikhah, A.M.; Pranoto, A. Far-infrared radiation with sauna method improves recovery of fatigue and muscle damage in athletes after submaximal physical exercise. Retos Nuevas Tend. Educ. Física Deporte Recreación 2024, 54, 57–62. [Google Scholar] [CrossRef]
- Katsuura, T.; Fukuda, S.; Okada, A.; Kikuchi, Y. Effect of ceramic-coated clothing on forearm blood flowduring exercise in a cool environment. Ann. Physiol. Anthropol. 1989, 8, 53–55. [Google Scholar] [CrossRef]
- Mantegazza, V.; Contini, M.; Botti, M.; Ferri, A.; Dotti, F.; Berardi, P.; Agostoni, P. Improvement in exercise capacity and delayed anaerobic metabolism induced by far-infrared-emitting garments in active healthy subjects: A pilot study. Eur. J. Prev. Cardiol. 2018, 25, 1744–1751. [Google Scholar] [CrossRef] [PubMed]
- Nunes, R.F.; Cidral-Filho, F.J.; Flores, L.J.; Nakamura, F.Y.; Rodriguez, H.F.; Bobinski, F.; De Sousa, A.; Petronilho, F.; Danielski, L.G.; Martins, M.M. Effects of far-infrared emitting ceramic materials on recovery during 2-week preseason of elite futsal players. J. Strength Cond. Res. 2020, 34, 235–248. [Google Scholar] [CrossRef] [PubMed]
- Furlan, J.P.; Mezzaroba, P.V.; Conrado, L.A.; Machado, F.A. Effect of ceramic-impregnated clothing on a 10 km running performance. Rev. Bras. Educ. Física Esporte 2018, 32, 189–198. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Lohman, T.G.; Roche, A.F.; Martorell, R. Anthropometric Standardization Reference Manual; Human Kinetics: Champaign, IL, USA, 1988. [Google Scholar]
- Durnin, J.V.; Womersley, J. Body fat assessed from total body density and its estimation from skinfold thickness: Measurements on 481 men and women aged from 16 to 72 years. Br. J. Nutr. 1974, 32, 77–97. [Google Scholar] [CrossRef]
- Brodie, D.A.; Eston, R.G. Body fat estimations by electrical impedance and infra-red interactance. Int. J. Sports Med. 1992, 13, 319–325. [Google Scholar] [CrossRef]
- Pareja-Blanco, F.; Rodríguez-Rosell, D.; Sánchez-Medina, L.; Sanchis-Moysi, J.; Dorado, C.; Mora-Custodio, R.; Yáñez-García, J.M.; Morales-Alamo, D.; Pérez-Suárez, I.; Calbet, J.A.L.; et al. Effects of velocity loss during resistance training on athletic performance, strength gains and muscle adaptations. Scand. J. Med. Sci. Sports 2017, 27, 724–735. [Google Scholar] [CrossRef]
- Borg, G. Borg’s Perceived Exertion and Pain Scales; Human Kinetics: Champaign, IL, USA, 1998. [Google Scholar]
- Harman, E.A.; Rosenstein, M.T.; Frykman, P.N.; ROSenStein, R.M. The effects of arms and countermovement on vertical jumping. Med. Sci. Sports Exerc. 1990, 22, 825–833. [Google Scholar] [CrossRef]
- McClymont, D.; Hore, A. Use of the reactive strength index (RSI) as an indicator of plyometric training conditions. In Science and Football V: The Proceedings of the Fifth World Congress on Sports Science and Football, Lisbon, Portugal; Routledge: London, UK, 2003; p. 16. [Google Scholar]
- McLellan, C.P.; Lovell, D.I.; Gass, G.C. The role of rate of force development on vertical jump performance. J. Strength Cond. Res. 2011, 25, 379–385. [Google Scholar] [CrossRef]
- Cormie, P.; McBride, J.M.; McCaulley, G.O. Power-time, force-time, and velocity-time curve analysis of the countermovement jump: Impact of training. J. Strength Cond. Res. 2009, 23, 177–186. [Google Scholar] [CrossRef]
- Haff, G.G.; Triplett, N.T. Essentials of Strength Training and Conditioning, 4th ed.; Human Kinetics: Champaign, IL, USA, 2015. [Google Scholar]
- Linthorne, N.P. Analysis of standing vertical jumps using a force platform. Am. J. Phys. 2001, 69, 1198–1204. [Google Scholar] [CrossRef]
- McMahon, J.J.; Lake, J.P.; Comfort, P. Reliability of and relationship between flight time to contraction time ratio and reactive strength index modified. Sports 2018, 6, 81. [Google Scholar] [CrossRef]
- Michael, D.J.; Daugherty, S.; Santos, A.; Ruby, B.C.; Kalns, J.E. Fatigue biomarker index: An objective salivary measure of fatigue level. Accid. Anal. Prev. 2012, 45, 68–73. [Google Scholar] [CrossRef] [PubMed]
- Kalns, J.; Baskin, J.; Reinert, A.; Michael, D.; Santos, A.; Daugherty, S.; Wright, J.K. Predicting success in the tactical air combat party training pipeline. Mil. Med. 2011, 176, 431–437. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Michael, D.J.; Valle, B.; Cox, J.; Kalns, J.E.; Fogt, D.L. Salivary biomarkers of physical fatigue as markers of sleep deprivation. J. Clin. Sleep Med. 2013, 9, 1325–1331. [Google Scholar] [CrossRef] [PubMed]
- Kuo, A.; Todd, J.J.; Witherspoon, J.W.; Lawal, T.A.; Elliott, J.; Chrismer, I.C.; Shelton, M.O.; Razaqyar, M.S.; Jain, M.S.; Vasavada, R. Reliability and validity of self-report questionnaires as indicators of fatigue in RYR1-related disorders. J. Neuromuscul. Dis. 2019, 6, 133–141. [Google Scholar] [CrossRef]
- Jason, L.A.; Kalns, J.; Richarte, A.; Katz, B.Z.; Torres, C. Saliva fatigue biomarker index as a marker for severe myalgic encephalomyelitis/chronic fatigue syndrome in a community based sample. Fatigue Biomed. Health Behav. 2021, 9, 189–195. [Google Scholar] [CrossRef]
- Bates, D. Fitting linear mixed-effects models using lme4. arXiv 2014, arXiv:1406.5823. [Google Scholar] [CrossRef]
- Lorah, J. Effect size measures for multilevel models: Definition, interpretation, and TIMSS example. Large-Scale Assess. Educ. 2018, 6, 8. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Leung, T.; Kuo, C.; Lee, C.; Kan, N.; Hou, C. Physiological effects of bioceramic material: Harvard step, resting metabolic rate and treadmill running assessments. Chin. J. Physiol. 2013, 56, 334–340. [Google Scholar] [CrossRef] [PubMed]
- Peake, J.M.; Neubauer, O.; Della Gatta, P.A.; Nosaka, K. Muscle damage and inflammation during recovery from exercise. J. Appl. Physiol. 2017, 122, 559–570. [Google Scholar] [CrossRef] [PubMed]
- Haugen, T.; Seiler, S.; Sandbakk, Ø.; Tønnessen, E. The training and development of elite sprint performance: An integration of scientific and best practice literature. Sports Med.-Open 2019, 5, 44. [Google Scholar] [CrossRef]
- Saw, A.E.; Main, L.C.; Gastin, P.B. Monitoring the athlete training response: Subjective self-reported measures trump commonly used objective measures: A systematic review. Br. J. Sports Med. 2016, 50, 281–291. [Google Scholar] [CrossRef]
- Halson, S.L. Monitoring fatigue and recovery. Sports Med. 2014, 44, 139–147. [Google Scholar] [CrossRef]
- Papacosta, E.; Nassis, G.P. Saliva as a tool for monitoring steroid, peptide and immune markers in sport and exercise science. J. Sci. Med. Sport 2011, 14, 424–434. [Google Scholar] [CrossRef]
- Brancaccio, P.; Maffulli, N.; Limongelli, F.M. Creatine kinase monitoring in sport medicine. Br. Med. Bull. 2007, 81, 209–230. [Google Scholar] [CrossRef]
- Hecksteden, A.; Pitsch, W.; Julian, R.; Pfeiffer, M.; Kellmann, M.; Ferrauti, A.; Meyer, T. A New Method to Individualize Monitoring of Muscle Recovery in Athletes. Int. J. Sports Physiol. Perform. 2017, 12, 1137–1142. [Google Scholar] [CrossRef]
- Nindl, B.C.; Leone, C.D.; Tharion, W.J.; Johnson, R.F.; Castellani, J.W.; Patton, J.F.; Montain, S.J. Physical performance responses during 72 h of military operational stress. Med. Sci. Sports Exerc. 2002, 34, 1814–1822. [Google Scholar] [CrossRef]
- Banfi, G.; Dolci, A. Free testosterone/cortisol ratio in soccer: Usefulness of a categorization of values. J. Sports Med. Phys. Fit. 2006, 46, 611. [Google Scholar]
- Halson, S.L.; Jeukendrup, A.E. Does overtraining exist? An analysis of overreaching and overtraining research. Sports Med. 2004, 34, 967–981. [Google Scholar] [CrossRef]

| Overall (N = 10) | FIR (N = 5) | Placebo (N = 5) | |
|---|---|---|---|
| Age (yrs) | 20.7 ± 3.2 | 21.8 ± 4.2 | 19.6 ± 1.5 |
| Height (cm) | 171.4 ± 8.8 | 174.7 ± 6.6 | 168.0 ± 10.0 |
| Weight (kg) | 75.6 ± 13.5 | 79.9 ± 8.8 | 71.4 ± 17.0 |
| Fat % (Skinfolds) | 23.2 ± 6.8 | 19.9 ± 6.5 | 26.5 ± 5.8 |
| Fat % (BIA) | 28.5 ± 5.1 | 24.9 ± 3.9 | 32.0 ± 3.6 |
| SMM (BIA, kg) | 25.7 ± 8.5 | 31.8 ± 5.0 | 19.7 ± 6.7 |
| Lifting Experience (yrs) | 4.4 ± 2.4 | 3.8 ± 2.1 | 4.9 ± 2.9 |
| 1 Rep Max (kg) | 274 ± 91 | 283 ± 67 | 266 ± 117 |
| ~85% of 1RM (kg) | 234 ± 77 | 241 ± 55 | 226 ± 100.0 |
| Reps Completed | 14.7 ± 2.2 | 12.4 ± 3.2 | 13.2 ± 3.0 |
| RPE | 8.8 ± 0.4 | 8.3 ± 0.3 | 8.7 ± 0.5 |
| Metric | Garment | Pre-Squat | 1 Day After | Percent Change from Pre-Squat Value | 2 Days After | Percent Change from Pre-Squat Value |
|---|---|---|---|---|---|---|
| Takeoff Velocity | FIR | 2.44 | 2.44 | 0.00 | 2.47 | 1.23 |
| Placebo | 2.50 | 2.42 | −3.20 | 2.43 | −2.80 | |
| mRSI | FIR | 35.19 | 37.56 | 6.73 | 37.57 | 6.76 |
| Placebo | 40.75 | 39.53 | −2.99 | 38.23 | −6.18 | |
| Jump Height | FIR | 29.99 | 30.41 | 1.40 | 31.16 | 3.90 |
| Placebo | 32.88 | 31.62 | −3.83 | 30.94 | −5.90 | |
| Force @ Zero Velocity | FIR | 1685.04 | 1697.26 | 0.72 | 1724.36 | 2.33 |
| Placebo | 1684.25 | 1628.77 | −3.29 | 1550.77 | −7.93 | |
| Eccentric RFD | FIR | 4806.40 | 5223.14 | 8.67 | 5491.60 | 14.26 |
| Placebo | 5520.21 | 5155.06 | −6.61 | 4350.41 | −21.19 | |
| Eccentric Duration | FIR | 0.39 | 0.36 | −7.69 | 0.37 | −5.13 |
| Placebo | 0.36 | 0.34 | −5.56 | 0.36 | 0.00 | |
| Braking Impulse | FIR | 42.17 | 45.25 | 7.30 | 46.44 | 10.13 |
| Placebo | 41.21 | 43.13 | 4.66 | 41.04 | −0.41 |
| Metric | Intercept (ES) | BETA_Time (Post) (ES) | BETA_Tights (FIR) (ES) | BETA_Interaction (ES) |
|---|---|---|---|---|
| Takeoff Velocity | 2.50 *** (0.14) | −0.08 * (−0.24) | −0.05 (−0.16) | 0.07 (0.23) |
| mRSI | 40.40 *** (0.20) | −0.87 (−0.08) | −5.21 (−0.47) | 3.25 * (0.30) |
| Jump Height | 32.76 *** (0.20) | −1.14 * (−0.15) | −2.77 (−0.36) | 1.56 (0.20) |
| Force @ Zero Velocity | 1664.44 *** (−0.03) | −35.68 (−0.10) | 20.59 (0.06) | 47.90 (0.13) |
| Eccentric RFD | 5433.32 *** (0.11) | −278.26 (−0.12) | −626.92 (−0.26) | 695.00 (0.29) |
| Eccentric Duration | 0.36 *** (−0.02) | −0.02 (−0.21) | 0.03 (0.29) | −0.01 (−0.08) |
| Braking Impulse | 40.86 *** (−0.14) | 2.27 (0.15) | 1.31 (0.09) | 0.81 (0.05) |
| Metric | Intercept (ES) | BETA_Time (Post) (ES) | BETA_Tights (FIR) (ES) | BETA_Interaction (ES) |
|---|---|---|---|---|
| Takeoff Velocity | 2.50 *** (0.12) | −0.06 * (−0.20) | −0.05 (−0.17) | 0.08 * (0.27) |
| mRSI | 40.47 *** (0.26) | −2.24 * (−0.22) | −5.28 (−0.53) | 4.61 *** (0.46) |
| Jump Height | 32.70 *** (0.19) | −1.76 ** (−0.23) | −2.71 (−0.35) | 2.93 ** (0.38) |
| Force @ Zero Velocity | 1664.34 *** (0.01) | −113.57 *** (−0.31) | 20.69 (0.06) | 152.89 *** (0.42) |
| Eccentric RFD | 5436.55 *** (0.17) | −1086.15 ** (−0.45) | −630.15 (−0.26) | 1771.34 *** (−0.22) |
| Eccentric Duration | 0.36 *** (−0.09) | 0.00 (0.00) | 0.03 (0.29) | −0.02 (−0.22) |
| Braking Impulse | 40.68 *** (−0.13) | 0.37 (0.02) | 1.49 (0.10) | 3.91 (0.25) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lever, J.R.; Ocobock, C.; Smith-Hale, V.; Metoyer, C.J.; Huebner, A.; Wagle, J.P.; Hauenstein, J.D. A Preliminary Investigation of the Efficacy of Far-Infrared-Emitting Garments in Enhancing Objective and Subjective Recovery Following Resistance Exercise. J. Funct. Morphol. Kinesiol. 2025, 10, 280. https://doi.org/10.3390/jfmk10030280
Lever JR, Ocobock C, Smith-Hale V, Metoyer CJ, Huebner A, Wagle JP, Hauenstein JD. A Preliminary Investigation of the Efficacy of Far-Infrared-Emitting Garments in Enhancing Objective and Subjective Recovery Following Resistance Exercise. Journal of Functional Morphology and Kinesiology. 2025; 10(3):280. https://doi.org/10.3390/jfmk10030280
Chicago/Turabian StyleLever, Jonathon R., Cara Ocobock, Valerie Smith-Hale, Casey J. Metoyer, Alan Huebner, John P. Wagle, and Jonathan D. Hauenstein. 2025. "A Preliminary Investigation of the Efficacy of Far-Infrared-Emitting Garments in Enhancing Objective and Subjective Recovery Following Resistance Exercise" Journal of Functional Morphology and Kinesiology 10, no. 3: 280. https://doi.org/10.3390/jfmk10030280
APA StyleLever, J. R., Ocobock, C., Smith-Hale, V., Metoyer, C. J., Huebner, A., Wagle, J. P., & Hauenstein, J. D. (2025). A Preliminary Investigation of the Efficacy of Far-Infrared-Emitting Garments in Enhancing Objective and Subjective Recovery Following Resistance Exercise. Journal of Functional Morphology and Kinesiology, 10(3), 280. https://doi.org/10.3390/jfmk10030280






