Guideline Adherence and Registry Recruitment of Congenital Primary Hypothyroidism: Data from the German Registry for Congenital Hypothyroidism (HypoDok)
Abstract
1. Introduction
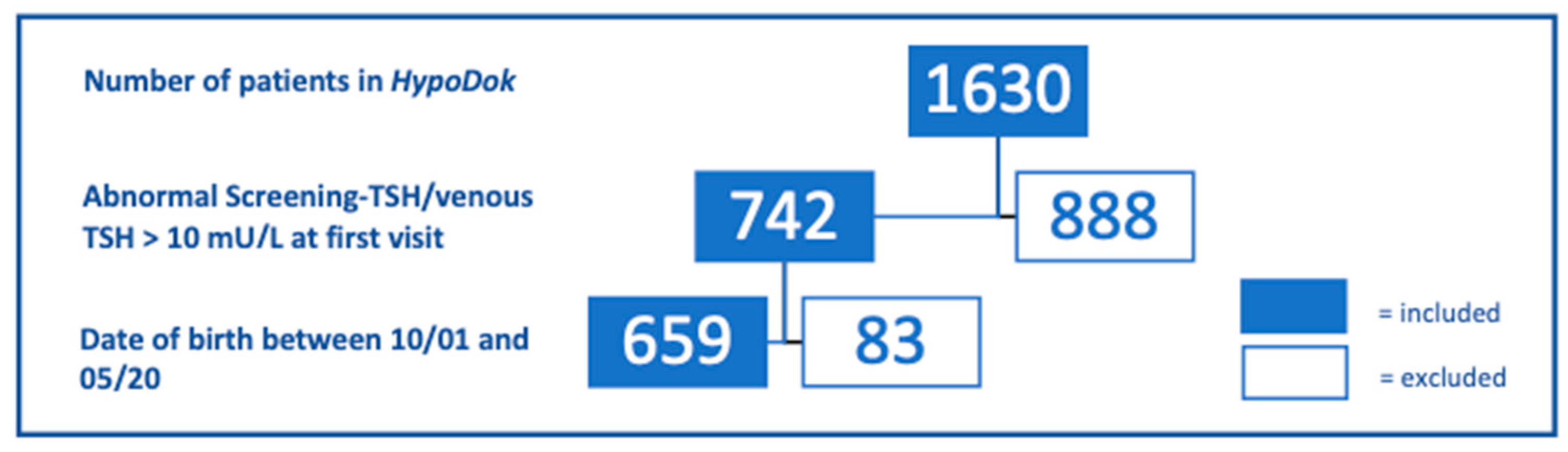
2. Patients/Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| Ab | antibody |
| APEDÖ | Austrian Working Group for Pediatric Endocrinology and Diabetology |
| AWMF | Association of the Scientific Medical Societies of Germany |
| CH | congenital primary hypothyroidism |
| DGKED | German Society for Pediatric Endocrinology and Diabetology |
| DGNS | German Society for Neonatal Screening |
| ERN | European Reference Network |
| fT4 | free thyroxine |
| HypoDok | German registry for congenital hypothyroidism |
| L-T4 | levothyroxine |
| PPV | positive predictive value |
| S2k | consensus-based guideline |
| Tg | thyreoglobuline |
| TPO | thyroid peroxidase |
| TRH | thyrotropin-releasing hormone |
| TSH | thyroid-stimulating hormone |
| TSHR-Ab | thyroid-stimulating hormone (TSH) receptor antibody |
| TT4 | total thyroxine |
References
- Zdraveska, N.; Kocova, M.; Nicholas, A.K.; Anastasovska, V.; Schoenmakers, N. Genetics of Gland-in-situ or Hypoplastic Congenital Hypothyroidism in Macedonia. Front. Endocrinol. 2020, 11, 413. [Google Scholar] [CrossRef]
- Tuli, G.; Munarin, J.; Tessaris, D.; Matarazzo, P.; Einaudi, S.; de Sanctis, L. Incidence of primary congenital hypothyroidism and relationship between diagnostic categories and associated malformations. Endocrine 2020. [CrossRef]
- Deutsche Gesellschaft für Neugeborenenscreening e.V. DGNS Screeningreports 2004–2017. Available online: http://www.screening-dgns.de/reports.php (accessed on 15 October 2020).
- Bettendorf, M. Thyroid disorders in children from birth to adolescence. Eur. J. Nucl. Med. Mol. Imaging 2002, 29 (Suppl. 2), S439–S446. [Google Scholar] [CrossRef] [PubMed]
- Peters, C.; van Trotsenburg, A.S.P.; Schoenmakers, N. DIAGNOSIS OF ENDOCRINE DISEASE: Congenital hypothyroidism: Update and perspectives. Eur. J. Endocrinol. 2018, 179, R297–R317. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine. Knowing What Works in Health Care: A Roadmap for the Nation; The National Academies Press: Washington, DC, USA, 2008; p. 278. [Google Scholar] [CrossRef]
- Lesho, E.P.; Myers, C.P.; Ott, M.; Winslow, C.; Brown, J.E. Do clinical practice guidelines improve processes or outcomes in primary care? Mil. Med. 2005, 170, 243–246. [Google Scholar] [CrossRef] [PubMed]
- Barth, J.H.; Misra, S.; Aakre, K.M.; Langlois, M.R.; Watine, J.; Twomey, P.J.; Oosterhuis, W.P. Why are clinical practice guidelines not followed? Clin. Chem. Lab. Med. 2016, 54, 1133–1139. [Google Scholar] [CrossRef] [PubMed]
- Krude, H. Diagnostik, Therapie und Verlaufskontrolle der Primären Angeborenen Hypothyreose. Available online: https://www.awmf.org/uploads/tx_szleitlinien/027-017l_S2k_Primaere_Angeborene_Hypothyreose_2011-abgelaufen.pdf (accessed on 20 September 2020).
- Rose, S.R.; Brown, R.S.; Foley, T.; Kaplowitz, P.B.; Kaye, C.I.; Sundararajan, S. Update of newborn screening and therapy for congenital hypothyroidism. Pediatrics 2006, 117, 2290–2303. [Google Scholar] [CrossRef] [PubMed]
- Leger, J.; Olivieri, A.; Donaldson, M.; Torresani, T.; Krude, H.; van Vliet, G.; Polak, M.; Butler, G.; Espe Pes Slep Jspe Apeg Appes, I.; Congenital Hypothyroidism Consensus Conference, G. European Society for Paediatric Endocrinology consensus guidelines on screening, diagnosis, and management of congenital hypothyroidism. J. Clin. Endocrinol. Metab. 2014, 99, 363–384. [Google Scholar] [CrossRef] [PubMed]
- Blümel, P.; Köstl, G. Konnatale Hypothyreose—Diagnose und Behandlungsempfehlung der APEDÖ. J. Für Klin. Endokrinol. Stoffwechs. 2019, 12, 14–18. [Google Scholar] [CrossRef]
- Ali, S.R.; Bryce, J.; Cools, M.; Korbonits, M.; Beun, J.G.; Taruscio, D.; Danne, T.; Dattani, M.; Dekkers, O.M.; Linglart, A.; et al. The current landscape of European registries for rare endocrine conditions. Eur. J. Endocrinol. 2019, 180, 89–98. [Google Scholar] [CrossRef]
- Ellerbroek, V.L.; Bonfig, W.; Dorr, H.G.; Bettendorf, M.; Hauffa, B.; Fricke-Otto, S.; Rohrer, T.; Reschke, F.; Schonau, E.; Schwab, K.O.; et al. Long-term Surveillance of Children with Congenital Hypothyroidism: Data from the German Registry for Congenital Hypothyroidism (AQUAPE “Hypo Dok”). Klin. Padiatr. 2015, 227, 199–205. [Google Scholar] [CrossRef] [PubMed]
- Institute of Epidemiology and Medical Biometry, University of Ulm. Anonymized AQUAPE/Hypothyroidism-Data Export HypoDok. Available online: https://buster.zibmt.uni-ulm.de/projekte/Hypothyreose/software (accessed on 30 April 2020).
- Gruters, A.; Krude, H. Detection and Treatment of Congenital Hypothyroidism. Nat. Rev. Endocrinol. 2011, 8, 104–113. [Google Scholar] [CrossRef]
- Universitätsklinik für Kinder- und Jugendheilkunde, Medizinische Universität Wien. Zahlen und Daten Neugeborenen-Screening. Available online: https://www.meduniwien.ac.at/hp/fileadmin/neugeborenenscreening/pdf/Zahlen_und_Daten_aus_dem_Neugeborenenscreening_2019.pdf (accessed on 8 January 2021).
- Gesundheit, B.F. Einführung eines Neugeborenen-Hörscreenings. Available online: https://www.g-ba.de/beschluesse/681/ (accessed on 7 May 2020).
- Inouye, B.M.; Dionise, Z.R.; Jiang, R.; Wolf, S.; Nicholl, L.; Pomann, G.M.; Wiener, J.S.; Purves, J.T.; Routh, J.C. National Imaging and Antibiotic Practice Patterns in Children Presenting With Urinary Tract Infection to Community Practices: Little Impact From the American Academy of Pediatrics Guidelines? Clin. Pediatr. 2019, 58, 1302–1308. [Google Scholar] [CrossRef] [PubMed]
- McMullan, B.J.; Hall, L.; James, R.; Mostaghim, M.; Jones, C.A.; Konecny, P.; Blyth, C.C.; Thursky, K.A. Antibiotic appropriateness and guideline adherence in hospitalized children: Results of a nationwide study. J. Antimicrob. Chemother. 2019. [Google Scholar] [CrossRef]
- Newman, R.E.; Hedican, E.B.; Herigon, J.C.; Williams, D.D.; Williams, A.R.; Newland, J.G. Impact of a guideline on management of children hospitalized with community-acquired pneumonia. Pediatrics 2012, 129, e597–e604. [Google Scholar] [CrossRef] [PubMed]
- Vezzani, S.; Giannetta, E.; Altieri, B.; Barbonetti, A.; Bellastella, G.; Certo, R.; Cignarelli, A.; Cinti, F.; D’Andrea, S.; Di Dalmazi, G.; et al. An Italian Survey of Compliance with Major Guidelines for L-Thyroxine of Primary Hypothyroidism. Endocr. Pract. 2018, 24, 419–428. [Google Scholar] [CrossRef] [PubMed]
- Kelnar, C.J. Evidence-based child health: SIGN and NICE. Arch. Dis. Child. Educ. Pract. Ed. 2008, 93, 190–198. [Google Scholar] [CrossRef]
- James, B.C.; Hammond, M.E. The challenge of variation in medical practice. Arch. Pathol. Lab. Med. 2000, 124, 1001–1003. [Google Scholar] [CrossRef]
- Mäkelä, M. Changing Professional Practice—Theory and Practice of Clinical Guidelines Implementation; DSI: Copenhagen, Denmark, 1999. [Google Scholar]
- Matlock, K.A.; Corathers, S.D.; Yayah Jones, N.H. Untreated congenital hypothyroidism due to loss to follow-up: Developing preventive strategies through quality improvement. J. Pediatr. Endocrinol. Metab. 2018, 31, 987–994. [Google Scholar] [CrossRef]
- Schechter, M.S.; Fink, A.K.; Homa, K.; Goss, C.H. The Cystic Fibrosis Foundation Patient Registry as a tool for use in quality improvement. BMJ Qual. Saf. 2014, 23 (Suppl. 1), i9–i14. [Google Scholar] [CrossRef]
- Bongers-Schokking, J.J.; de Muinck Keizer-Schrama, S.M. Influence of timing and dose of thyroid hormone replacement on mental, psychomotor, and behavioral development in children with congenital hypothyroidism. J. Pediatr. 2005, 147, 768–774. [Google Scholar] [CrossRef] [PubMed]
- Oerbeck, B.; Sundet, K.; Kase, B.F.; Heyerdahl, S. Congenital hypothyroidism: Influence of disease severity and L-thyroxine treatment on intellectual, motor, and school-associated outcomes in young adults. Pediatrics 2003, 112, 923–930. [Google Scholar] [CrossRef] [PubMed]
- Aleksander, P.E.; Bruckner-Spieler, M.; Stoehr, A.M.; Lankes, E.; Kuhnen, P.; Schnabel, D.; Ernert, A.; Stablein, W.; Craig, M.E.; Blankenstein, O.; et al. Mean High-Dose l-Thyroxine Treatment Is Efficient and Safe to Achieve a Normal IQ in Young Adult Patients With Congenital Hypothyroidism. J. Clin. Endocrinol. Metab. 2018, 103, 1459–1469. [Google Scholar] [CrossRef]
- National Center for Advancing Translational Sciences. RaDaR- Rare Diseases Registry Program. Available online: https://registries.ncats.nih.gov/about-radar/ (accessed on 8 January 2021).
- Ali, S.R.; Bryce, J.; Tan, L.E.; Hiort, O.; Pereira, A.M.; van den Akker, E.L.T.; Appelman-Dijkstra, N.M.; Bertherat, J.; Cools, M.; Dekkers, O.M.; et al. The EuRRECa Project as a Model for Data Access and Governance Policies for Rare Disease Registries That Collect Clinical Outcomes. Int. J. Environ. Res. Public Health 2020, 17, 8743. [Google Scholar] [CrossRef] [PubMed]
- de Vries, F.; Bruin, M.; Cersosimo, A.; van Beuzekom, C.N.; Ahmed, S.F.; Peeters, R.P.; Biermasz, N.R.; Hiort, O.; Pereira, A.M. An overview of clinical activities in Endo-ERN: The need for alignment of future network criteria. Eur. J. Endocrinol. 2020, 183, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Storf, H.; Stausberg, J.; Kindle, G.; Quadder, B.; Schlangen, M.; Walter, M.C.; Uckert, F.; Wagner, T.O.F.; Strategiegruppe, N.R. Patient registries for rare diseases in Germany: Concept paper of the NAMSE strategy group. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2020, 63, 761–770. [Google Scholar] [CrossRef] [PubMed]
- German Childhoood Cancer Registry: Annual Report of 2018. Available online: https://www.kinderkrebsregister.de/dkkr/ergebnisse/jahresberichte.html (accessed on 3 August 2020).
| Statement 1 | Initial TSH determination sufficient to initiate confirmatory testing, TRH test not required |
| Statement 2 | Confirmation of CH by low serum fT4 or TT4 concentrations Premature infants/neonates in intensive care: fT4 and TT4 are required at same time |
| Statement 3 | Ultrasonography of thyroid gland should be performed Only restrictive use of scintigraphy |
| Statement 4 | Hearing test: at confirmation and in the course of treatment |
| Statement 7 | Start L-T4 therapy as early as possible At least before day 14 |
| Statement 8 | Initial daily L-thyroxine dose 10 µg/kg–15 µg/kg |
| Statement 9 | Timepoints for follow-up: 1, 2, and 4 weeks after start of therapy Subsequently at 3-month intervals during the first two years of life |
| Statement 11 | Monitoring of psychomotor development: During the first two years of therapy Before start of school |
| Group A “Before Guideline” 10/2001–1/2011 | Group B “After Guideline” 2/2011–05/2020 | p-Value | |
|---|---|---|---|
| Gestational age (weeks) | 40 (38; 41) (n = 314) | 40 (38; 41) (n = 327) | 1.00 |
| Birth weight [g] | 3370 (2951; 3690) (n = 320) | 3395 (2970; 3730) (n = 330) | 1.00 |
| Birth length [cm] | 51 (49; 53) (n = 259) | 51 (49; 53) (n = 324) | 1.00 |
| 10 min Apgar score | 10 (8;10) (n = 322) | 10 (8; 10) (n = 319) | 1.00 |
| Parental target height (Tanner) [cm] | 172.5 (168.5; 176.5) (n = 271) | 172.3 (168; 176) (n = 274) | 1.00 |
| Female [%] | 63.6 (n = 327) | 60.6 (n = 332) | 1.00 |
| Premature babies (<37 weeks) [%] | 8.6 (n = 314) | 10.4 (n = 327) | 1.00 |
| Year | Number of Confirmed Cases of CH in Newborn Screening | Number of New Cases of CH Documented in HypoDok | % N HypoDok/N Newborn Screening |
|---|---|---|---|
| (a) Germany | |||
| 2004 | 222 | 29 | 13.1 |
| 2005 | 187 | 22 | 11.8 |
| 2006 | 165 | 26 | 15.8 |
| 2007 | 163 | 35 | 21.5 |
| 2008 | 184 | 47 | 25.5 |
| 2009 | 195 | 52 | 26.7 |
| 2010 | 207 | 40 | 19.3 |
| 2011 | 207 | 36 | 17.4 |
| 2012 | 205 | 44 | 21.5 |
| 2013 | 211 | 43 | 20.4 |
| 2014 | 213 | 29 | 13.6 |
| 2015 | 235 | 29 | 12.3 |
| 2016 | 242 | 28 | 11.6 |
| 2017 | 279 | 39 | 14.0 |
| average | 208 | 36 | 17.5 |
| (b) Austria | |||
| 2015 | 25 | 2 | 8.0 |
| 2016 | 32 | 2 | 6.3 |
| 2017 | 35 | 4 | 11.4 |
| 2018 | 24 | 1 | 4.2 |
| 2019 | 31 | 5 | 16.1 |
| average | 29 | 3 | 10.3 |
| Group A “Before Guideline” 10/2001–1/2011 | Group B “After Guideline” 2/2011–05/2020 | p-Value | |
|---|---|---|---|
| (a) Diagnostics | |||
| TT4 and/or fT4 determined at diagnosis [%] † | 34.9 * (n = 327) | 24.4 * (n = 332) | 0.02 |
| Serum TSH determined at diagnosis [%] † | 36.1 * (n = 327) | 23.2 * (n = 332) | 0.002 |
| Ultrasonography performed [%] | 92.6 (n = 323) | 92.1 (n = 328) | 0.86 |
| Scintigraphy performed [%] | 5.0 (n = 318) | 1.6 (n = 309) | 0.17 |
| Hearing test 14 days around start of treatment [%] | 24.4 * (n = 172) | 11.8 * (n = 229) | 0.01 |
| (b) Treatment | |||
| Age at start of treatment [d] | 6 (5; 9) (n = 316) | 6 (5; 8) (n = 318) | 0.55 |
| Dose of L-T4 at start [µg/d] | 50 (50; 50) (n = 122) | 50 (50; 50) (n = 131) | 1.00 |
| (c) Treatment monitoring | |||
| Follow-ups during first year of life [n] | 5 (3; 7) (n = 293) | 5 (3; 7) (n = 320) | 0.58 |
| Follow-ups during second year of life [n] | 3 (2; 4) (n = 255) | 3 (2; 4) (n = 259) | 0.33 |
| Follow-up 1 week after start of treatment [%] | 24.2 (n = 327) | 32.5 (n = 332) | 0.17 |
| Follow-up 2 weeks after start of treatment [%] | 31.2 (n = 327) | 38.0 (n = 332) | 0.41 |
| Follow-up 3–4 weeks after start of treatment [%] | 34.0 (n = 327) | 41.9 (n = 332) | 0.29 |
| Hearing test performed within the first 3 years of life (%) | 46.4 (=276) | 40.0 (n = 320) | 0.58 |
| Developmental assessment performed [%] | 49.3 * (n = 302) | 24.8 * (n = 327) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thomann, J.; Tittel, S.R.; Voss, E.; Oeverink, R.; Palm, K.; Fricke-Otto, S.; Kapelari, K.; Holl, R.W.; Woelfle, J.; Bettendorf, M. Guideline Adherence and Registry Recruitment of Congenital Primary Hypothyroidism: Data from the German Registry for Congenital Hypothyroidism (HypoDok). Int. J. Neonatal Screen. 2021, 7, 10. https://doi.org/10.3390/ijns7010010
Thomann J, Tittel SR, Voss E, Oeverink R, Palm K, Fricke-Otto S, Kapelari K, Holl RW, Woelfle J, Bettendorf M. Guideline Adherence and Registry Recruitment of Congenital Primary Hypothyroidism: Data from the German Registry for Congenital Hypothyroidism (HypoDok). International Journal of Neonatal Screening. 2021; 7(1):10. https://doi.org/10.3390/ijns7010010
Chicago/Turabian StyleThomann, Julia, Sascha R. Tittel, Egbert Voss, Rudolf Oeverink, Katja Palm, Susanne Fricke-Otto, Klaus Kapelari, Reinhard W. Holl, Joachim Woelfle, and Markus Bettendorf. 2021. "Guideline Adherence and Registry Recruitment of Congenital Primary Hypothyroidism: Data from the German Registry for Congenital Hypothyroidism (HypoDok)" International Journal of Neonatal Screening 7, no. 1: 10. https://doi.org/10.3390/ijns7010010
APA StyleThomann, J., Tittel, S. R., Voss, E., Oeverink, R., Palm, K., Fricke-Otto, S., Kapelari, K., Holl, R. W., Woelfle, J., & Bettendorf, M. (2021). Guideline Adherence and Registry Recruitment of Congenital Primary Hypothyroidism: Data from the German Registry for Congenital Hypothyroidism (HypoDok). International Journal of Neonatal Screening, 7(1), 10. https://doi.org/10.3390/ijns7010010






