12 Weeks of Supervised Team Sports in Danish Municipal Health Center Lowers Systolic Blood Pressure and Increases Performance in Hypertensive Chronic Obstructive Pulmonary Disease and Type 2 Diabetes Mellitus Patients
Abstract
1. Introduction
2. Methods
2.1. Subjects
2.2. Training
2.3. Measuring and Test Procedures
2.3.1. Physiological Measures
2.3.2. Performance Tests
2.4. Statistics
3. Results
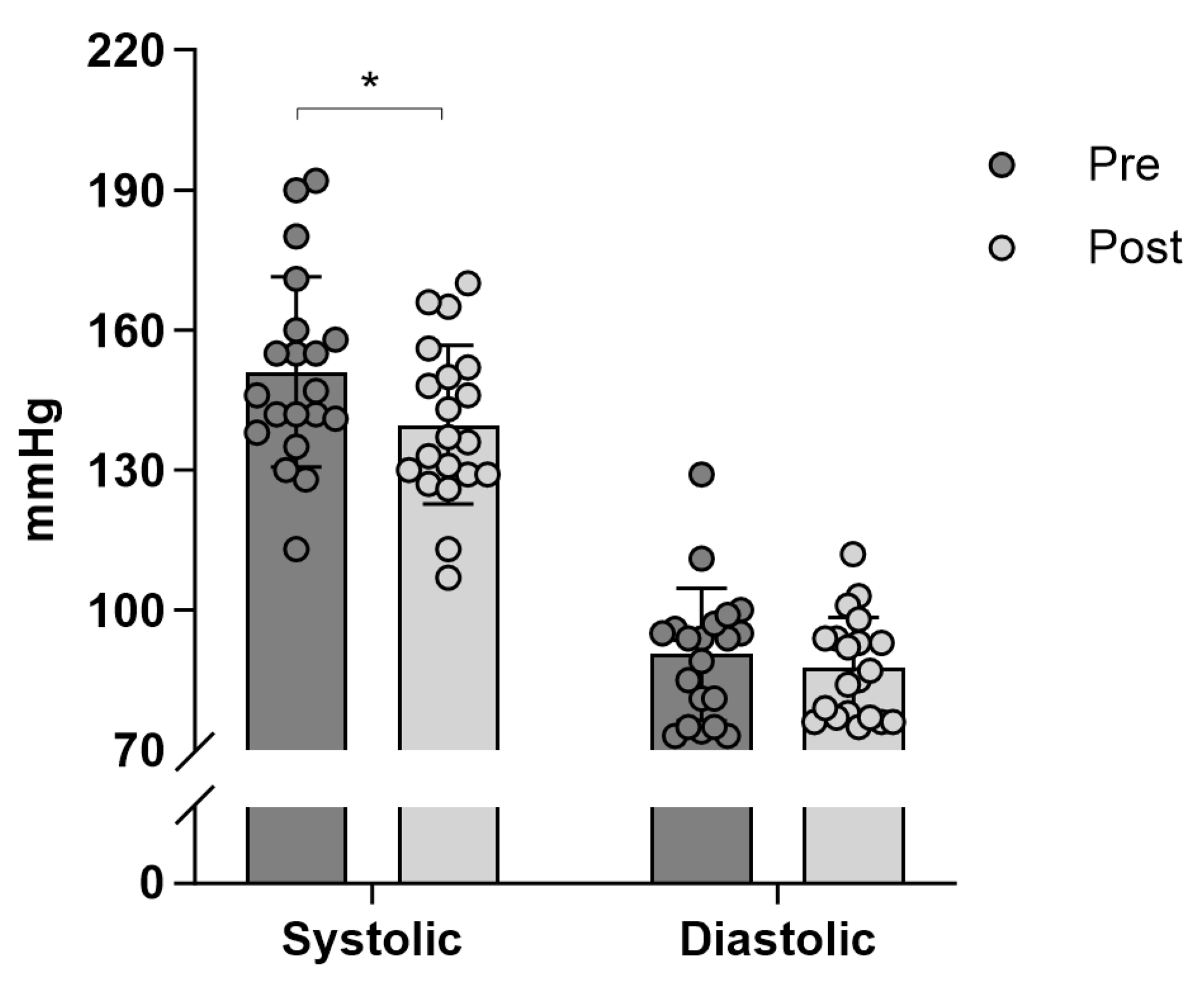
3.1. Blood Pressure
3.2. Body Mass
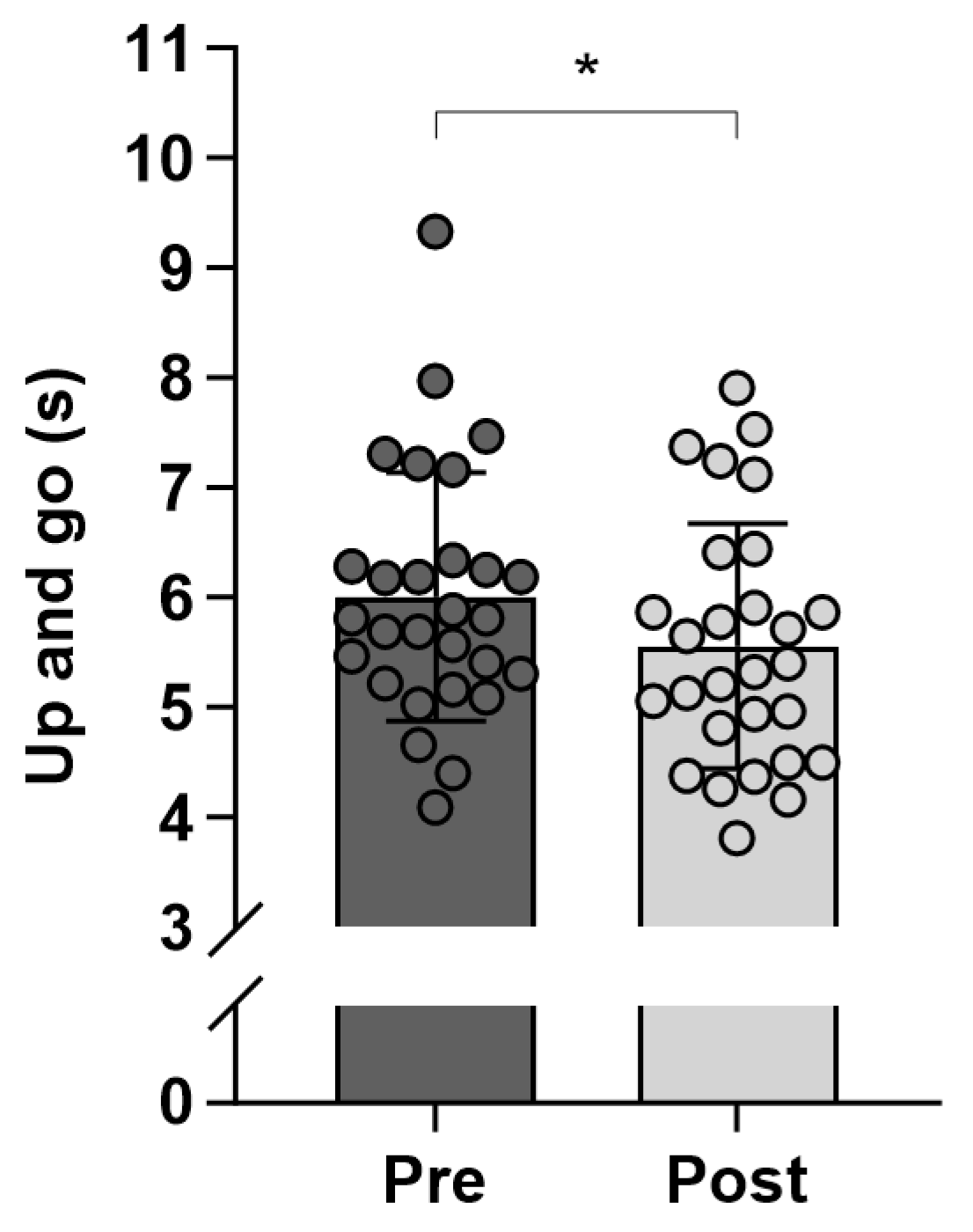
3.3. Functional Capacity
4. Discussion
5. Conclusions
6. Perspectives
7. Practical Applications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Abdelhafiz, A.H.; Sinclair, A.J. Diabetes, nutrition, and exercise. Clin. Geriatr. Med. 2015, 31, 439–451. [Google Scholar] [CrossRef] [PubMed]
- Houterman, S. Predicting cardiovascular risk in the elderly in different European countries. Eur. Heart J. 2002, 23, 294–300. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, M.T.; Vorup, J.; Nistrup, A.; Wikman, J.M.; Alstrøm, J.M.; Melcher, P.S.; Pfister, G.U.; Bangsbo, J. Effect of team sports and resistance training on physical function, quality of life, and motivation in older adults. Scand. J. Med. Sci. Sports 2017, 27, 852–864. [Google Scholar] [CrossRef] [PubMed]
- Mancia, G.; Kreutz, R.; Brunström, M.; Burnier, M.; Grassi, G.; Januszewicz, A.; Muiesan, M.L.; Tsioufis, K.; Agabiti-Rosei, E.; Algharably, E.A.E.; et al. 2023 esh guidelines for the management of arterial hypertension the task force for the management of arterial hypertension of the european society of hypertension: Endorsed by the international society of hypertension (Ish) and the european renal association (Era). J. Hypertens. 2023, 41, 1874–2071. [Google Scholar]
- Barnes, P.J. Inflammatory mechanisms in patients with chronic obstructive pulmonary disease. J. Allergy Clin. Immunol. 2016, 138, 16–27. [Google Scholar] [CrossRef]
- Medina-Leyte, D.J.; Zepeda-García, O.; Domínguez-Pérez, M.; González-Garrido, A.; Villarreal-Molina, T.; Jacobo-Albavera, L. Endothelial dysfunction, inflammation and coronary artery disease: Potential biomarkers and promising therapeutical approaches. Int. J. Mol. Sci. 2021, 22, 3850. [Google Scholar] [CrossRef]
- Santos, L.P.; Umpierre, D. Exercise, cardiovascular health, and risk factors for atherosclerosis: A narrative review on these complex relationships and caveats of literature. Front. Physiol. 2020, 11, 840. [Google Scholar] [CrossRef]
- Seo, D.Y.; Bae, J.H.; Li, X.; Han, J. Exercise training and cardiovascular health: Mechanisms, benefits, and therapeutic implications in cardiovascular disease. CardioMetab. Syndr. J. 2023, 3, 123. [Google Scholar] [CrossRef]
- Vorup, J.; Pedersen, M.T.; Melcher, P.S.; Dreier, R.; Bangsbo, J. Effect of floorball training on blood lipids, body composition, muscle strength, and functional capacity of elderly men. Scand. J. Med. Sci. Sports 2017, 27, 1489–1499. [Google Scholar] [CrossRef]
- Møller, T.K.; Nielsen, T.T.; Andersen, R.; Lundager, I.; Hansen, H.F.; Ottesen, L.; Krustrup, P.; Randers, M.B. Health effects of 12 weeks of team-sport training and fitness training in a community health centre for sedentary men with lifestyle diseases. BioMed Res. Int. 2018, 2018, 1–9. [Google Scholar] [CrossRef]
- Vorup, J.; Pedersen, M.T.; Brahe, L.K.; Melcher, P.S.; Alstrøm, J.M.; Bangsbo, J. Effect of small-sided team sport training and protein intake on muscle mass, physical function and markers of health in older untrained adults: A randomized trial. PLoS ONE 2017, 12, e0186202. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, M.T.; Vorup, J.; Bangsbo, J. Effect of a 26-month floorball training on male elderly’s cardiovascular fitness, glucose control, body composition, and functional capacity. J. Sport. Health Sci. 2018, 7, 149–158. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, G.; Wikman, J.M.; Jensen, C.J.; Schmidt, J.F.; Gliemann, L.; Andersen, T.R. Health promotion: The impact of beliefs of health benefits, social relations and enjoyment on exercise continuation. Scand. J. Med. Sci. Sports 2014, 24, 66–75. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, M.T.; Nørregaard, L.B.; Jensen, T.D.; Frederiksen, A.S.; Ottesen, L.; Bangsbo, J. The effect of 5 years of team sport on elderly males’ health and social capital—An interdisciplinary follow-up study. Health Sci. Rep. 2022, 5, e760. [Google Scholar] [CrossRef]
- Bauman, A.E.; Reis, R.S.; Sallis, J.F.; Wells, J.C.; Loos, R.J.; Martin, B.W. Correlates of physical activity: Why are some people physically active and others not? Lancet 2012, 380, 258–271. [Google Scholar] [CrossRef]
- Pedersen, B.K.; Saltin, B. Exercise as medicine—Evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand. J. Med. Sci. Sports 2015, 25, 1–72. [Google Scholar] [CrossRef]
- Andersen, L.J.; Randers, M.B.; Westh, K.; Martone, D.; Hansen, P.R.; Junge, A.; Dvorak, J.; Bangsbo, J.; Krustrup, P. Football as a treatment for hypertension in untrained 30–55-year-old men: A prospective randomized study. Scand. J. Med. Sci. Sports 2010, 20, 98–102. [Google Scholar] [CrossRef]
- Gunnarsson, T.P.; Ehlers, T.S.; Baasch-Skytte, T.; Lund, A.P.; Tamariz-Ellemann, A.; Gliemann, L.; Nyberg, M.; Bangsbo, J. Hypertension is associated with blunted NO-mediated leg vasodilator responsiveness that is reversed by high-intensity training in postmenopausal women. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2020, 319, R712–R723. [Google Scholar] [CrossRef]
- Gouzi, F.; Maury, J.; Bughin, F.; Blaquière, M.; Ayoub, B.; Mercier, J.; Perez-Martin, A.; Pomiès, P.; Hayot, M. Impaired training-induced adaptation of blood pressure in COPD patients: Implication of the muscle capillary bed. Int. J. Chron. Obstruct Pulmon Dis. 2016, 11, 2349–2357. [Google Scholar] [CrossRef]
- Li, J.; Cheng, W.; Ma, H. A comparative study of health efficacy indicators in subjects with t2dm applying power cycling to 12 weeks of low-volume high-intensity interval training and moderate-intensity continuous training. J. Diabetes Res. 2022, 2022, 9273830. [Google Scholar] [CrossRef]
- Dobrosielski, D.A.; Gibbs, B.B.; Ouyang, P.; Bonekamp, S.; Clark, J.M.; Wang, N.Y.; Silber, H.A.; Shapiro, E.P.; Stewart, K.J. Effect of exercise on blood pressure in type 2 diabetes: A randomized controlled trial. J. Gen. Intern. Med. 2012, 27, 1453–1459. [Google Scholar] [CrossRef] [PubMed]
- Ambelu, T.; Teferi, G. The impact of exercise modalities on blood glucose, blood pressure and body composition in patients with type 2 diabetes mellitus. BMC Sports Sci. Med. Rehabil. 2023, 15, 153. [Google Scholar] [CrossRef] [PubMed]
- Lewington, S.; Clarke, R.; Qizilbash, N.; Peto, R.; Collins, R. Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002, 360, 1903–1913. [Google Scholar]
- Sjúrðarson, T.; Kyhl, K.; Nordsborg, N.B.; Kollslíð, R.; Andersen, L.J.; Krustrup, P.; Mohr, M. 15 weeks of soccer training increases left ventricular mass and improves indices of left ventricular diastolic function in previously sedentary, mildly hypertensive, middle-aged women. Eur. J. Appl. Physiol. 2024, 124, 1621–1629. [Google Scholar] [CrossRef] [PubMed]
- Duncan, M.J.; Mowle, S.; Noon, M.; Eyre, E.; Clarke, N.D.; Hill, M.; Tallis, J.; Julin, M. The Effect of 12-Weeks Recreational Football (Soccer) for Health Intervention on Functional Movement in Older Adults. Int. J. Environ. Res. Public. Health. 2022, 19, 13625. [Google Scholar] [CrossRef]
- Lorenz, D.; Morrison, S. Current Concepts In Periodization of Strength and Conditioning for the Sports Physical Therapist. Int. J. Sports Phys. Ther. 2015, 10, 734–747. [Google Scholar]
- Francisco de Lima, F.; Marçal Camillo, C.A.; Grigoletto, I.; Uzeloto, J.; Marques Vanderlei, F.; Ramos, D.; Burtin, C.; Cipulo Ramos, E.M. Combining functional exercises with exercise training in COPD: A randomized controlled trial. Physiother. Theory Pract. 2024, 40, 952–961. [Google Scholar] [CrossRef] [PubMed]
- Janssen, S.M.; Connelly, D.M. The effects of exercise interventions on physical function tests and glycemic control in adults with type 2 diabetes: A systematic review. J. Bodyw. Mov. Ther. 2021, 28, 283–293. [Google Scholar] [CrossRef]
- Engdal Larsen, S.; Ottesen, L.S.; Hansen, H.F. Implementering af Brobygning: Fra Kommunalt Træningsforløb til Idrætsforeninger eller Idrætsfællesskaber [Internet]. Center for Holdspil og Sundhed, Institut for Idræt og Ernæring, Københavns Universitet. 2020. Available online: https://holdspil.ku.dk/nyheder/2020/rapport-implementering-af-brobygning/WEB_Implementering_af_brobygning.pdf (accessed on 5 March 2025).
- Engdal, S.; Hansen, H.F.; Ottesen, L.S. Mind the gap: Building bridges between public sector exercise programmes and civil society sports associations. An integrative review of the literature. Eur. J. Sport. Soc. 2023, 20, 279–298. [Google Scholar] [CrossRef]
| COPD (n = 12) | T2DM (n = 16) | |
|---|---|---|
| Age (years) | 69.4 ± 5.9 | 64.5 ± 10.7 |
| Sex (Male n/Female n) | 8/8 | 5/5 |
| Body mass (kg) | 75.2 ± 16.9 | 107.3 ± 21.0 |
| Systolic Blood Pressure (mmHg) | 150.0 ± 13.2 | 151.7 ± 24.5 |
| Diastolic Blood Pressure (mmHg) | 98.8 ± 15.2 | 84.9 ± 10.6 |
| Week | Duration | Day 1 (Monday) | Day 2 (Wednesday) |
|---|---|---|---|
| 1 | 60 min | Ball handling | Ball handling |
| 2 | 60 min | Cone Ball | Cone Ball |
| 3 | 60 min | Floorball | Circuit training |
| 4 | 60 min | Floorball | Circuit training |
| 5 | 60 min | Cone Ball | Floorball |
| 6 | 60 min | Cone Ball | Floorball |
| 7 | 60 min | Circuit training | Cone Ball |
| 8 | 60 min | Circuit training | Cone Ball |
| 9 | 60 min | Floorball | Cone Ball |
| 10 | 60 min | Floorball | Cone Ball |
| 11 | 60 min | Floorball | Circuit training |
| 12 | 60 min | Floorball | Circuit training |
| Chair Stand (s) | Five Rep (s) | Up and Go (s) | Bicep Curl (n) | Hand Grip (kg) | Six MWT (m) | |
|---|---|---|---|---|---|---|
| COPD | n = 12 | n = 12 | n = 12 | n = 12 | n = 12 | n = 2 |
| Pre | 14.9 ± 4.5 | 10.6 ± 3.1 | 6.3 ± 1.4 | 15.8 ± 3.8 | 32.7 ± 10.8 | 532.2 ± 51.5 |
| Post | 15.5 ± 5.2 | 10.1 ± 2.9 | 5.9 ± 1.3 * | 17.0 ± 3.7 * | 34.3 ± 12.3 | 539.8 ± 95.8 |
| ∆ (95% CI) | 0.6 (−1.0 to 2.2) | −0.5 (−1.6 to 0.6) | −0.5 (−0.8 to −0.1) | 1.2 (0.2 to 2.1) | 1.7 (−0.5 to 3.8) | 7.6 (−390.5 to 405.6) |
| p-value | 0.437 | 0.337 | 0.011 | 0.023 | 0.112 | 0.849 |
| T2DM | n = 16 | n = 16 | n = 16 | n = 16 | n = 16 | n = 8 |
| Pre | 14.6 ± 2.6 | 10.5 ± 1.9 | 5.8 ± 0.9 | 19.9 ± 5.4 | 33.1 ± 8.0 | 540.9 ± 75.5 |
| Post | 14.8 ± 2.7 | 10.2 ± 2.0 | 5.3 ± 0.9 ** | 20.6 ± 5.1 | 33.3 ± 9.9 | 560.2 ± 75.6 * |
| ∆ (95% CI) | 0.2 (−1.3 to 1.7) | −0.3 (−1.1 to 0.5) | −0.4 (−0.7 to −0.2) | 0.8 (−2.0 to 3.5) | 0.2 (−2.1 to 2.4) | 19.3 (1.3 to 37.2) |
| p-value | 0.795 | 0.478 | 0.005 | 0.570 | 0.862 | 0.040 |
| All | n = 28 | n = 28 | n = 28 | n = 28 | n = 28 | n = 10 |
| Pre | 14.8 ± 3.5 | 10.5 ± 2.5 | 6.0 ± 1.1 | 18.1 ± 5.1 | 32.9 ± 9.1 | 538.7 ± 66.9 |
| Post | 15.1 ± 3.9 | 10.1 ± 2.4 | 5.6 ± 1.1 *** | 19.1 ± 4.8 | 33.7 ± 10.8 | 555.1 ± 74.0 |
| ∆ (95% CI) | 0.4 (−0.7 to 1.4) | −0.4 (−1.0 to 0.2) | −0.5 (−0.7 to −0.3) | 1.0 (−0.6 to 2.5) | 0.8 (−0.7 to 2.3) | 16.3 (−2.7 to 35.4) |
| p-value | 0.483 | 0.223 | <0.001 | 0.228 | 0.272 | 0.082 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Atti, J.; Kissow, J.; Bangsbo, J. 12 Weeks of Supervised Team Sports in Danish Municipal Health Center Lowers Systolic Blood Pressure and Increases Performance in Hypertensive Chronic Obstructive Pulmonary Disease and Type 2 Diabetes Mellitus Patients. J. Funct. Morphol. Kinesiol. 2025, 10, 209. https://doi.org/10.3390/jfmk10020209
Atti J, Kissow J, Bangsbo J. 12 Weeks of Supervised Team Sports in Danish Municipal Health Center Lowers Systolic Blood Pressure and Increases Performance in Hypertensive Chronic Obstructive Pulmonary Disease and Type 2 Diabetes Mellitus Patients. Journal of Functional Morphology and Kinesiology. 2025; 10(2):209. https://doi.org/10.3390/jfmk10020209
Chicago/Turabian StyleAtti, Jesper, Julie Kissow, and Jens Bangsbo. 2025. "12 Weeks of Supervised Team Sports in Danish Municipal Health Center Lowers Systolic Blood Pressure and Increases Performance in Hypertensive Chronic Obstructive Pulmonary Disease and Type 2 Diabetes Mellitus Patients" Journal of Functional Morphology and Kinesiology 10, no. 2: 209. https://doi.org/10.3390/jfmk10020209
APA StyleAtti, J., Kissow, J., & Bangsbo, J. (2025). 12 Weeks of Supervised Team Sports in Danish Municipal Health Center Lowers Systolic Blood Pressure and Increases Performance in Hypertensive Chronic Obstructive Pulmonary Disease and Type 2 Diabetes Mellitus Patients. Journal of Functional Morphology and Kinesiology, 10(2), 209. https://doi.org/10.3390/jfmk10020209








