1. Introduction
Gender dysphoria is characterized by the clinically significant distress that stems from an incongruence between an individual’s experienced gender identity and their sex assigned at birth [
1]. This condition is estimated to affect 0.5% of the global population, which translates to approximately 25 million people. For a significant number of transmasculine and gender-diverse individuals, the presence of breasts serves as a primary source of this dysphoria, leading to considerable social, physical, and psychological difficulties [
2]. This profound distress frequently leads to compensatory behaviors, most notably chest binding, to conceal the female-like thoracic contour. Although this practice can offer temporary psychological comfort, it is often linked to adverse physical effects, such as skin rashes, acne, limitations on physical activity, and in some cases, respiratory issues [
3]. Moreover, the long-term use of binders can have a detrimental effect on skin elasticity and cause stromal fibrosis, which not only complicates future surgical procedures but can also negatively affect the final esthetic results [
4]. As a precursor to surgery, gender-affirming hormone therapy (GAHT) is frequently the initial medical step, inducing desired physical transformations and enhancing quality of life (QoL) [
2,
5]. For many individuals, this can serve as preparation for chest affirmation surgery; however, transition pathways are highly individualized, and not all transmasculine or non-binary people pursue the same steps, sequence, or surgical procedures.
In this context, gender-affirming mastectomy, commonly known as “top surgery,” stands as a fundamental component of transgender healthcare [
6]. For many transmasculine individuals, it is the first, and occasionally the only, surgical intervention they seek, underscoring its pivotal role in their affirmation journey [
6].
While the overall effectiveness of chest masculinization is widely recognized, there is a gap in the literature concerning technical adjustments for patients with unique anatomical features or esthetic preferences that differ from a conventional masculine chest. A notable surgical challenge is the management of large breast volumes on lean body frames, where achieving a natural and proportional contour demands precise planning to prevent an unnatural look [
7].
Several previous case series have described the psychological outcomes of gender-affirming mastectomy in individual patients or small cohorts [
8,
9]. However, most of these studies have primarily focused on binary masculinization outcomes, without examining patient-centered goals such as the pursuit of an esthetic androgynous chest [
8,
9].
We present a novel case report detailing the successful achievement of an androgynous esthetic in a tall, lean patient with significant breast volume, offering a contribution to the field’s growing need for individualized surgical strategies. The present case provides an original contribution by integrating a multimodal psychological and physical performance assessments with a focus on individualized esthetic objectives, highlighting how these dimensions interact in shaping postoperative adjustment and identity integration. Moreover, this study aims to provide a comprehensive review of the current literature on the profound psychological impact of gender-affirming mastectomy.
2. Methods
We present a case of a 23-year-old transgender man, assigned female at birth (AFAB), undergoing GAHT and gender-affirming surgery with particular emphasis on the psychological impact of bilateral mastectomy.
Secondarily, a comprehensive review of the literature on this specific issue was conducted examining publications from January 2000 through June 2025 using PubMed, the Cochrane Library, and the Web of Science database. Specific keywords used in the search were: “transgender men”, “transgender male”, “female-to-male”, “FTM”, “assigned female at birth”, “gender-diverse individuals”, “gender incongruence”, “gender dysphoria”. These keywords were paired with keywords related to surgical procedure and psychological impact: “gender-affirming surgery”, “top surgery”, “mastectomy”, “chest masculinization surgery”, “bilateral mastectomy”, “gender-confirming surgery”, “psychological well-being”, “mental health”, “body image”, “quality of life”, “depression”, “anxiety”, “self-esteem”, “emotional outcomes”, “psychosocial impact”.
Two independent reviewers (G.S., M.C.Z.) screened the titles and abstracts of all selected articles. No specific inclusion or exclusion criteria were initially applied at the study design. The full texts of the selected articles were reviewed, and incongruities were resolved by a third author (A.A.) to confirm consistency in study selection. Citation tracking was also performed on the bibliographies of articles selected for review, which identified additional relevant literature. Studies were selected based on rigorous inclusion criteria to ensure high-quality evidence. We included only those publications that provided detailed surgical outcome reporting and psychological outcome measurements using validated assessment tools. Special attention was given to studies that included patients with varied body habitus and breast volumes, as these factors significantly influence surgical planning and outcomes. The main thematic areas of interest were identified, and data were summarized and discussed for each specific area. Data were analyzed qualitatively and presented in a narrative and structured fashion. No attempt to perform a quantitative analysis was made.
3. Case Report
A 23-year-old transgender male patient, AFAB, first presented to the Gender Incongruence Outpatient Clinic at the “Renato Dulbecco” University Hospital of Catanzaro for evaluation related to gender dysphoria. The patient reported a longstanding incongruence between his assigned sex at birth and his experienced gender identity, which had been a source of significant psychological distress since adolescence. This suffering manifested as persistent emotional distress, pervasive feelings of inadequacy, social withdrawal, and marked anticipatory anxiety in gendered and body-exposing contexts. The patient reported chronic avoidance of situations requiring chest exposure, persistent shame linked to bodily incongruence, and significant functional impairments in peer interactions and intimate relationships. These difficulties extended to self-esteem regulation and identity development.
At the time of the initial assessment (T0), the patient reported a stable psychosocial background and denied any significant medical or psychiatric history. Developmental milestones were achieved appropriately, and psychomotor development was reported as within normal limits. He reported regular menstrual cycles and no use of hormonal treatments prior to presentation.
On physical examination, the patient was found to be overweight, with a body mass index (BMI) of 28.1 kg/m2 (weight: 89 kg; height: 178 cm). No abnormalities were noted on systemic examination.
Following a comprehensive evaluation conducted by the multidisciplinary team, a diagnosis of gender dysphoria was established by our trained psychiatrist (C.S.G.) in accordance with the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria [
1]. The patient met the diagnostic threshold due to the presence of a strong and persistent identification with the male gender, a marked discomfort with secondary sex characteristics, and a desire for gender-affirming medical and surgical interventions.
During clinical interviews, the patient expressed a clear and consistent desire to undergo hormone therapy and gender-affirming chest surgery (bilateral mastectomy), which he perceived as crucial for aligning his physical appearance with his gender identity and alleviating gender-related distress.
The patient described a persistent depressed mood, marked anhedonia, significant fatigue, and sleep disturbances during late adolescence, fulfilling several DSM-5 criteria for a moderate depressive episode [
1]. Importantly, these symptoms were attributed not to the transgender identity itself, but to the distress stemming from the incongruence between gender identity and physical embodiment. This distinction is essential in avoiding the medicalization of transgender identities and framing the psychological distress within a context of lived incongruence. In this context, the role of the mental health professional extended beyond diagnostic assessment, encompassing a supportive function throughout the patient’s journey. Psychological support was conceived as a space for reflection, identity integration, and empowerment, reinforcing the therapeutic alliance in the broader framework of gender affirmation.
Throughout the clinical pathway, the patient maintained a collaborative and trusting relationship with the multidisciplinary healthcare team. Attendance at follow-up appointments exceeded 95%, and adherence to hormonal therapy and lifestyle recommendations remained consistently high. The patient actively participated in shared decision-making and reported perceiving the healthcare team as a secure base during the transition journey, which likely facilitated psychological resilience and treatment adherence.
3.1. Endocrinological Management
A tailored treatment plan was established, beginning with GAHT. Informed consent was obtained for all procedures, and the patient demonstrated full understanding of the risks, benefits, and expected outcomes.
As part of the comprehensive care plan, the patient was advised to follow a hypocaloric Mediterranean diet combined with regular physical activity, to optimize metabolic parameters and support overall well-being during medical transition. Testosterone therapy was initiated and monitored closely, according to previously published data [
5]. Treatment regimens were adjusted based on serum total testosterone levels and hematocrit trends, in accordance with international guidelines [
10]. During the first six months, the patient received 250 mg testosterone intramuscularly every 3 weeks. In the following three months, the interval was extended to every 4 weeks. Subsequently, therapy was transitioned to testosterone undecanoate 1000 mg intramuscularly every 12 weeks, which was better tolerated and more convenient for long-term maintenance.
Throughout this period, the patient experienced progressive masculinizing changes, including voice deepening, increased muscle mass, and cessation of menses. Regular follow-up visits allowed for the evaluation of clinical response and laboratory monitoring, with no significant adverse effects reported.
3.2. Surgical Procedures
After two years of hormonal therapy, the patient (age 25) underwent chest masculinization surgery with a specific desire for androgynous esthetic results. At the time of surgery, he presented a height of 178 cm and weight of 65 kg (BMI 20.5 kg/m
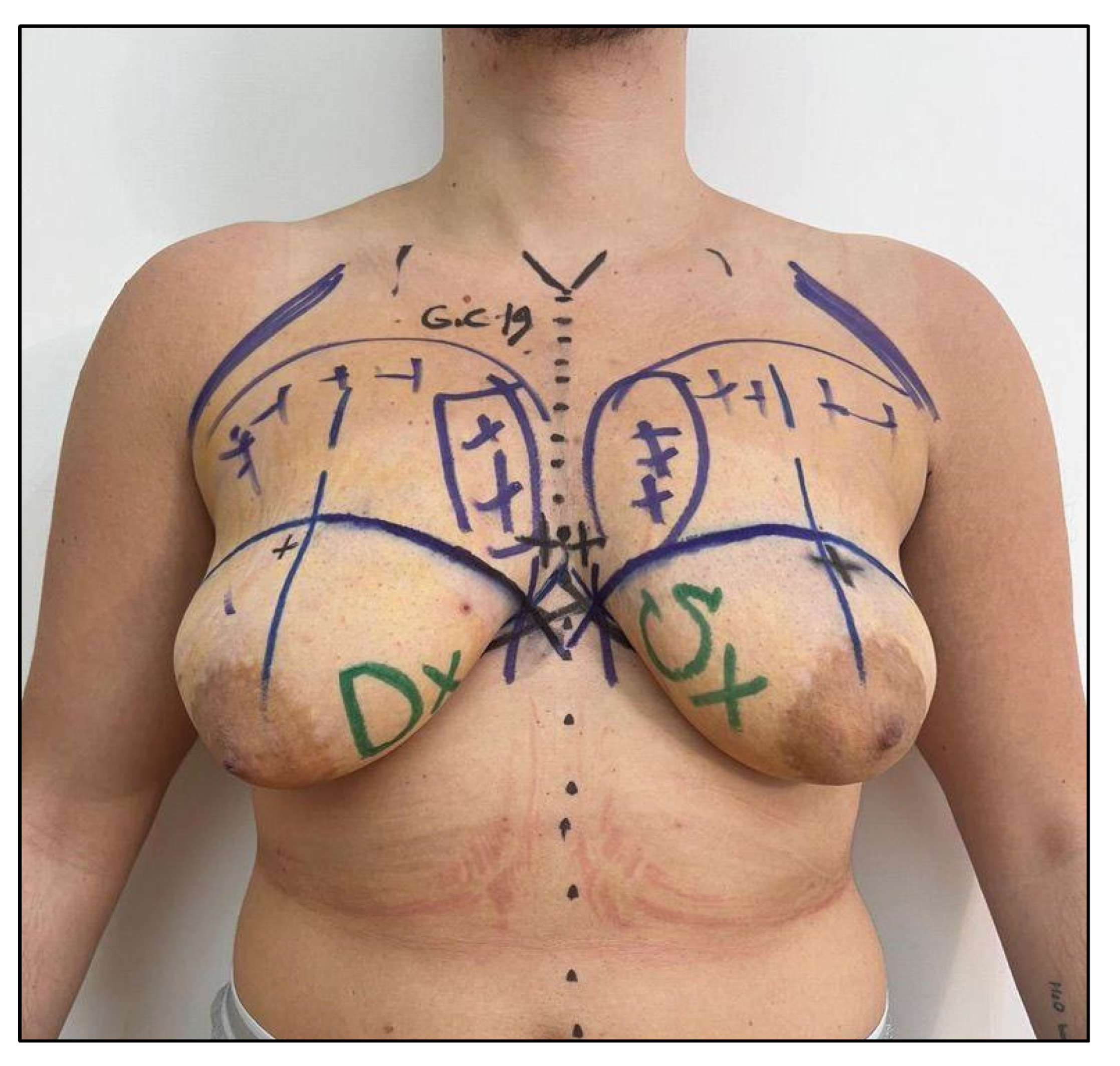
2). The patient displayed a characteristically tall, lean frame that required special consideration in surgical planning. The preoperative assessment revealed bilateral breast tissue measuring 400 mL each (cup size 40C), presenting a significant volume requiring careful management to achieve the desired outcome (
Figure 1).
Initial physical examination demonstrated several favorable factors for surgery. The patient’s breast tissue was symmetrically distributed with good skin elasticity, and notably, there was no significant ptosis despite the considerable breast volume. The tall, lean frame provided good overall proportions that would facilitate achieving natural-appearing chest contours.
The surgical technique chosen involved radical mastectomy with free nipple grafting, rather than nipple–areola complex preservation on a pedicle. This decision was made based on the significant breast volume (400 mL bilateral) and the desire to achieve optimal chest wall contouring. The nipples were harvested, trimmed to appropriate size, and grafted in anatomically optimal positions determined by preoperative marking and intraoperative assessment (
Figure 2). Preoperative markings were carefully designed and documented (
Figure 2), with specific attention to the patient’s unique anatomical characteristics.
The surgical procedure involved complete bilateral tissue removal of the 400 mL breast volume. Meticulous attention was paid to chest wall contouring, with the final esthetic refinements carefully adapted to the patient’s unique frame. The free nipple grafts were positioned to create a natural-appearing, androgynous chest esthetic that harmonized with the patient’s overall body proportions. Additionally, muscular sculpture (MS) of the chest was performed to improve the virilization of the patient according to our previous procedures [
11].
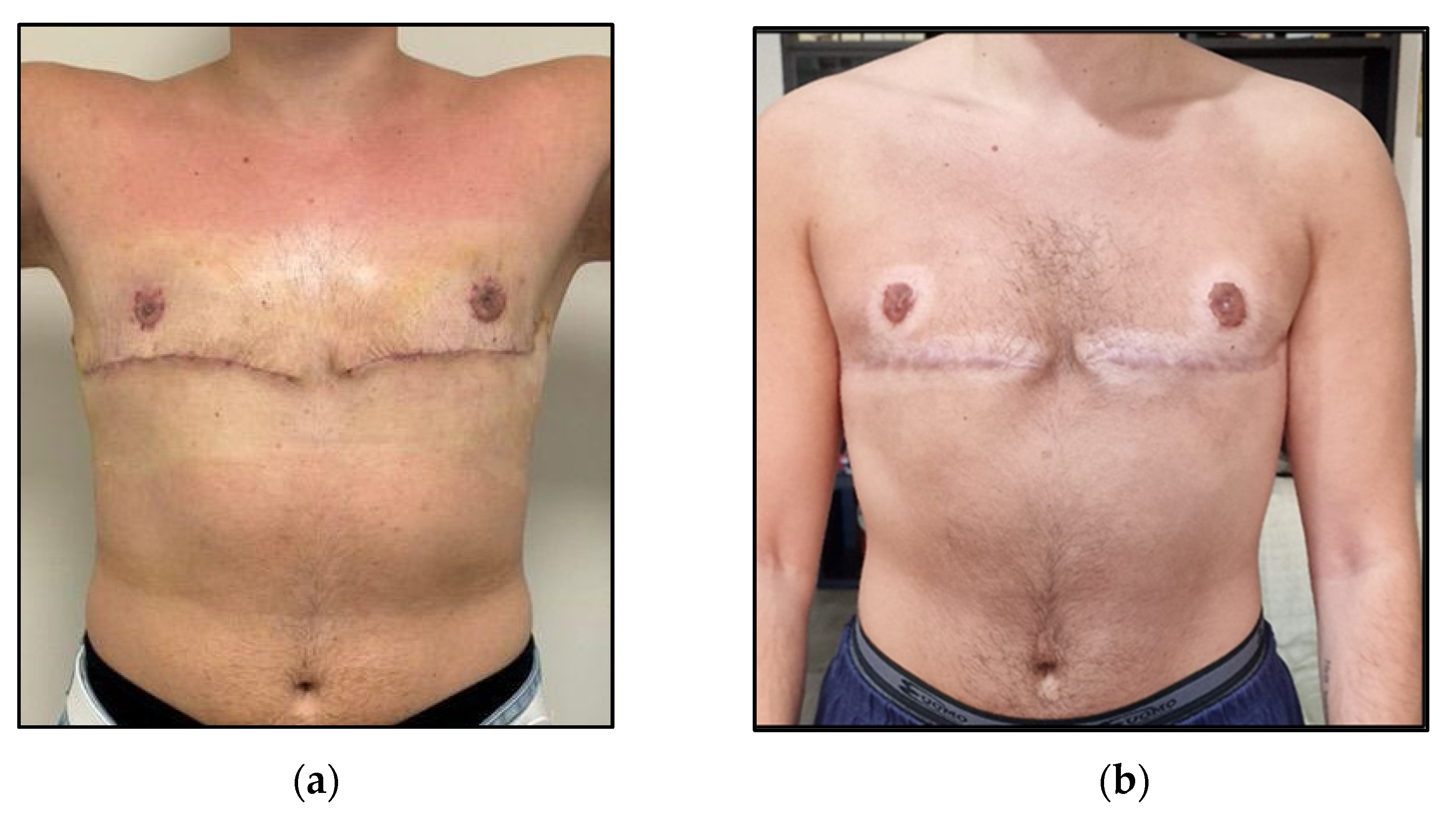
The postoperative course proved remarkably successful, with excellent esthetic outcomes achieved at one-month and 12 months follow-up (
Figure 3). The final chest wall contour demonstrated natural proportions that complemented the patient’s height and frame, with no complications encountered throughout the recovery period. The free nipple grafts healed completely with good retention of color and position.
3.3. Physical Performance Assessment
Physical performance evaluation was conducted before undergoing GAHT (T0), one week before surgery (two years after the start of GAHT) (T1) and 6 months post-surgery (T2). The following tests were administered:
The Handgrip strength (HG) test was performed on the dominant upper limb to evaluate the maximum isometric strength of the hand and forearm muscles using a Jamar hydraulic hand dynamometer [
12]. The participant was instructed to contract as hard as possible for three seconds maintaining the elbow at right angles. Three trials were performed, and the best one was considered for the result.
30 s chair stand test (30-CST) was used to evaluate lower limb muscular performance [
13]. The participant was asked to stand up and sit down as many consecutive times as possible. The number of times (i.e., repetitions) the patient comes to a full standing position in 30 s was recorded.
The one-repetition maximum (1RM) bench press protocol was used to assess dynamic muscle strength [
14]. The protocol used included the estimated 1RM bench press, calculated as the maximum weight lifted by applying Brzycki formula [
15].
HG showed progressive improvement across all time points. Lower limb performance, measured via the 30-CST, improved from T0 to T1, with a slight decrease at T2. Dynamic upper body strength, assessed using the estimated 1 RM bench press, increased significantly from 35.0 kg at T0 to 56.6 kg at T1, followed by a moderate reduction to 50.0 kg at T2.
These results suggest a general improvement in physical performance over time, particularly in upper body strength, with minor fluctuations potentially related to the surgical intervention and recovery phase.
3.4. Psychological and Neuropsychological Assessment
Psychological and neuropsychological assessments were conducted one week before surgery (T1), 6 months (T2) and 12 months after surgery (T3), using a multimethod approach combining psychometric and projective tools, aimed at capturing the complexity of body image integration and self-perception after gender-affirming mastectomy.
The following standardized instruments were administered:
The Body Uneasiness Test (BUT) to quantitatively assess body-related distress, dysmorphic concerns, and discomfort with specific body areas. This allowed for the measurement of somatoperceptive dysregulation commonly reported in transgender individuals undergoing transition [
16].
The Marlowe–Crowne Social Desirability Scale (MC-SDS) (33-item version) to evaluate the tendency to respond in a socially acceptable or idealized manner. This tool served as a control variable for the interpretation of self-reported emotional and body-related responses [
17].
The Human Figure Drawing Test (DFH), administered in two consecutive tasks: the first involved drawing a human figure freely, and the second invited the patient to draw a self-representation as perceived six months after the surgical intervention. This projective technique was used to explore implicit aspects of the embodied self, emotional resonance with physical transformation, and the subjective integration of the new body image [
18]. Drawings were analyzed through a clinical projective framework, focusing on structural organization, body part salience, graphical consistency, and implicit gender identity cues. Interpretation of the DFH was conducted within a psychodynamic and clinical-phenomenological framework, focusing on the symbolic expression of unconscious body representations, affective embodiment, and pre-verbal dimensions of self-image. Differences between the first and second figure provided insight into the degree of internalized bodily congruence, visibility of identity markers, and affective embodiment post-surgery. Although the DFH is not classified among standardized psychometric tools within evidence-based diagnostic systems, its inclusion in the present study is methodologically justified by the exploratory and integrative design adopted (
Appendix A).
The assessment was embedded within a therapeutic relationship oriented toward affective regulation, gender identity consolidation, and the reconstruction of a coherent self-narrative following medical transition.
Results of standardized tests are summarized in
Table 2 and discussed below. Drawings of DFH are shown in
Figure S1.
3.4.1. Body Uneasiness Test (BUT)
The extremely high score at T1 indicates severe generalized body discomfort, consistent with experiences of gender dysphoria, body shame, and somatic rejection. Social avoidance, dysmorphic ideation, and significant distress related to the chest area (breasts) are likely present. The significant reduction (from 143 to 124) at T2 indicates initial improvement, though levels of discomfort remain high. It is plausible that the body is undergoing a process of re-elaboration, intended as a dynamic and progressive psychological reorganization of body image. Finally, at T3 (12 months post-surgery), the score drops dramatically to 17, falling within a range of psychophysical well-being. This value suggests an almost complete resolution of body discomfort, with acceptance, recognition, and integration of the post-transition male body. It is a strong indicator of identity coherence between internal self-image and physical form.
The trajectory of the scores highlights a complete transformative process, where thoracic surgery has triggered a positive reconstruction of body image. This finding is fully consistent with what was observed in the DFH and the clinical narrative. The BUT documents a clear evolution from dysphoric distress to bodily and psychological well-being, reinforcing the clinical effectiveness of gender-affirming mastectomy in improving self-image.
3.4.2. Marlowe–Crowne Social Desirability Scale (MC-SDS)
The slight but consistent increase in scores may reflect social adaptation mechanisms and identity defenses activated within the context of transition. It is important to consider that, despite a body that is now integrated (as shown by the BUT), the regulation of social image remains active—perhaps as a residue of previous vulnerability or as a result of exposure to internalized masculine norms. The MC-SDS reveals a growing tendency to control how one is perceived by others, which does not negate the well-being achieved but calls for clinical monitoring of deeper relational and identity dimensions, even in the post-transition phase.
The increase to 18 at T2 suggests greater social desirability, likely linked to the need for external validation during the transition phase. At this stage, the need to be recognized in the new gender role and the pressure to conform to socially accepted models of masculinity may intensify. The score of 20 at T3, while still within the normal range, indicates a persistent inclination toward social approval. However, it does not appear pathological. At this stage, the individual may manage their responses with greater control, perhaps to maintain a coherent image of a ‘successful man’ after the transition. This should be interpreted alongside the marked improvement shown in the BUT.
3.4.3. Human Figure Drawing Test (DFH)
At T
1, the drawing illustrated prominently shaded breasts, thick and disproportionate lower limbs, and arms with repeated outlines (
Figure S1). The figure was faceless, with undefined hands and no visible genitalia. The image evoked a fragmented and dysphoric body perception, with overemphasis on the chest suggesting an intrusive and alien bodily region. The lack of facial detail implied a dissociation from identity, and the body’s mass appeared to carry a weight of incongruence.
Six months after surgery (T
2), the second figure reflected a flatter chest, narrower waist, and more athletic limbs (
Figure S1). Shoulders were broader, and the musculature was lightly indicated. While the face was again absent, the entire body showed greater balance and cohesion. The drawing exhibited cleaner contours and symmetrical posture. Compared to the first, there was a significant reduction in dysphoric traits and a shift toward masculine embodiment.
Finally, at T
3, the drawing presented a flat chest, muscular limbs and stable stance (
Figure S1). Although the face remained unexpressed, the overall composition communicated a stable and integrated male identity. This drawing no longer showed signs of internal conflict or dissonance, and instead reflected a quiet ownership of the body, consistent with psychological and physical affirmation.
The progression across the three figures demonstrates a symbolic narrative of transformation: from dysphoria, dis-identification, and fragmentation (T1), to emerging congruence and structure (T2), to internalized masculine embodiment and self-coherence (T3). This trajectory reflects the psychological adaptation measured though the BUT.
4. Review of the Literature
The therapeutic effectiveness of gender-affirming mastectomy is well-established, supported by a strong body of evidence that shows high safety profiles and exceptionally high patient satisfaction. Data from systematic reviews and large-scale studies consistently indicate satisfaction rates above 90%. For instance, a comprehensive review involving 1324 patients reported an overall satisfaction rate of 96.8% [
19]. Similarly, a recent Brazilian study documented a marked increase in satisfaction with both chest and nipple appearance following the surgery [
20]. This widespread satisfaction is further supported by the extremely low incidence of surgical regret reported in the literature (median Decision Regret Scale score 0.0 (IQR 0.0-0.0), on a 100-point scale) [
19,
21].
This becomes especially critical when a patient desires an androgynous esthetic, compelling the surgeon to adopt a more nuanced, artistic, and patient-guided strategy that transcends standard binary anatomical models. This shift in patient objectives signifies a new frontier in gender-affirming surgery, requiring advanced surgical planning and execution to address established risks, like hematoma, while delivering highly customized outcomes [
22].
The significant psychological advantages of this surgery have been rigorously measured using validated patient-reported outcome measures (PROMs). A pivotal prospective study employed the BREAST-Q and the BUT, revealing statistically significant improvements after surgery in several key-areas [
23]. These included satisfaction with breasts, psychosocial well-being and sexual well-being, in addition to a substantial decrease in overall body-related distress [
23].
A prospective study evaluated 21 trans men preoperatively and at 4 and 12 months postoperatively [
24]. BREAST-Q and Body Exposure during Sexual Activities Questionnaire were used to assess the potential improvement in body awareness during sexual intercourse. Results showed significant improvements in psychological well-being, chest satisfaction, and body awareness during sexual intercourse as early as 4 months after surgery [
24]. Interestingly, nipple–areolar complex sensitivity recovery, evaluated though the Semmes-Weinstein monofilament, did not correlate with improvements in sexual well-being [
24].
Another prospective study on 111 transmasculine and non-binary adults used validated PROMs including BREAST-Q, BODY-Q, Body Image Quality of Life Inventory (BIQLI), Transgender Congruence Scale, Patient Health Questionnaire (PHQ)-9, and General Anxiety Disorder-7 (GAD-7) [
25]. The results showed significant post-mastectomy psychological benefits, such as notable improvements in psychosocial and sexual well-being, increased gender congruence, and substantial reductions in depression and anxiety) [
25]. Although hypertrophic scarring was relatively common, overall patient satisfaction remained high, underscoring the therapeutic effectiveness of the procedure in improving mental health and quality of life in transmasculine and non-binary individuals [
25].
Similarly, a prospective cohort study conducted in the USA evaluated 70 transmasculine individuals both preoperatively and six months postoperatively [
26]. The analysis demonstrated statistically significant improvements in depressive symptoms and anxiety symptoms. Additionally, notable enhancements were observed in psychosocial functioning, sexual functioning and overall body image [
26]. The mean patient satisfaction rate regarding surgical outcomes was 93.1%. Collectively, these findings underscore the therapeutic benefit of chest surgery in this population, highlighting its positive effects on mental health that transcend solely physical appearance [
26].
These results are corroborated by recent meta-analyses, which confirm that gender-affirming surgeries yield significant and lasting enhancements in mental health and overall quality of life [
27]. The consistent reporting of such positive results across various patient groups, surgical methods, and evaluation tools reinforces the classification of this procedure as a medically necessary intervention, not merely an elective one [
20,
28].
The same positive outcomes appear to be confirmed in younger transmasculine populations. A recent single-institution longitudinal study conducted in the USA evaluated the impact of gender-affirming care, including top surgery, on mental health and treatment outcomes in transmasculine and nonbinary adolescents and young adults [
29]. Outcomes were measured using the PHQ-2, chest and gender dysphoria scales, and surgical satisfaction scales. Results showed significant reductions in depressive symptoms and dysphoria following surgery [
29]. Participants reported high satisfaction with surgical outcomes and recovery, often contributing to the reduction in suicidal ideation. Another qualitative study evaluated 30 transmasculine individuals aged 13–21; nearly half had undergone masculinizing chest surgery [
30]. Participants described severe psychological and physical burdens related to chest dysphoria, which were not alleviated by testosterone alone. Those who received mastectomy reported near-complete resolution of dysphoria, no regret, and marked improvements in quality of life and functioning [
30].
The growing sophistication of this field is evident in the evolution of outcome assessment methods. Initial evaluations relied on generic quality of life instruments, like the Short-Form Health Survey (SF-36), or adapted body-part-specific tools such as the BREAST-Q and BODY-Q [
22,
28,
31]. More recently, the focus has shifted to highly specialized, transgender-specific questionnaires. Although early research using these adapted instruments was vital for establishing initial evidence, it was constrained by language and concepts not specifically designed for the transgender population, such as questions regarding bra fit [
32]. A significant step forward has been the creation of validated tools like the TRANS-Q and the Essen Transidentity Quality of Life Inventory (ETLI) [
32,
33,
34]. These instruments are tailored to capture the unique aspects of the transgender experience, evaluating areas like gender congruence, satisfaction with appearance both clothed and unclothed, and the effects of living openly as a transgender individual. This advancement in methodology marks a shift towards a more patient-centric approach to care, aiming to validate and quantify the outcomes that are most meaningful to the lived realities of transgender people [
28,
32].
Long-term data on gender-affirming mastectomy remain limited, particularly for trans men. In a follow-up study of patients treated between 1970 and 1990, transmasculine participants reported sustained improvements in body congruence, especially in relation to chest [
35]. Mental health outcomes also improved, with reduced suicidal ideation and resolution of gender dysphoria–related comorbidities. No regrets were reported, suggesting durable benefits in trans men over decades [
35].
5. Discussion
Gender dysphoria is increasingly understood as an embodied form of distress rather than a purely cognitive mismatch between assigned and self-identified gender. Neuropsychological models highlight dysregulation in the interoceptive–affective network—responsible for bodily self-awareness and emotional salience—as a key contributor [
36,
37]. In this context, interventions that realign the body with gender identity, such as gender-affirming surgery, may help re-establish affective and perceptual coherence [
38,
39].
Our clinical case supports this view. Through a longitudinal, multimodal assessment, we observed that the most psychologically transformative event was not the initiation of hormone therapy or physical performance changes, but the gender-affirming mastectomy. This surgical intervention catalyzed a symbolic and emotional realignment between body image and internal identity, leading to a more stable, integrated masculine self-perception. The surgery functioned not merely as a physical correction but as a therapeutic turning point.
Improvements in physical performance, especially upper body strength, contributed to gender congruence by reinforcing bodily control and authenticity. Though not perceived as transformative as surgery, these gains complemented the embodiment process, enhancing confidence and alignment with the internal body schema.
Body image and gender congruence evolved together as the patient integrated a physical form congruent with his affirmed gender. Literature supports this trajectory, showing that chest masculinization increases psychological well-being, reduces fear of misgendering, and facilitates social interactions [
40].
In our case, careful surgical planning, attentive to both anatomical and esthetic goals, supported this process. In particular, this case represents the first reported application of MS [
11] in a transgender individual. Shared decision-making ensured alignment with identity aspirations and psychosocial expectations especially at one-year follow-up from surgery, probably due to highly satisfying pectoral MS. Research has consistently shown that satisfaction with chest reconstruction is closely linked to individualized esthetic embodiments and the degree of perceived congruence between one’s gender identity and bodily appearance [
41].
From a psychological perspective, mastectomy not only relieved dysphoria but restructured the patient’s relationship with his body [
42]. Postoperative assessments showed marked improvements in body image and symbolic self-representation. The DFH evolved from fragmented to integrated, the BUT score improved significantly, and MC-SDS scores suggested a growing attention to social perception during identity consolidation. One-year post-surgery, the patient exhibited stable body image satisfaction and integrated gender identity. The combination of reduced dysphoric detachment, increased control over bodily presentation, and affective congruence revealed the deep impact of surgical embodiment. Thus, surgery represented the event with the greatest symbolic and perceptual impact, but it was embedded within a broader process of identity reconstruction, made possible by a therapeutic alliance and a coherent autobiographical narrative.
Finally, social desirability and esthetic norms remain influential. Some patients may feel pressured to conform to binary ideals. In this case, tailored surgical outcomes aligned with the patient’s personal body map, supporting authenticity over conformity. Personalized approaches reduce internalized distress and support well-being. This finding may reflect a strengthening of identity and a desire to control one’s public image, but it could also signal an adaptation to new normative masculine standards.
To better capture these dynamics, the integration of quantitative, projective, and relational tools is essential. Instruments such as the Transgender Congruence Scale or Gender Minority Stress and Resilience Measure may further enrich outcome evaluation. Overall, gender-affirming sculptured mastectomy should be recognized not only for its clinical efficacy but also for its identity-affirming potential within holistic care pathways.
6. Conclusions
In conclusion, this case report underscores the importance of gender-affirming surgery as a psychologically transformative process that supports the alignment of gender identity and body image, while helping to maintain physical performance and improve self-perception. In the present case, while GAHT and functional changes contributed to the alignment process, it was the surgical intervention that marked the most profound shift in the patient’s psychological trajectory. Through a multidimensional evaluation incorporating projective and quantitative tools, we demonstrated how chest masculinization, especially by applying the MS technique, can reduce interoceptive–affective dissonance and foster a stable, embodied masculine identity.
These findings highlight the significant role that gender-affirming surgeries can play within transgender healthcare, with implications that extend beyond physical congruence to emotional and social dimensions, within the broader context of diverse and individualized transition trajectories.