Dynamic Navigated “Sandwich” Technique: A Novel Surgical Approach for Safe Osteotomies in the Rehabilitation of an Atrophic Posterior Mandible: A Case Report
Abstract
1. Introduction
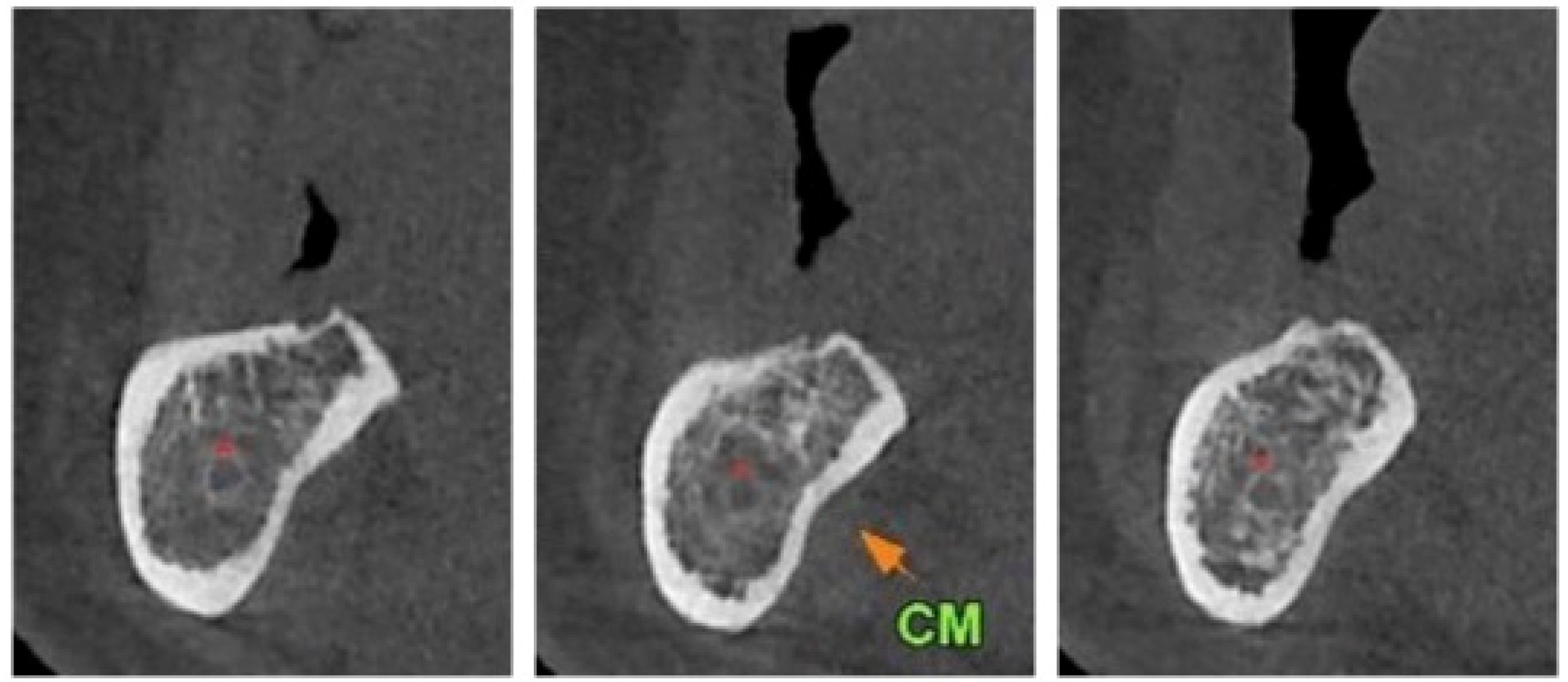
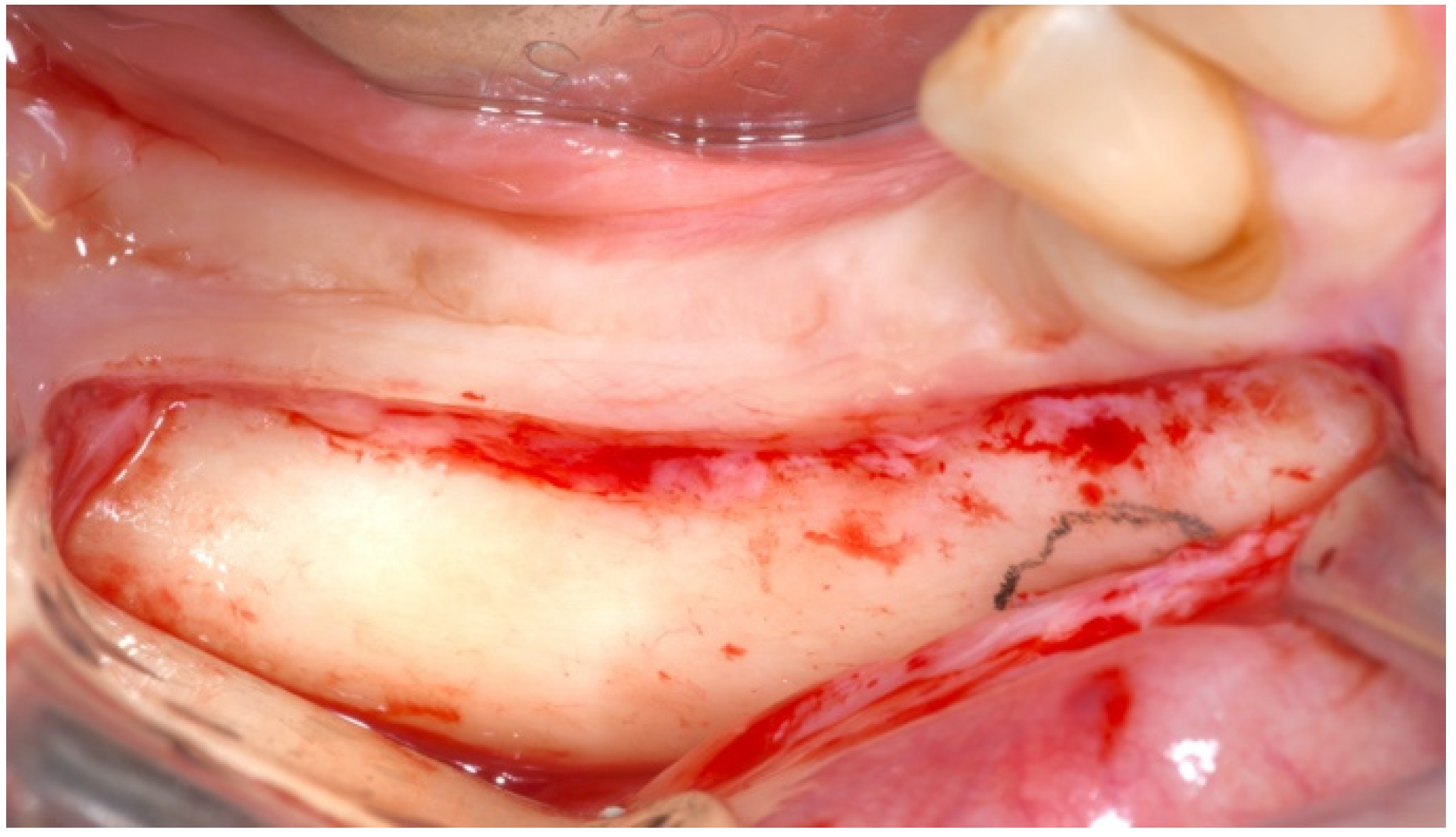
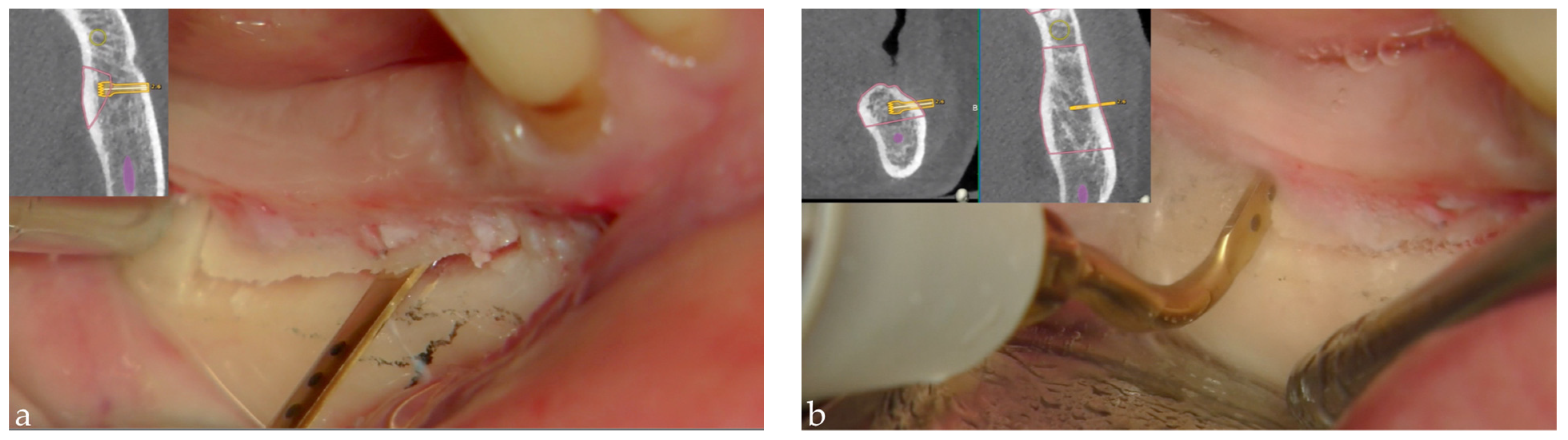
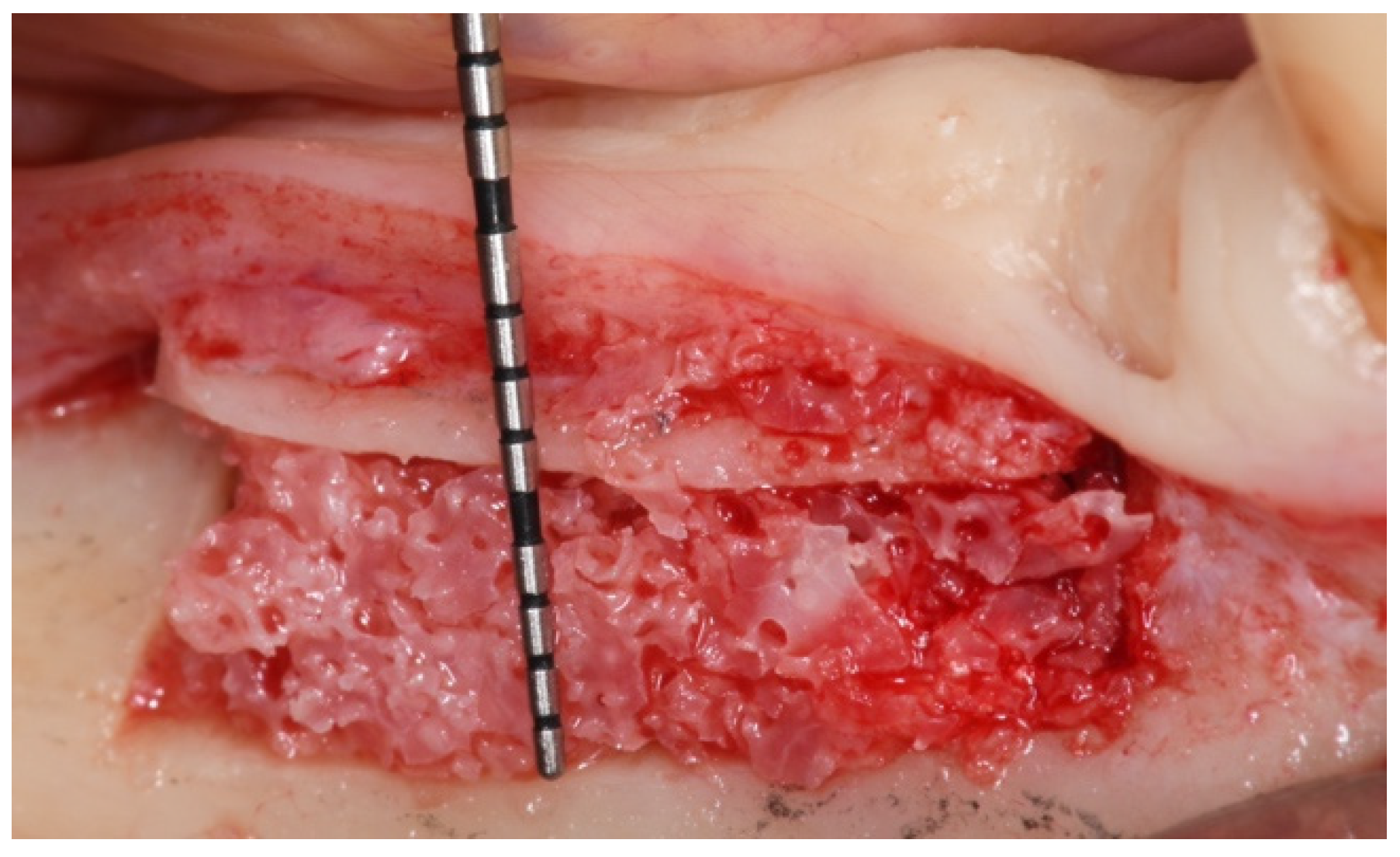
2. Materials and Methods
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Chiapasco, M.; Casentini, P.; Zaniboni, M. Bone Augmentation Procedures in Implant Dentistry. Int. J. Oral Maxillofac. Implant. 2009, 24, 237–259. [Google Scholar]
- Esposito, M.; Grusovin, M.G.; Felice, P.; Karatzopoulos, G.; Worthington, H.V.; Coulthard, P. The efficacy of horizontal and vertical bone augmentation procedures for dental implants-A Cochrane systematic review. Eur. J. Oral Implantol. 2009, 2, 167–184. [Google Scholar] [PubMed]
- Schettler, D. Sandwich-technic with cartilage transplant for raising the alveolar process in the lower jaw. Fortschr. Kiefer Gesichtschir. 1976, 20, 61–63. [Google Scholar] [PubMed]
- Stoelinga, P.J.W.; Tidemann, J.S.; Berger, H.; de Koonen, A. Interpositional bone graft augmentation of the atrophic mandible. J. Oral Surg. 1978, 36, 30–32. [Google Scholar]
- Zins, J.E.; Kusiak, J.F.; Whitaker, L.A. The influence of the recipient site on bone grafts to the face. Plast. Reconstr. Surg. 1984, 73, 371–381. [Google Scholar] [CrossRef]
- Misch, C.M.; Misch, C.E.; Resnik, R.R.; Ismail, Y.H. Reconstruction of maxillary alveolar defects with mandibular symphysis grafts for dental implants: A preliminary procedural report. Int. J. Oral Maxillofac. Implant. 1992, 7, 360–366. [Google Scholar]
- Felice, P.; Marchetti, C.; Iezzi, G.; Piattelli, A.; Worthington, H.; Pellegrino, G.; Esposito, M. Vertical ridge augmentation of the atrophic posterior mandible with interpositional bloc grafts: Bone from the iliac crest vs. bovine anorganic bone. Clinical and histological results up to one year after loading from a randomized-controlled clinical trial. Clin. Oral Implant. Res. 2009, 20, 1386–1393. [Google Scholar] [CrossRef]
- Block, M.S.; Emery, R.W.; Lank, K.; Ryan, J. Implant Placement Accuracy Using Dynamic Navigation. Int. J. Oral Maxillofac. Implant. 2017, 32, 92–99. [Google Scholar] [CrossRef]
- Felice, P.; Barausse, C.; Zucchelli, G.; Piattelli, M.; Ippolito, D.R. Interpositional Augmentation Technique in the Treatment of Posterior Mandibular Atrophies: A Retrospective Study Comparing 129 Autogenous and Heterologous Bone Blocks with 2 to 7 Years Follow-Up. Int. J. Period. Rest. Dent. 2017, 37, 469–480. [Google Scholar] [CrossRef]
- Esposito, M.; Buti, J.; Barausse, C.; Gasparro, R.; Sammartino, G.; Felice, P. Short implants versus longer implants in vertically augmented atrophic mandibles: A systematic review of randomised controlled trials with a 5-year post- loading follow-up. Int. J. Oral Implantol. 2019, 12, 267–280. [Google Scholar]
- Felice, P.; Barausse, C.; Pistilli, R.; Ippolito, D.R.; Esposito, M. Short implants versus longer implants in vertically augmented posterior mandibles: Result at 8 years after loading from a randomised controlled trial. Eur. J. Oral Implantol. 2018, 11, 385–395. [Google Scholar]
- Barausse, C.; Maranesi, T.; Pistilli, R.; Felice, P. Short implants: An alternative to bone augmentation in atrophic patients. Dental. Cadmos. 2017, 85, 485–499. (In Italian) [Google Scholar] [CrossRef]
- Bolle, C.; Felice, P.; Barausse, C.; Pistilli, V.; Trullenque-Eriksson, A.; Esposito, M. 4 mm long vs longer implants in augmented bone in posterior atrophic jaws: 1-year post-loading results from a multi-centre randomised controlled trial. Eur. J. Oral Implantol. 2018, 11, 31–47. [Google Scholar] [PubMed]
- Esposito, M.; Barausse, C.; Pistilli, R.; Piattelli, M.; Di Simone, S.; Ippolito, D.R.; Felice, P. Posterior atrophic jaws rehabilitated with prostheses supported by 5 × 5 mm implants with a nanostructured calcium-incorporated titanium surface or by longer implants in augmented bone. Five-year results from a randomised controlled trial. Eur. J. Oral Implantol. 2019, 12, 39–54. [Google Scholar]
- Felice, P.; Barausse, C.; Pistilli, R.; Ippolito, D.R.; Esposito, M. Five-year results from a randomised controlled trial comparing prostheses supported by 5-mm long implants or by longer implants in augmented bone in posterior atrophic edentulous jaws. Int. J. Oral Implantol. 2019, 12, 25–37. [Google Scholar]
- Felice, P.; Pistilli, R.; Barausse, C.; Piattelli, M.; Buti, J.; Esposito, M. Posterior atrophic jaws rehabilitated with prostheses supported by 6-mm-long 4-mm-wide implants or by longer implants in augmented bone. Five-year post-loading results from a within-person randomised controlled trial. Int. J. Oral Implantol. 2019, 12, 57–72. [Google Scholar]
- Esposito, M.; Barausse, C.; Pistilli, R.; Checchi, V.; Diazzi, M.; Gatto, M.R.; Felice, P. Posterior jaws rehabilitated with partial prostheses supported by 4.0 × 4.0 mm or by longer implants: Four-month post-loading data from a randomised controlled trial. Eur. J. Oral Implantol. 2015, 8, 221–230. [Google Scholar]
- Felice, P.; Barausse, C.; Pistilli, R.; Spinato, S.; Bernardello, F. Guided “Sandwich” Technique: A Novel Surgical Approach for Safe Osteotomies in the Treatment of Vertical Bone Defects in the Posterior Atrophic Mandible: A Case Report. Implant. Dent. 2014, 23, 738–744. [Google Scholar] [CrossRef]
- Lamazza, L.; Garreffa, G.; Laurito, D.; Lollobrigida, M.; Palmieri, L.; De Biase, A. Temperature Values Variability in Piezoelectric Implant Site Preparation: Differences between Cortical and Corticocancellous Bovine Bone. BioMed Res. Int. 2016, 2016, 6473680. [Google Scholar] [CrossRef][Green Version]
- Stefanelli, L.; De Groot, B.; Lipton, D.; Mandelaris, G. Accuracy of a Dynamic Dental Implant Navigation System in a Private Practice. Int. J. Oral Maxillofac. Implants. 2019, 34, 205–213. [Google Scholar] [CrossRef]
- Kaewsiri, D.; Panmekiate, S.; Subbalekha, K.; Mattheos, N.; Pimkhaokham, A. The accuracy of static vs. dynamic computer-assisted implant surgery in single tooth space: A randomized controlled trial. Clin. Oral Implant. Res. 2019, 30, 505–514. [Google Scholar] [CrossRef]
- Franchina, A.; Stefanelli, L.V.; Gorini, S.; Fedi, S.; Lizio, G.; Pellegrino, G. Digital Approach for the Rehabilitation of the Edentulous Maxilla with Pterygoid and Standard Implants: The Static and Dynamic Computer-Aided Protocols. Methods Protoc. 2020, 3, 84. [Google Scholar] [CrossRef] [PubMed]
- Pellegrino, G.; Pavanelli, F.; Ferri, A.; Lizio, G.; Parulli, R.; Marchetti, C. Ultrasonic Navigation for the Treatment of Medication-Related Jaw Osteonecrosis Involving the Inferior Alveolar Nerve: A Case Report and Protocol Review. Methods Protoc. 2020, 3, 70. [Google Scholar] [CrossRef]
- Pellegrino, G.; Taraschi, V.; Zacchino, A.; Ferri, A.; Marchetti, C. Dynamic navigation: A prospective clinical trial to evaluate the accuracy of implant placement. Int. J. Comput. Dent. 2019, 22, 139–147. [Google Scholar]
- Ferrini, F.; Capparé, P.; Vinci, R.; Gherlone, E.F.; Sannino, G. Digital versus Traditional Workflow for Posterior Maxillary Rehabilitations Supported by One Straight and One Tilted Implant: A 3-Year Prospective Comparative Study. BioMed Res. Int. 2018, 2018, 4149107. [Google Scholar] [CrossRef] [PubMed]
- Polizzi, E.; Tetè, G.; Bova, F.; Pantaleo, G.; Gastaldi, G.; Capparè, P.; Gherlone, E. Antibacterial properties and side effects of chlorhexidinebased mouthwashes. A prospective, randomized clinical study. J. Osseointegration. 2020, 12, 230. [Google Scholar]
- Felice, P.; Bertacci, A.; Bonifazi, L.; Karaban, M.; Canullo, L.; Pistilli, R.; Sammartino, P.; Gasparro, R.; Barausse, C. A proposed protocol for ordinary and extraordinary hygienic maintenance in different implant prosthetic scenarios. Appl. Sci. 2021, 11, 2957. [Google Scholar] [CrossRef]
- Parisi, M.R.; Tecco, S.; Gastaldi, G.; Polizzi, E.; D’Amicantonio, T.; Negri, S.; Gardini, I.; Schlusnus, K.; Gherlone, E.; Capparè, P.; et al. Point-of-care testing for hepatitis C virus infection at alternative and high-risk sites: An Italian pilot study in a dental clinic. New Microbiol. 2017, 40, 242–245. [Google Scholar]
- Vinci, R.; Rebaudi, A.; Capparè, P.; Gherlone, E. Microcomputed and histologic evaluation of calvarial bone grafts: A pilot study in humans. Int. J. Periodontics Restor. Dent. 2011, 31, e29–e36. [Google Scholar]
- Traini, T.; Piattelli, A.; Caputi, S.; Degidi, M.; Mangano, C.; Scarano, A.; Perrotti, V.; Iezzi, G. Regeneration of human bone using different bone substitute biomaterials. Clin. Implant. Dent. Relat Res. 2015, 17, 150–162. [Google Scholar] [CrossRef] [PubMed]
- Sberna, M.T.; Rizzo, G.; Zacchi, E.; Capparè, P.; Rubinacci, A. A preliminary study of the use of peripheral quantitative computed tomography for investigating root canal anatomy. Int. Endod. J. 2009, 42, 66–75. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Felice, P.; Bonifazi, L.; Karaban, M.; Berti, C.; Pellegrino, G.; Barausse, C. Dynamic Navigated “Sandwich” Technique: A Novel Surgical Approach for Safe Osteotomies in the Rehabilitation of an Atrophic Posterior Mandible: A Case Report. Methods Protoc. 2021, 4, 34. https://doi.org/10.3390/mps4020034
Felice P, Bonifazi L, Karaban M, Berti C, Pellegrino G, Barausse C. Dynamic Navigated “Sandwich” Technique: A Novel Surgical Approach for Safe Osteotomies in the Rehabilitation of an Atrophic Posterior Mandible: A Case Report. Methods and Protocols. 2021; 4(2):34. https://doi.org/10.3390/mps4020034
Chicago/Turabian StyleFelice, Pietro, Lorenzo Bonifazi, Maryia Karaban, Cesare Berti, Gerardo Pellegrino, and Carlo Barausse. 2021. "Dynamic Navigated “Sandwich” Technique: A Novel Surgical Approach for Safe Osteotomies in the Rehabilitation of an Atrophic Posterior Mandible: A Case Report" Methods and Protocols 4, no. 2: 34. https://doi.org/10.3390/mps4020034
APA StyleFelice, P., Bonifazi, L., Karaban, M., Berti, C., Pellegrino, G., & Barausse, C. (2021). Dynamic Navigated “Sandwich” Technique: A Novel Surgical Approach for Safe Osteotomies in the Rehabilitation of an Atrophic Posterior Mandible: A Case Report. Methods and Protocols, 4(2), 34. https://doi.org/10.3390/mps4020034







