Dynamic Macronutrient Meal-Equivalent Menu Method: Towards Individual Nutrition Intervention Programs
Abstract
1. Introduction
2. Methodology
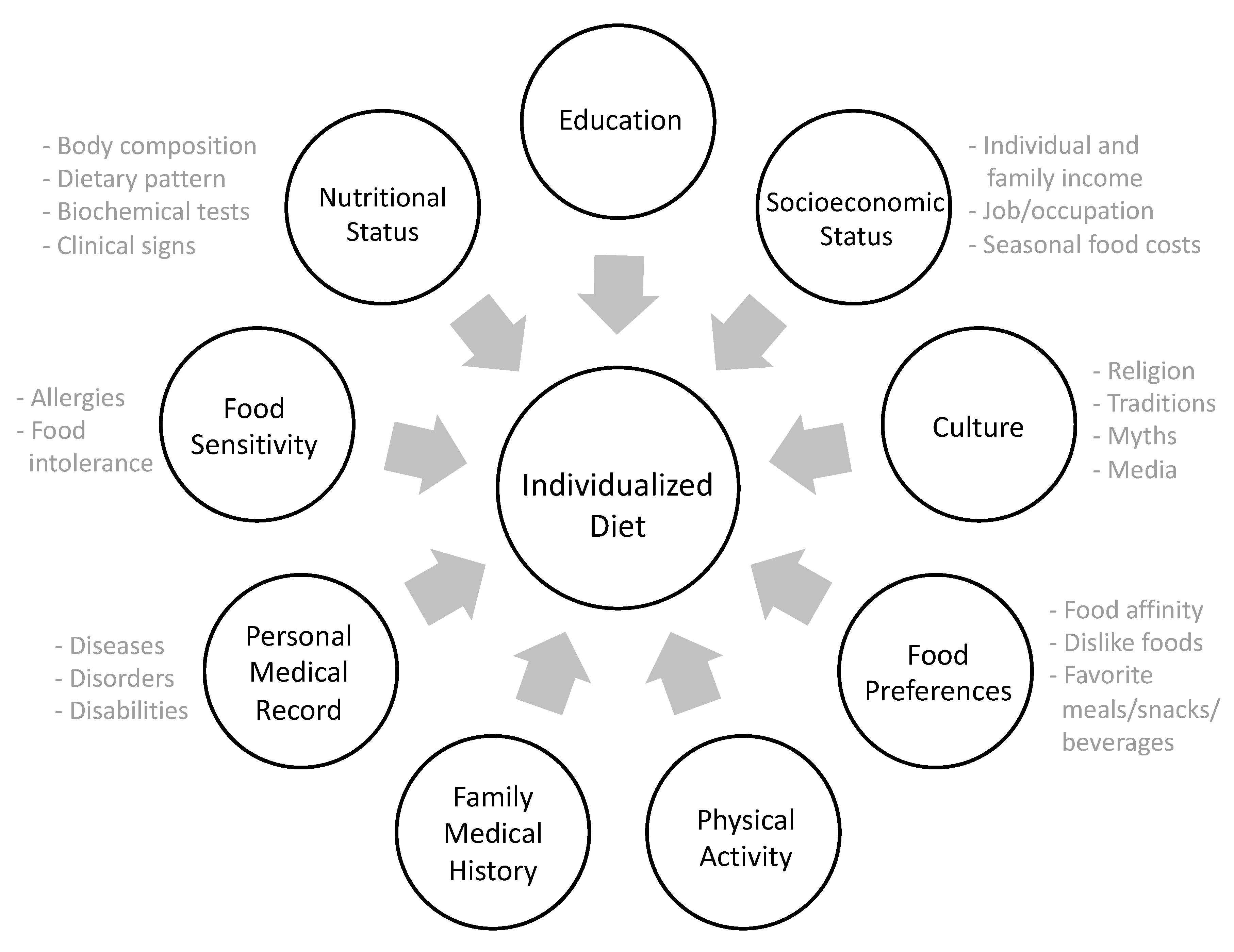
2.1. Understanding Individuals and Involving Them in the Process
2.2. Individualized Macronutrient Meal-Equivalent Menu Method as Part of the Nutrition Care Process
2.3. Energy and Macronutrient Distribution
3. Analysis
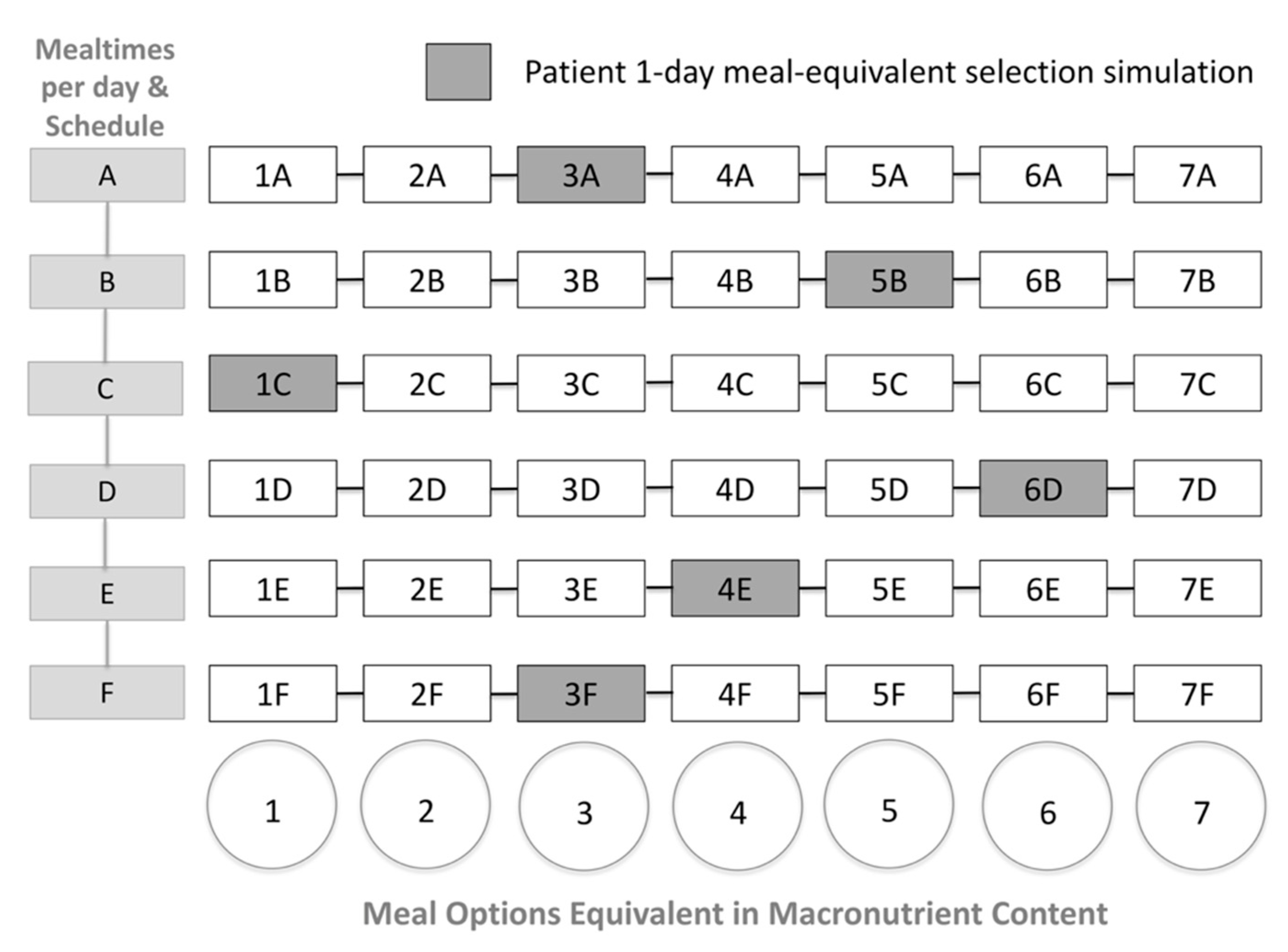
Mealtime Planning
4. Expected Result
4.1. Dynamic Macronutrient Meal-Equivalent Menu
4.2. Follow-up Sessions
4.3. Summarizing the MEM steps
- Assess the nutritional status and physical activity level to calculate the theoretical energy and macronutrients.
- Adjustments in daily caloric intake (restriction/addition) should be made considering the individual’s health status.
- The macronutrients intake should be calculated in the following order: protein (g/kg BW/day), fat, and carbohydrates.
- The SFSs/day/food group are set according to the patient preferences, socioeconomic and cultural background, as well as theoretical energy and macronutrient calculations.
- Once SFS/day have been established, the obtained energy (kcal/day) and macronutrient content (g/day) must be compared with the theoretical estimates within acceptable variations: protein ±1 g/day, fat ± 1 g/day, carbohydrate ± 2 g/day, and energy ± 15 kcal/day.
- Based on the individual schedule and a healthy mealtime distribution, the RDN plans the required mealtimes.
- Total SFS/day are distributed within the planned schedule. Therefore, each meal will be equivalent in energy and macronutrient content.
- The meal options will be designed depending on the patient’s access to food and regular meals maintaining the SFS/meal.
- Seven interchangeable meal options within each mealtime will be provided by the RDN, enabling patients to make healthy meal-choices in a guided format whilst adhering to a dietary plan.
- During the follow-up sessions, the RDN will evaluate how the mealtimes and food options worked for the patient, making adaptations for the next period.
5. Discussion
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- U.S. Department of Health and Human Services and U.S. Department of Agriculture. 2015–2020 Dietary Guidelines for Americans, 8th ed. Available online: http://health.gov/dietaryguidelines/2015/guidelines/ (accessed on 16 May 2019).
- Food and Agriculture Organization. El Estado De Las Guías Alimentarias Basadas En Alimentos En América Latina Y El Caribe. [The Status of Food-Based Dietary Guidelines in Latin America and the Caribbean.] 2014. Available online: http://www.fao.org/3/a-i3677s.pdf (accessed on 16 May 2019).
- Pérez-Escamilla, R. The Mexican Dietary and Physical Activity Guidelines: Moving Public Nutrition Forward in a Globalized World. J. Nutr. 2016, 146, 1924S–1927S. [Google Scholar] [CrossRef]
- de Roos, B. Personalised nutrition: Ready for practice? Proc. Nutr. Soc. 2013, 72, 48–52. [Google Scholar] [CrossRef]
- Lacey, K.; Pritchett, E. Nutrition Care Process and Model: ADA adopts road map to quality care and outcomes management. J. Am. Diet. Assoc. 2003, 103, 1061–1072. [Google Scholar] [CrossRef]
- Academy of Nutrition and Dietetics. Definition of Terms List 2017. Available online: https://www.eatrightpro.org/-/media/eatrightpro-files/practice/scope-standards-of-practice/academydefinitionoftermslist.pdf (accessed on 16 May 2019).
- Camp, K.M.; Trujillo, E. Position of the Academy of Nutrition and Dietetics: Nutritional genomics. J. Acad. Nutr. Diet. 2014, 114, 299–312. [Google Scholar] [CrossRef]
- Kohlmeier, M.; De Caterina, R.; Ferguson, L.R.; Görman, U.; Allayee, H.; Prasad, C.; Kang, J.X.; Nicoletti, C.F.; Martinez, J.A. Guide and Position of the International Society of Nutrigenetics/Nutrigenomics on Personalized Nutrition: Part 2-Ethics, Challenges and Endeavors of Precision Nutrition. J. Nutr. Nutr. 2016, 9, 28–46. [Google Scholar] [CrossRef]
- Poínhos, R.; van der Lans, I.A.; Rankin, A.; Fischer, A.R.; Bunting, B.; Kuznesof, S.; Stewart-Knox, B.; Frewer, L.J. Psychological determinants of consumer acceptance of personalised nutrition in 9 European countries. PLoS ONE 2014, 9, e110614. [Google Scholar] [CrossRef]
- Weir, M.; Morin, K.; Ries, N.; Castle, D. Canadian health care professionals’ knowledge, attitudes and perceptions of nutritional genomics. Br. J. Nutr. 2010, 104, 1112–1119. [Google Scholar] [CrossRef]
- Dorner, B.; Friedrich, E.K. Position of the Academy of Nutrition and Dietetics: Individualized Nutrition Approaches for Older Adults: Long-Term Care, Post-Acute Care, and Other Settings. J. Acad. Nutr. Diet. 2018, 118, 724–735. [Google Scholar] [CrossRef]
- Rapacciuolo, A.; Perrone Filardi, P.; Cuomo, R.; Mauriello, V.; Quarto, M.; Kisslinger, A.; Savarese, G.; Illario, M.; Tramontano, D. The Impact of Social and Cultural Engagement and Dieting on Well-Being and Resilience in a Group of Residents in the Metropolitan Area of Naples. J. Aging Res. 2016, 2016, 4768420. [Google Scholar] [CrossRef]
- Schröder, H.; Gomez, S.F.; Ribas-Barba, L.; Pérez-Rodrigo, C.; Bawaked, R.A.; Fíto, M.; Serra-Majem, L. Monetary Diet Cost, Diet Quality, and Parental Socioeconomic Status in Spanish Youth. PLoS ONE 2016, 11, e0161422. [Google Scholar] [CrossRef]
- Lutz, L.J.; Gaffney-Stomberg, E.; Williams, K.W.; McGraw, S.M.; Niro, P.J.; Karl, J.P.; Cable, S.J.; Cropper, T.L.; McClung, J.P. Adherence to the Dietary Guidelines for Americans Is Associated with Psychological Resilience in Young Adults: A Cross-Sectional Study. J. Acad. Nutr. Diet. 2017, 117, 396–403. [Google Scholar] [CrossRef]
- Schiavo, L.; Scalera, G.; Pilone, V.; De Sena, G.; Ciorra, F.R.; Barbarisi, A. Patient adherence in following a prescribed diet and micronutrient supplements after laparoscopic sleeve gastrectomy: Our experience during 1 year of follow-up. J. Hum. Nutr. Diet. 2017, 30, 98–104. [Google Scholar] [CrossRef]
- Mabry, J.; Farris, P.E.; Forro, V.A.; Findholt, N.E.; Purnell, J.Q.; Davis, M.M. Environmental, Behavioral, and Cultural Factors That Influence Healthy Eating in Rural Women of Childbearing Age: Findings From a PhotoVoice Study. Glob. Qual. Nurs. Res. 2016, 3, 2333393615622176. [Google Scholar] [CrossRef]
- Limon-Miro, A.T.; Lopez-Teros, V.; Astiazaran-Garcia, H. Dietary Guidelines for Breast Cancer Patients: A Critical Review. Adv. Nutr. 2017, 8, 613–623. [Google Scholar] [CrossRef]
- Martinez, J.A.; Navas-Carretero, S.; Saris, W.H.; Astrup, A. Personalized weight loss strategies-the role of macronutrient distribution. Nat. Rev. Endocrinol. 2014, 10, 749–760. [Google Scholar] [CrossRef]
- Carreiro, A.L.; Dhillon, J.; Gordon, S.; Higgins, K.A.; Jacobs, A.G.; McArthur, B.M.; Redan, B.W.; Rivera, R.L.; Schmidt, L.R.; Mattes, R.D. The Macronutrients, Appetite, and Energy Intake. Annu. Rev. Nutr. 2016, 36, 73–103. [Google Scholar] [CrossRef]
- Jensen, M.D.; Ryan, D.H.; Apovian, C.M.; Ard, J.D.; Comuzzie, A.G.; Donato, K.A.; Hu, F.B.; Hubbard, V.S.; Jakicic, J.M.; Kushner, R.F.; et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines; Obesity Society. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J. Am. Coll. Cardiol. 2014, 63, 2985–3023. [Google Scholar] [CrossRef]
- Larsen, T.M.; Dalskov, S.M.; van Baak, M.; Jebb, S.A.; Papadaki, A.; Pfeiffer, A.F.; Martinez, J.A.; Handjieva-Darlenska, T.; Kunešová, M.; Pihlsgård, M.; et al. Diet, Obesity, and Genes (Diogenes) Project. Diets with high or low protein content and glycemic index for weight-loss maintenance. N. Engl. J. Med. 2010, 363, 2102–2113. [Google Scholar] [CrossRef]
- Morrison. Manual of Clinical Nutrition Management, 14th ed.; Compass Group Inc.: Armonk, NY, USA, 2013. [Google Scholar]
- Institute of Medicine (IOM). Food and Nutrition Board. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients); National Academies Press: Washington, DC, USA, 2002. [Google Scholar]
- Gomes, F.; Schuetz, P.; Bounoure, L.; Austin, P.; Ballesteros-Pomar, M.; Cederholm, T.; Fletcher, J.; Laviano, A.; Norman, K.; Poulia, K.A.; et al. ESPEN guidelines on nutritional support for polymorbid internal medicine patients. Clin. Nutr. 2018, 37, 336–353. [Google Scholar] [CrossRef]
- Wheeler, M.L.; Daly, A.; Evert, A.; Franz, M.; Geil, P.; Holzmeister, L.A.; Kulkarni, K.; Loghmani, E.; Ross, T.A.; Woolf, P. Choose Your Foods: Exchange Lists for Diabetes, Sixth Edition, 2008: Description and Guidelines for Use. J. Am. Diet. Assoc. 2008, 108, 883–888. [Google Scholar] [CrossRef]
- Tomé, D.; Bos, C. Dietary protein and nitrogen utilization. J. Nutr. 2000, 130, 1868S–1873S. [Google Scholar] [CrossRef]
- Food and Agriculture Organization. Dietary Assessment: A Resource Guide to Method Selection and Application in Low Resource Settings 2018. Available online: http://www.fao.org/3/i9940en/I9940EN.pdf (accessed on 21 May 2019).
- Perez-Lizaur, A.B.; Palacios-Gonzalez, B.P.; Castro-Becerra, A.L.; Flores-Galicia, I. SMAE: Sistema Mexicano De Alimentos Equivalentes [SMAE: Mexican Equivalent Food System], 4th ed.; FNS: Reynosa, Mexico, 2014.
- Mushtaq, R.; Akram, A.; Mushtaq, R.; Khwaja, S.; Ahmed, S. The role of inflammatory markers following Ramadan Fasting. Pak. J. Med. Sci. 2019, 35, 77–81. [Google Scholar] [CrossRef]
- Byrne, N.M.; Meerkin, J.D.; Laukkanen, R.; Ross, R.; Fogelholm, M.; Hills, A.P. Weight loss strategies for obese adults: Personalized weight management program vs. standard care. Obesity (Silver Spring) 2006, 14, 1777–1788. [Google Scholar] [CrossRef]
- Calvo-Malvar, M.M.; Leis, R.; Benítez-Estévez, A.J.; Sánchez-Castro, J.; Gude, F. A randomised, family-focused dietary intervention to evaluate the Atlantic diet: The GALIAT study protocol. BMC Public Health 2016, 16, 820. [Google Scholar] [CrossRef]
- Conchin, S.; Carey, S. The expert’s guide to mealtime interventions-A Delphi method survey. Clin. Nutr. 2018, 37, 1992–2000. [Google Scholar] [CrossRef]

© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Limon-Miro, A.T.; Lopez-Teros, V.; Astiazaran-Garcia, H. Dynamic Macronutrient Meal-Equivalent Menu Method: Towards Individual Nutrition Intervention Programs. Methods Protoc. 2019, 2, 78. https://doi.org/10.3390/mps2030078
Limon-Miro AT, Lopez-Teros V, Astiazaran-Garcia H. Dynamic Macronutrient Meal-Equivalent Menu Method: Towards Individual Nutrition Intervention Programs. Methods and Protocols. 2019; 2(3):78. https://doi.org/10.3390/mps2030078
Chicago/Turabian StyleLimon-Miro, Ana Teresa, Veronica Lopez-Teros, and Humberto Astiazaran-Garcia. 2019. "Dynamic Macronutrient Meal-Equivalent Menu Method: Towards Individual Nutrition Intervention Programs" Methods and Protocols 2, no. 3: 78. https://doi.org/10.3390/mps2030078
APA StyleLimon-Miro, A. T., Lopez-Teros, V., & Astiazaran-Garcia, H. (2019). Dynamic Macronutrient Meal-Equivalent Menu Method: Towards Individual Nutrition Intervention Programs. Methods and Protocols, 2(3), 78. https://doi.org/10.3390/mps2030078






