The Value of Cognitive Pretesting: Improving Validity and Revealing Blind Spots through the Development of a Newborn Screening Parent Experiences Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Cognitive Pretest Recruitment
2.2. Cognitive Pretest Interviews
3. Results
3.1. Plain Language Definitions
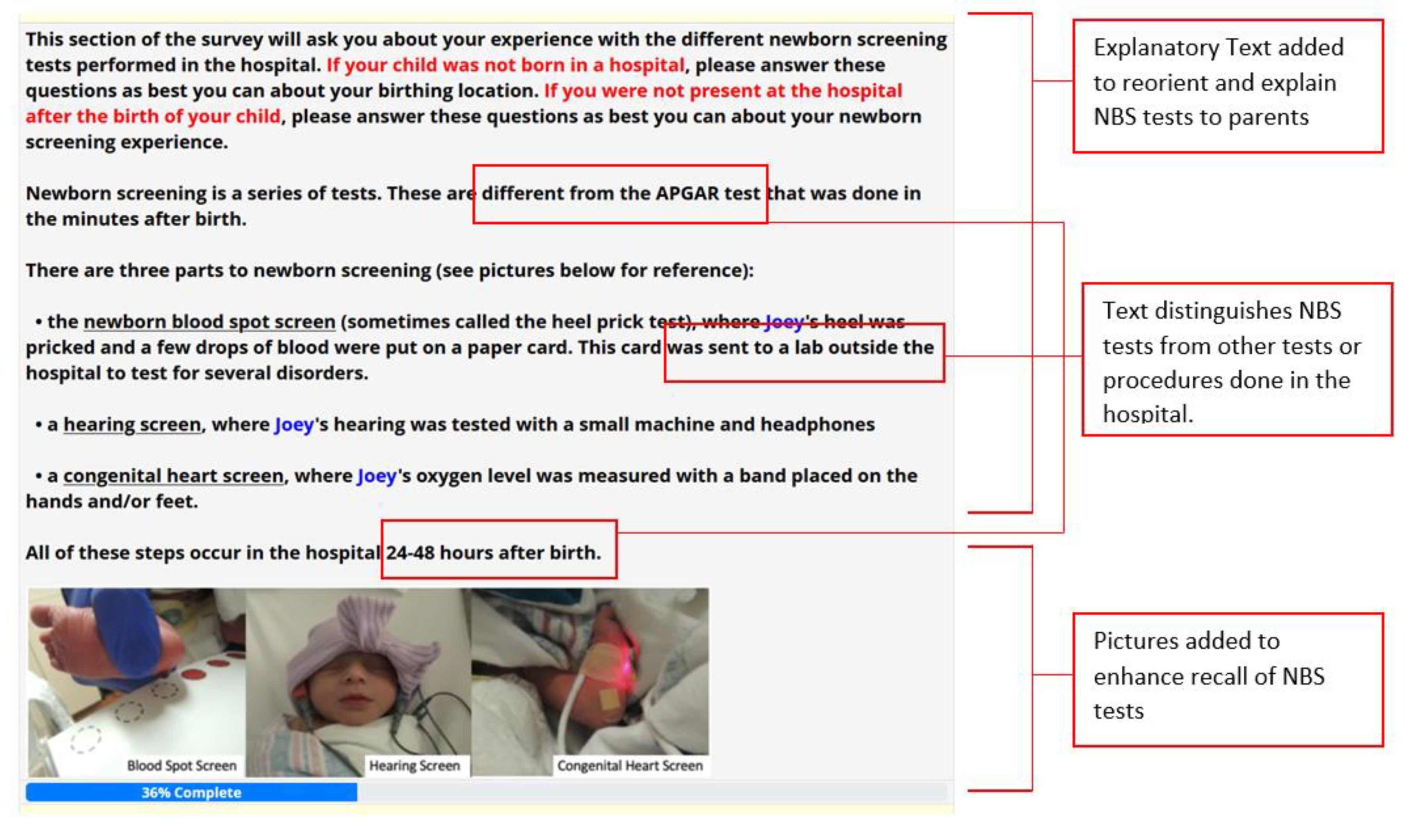
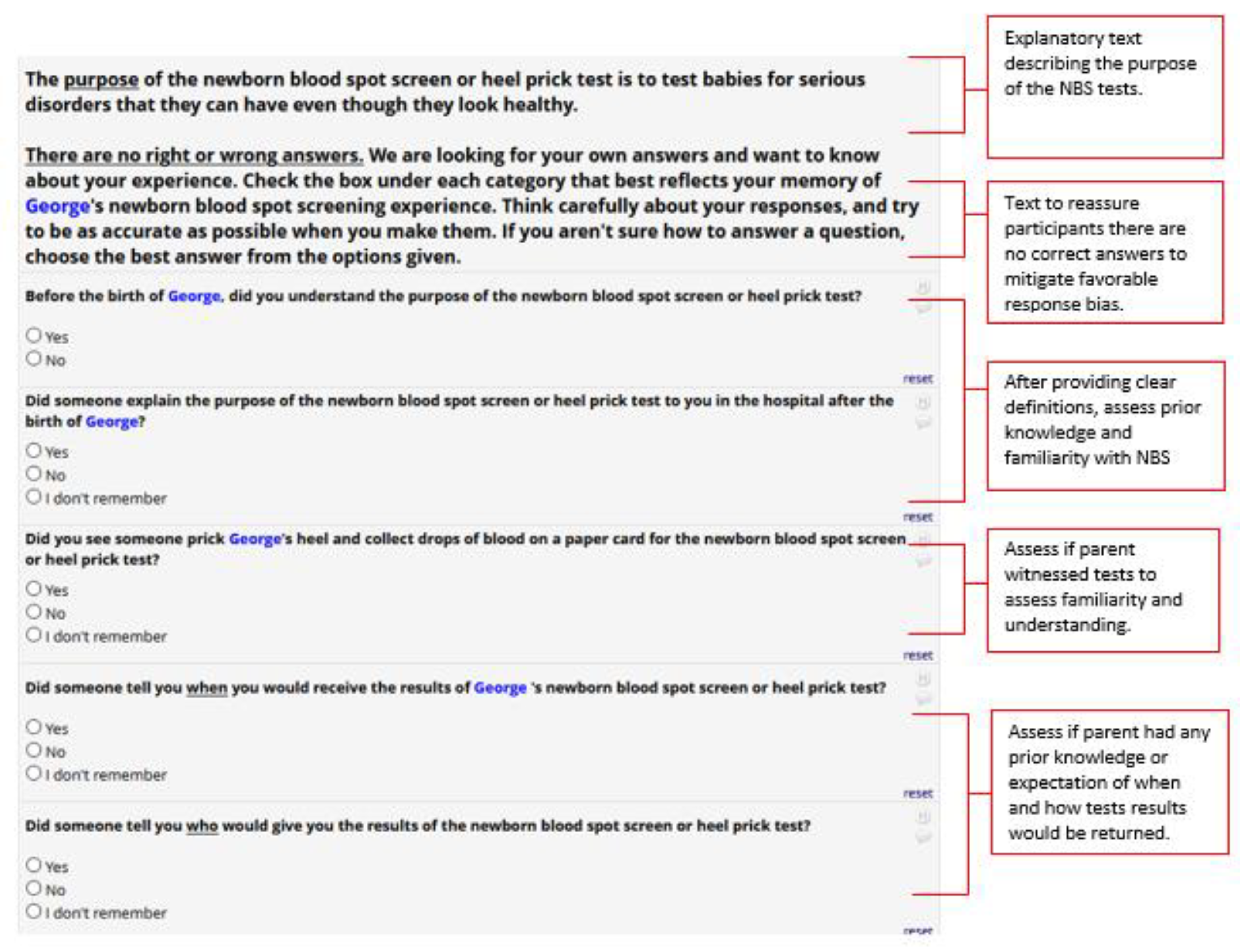
3.2. Newborn Screening: Testing Experiences
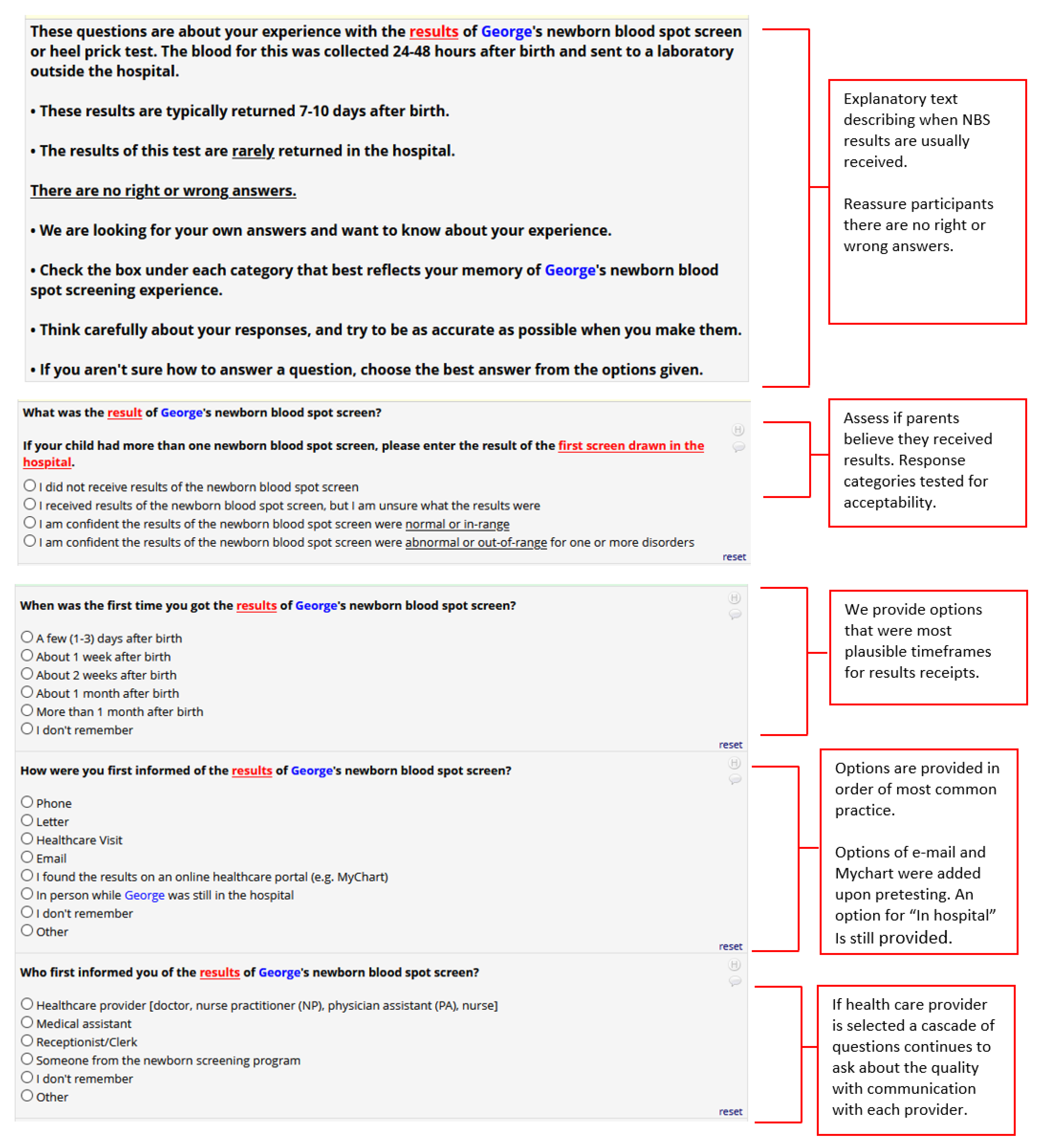
3.3. Newborn Screening: Result Communication Expectations
3.4. Newborn Screening: Provider Communication
3.5. Overall Survey Applicability, Accessibility, Appearance, and Flow
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Simon, N.-J.; Atkins, A.; Yusuf, C.; Tarini, B.A. Systems Integration: The Next Frontier of Newborn Screening Timeliness. J. Public Health Manag. Pract. 2020, 26, E8–E15. [Google Scholar] [CrossRef] [PubMed]
- Cochran, A.L.; Tarini, B.A.; Kleyn, M.; Zayas-Caban, G. Newborn Screening Collection and Delivery Processes in Michigan Birthing Hospitals: Strategies to Improve Timeliness. Matern. Child Health J. 2018, 10, 1436–1443. [Google Scholar] [CrossRef]
- Schmidt, J.L.; Castellanos-Brown, K.; Childress, S.; Bonhomme, N.; Oktay, J.S.; Terry, S.F.; Kyler, P.; Davidoff, D.; Green, C. The Impact of False-Positive Newborn Screening Results on Families: A Qualitative Study. Genet. Med. 2012, 14, 76–80. [Google Scholar] [CrossRef] [Green Version]
- Association of Public Health Laboratories. Newborn Screening Timeliness: Survey Report. Available online: https://www.aphl.org/AboutAPHL/publications/Documents/NBSTimelinessSuveyReport_10-2014.pdf (accessed on 30 May 2021).
- Finan, C.; Nasr, S.Z.; Rothwell, E.; Tarini, B.A. Primary Care Providers’ Experiences Notifying Parents of Cystic Fibrosis Screening Results. Clin. Pediatr. 2015, 54, 67–75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Farrell, M.H.; Christopher, S.A.; Tluczek, A.; Kennedy-Parker, K.; La Pean, A.; Eskra, K.; Hoffman, G.; Panepinto, J.; Farrell, P.M. Improving Communication between Doctors and Parents after Newborn Screening. WMJ 2011, 110, 221–227. [Google Scholar]
- Lewis, M.A.; Bonhomme, N.; Bloss, C.S. A New Era, New Strategies: Education and Communication Strategies to Manage Greater Access to Genomic Information. Hastings Cent. Rep. 2018, 18, S25–S27. [Google Scholar] [CrossRef] [Green Version]
- Evans, A.; LeBlanc, K.; Bonhomme, N.; Shone, S.M.; Gaviglio, A.; Freedenberg, D.; Penn, J.; Johnson, C.; Vogel, B.; Dolan, S.M.; et al. A Newborn Screening Education Best Practices Framework: Development and Adoption. Int. J. Neonatal. Screen. 2019, 5, 22. [Google Scholar] [CrossRef] [Green Version]
- Evans, A.; Lynch, M.; Johnson, M.; Bonhomme, N. Assessing the Newborn Screening Education Needs of Families Living in Medically Underserved Areas. J. Genet. Couns. 2020, 29, 658–667. [Google Scholar] [CrossRef] [PubMed]
- Tarini, B.A.; Simon, N.-J.; Payne, K.; Gebremariam, A.; Rose, A.; Prosser, L.A. An Assessment of Public Preferences for Newborn Screening Using Best-Worst Scaling. J. Pediatric 2018, 201, 62–68. [Google Scholar] [CrossRef]
- DeLuca, J.M. Public Attitudes Toward Expanded Newborn Screening. J. Pediatric Nurs. 2018, 38, e19–e23. [Google Scholar] [CrossRef] [PubMed]
- Evans, A.; Bonhomme, N.; Goodman, A. Newborn Screening and Health Communications. Genet. Test. Mol. Bioarkers. 2018, 22, 507–508. [Google Scholar] [CrossRef]
- Joseph, G.; Chen, F.; Harris-Wair, J.; Puck, J.M.; Young, C.; Koenig, B.A. Parental Views on Expanded Newborn Screening Using Whole Genome Sequencing. Pediatrics 2016, 137, S36–S46. [Google Scholar] [CrossRef] [Green Version]
- Willis, G.B.; Schechter, S. Evaluation of Cognitive Interviewing Techniques: Do the Results Generalize to the Field? Bull. Methodol. Sociol. 1997, 5, 40–66. [Google Scholar] [CrossRef]
- Collins, D. Presting Survey Instruments: An Overview of Cognitive Methods. Qual. Life Res. 2003, 12, 229–238. [Google Scholar] [CrossRef] [PubMed]
- Willis, G.B.; Artino, A.R. What do our Respondents Think We’re Asking? Using Cognitive Interviewing to Improve Medical Education Surveys. J. Med. Educ. 2013, 5, 353–356. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koskey, K.L.K. Using the Cognitive Pretesting Method to Gain Insight into Participants’ Experiences: An Illustration and Methodological Reflection. Int. J. Qual. Methods 2016. [Google Scholar] [CrossRef] [Green Version]
- Standards and Guidelines for Cognitive Interviews. Available online: https://wwwn.cdc.gov/qbank/CI-Standards.aspx#/Home (accessed on 30 May 2021).
- United States Census Bureau. American Community Survey (ACS). Available online: https://www2.census.gov/programs-surveys/acs/methodology/questionnaires/2020/quest20.pdf (accessed on 30 May 2021).
- The Child Health Questionnaire (CHQ). Available online: https://healthactchq.com/surveys/pdf/overviews/CHQ_Overview.pdf (accessed on 30 May 2021).
- Street, R.L. Physicians Communication and Parents’ Evaluations of Pediatric Consultations. Med. Care. 1991, 29, 1146–1152. [Google Scholar] [CrossRef]
- Chew, L.D.; Bradley, K.A.; Boyko, E.J. Brief Questions to Identify Patients with Inadequate Health Literacy. Fam. Med. 2004, 36, 588–594. [Google Scholar] [PubMed]
- Squires, J.; Bricker, D.; Twombley, E. Ages & Stages Questionnaires: Social Emotional, Second Edition (ASQ: SE-2) A Parent-Completed Child Monitoring System for Social-Emotional Behaviors; Paul, H., Ed.; Brookes Publishing Co., Inc.: Baltimore, MD, USA, 2002. [Google Scholar]
- PAR. Parenting Stress Index™, Fourth Edition (PSI™-4). 2016. Available online: https://www.parinc.com/Products/Pkey/333 (accessed on 2 July 2021).
- Kerruish, N.; Settle, K.; Campbell-Stokes, P.; Taylor, B.J. Vulnerable Baby Scale: Development and Piloting of a Study Questionnaire to Measure Maternal Perceptions of their Baby’s Vulnerability. J. Paediatr. Child Health 2005, 41, 419–423. [Google Scholar] [CrossRef]
- Pilkonis, P.A.; Choi, S.W.; Reise, S.P.; Stover, A.M.; Riley, W.T.; Cella, D. and the PROMIS Cooperative Group. Item banks for measuring emotional distress from the Patient-Reported outcomes Measurement Information System (PROMIS): Depression, Anxiety, and Anger. Assessment 2011, 18, 263–283. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research Electronic Data Capture (REDCap)—A Meta-drive Methodology and Workflow Process for Providing Translational Research Informatics Support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [Green Version]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, L.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef]
- El-Hattab, A.W.; Almannai, M.; Sutton, V.R. Newborn Screening: History, Current Status, and Future Directions. Pediatr. Clin. N. Am. 2018, 65, 389–405. [Google Scholar] [CrossRef] [PubMed]
- Nicholls, S.G.; Wilson, B.J.; Etchegary, H.; Brehaut, J.C.; Potter, B.K.; Hayeems, R.; Chakraborty, P.; Milburn, J.; Pullman, D.; Turner, L.; et al. Benefits and Burnes of Newborn Screening: Public Understanding and Decision-Making. Per. Med. 2014, 11, 593–607. [Google Scholar] [CrossRef]
- Kreuter, F.; Presser, S.; Tourangeau, R. Social Desirability Bias in CATI, IVR, and Web-Surveys. Public Opin. Q. 2008, 72, 847–865. [Google Scholar] [CrossRef] [Green Version]
- Etchegary, H.; Nicholls, S.T.; Tessier, L.; Simmonds, C.; Potter, B.K.; Brehaut, J.C.; Pullman, D.; Hayemms, R.; Zelenietz, S.; Lamoureux, M.; et al. Consent for newborn screening: Parents’ and health-care professionals’ experiences of consent in practice. Eur. J. Hum. J. 2016, 24, 1530–1534. [Google Scholar] [CrossRef] [PubMed]
- Gary-Burrows, K.A.; Willis, T.A.; Foy, R.; Rathfelder, M.; Bland, P.; Chin, A.; Hodgson, S.; Ibegbuan, G.; Prestwich, G.; Samuel, K.; et al. Role of Patient and Public Involvement in Implementation Research: A Consensus Study. BMJ Qual. Saf. 2018, 27, 858–864. [Google Scholar] [CrossRef] [Green Version]
| General Probes | |
|---|---|
| Probes for each survey section: | |
| Talk me through what you are thinking about as you take the survey. | |
| Did you find any questions difficult to answer? | |
| Which of the questions were you not sure how to answer? | |
| What was your overall impression of this section of the survey? | |
| Probes for pauses or hesitation during a survey response: | |
| What were you thinking about as you were answering this question? | |
| Do any of these categories seem to restrict your answer? Are there too many options to choose from? | |
| Are there any choices that aren’t here that would better match your answer? | |
| Specific Probes | |
| Survey Introduction and Pretesting Experience | |
| What questions do you have about the study? About pretesting? | |
| When you first open the survey, you see a logo associated with our study. When you see the logo, what comes to mind? | |
| How well do you think the logo represents the study? | |
| How could we better describe the study to the survey taker? | |
| Survey Eligibility and Enrollment | |
| When I asked you about [TPN, blood transfusions], what did you think about? What came to mind? | |
| What feedback do you have on the order that we ask these questions? | |
| Do you think you understood the study the way we described it? How would you describe the study to someone? | |
| Do you have any suggestions that might help us improve how we ask participants how they would like to receive the survey? | |
| Pregnancy and Delivery | |
| Were you already familiar with the medical conditions listed here? | |
| Were there any conditions that you weren’t sure how to answer because you didn’t know exactly what the term meant? | |
| Child-Wellbeing | |
| We ask a number of questions about how healthy your baby is at the end of the first section. Can you talk me through what you were thinking about as you answered these questions? | |
| We include a list of conditions or health problems that you could have been told your child has: Are there any conditions on this list that you aren’t sure how to answer? How would you describe or categorize your child’s condition? | |
| Newborn Screening | |
| When we first introduced newborn screening in this last section, what were you thinking about? | |
| Where did you first learn about newborn screening? What do you remember about the [newborn bloodspot, congenital heart screen, hearing] test in the hospital? Tell me about when you first learned about newborn screening tests? How were these tests explained? Is there a difference to being “told” that you had a test vs being “explained” that you had a test? Tell me about how learned about the results of the newborn screening tests. | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Simon, N.-J.; Atkins, A.; Miller, B.; Bonhomme, N.; Tarini, B. The Value of Cognitive Pretesting: Improving Validity and Revealing Blind Spots through the Development of a Newborn Screening Parent Experiences Survey. Int. J. Neonatal Screen. 2021, 7, 41. https://doi.org/10.3390/ijns7030041
Simon N-J, Atkins A, Miller B, Bonhomme N, Tarini B. The Value of Cognitive Pretesting: Improving Validity and Revealing Blind Spots through the Development of a Newborn Screening Parent Experiences Survey. International Journal of Neonatal Screening. 2021; 7(3):41. https://doi.org/10.3390/ijns7030041
Chicago/Turabian StyleSimon, Norma-Jean, Anne Atkins, Brianne Miller, Natasha Bonhomme, and Beth Tarini. 2021. "The Value of Cognitive Pretesting: Improving Validity and Revealing Blind Spots through the Development of a Newborn Screening Parent Experiences Survey" International Journal of Neonatal Screening 7, no. 3: 41. https://doi.org/10.3390/ijns7030041
APA StyleSimon, N.-J., Atkins, A., Miller, B., Bonhomme, N., & Tarini, B. (2021). The Value of Cognitive Pretesting: Improving Validity and Revealing Blind Spots through the Development of a Newborn Screening Parent Experiences Survey. International Journal of Neonatal Screening, 7(3), 41. https://doi.org/10.3390/ijns7030041







