The Effects of Exercise and Kinesio Tape on Physical Limitations in Patients with Knee Osteoarthritis
Abstract
:1. Introduction
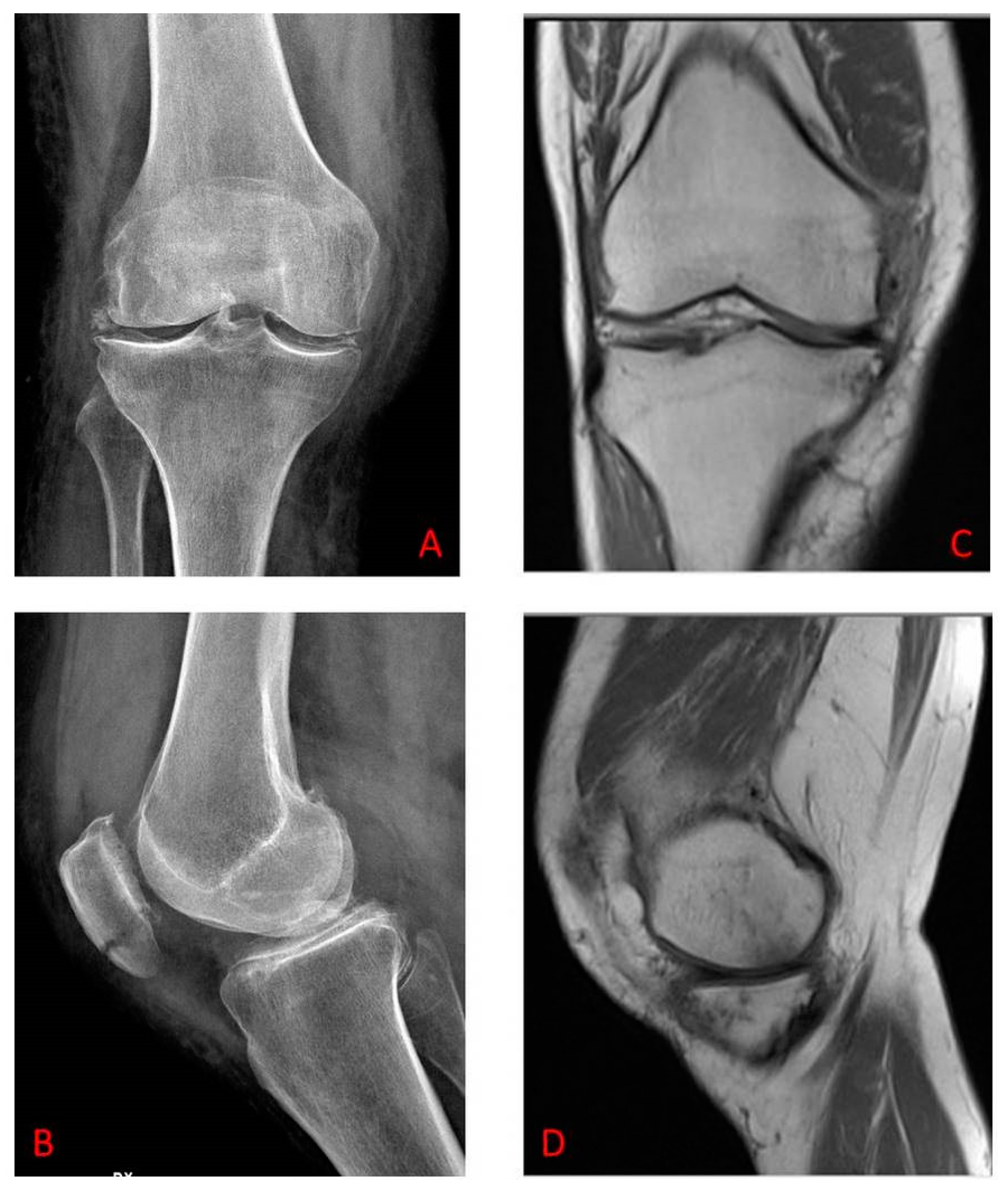
2. Materials and Methods
2.1. Patients
2.2. Sample Size Calculations
2.3. Study Protocol
2.4. Kinesio Tape Application
2.5. Exercise Protocol
2.6. Functional Test
2.7. Statistical Analysis
3. Results
3.1. Baseline Characteristics
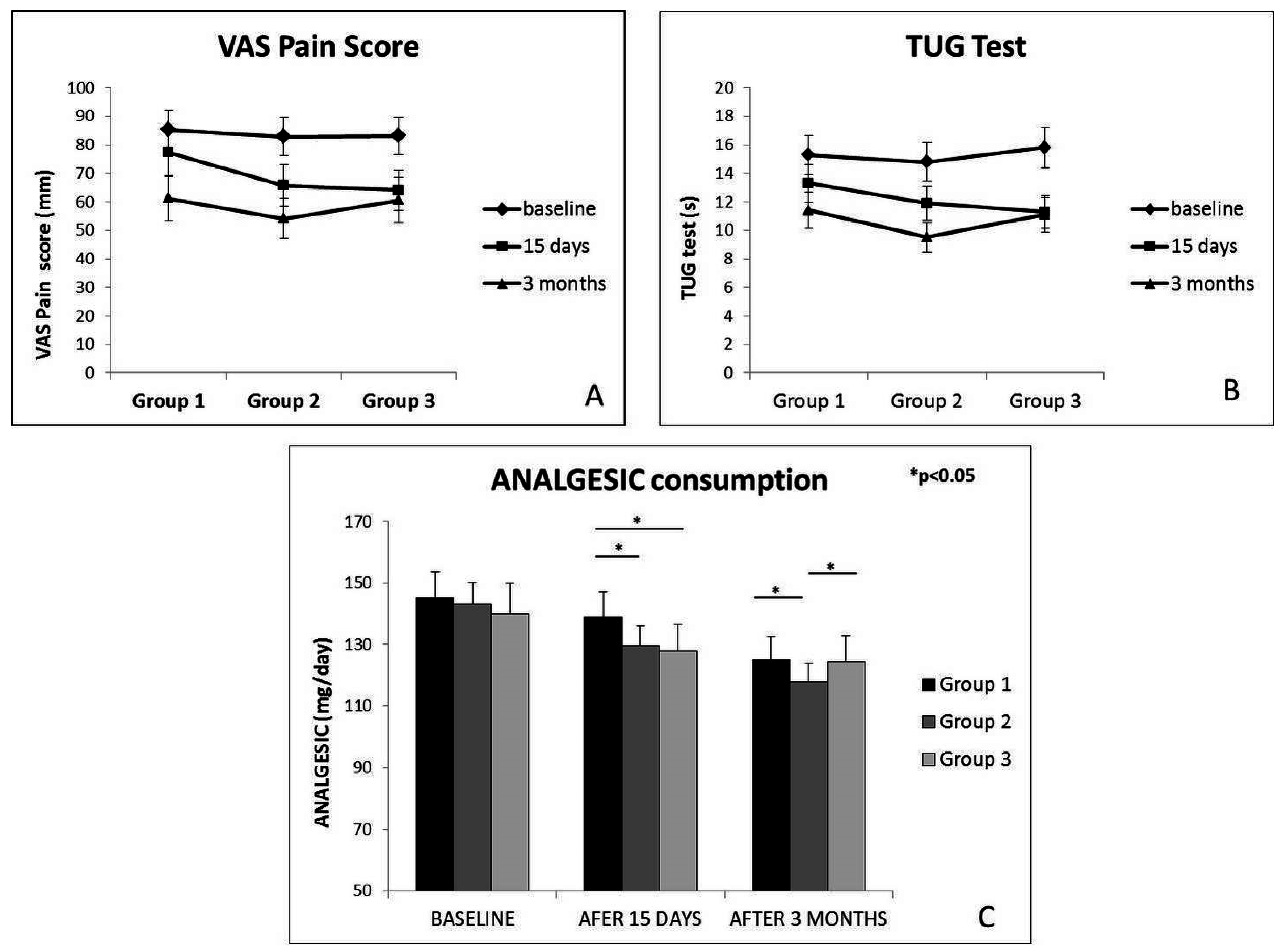
3.2. WOMAC Score
3.3. VAS Pain Score
3.4. TUG Test
3.5. Daily Amount of Analgesic Consumption
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| KT | kinesio taping |
| OA | osteoarthritis |
| WOMAC | Western Ontario and McMaster Universities Arthritis Index |
| VAS | Visual Analogue Scaling |
| TUG | Timed Up and Go |
References
- Huang, C.Y.; Hsieh, T.H.; Lu, S.C.; Su, F.C. Effect of the Kinesio tape to muscle activity and vertical jump performance in healthy inactive people. Biomed. Eng. Online 2011, 10, 70. [Google Scholar] [CrossRef] [PubMed]
- Aguilar-Ferrándiz, M.E.; Castro-Sánchez, A.M.; Matarán-Peñarrocha, G.A.; García-Muro, F.; Serge, T.; Moreno-Lorenzo, C. Effects of kinesio taping on venous symptoms, bioelectrical activity of the gastrocnemius muscle, range of ankle motion, and quality of life in postmenopausal women with chronic venous insufficiency: A randomized controlled trial. Arch. Phys. Med. Rehabil. 2013, 94, 2315–2328. [Google Scholar] [CrossRef] [PubMed]
- Williams, S.; Whatman, C.; Hume, P.A.; Sheerin, K. Kinesio taping in treatment and prevention of sports injuries: A meta-analysis of the evidence for its effectiveness. Sports Med. 2012, 42, 153–164. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.Y.; Kim, E.H.; Kim, J.; Yoon, Y.W. Kinesio taping improves pain, range of motion, and proprioception in older patients with knee osteoarthritis: A randomized controlled trial. Am. J. Phys. Med. Rehabil. 2015, 94, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Crossley, K.M.; Vicenzino, B.; Lentzos, J.; Schache, A.G.; Pandy, M.G.; Ozturk, H.; Hinman, R.S. Exercise, education, manual-therapy and taping compared to education for patellofemoral osteoarthritis: A blinded, randomised clinical trial. Osteoarthr. Cartil. 2015, 23, 1457–1464. [Google Scholar] [CrossRef] [PubMed]
- Mobasheri, A.; Kalamegam, G.; Musumeci, G.; Batt, M.E. Chondrocyte and mesenchymal stem cell-based therapies for cartilage repair in osteoarthritis and related orthopaedic conditions. Maturitas 2014, 78, 188–198. [Google Scholar] [CrossRef] [PubMed]
- Mobasheri, A.; Matta, C.; Zákány, R.; Musumeci, G. Chondrosenescence: Definition, hallmarks and potential role in the pathogenesis of osteoarthritis. Maturitas 2015, 80, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Musumeci, G.; Aiello, F.C.; Szychlinska, M.A.; Di Rosa, M.; Castrogiovanni, P.; Mobasheri, A. Osteoarthritis in the XXIst century: Risk factors and behaviours that influence disease onset and progression. Int. J. Mol. Sci. 2015, 16, 6093–6112. [Google Scholar] [CrossRef] [PubMed]
- Musumeci, G.; Szychlinska, M.A.; Mobasheri, A. Age-related degeneration of articular cartilage in the pathogenesis of osteoarthritis: Molecular markers of senescent chondrocytes. Histol. Histopathol. 2015, 30, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Giunta, S.; Castorina, A.; Marzagalli, R.; Szychlinska, M.A.; Pichler, K.; Mobasheri, A.; Musumeci, G. Ameliorative effects of PACAP against cartilage degeneration. Morphological, immunohistochemical and biochemical evidence from in vivo and in vitro models of rat osteoarthritis. Int. J. Mol. Sci. 2015, 16, 5922–5944. [Google Scholar] [CrossRef] [PubMed]
- Fransen, M.; McConnell, S.; Harmer, A.R.; van der Esch, M.; Simic, M.; Bennell, K.L. Exercise for osteoarthritis of the knee. Cochrane Database Syst. Rev. 2015, 1, CD004376. [Google Scholar] [PubMed]
- Knobloch, T.J.; Madhavan, S.; Nam, J.; Agarwal, S., Jr.; Agarwal, S. Regulation of chondrocytic gene expression by biomechanical signals. Crit. Rev. Eukaryot. Gene Expr. 2008, 18, 139–150. [Google Scholar] [CrossRef] [PubMed]
- Castrogiovanni, P.; Musumeci, G. Which is the best physical treatment for osteoarthritis? J. Funct. Morphol. Kinesiol. 2016, 1, 54–68. [Google Scholar] [CrossRef]
- Musumeci, G. The Effect of mechanical loading on articular cartilage. J. Funct. Morphol. Kinesiol. 2016, 1, 154–161. [Google Scholar] [CrossRef]
- Kalron, A.; Bar-Sela, S. A systematic review of the effectiveness of kinesio taping—Fact or fashion? Eur. J. Phys. Rehabil. Med. 2013, 49, 699–709. [Google Scholar] [PubMed]
- Anandkumar, S.; Sudarshan, S.; Nagpal, P. Efficacy of kinesio taping on isokinetic quadriceps torque in knee osteoarthritis: A double blinded randomized controlled study. Physiother. Theory Pract. 2014, 30, 375–383. [Google Scholar] [CrossRef] [PubMed]
- Halski, T.; Ptaszkowski, K.; Słupska, L.; Paprocka-Borowicz, M.; Dymarek, R.; Taradaj, J.; Bidzińska, G.; Marczyński, D.; Cynarska, A.; Rosińczuk, J. Short-term effects of kinesio taping and cross taping application in the treatment of latent upper trapezius trigger points: A prospective, single-blind, randomized, sham-controlled trial. Evid. Based Complement. Altern. Med. 2015, 2015, 191925. [Google Scholar] [CrossRef] [PubMed]
- Mutlu, E.K.; Mustafaoglu, R.; Birinci, T.; Razak Ozdincler, A. Does kinesio taping of the knee improve pain and functionality in patients with knee osteoarthritis? A randomized controlled clinical trial. Am. J. Phys. Med. Rehabil. 2016. [Google Scholar] [CrossRef]
- Kocyigit, F.; Turkmen, M.B.; Acar, M.; Guldane, N.; Kose, T.; Kuyucu, E.; Erdil, M. Kinesio taping or sham taping in knee osteoarthritis? A randomized, double-blind, sham-controlled trial. Complement. Ther. Clin. Pract. 2015, 21, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Song, C.Y.; Huang, H.Y.; Chen, S.C.; Lin, J.J.; Chang, A.H. Effects of femoral rotational taping on pain, lower extremity kinematics, and muscle activation in female patients with patellofemoral pain. J. Sci. Med. Sport 2015, 18, 388–393. [Google Scholar] [CrossRef] [PubMed]
- Chang, W.D.; Chen, F.C.; Lee, C.L.; Lin, H.Y.; Lai, P.T. Effects of kinesio taping versus mcconnell taping for patellofemoral pain syndrome. A systematic review and meta-analysis. Evid. Based Complement. Altern. Med. 2015, 2015, 471208. [Google Scholar] [CrossRef] [PubMed]
- Bennell, K.L.; Hinman, R.S.; Metcalf, B.R.; Buchbinder, R.; McConnell, J.; McColl, G.; Green, S.; Crossley, K.M. Efficacy of physiotherapy management of knee joint osteoarthritis, a randomised, double blind, placebo controlled trial. Ann. Rheum. Dis. 2005, 64, 906–912. [Google Scholar] [CrossRef] [PubMed]
- Musumeci, G.; Trovato, F.M.; Loreto, C.; Leonardi, R.; Szychlinska, M.A.; Castorina, S.; Mobasheri, A. Lubricin expression in human osteoarthritic knee meniscus and synovial fluid, a morphological, immunohistochemical and biochemical study. Acta Histochem. 2014, 116, 965–972. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Nuki, G.; Moskowitz, R.W.; Abramson, S.; Altman, R.D.; Arden, N.K.; Bierma-Zeinstra, S.; Brandt, K.D.; Croft, P.; Doherty, M.; et al. OARSI recommendations for the management of hip and knee osteoarthritis, part III, Changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthr. Cartil. 2010, 18, 476–499. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, L.; Hagen, K.B.; Bijlsma, J.W.; Andreassen, O.; Christensen, P.; Conaghan, P.G.; Doherty, M.; Geenen, R.; Hammond, A.; Kjeken, I.; et al. European League Against Rheumatism (EULAR). EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis. Ann. Rheum. Dis. 2013, 72, 1125–1135. [Google Scholar] [CrossRef] [PubMed]
- Angst, F.; Pap, G.; Mannion, A.F.; Herren, D.B.; Aeschlimann, A.; Schwyzer, H.K.; Simmen, B.R. Comprehensive assessment of clinical outcome and quality of life after total shoulder arthroplasty. Usefulness and validity of subjective outcome measurement. Arthritis Rheum. 2004, 51, 819–828. [Google Scholar] [CrossRef] [PubMed]
- Quintana, J.M.; Escobar, A.; Arostegui, I.; Bilbao, A.; Azkarate, J.; Goenaga, J.I.; Arenaza, J.C. Health-Related Quality of Life and Appropriateness of Knee or Hip Joint Replacement. Arch. Intern. Med. 2006, 166, 220–226. [Google Scholar] [CrossRef] [PubMed]
- Hawker, G.A.; Mian, S.; Kendzerska, T.; French, M. Measures of adult pain, Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res. 2011, 63, S240–S252. [Google Scholar]
- Erel, S.; Şimşek, İ.E.; Özkan, H. Analysis of the reliability and validity of the Turkish version of the intermittent and constant osteoarthritis pain questionnaire. Acta Orthop. Traumatol. Turc. 2015, 49, 508–512. [Google Scholar] [PubMed]
- Bohannon, R.W. Reference values for the timed up and go test, a descriptive meta-analysis. J. Geriatr. Phys. Ther. 2006, 29, 64–68. [Google Scholar] [CrossRef] [PubMed]
- Bennell, K.L.; Hinman, R.S.; Crossley, K.M.; Metcalf, B.R.; Buchbinder, R.; Green, S.; McColl, G. Is the Human Activity Profile a useful measure in people with knee osteoarthritis? J. Rehabil. Res. Dev. 2004, 41, 621–630. [Google Scholar] [CrossRef] [PubMed]
- Podsiadlo, D.; Richardson, S. The timed “Up & Go”, a test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [PubMed]
- Pichler, K.; Loreto, C.; Leonardi, R.; Reuber, T.; Weinberg, A.M.; Musumeci, G. In rat with glucocorticoid-induced osteoporosis, RANKL is downregulated in bone cells by physical activity (treadmill and vibration stimulation training). Histol. Histopathol. 2013, 28, 1185–1196. [Google Scholar] [PubMed]
- Musumeci, G.; Loreto, C.; Leonardi, R.; Castorina, S.; Giunta, S.; Carnazza, M.L.; Trovato, F.M.; Pichler, K.; Weinberg, A.M. The effects of physical activity on apoptosis and lubricin expression in articular cartilage in rats with glucocorticoid-induced osteoporosis. J. Bone Miner. Metab. 2013, 31, 274–284. [Google Scholar] [CrossRef] [PubMed]
- Musumeci, G.; Trovato, F.M.; Imbesi, R.; Castrogiovanni, P. Effects of dietary extra-virgin olive oil on oxidative stress resulting from exhaustive exercise in rat skeletal muscle: A morphological study. Acta. Histochem. 2014, 116, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Musumeci, G.; Trovato, F.M.; Pichler, K.; Weinberg, A.M.; Loreto, C.; Castrogiovanni, P. Extra-virgin olive oil diet and mild physical activity prevent cartilage degeneration in an osteoarthritis model. An “in vivo” and “in vitro” study on lubricin expression. J. Nutr. Biochem. 2013, 24, 2064–2075. [Google Scholar] [CrossRef] [PubMed]
- Musumeci, G. The effects of exercise on physical limitations and fatigue in rheumatic diseases. World J. Orthop. 2015, 6, 762–769. [Google Scholar] [CrossRef] [PubMed]
- Leeuwenburgh, C.; Heinecke, J.W. Oxidative stress and antioxidants in exercise. Curr. Med. Chem. 2001, 8, 829–838. [Google Scholar] [CrossRef] [PubMed]
- Page, C.J.; Hinman, R.S.; Bennell, K.L. Physiotherapy management of knee osteoarthritis. Int. J. Rheum. Dis. 2011, 14, 145–151. [Google Scholar] [CrossRef] [PubMed]
- Abulhasan, J.F.; Snow, M.D.; Anley, C.M.; Bakhsh, M.; Grey, M.J. An extensive evaluation of different knee stability assessment measures, a systematic review. J. Funct. Morphol. Kinesiol. 2016, 1, 209–229. [Google Scholar] [CrossRef]
- Yusuf, E.; Kortekaas, M.C.; Watt, I.; Huizinga, T.W.; Kloppenburg, M. Do knee abnormalities visualised on MRI explain knee pain in knee osteoarthritis? A systematic review. Ann. Rheum. Dis. 2011, 70, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Hochberg, M.C.; Altman, R.D.; April, K.T.; Benkhalti, M.; Guyatt, G.; McGowan, J.; Towheed, T.; Welch, V.; Wells, G.; Tugwell, P. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res. 2012, 64, 465–474. [Google Scholar] [CrossRef]
- Musumeci, G.; Loreto, C.; Imbesi, R.; Trovato, F.M.; di Giunta, A.; Lombardo, C.; Castorina, S.; Castrogiovanni, P. Advantages of exercise in rehabilitation, treatment and prevention of altered morphological features in knee osteoarthritis. A narrative review. Histol. Histopathol. 2014, 29, 707–719. [Google Scholar] [PubMed]
- Knoop, J.; Dekker, J.; van der Leeden, M.; van der Esch, M.; Thorstensson, C.A.; Gerritsen, M.; Voorneman, R.E.; Peter, W.F.; de Rooij, M.; Romviel, S.; et al. Knee joint stabilization therapy in patients with osteoarthritis of the knee, a randomized, controlled trial. Osteoarthr. Cartil. 2013, 21, 1025–1034. [Google Scholar] [CrossRef] [PubMed]
- Musumeci, G.; Castrogiovanni, P.; Trovato, F.M.; Imbesi, R.; Giunta, S.; Szychlinska, M.A.; Loreto, C.; Castorina, S.; Mobasheri, A. Moderate physical activity ameliorates cartilage degeneration in a rat model of aging, a study on lubricin expression. Scand. J. Med. Sci. Sports 2015, 25, e222–e230. [Google Scholar] [CrossRef] [PubMed]
- Richette, P.; Sautreuil, P.; Coudeyre, E.; Chevalier, X.; Revel, M.; Rannou, F. Usefulness of taping in lower limb osteoarthritis. French clinical practice guidelines. Jt. Bone Spine 2008, 75, 475–478. [Google Scholar] [CrossRef] [PubMed]


| Baseline Characteristics | Group 1 | Group 2 | Group 3 | p-Value |
|---|---|---|---|---|
| Gender | n.s. | |||
| Female | 8 | 10 | 9 | |
| Male | 11 | 9 | 10 | |
| Age (year) | 63.90 ± 15.4 | 64.20 ± 14.5 | 64.80 ± 14.2 | n.s. |
| Height (cm) | 163.5 ± 11.5 | 162.8 ± 12.2 | 165.1 ± 9.9 | n.s. |
| Weight (kg) | 73.2 ± 22.8 | 71.8 ± 24.2 | 74.5 ± 21.5 | n.s. |
| Grade of OA | n.s. | |||
| II | 9 | 8 | 9 | |
| III | 10 | 11 | 10 | |
| Involvement | n.s. | |||
| Right-side | 6 | 7 | 6 | |
| Left-side | 7 | 6 | 6 | |
| Bilateral | 6 | 6 | 7 | |
| Presence of comorbidities | n.s. | |||
| None | 19 | 19 | 19 | |
| Total | 19 | 19 | 19 |
| Test | Group | Baseline | After 15 Days | After 3 Months | p (Baseline vs. after 15 Days) | p (Baseline vs. after 3 Months) | p (After 15 Days vs. after 3 Months) | |
|---|---|---|---|---|---|---|---|---|
| WOMAC Score (mean ± SD) | Group 1 | Pain | 40.3 ± 4.03 | 37.0 ± 3.88 | 33.3 ± 3.10 | * | * | * |
| Stiffness | 40.9 ± 3.69 | 38.1 ± 3.20 | 31.6 ± 2.22 | * | * | * | ||
| Function | 41.6 ± 3.32 | 37.8 ± 2.50 | 35.0 ± 1.52 | * | * | * | ||
| Group 2 | Pain | 41.5 ± 2.53 | 33.2 ± 1.93 | 28.3 ± 0.93 | * | * | n.s. | |
| Stiffness | 42.1 ± 3.19 | 29.3 ± 2.10 | 28.7 ± 1.72 | * | * | n.s. | ||
| Function | 40.3 ± 4.82 | 34.1 ± 2.00 | 32.8 ± 1.02 | * | * | n.s. | ||
| Group 3 | Pain | 41.2 ± 3.23 | 32.8 ± 2.63 | 31.5 ± 1.63 | * | * | n.s. | |
| Stiffness | 40.5 ± 3.89 | 28.9 ± 1.40 | 30.9 ± 1.42 | * | * | n.s. | ||
| Function | 40.9 ± 2.52 | 35.8 ± 1.70 | 34.9 ± 1.72 | * | * | n.s. | ||
| VAS Pain Score (mm) (mean ± SD) | Group 1 | 85.3 ± 7.03 | 77.3 ± 6.88 | 61.1 ± 7.87 | * | * | * | |
| Group 2 | 82.9 ± 5.87 | 65.8 ± 5.25 | 54.1 ± 5.09 | * | * | * | ||
| Group 3 | 83.1 ± 8.65 | 64.1 ± 4.95 | 60.6 ± 5.91 | * | * | n.s. | ||
| TUG Test (s) (mean ± SD) | Group 1 | 15.3 ± 1.03 | 13.3 ± 1.08 | 11.4 ± 1.01 | * | * | * | |
| Group 2 | 14.8 ± 1.60 | 11.9 ± 2.70 | 9.5 ± 1.60 | * | * | * | ||
| Group 3 | 15.8 ± 2.05 | 11.3 ± 2.00 | 11.1 ± 0.99 | * | * | n.s. | ||
| Analgesic (mg/day) (mean ± SD) | Group 1 | 145.0 ± 8.54 | 138.9 ± 7.47 | 125.1 ± 6.89 | * | * | * | |
| Group 2 | 143.0 ± 6.57 | 129.5 ± 5.95 | 117.9 ± 6.02 | * | * | * | ||
| Group 3 | 140.0 ± 8.03 | 127.7 ± 6.99 | 124.3 ± 6.96 | * | * | n.s. | ||
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castrogiovanni, P.; Di Giunta, A.; Guglielmino, C.; Roggio, F.; Romeo, D.; Fidone, F.; Imbesi, R.; Loreto, C.; Castorina, S.; Musumeci, G. The Effects of Exercise and Kinesio Tape on Physical Limitations in Patients with Knee Osteoarthritis. J. Funct. Morphol. Kinesiol. 2016, 1, 355-368. https://doi.org/10.3390/jfmk1040355
Castrogiovanni P, Di Giunta A, Guglielmino C, Roggio F, Romeo D, Fidone F, Imbesi R, Loreto C, Castorina S, Musumeci G. The Effects of Exercise and Kinesio Tape on Physical Limitations in Patients with Knee Osteoarthritis. Journal of Functional Morphology and Kinesiology. 2016; 1(4):355-368. https://doi.org/10.3390/jfmk1040355
Chicago/Turabian StyleCastrogiovanni, Paola, Angelo Di Giunta, Claudia Guglielmino, Federico Roggio, Domenico Romeo, Federica Fidone, Rosa Imbesi, Carla Loreto, Sergio Castorina, and Giuseppe Musumeci. 2016. "The Effects of Exercise and Kinesio Tape on Physical Limitations in Patients with Knee Osteoarthritis" Journal of Functional Morphology and Kinesiology 1, no. 4: 355-368. https://doi.org/10.3390/jfmk1040355
APA StyleCastrogiovanni, P., Di Giunta, A., Guglielmino, C., Roggio, F., Romeo, D., Fidone, F., Imbesi, R., Loreto, C., Castorina, S., & Musumeci, G. (2016). The Effects of Exercise and Kinesio Tape on Physical Limitations in Patients with Knee Osteoarthritis. Journal of Functional Morphology and Kinesiology, 1(4), 355-368. https://doi.org/10.3390/jfmk1040355