Ethical Considerations for Equitable Access to Genomic Sequencing for Critically Ill Neonates in the United States
Abstract
:1. Introduction
2. Factors Impacting the Variability in Access to Genomic Sequencing
2.1. Insurance Approval Requirements
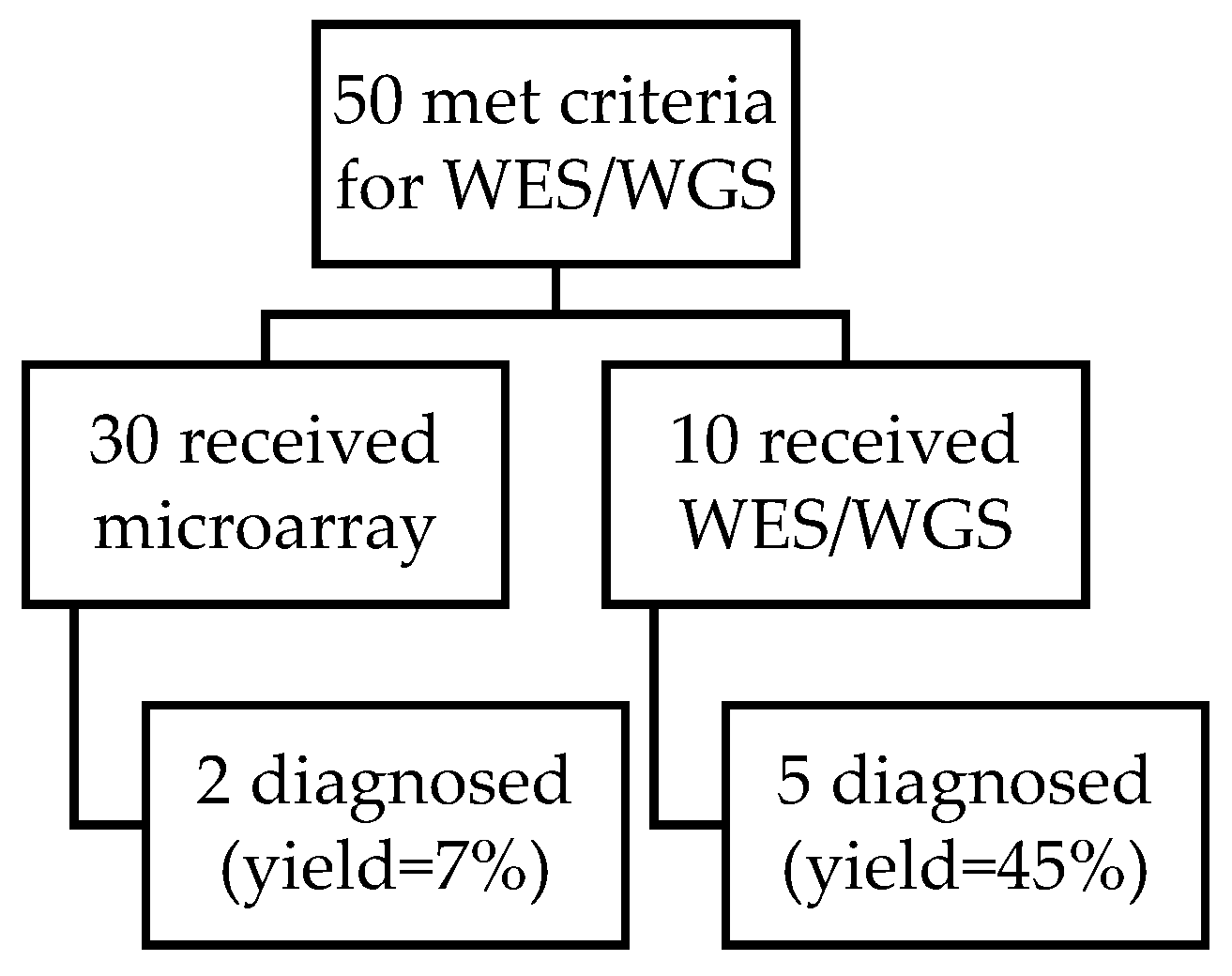
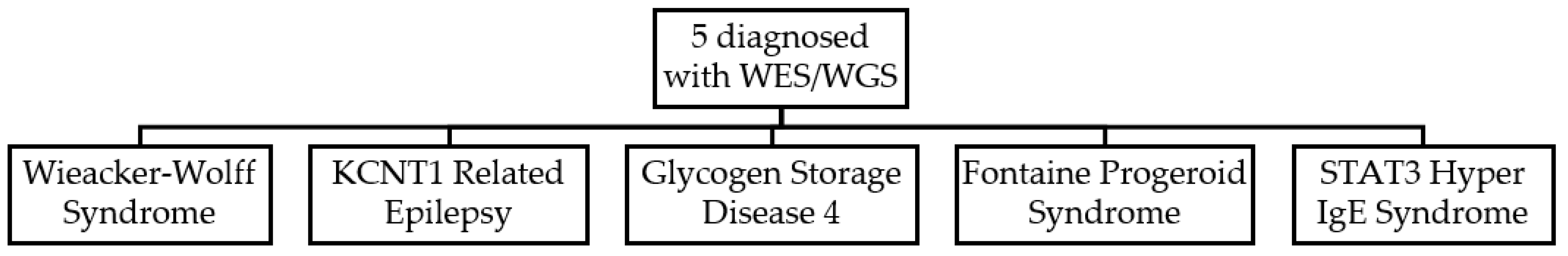
2.2. Hospital Review/Approval Committees
2.3. Inconsistent Definitions of “Change of Management” Impacts Insurance Coverage Policies
3. Ethical Implications for Barriers to Genomic Sequencing
3.1. Legal Implications
3.2. Psychosocial Implications for Parents and Providers
4. Considerations to Promote Access to Genomic Sequencing
4.1. Standardized Approval of Genomic Sequencing for All Neonates with Phenotype Known to Have High Yield
4.2. Creative Technological Solutions to Extend Genetic Evaluation to Areas without Genetics Experts
5. Opportunities for Future Research
- Measure the short- and long-term healthcare outcomes for critically ill neonates, stratified by phenotype, who did and did not receive genomic sequencing while in the NICU.
- Characterize social indicators that may predict health disparities regarding access to genomic sequencing.
- Evaluate the criteria used to make decisions about which patients can access genomic sequencing within hospital-based committee structures.
- Explore whether prior-authorization and/or hospital-based committee approval for genomic sequencing in the inpatient setting contributes to the perceived ‘hospital ethical climate’ and/or moral distress for genetics specialists and other neonatal providers.
- Explore the parental experience of navigating prior authorization, hospital-based committee approval, and/or other barriers to genomic sequencing in the NICU to better understand their psychosocial impact. Although prior research identified psychosocial distress in parents of undiagnosed children, few studies have occurred in parents of newborns who are still in the hospital.
- Development and implementation of mobile applications and/or decision support tools for neonatal providers to extend genetics evaluation to NICUs in geographic areas where this access does not exist or is limited.
- Development and implementation of interactive education modules for neonatal trainees and/or current neonatal providers to support their decision making, triage, and advocacy for access to genomic sequencing for their patients.
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Therrell, B.L.; Padilla, C.D.; Loeber, J.G.; Kneisser, I.; Saadallah, A.; Borrajo, G.J.; Adams, J. Current status of newborn screening worldwide: 2015. Semin. Perinatol. 2015, 39, 171–187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cabello, J.F.; Novoa, F.; Huff, H.V.; Colombo, M. Expanded Newborn Screening and Genomic Sequencing in Latin America and the Resulting Social Justice and Ethical Considerations. Int. J. Neonatal Screen. 2021, 7, 6. [Google Scholar] [CrossRef] [PubMed]
- Fabie, N.A.V.; Pappas, K.B.; Feldman, G.L. The Current State of Newborn Screening in the United States. Pediatr. Clin. N. Am. 2019, 66, 369–386. [Google Scholar] [CrossRef] [PubMed]
- Stark, Z.; Ellard, S. Rapid genomic testing for critically ill children: Time to become standard of care? Eur. J. Hum. Genet. 2021, 1–8. [Google Scholar] [CrossRef]
- Stark, Z.; Tan, T.Y.; Chong, B.; Brett, G.R.; Yap, P.; Walsh, M.; Yeung, A.; Peters, H.; Mordaunt, D.; Cowie, S.; et al. A prospective evaluation of whole-exome sequencing as a first-tier molecular test in infants with suspected monogenic disorders. Genet. Med. 2016, 18, 1090–1096. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kingsmore, S.F.; Cakici, J.A.; Clark, M.M.; Gaughran, M.; Feddock, M.; Batalov, S.; Bainbridge, M.N.; Carroll, J.; Caylor, S.A.; Clarke, C.; et al. A Randomized, Controlled Trial of the Analytic and Diagnostic Performance of Singleton and Trio, Rapid Genome and Exome Sequencing in Ill Infants. Am. J. Hum. Genet. 2019, 105, 719–733. [Google Scholar] [CrossRef]
- Clark, M.M.; Hildreth, A.; Batalov, S.; Ding, Y.; Chowdhury, S.; Watkins, K.; Ellsworth, K.; Camp, B.; Kint, C.I.; Yacoubian, C.; et al. Diagnosis of genetic diseases in seriously ill children by rapid whole-genome sequencing and automated phenotyping and interpretation. Sci. Transl. Med. 2019, 11, eaat6177. [Google Scholar] [CrossRef]
- Farnaes, L.; Hildreth, A.; Sweeney, N.M.; Clark, M.M.; Chowdhury, S.; Nahas, S.; Cakici, J.A.; Benson, W.; Kaplan, R.H.; Kronick, R.; et al. Rapid whole-genome sequencing decreases infant morbidity and cost of hospitalization. NPJ Genom. Med. 2018, 3, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Dimmock, D.; Caylor, S.; Waldman, B.; Benson, W.; Ashburner, C.; Carmichael, J.L.; Carroll, J.; Cham, E.; Chowdhury, S.; Cleary, J.; et al. Project Baby Bear: Rapid precision care incorporating rWGS in 5 California children’s hospitals demonstrates improved clinical outcomes and reduced costs of care. Am. J. Hum. Genet. 2021, 108, 1231–1238. [Google Scholar] [CrossRef]
- Brunelli, L.; Jenkins, S.M.; Gudgeon, J.M.; Bleyl, S.B.; Miller, C.E.; Tvrdik, T.; Dames, S.A.; Ostrander, B.; Daboub, J.A.F.; Zielinski, B.A.; et al. Targeted gene panel sequencing for the rapid diagnosis of acutely ill infants. Mol. Genet. Genom. Med. 2019, 7, e00796. [Google Scholar] [CrossRef] [Green Version]
- Daoud, H.; Luco, S.M.; Li, R.; Bareke, E.; Beaulieu, C.; Jarinova, O.; Carson, N.; Nikkel, S.M.; Graham, G.E.; Richer, J.; et al. Next-generation sequencing for diagnosis of rare diseases in the neonatal intensive care unit. Can. Med. Assoc. J. 2016, 188, E254–E260. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- French, C.E.; Delon, I.; Dolling, H.; Sanchis-Juan, A.; Shamardina, O.; Mégy, K.; Raymond, F.L. Whole genome sequencing reveals that genetic conditions are frequent in intensively ill children. Intensive Care Med. 2019, 45, 627–636. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meng, L.; Pammi, M.; Saronwala, A.; Magoulas, P.; Ghazi, A.R.; Vetrini, F.; Lalani, S.R. Use of Exome Sequencing for Infants in Intensive Care Units: Ascertainment of Severe Single-Gene Disorders and Effect on Medical Management. JAMA Pediatr. 2017, 171, e173438. [Google Scholar] [CrossRef]
- Petrikin, J.E.; Cakici, J.A.; Clark, M.M.; Willig, L.K.; Sweeney, N.M.; Farrow, E.G.; Saunders, C.J.; Thiffault, I.; Miller, N.A.; Zellmer, L.; et al. The NSIGHT1-randomized controlled trial: Rapid whole-genome sequencing for accelerated etiologic diagnosis in critically ill infants. NPJ Genom. Med. 2018, 3, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Willig, L.; Petrikin, J.E.; Smith, L.D.; Saunders, C.J.; Thiffault, I.; Miller, N.A.; Soden, S.E.; Cakici, J.; Herd, S.M.; Twist, G.; et al. Whole-genome sequencing for identification of Mendelian disorders in critically ill infants: A retrospective analysis of diagnostic and clinical findings. Lancet Respir. Med. 2015, 3, 377–387. [Google Scholar] [CrossRef] [Green Version]
- Brunelli, L.; Mao, R.; Jenkins, S.M.; Bleyl, S.B.; Dames, S.A.; Miller, C.E.; Ostrander, B.; Tvrdik, T.; Andrews, S.; Flores, J.; et al. A rapid gene sequencing panel strategy to facilitate precision neonatal medicine. Am. J. Med. Genet. Part A 2017, 173, 1979–1982. [Google Scholar] [CrossRef] [PubMed]
- Krantz, I.D.; Medne, L.; Weatherly, J.M.; Wild, K.T.; Biswas, S.; Devkota, B. Effect of Whole-Genome Sequencing on the Clinical Management of Acutely Ill Infants with Suspected Genetic Disease: A Randomized Clinical Trial. JAMA Pediatr. 2021, 175, 1218–1226. [Google Scholar]
- Stark, Z.; Schofield, D.; Martyn, M.; Rynehart, L.; Shrestha, R.; Alam, K.; Lunke, S.; Tan, T.Y.; Gaff, C.L.; White, S.M. Does genomic sequencing early in the diagnostic trajectory make a difference? A follow-up study of clinical outcomes and cost-effectiveness. Genet. Med. 2019, 21, 173–180. [Google Scholar] [CrossRef]
- Stark, Z.; Schofield, D.; Alam, K.; Wilson, W.; Mupfeki, N.; Macciocca, I.; Shrestha, R.; White, S.M.; Gaff, C. Prospective comparison of the cost-effectiveness of clinical whole-exome sequencing with that of usual care overwhelmingly supports early use and reimbursement. Genet. Med. 2017, 19, 867–874. [Google Scholar] [CrossRef] [Green Version]
- Hayeems, R.Z.; Bhawra, J.; Tsiplova, K.; Meyn, M.S.; Monfared, N.; Bowdin, S.; Stavropoulos, D.J.; Marshall, C.R.; Basran, R.; Shuman, C.; et al. Care and cost consequences of pediatric whole genome sequencing compared to chromosome microarray. Eur. J. Hum. Genet. 2017, 25, 1303–1312. [Google Scholar] [CrossRef] [Green Version]
- Swaggart, K.A.; Swarr, D.T.; Tolusso, L.K.; He, H.; Dawson, D.B.; Suhrie, K.R. Making a Genetic Diagnosis in a Level IV Neonatal Intensive Care Unit Population: Who, When, How, and at What Cost? J. Pediatr. 2019, 213, 211–217.e4. [Google Scholar] [CrossRef] [PubMed]
- Franck, L.S.; Kriz, R.M.; Rego, S.; Garman, K.; Hobbs, C.; Dimmock, D. Implementing Rapid Whole-Genome Sequencing in Critical Care: A Qualitative Study of Facilitators and Barriers to New Technology Adoption. J. Pediatr. 2021, 237, 237–243.e2. [Google Scholar] [CrossRef] [PubMed]
- Jooma, S.; Hahn, M.J.; Hindorff, L.A.; Bonham, V.L. Defining and Achieving Health Equity in Genomic Medicine. Ethn. Dis. 2019, 29 (Suppl. 1), 173–178. [Google Scholar] [CrossRef] [PubMed]
- Nolan, D.; Carlson, M. Whole exome sequencing in pediatric neurology patients: Clinical implications and estimated cost analysis. J. Child Neurol. 2016, 31, 887–894. [Google Scholar] [CrossRef]
- Suther, S.; Kiros, G.-E. Barriers to the use of genetic testing: A study of racial and ethnic disparities. Genet. Med. 2009, 11, 655–662. [Google Scholar] [CrossRef] [Green Version]
- Kapil, S.; Fishler, K.P.; Euteneuer, J.C.; Brunelli, L. Many newborns in level IV NICUs are eligible for rapid DNA sequencing. Am. J. Med. Genet. Part A 2018, 179, 280–284. [Google Scholar] [CrossRef]
- Phillips, K.A.; Deverka, P.A.; Trosman, J.R.; Douglas, M.; Chambers, J.D.; Weldon, C.B.; Dervan, A.P. Payer coverage policies for multigene tests. Nat. Biotechnol. 2017, 35, 614–617. [Google Scholar] [CrossRef] [Green Version]
- Trosman, J.R.; Weldon, C.B.; Slavotinek, A.; Norton, M.E.; Douglas, M.P.; Phillips, K.A. Perspectives of US private payers on insurance coverage for pediatric and prenatal exome sequencing: Results of a study from the Program in Prenatal and Pediatric Genomic Sequencing (P3EGS). Genet. Med. 2019, 22, 283–291. [Google Scholar] [CrossRef]
- Kahan, N.R.; Chinitz, D.P.; Waitman, D.-A.; Kahan, E. When gatekeepers meet the sentinel: The impact of a prior authorization requirement for cefuroxime on the prescribing behaviour of community-based physicians. Br. J. Clin. Pharmacol. 2006, 61, 341–344. [Google Scholar] [CrossRef]
- Marchant, G.L.R. Genomic malpractice: An emerging tide or gentle ripple? Food Drug Law J. 2018, 73, 1–37. [Google Scholar]
- Graungaard, H.A.; Skov, L. Why do we need a diagnosis? A qualitative study of parents’ experiences, coping and needs, when the newborn child is severely disabled. Child Care Health Dev. 2007, 33, 296–307. [Google Scholar] [CrossRef] [PubMed]
- Lopes, M.T.; Koch, V.H.; Sarrubbi-Junior, V.; Gallo, P.R.; Carneiro-Sampaio, M. Difficulties in the diagnosis and treatment of rare diseases according to the perceptions of patients, relatives and health care professionals. Clinics 2018, 73, e68. [Google Scholar] [CrossRef] [PubMed]
- McConkie-Rosell, A.; Hooper, S.R.; Pena, L.D.; Schoch, K.; Spillmann, R.C.; Jiang, Y.H.; Shashi, V. Psychosocial Profiles of Parents of Children with Undiagnosed Diseases: Managing Well or Just Managing? J. Genet. Couns. 2018, 27, 935–946. [Google Scholar] [CrossRef] [PubMed]
- Madeo, A.C.; O’Brien, K.E.; Bernhardt, B.A.; Biesecker, B.B. Factors associated with perceived uncertainty among parents of children with undiagnosed medical conditions. Am. J. Med. Genet. Part A 2012, 158A, 1877–1884. [Google Scholar] [CrossRef] [Green Version]
- Epstein, E.G.; Whitehead, P.B.; Prompahakul, C.; Thacker, L.R.; Hamric, A.B. Enhancing Understanding of Moral Distress: The Measure of Moral Distress for Health Care Professionals. AJOB Empir. Bioeth. 2019, 10, 113–124. [Google Scholar] [CrossRef]
- Braithwaite, M. Nurse Burnout and Stress in the NICU. Adv. Neonatal Care 2008, 8, 343–347. [Google Scholar] [CrossRef]
- Bernhardt, B.A.; Silver, R.; Rushton, C.H.; Micco, E.; Geller, G. What keeps you up at night? Genetics professionals’ distressing experiences in patient care. Genet. Med. 2010, 12, 289–297. [Google Scholar] [CrossRef] [Green Version]
- Wagner, C. Moral distress as a contributor to nurse burnout. AJN Am. J. Nurs. 2015, 115, 11. [Google Scholar] [CrossRef]
- Barr, P. Moral Distress and Considering Leaving in NICU Nurses: Direct Effects and Indirect Effects Mediated by Burnout and the Hospital Ethical Climate. Neonatology 2020, 117, 646–649. [Google Scholar] [CrossRef]
- Srivastava, S.; Love-Nichols, J.A.; Dies, K.A.; Ledbetter, D.H.; Martin, C.L.; Chung, W.K.; Firth, H.V.; Frazier, T.; Hansen, R.L.; Prock, L.; et al. Meta-analysis and multidisciplinary consensus statement: Exome sequencing is a first-tier clinical diagnostic test for individuals with neurodevelopmental disorders. Genet. Med. 2019, 22, 1731–1732. [Google Scholar] [CrossRef]
- Srivastava, S.; Cohen, J.S.; Vernon, H.; Barañano, K.; McClellan, R.; Jamal, L.; Naidu, S.; Fatemi, A. Clinical whole exome sequencing in child neurology practice. Ann. Neurol. 2014, 76, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Tarailo-Graovac, M.; Shyr, C.; Ross, C.J.; Horvath, G.A.; Salvarinova, R.; Ye, X.C.; van Karnebeek, C.D. Exome sequencing and the management of neurometabolic disorders. N. Engl. J. Med. 2016, 374, 2246–2255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Retterer, K.; Juusola, J.; Cho, M.T.; Vitazka, P.; Millan, F.; Gibellini, F.; Vertino-Bell, A.; Smaoui, N.; Neidich, J.; Monaghan, K.G.; et al. Clinical application of whole-exome sequencing across clinical indications. Genet. Med. 2016, 18, 696–704. [Google Scholar] [CrossRef] [PubMed] [Green Version]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
P. Fishler, K.; Euteneuer, J.C.; Brunelli, L. Ethical Considerations for Equitable Access to Genomic Sequencing for Critically Ill Neonates in the United States. Int. J. Neonatal Screen. 2022, 8, 22. https://doi.org/10.3390/ijns8010022
P. Fishler K, Euteneuer JC, Brunelli L. Ethical Considerations for Equitable Access to Genomic Sequencing for Critically Ill Neonates in the United States. International Journal of Neonatal Screening. 2022; 8(1):22. https://doi.org/10.3390/ijns8010022
Chicago/Turabian StyleP. Fishler, Kristen, Joshua C. Euteneuer, and Luca Brunelli. 2022. "Ethical Considerations for Equitable Access to Genomic Sequencing for Critically Ill Neonates in the United States" International Journal of Neonatal Screening 8, no. 1: 22. https://doi.org/10.3390/ijns8010022
APA StyleP. Fishler, K., Euteneuer, J. C., & Brunelli, L. (2022). Ethical Considerations for Equitable Access to Genomic Sequencing for Critically Ill Neonates in the United States. International Journal of Neonatal Screening, 8(1), 22. https://doi.org/10.3390/ijns8010022





