Nasal Surgery Versus Pharyngeal Surgery in the Treatment of Obstructive Sleep Apnea
Abstract
:Introduction
Materials and Methods
Results
Discussion
Conclusions
Highlights
- ✓
- This study is based on a randomized interventional, prospective study on patients referred by the general practitioner (GP) to the outpatient department for query obstructive sleep apnea.
- ✓
- The diagnosis of OSA was made using a home sleep apnea test. The outcomes of both nasal and pharyngeal surgery were measured with the same home sleep apnea test.
- ✓
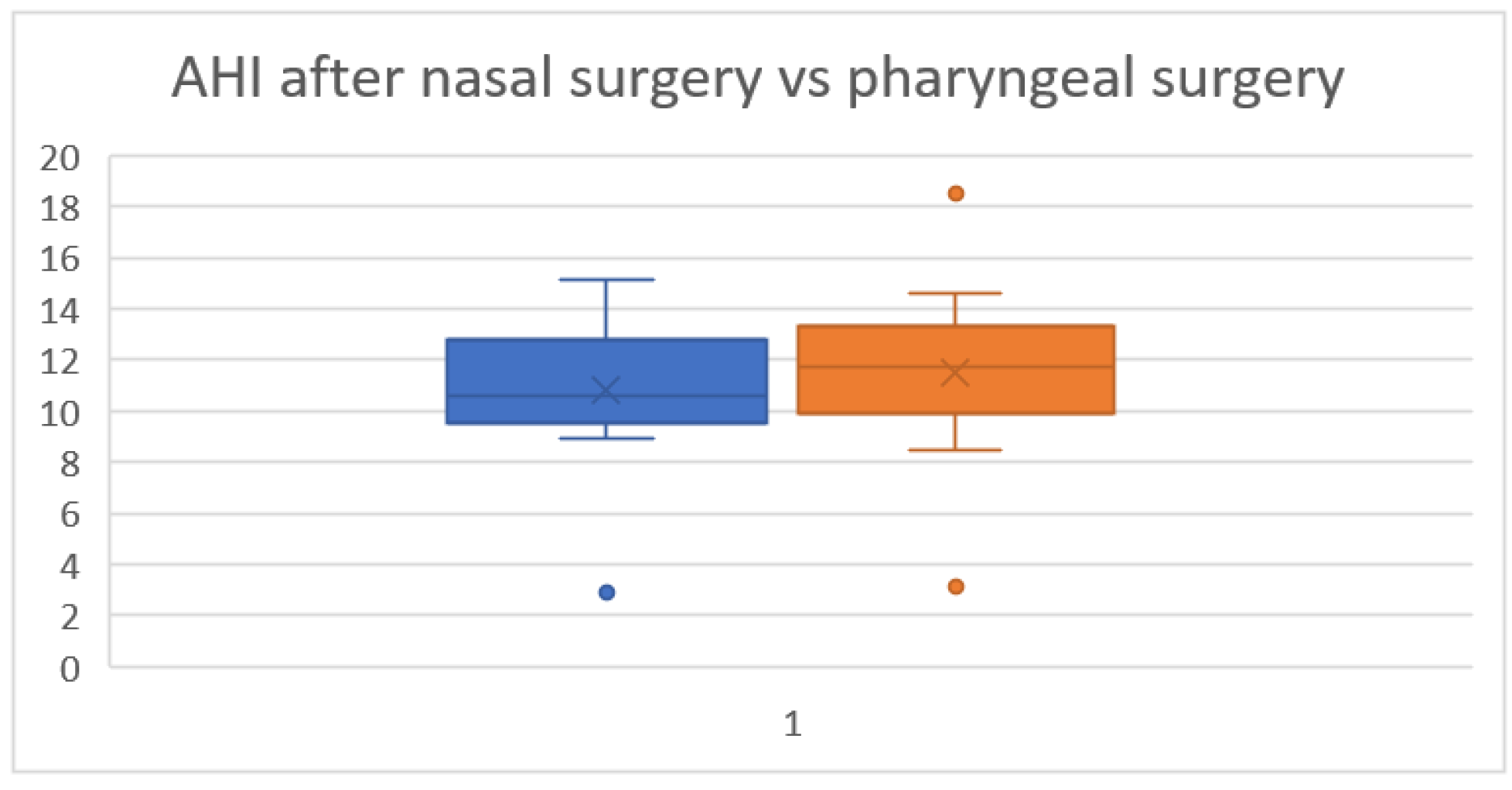
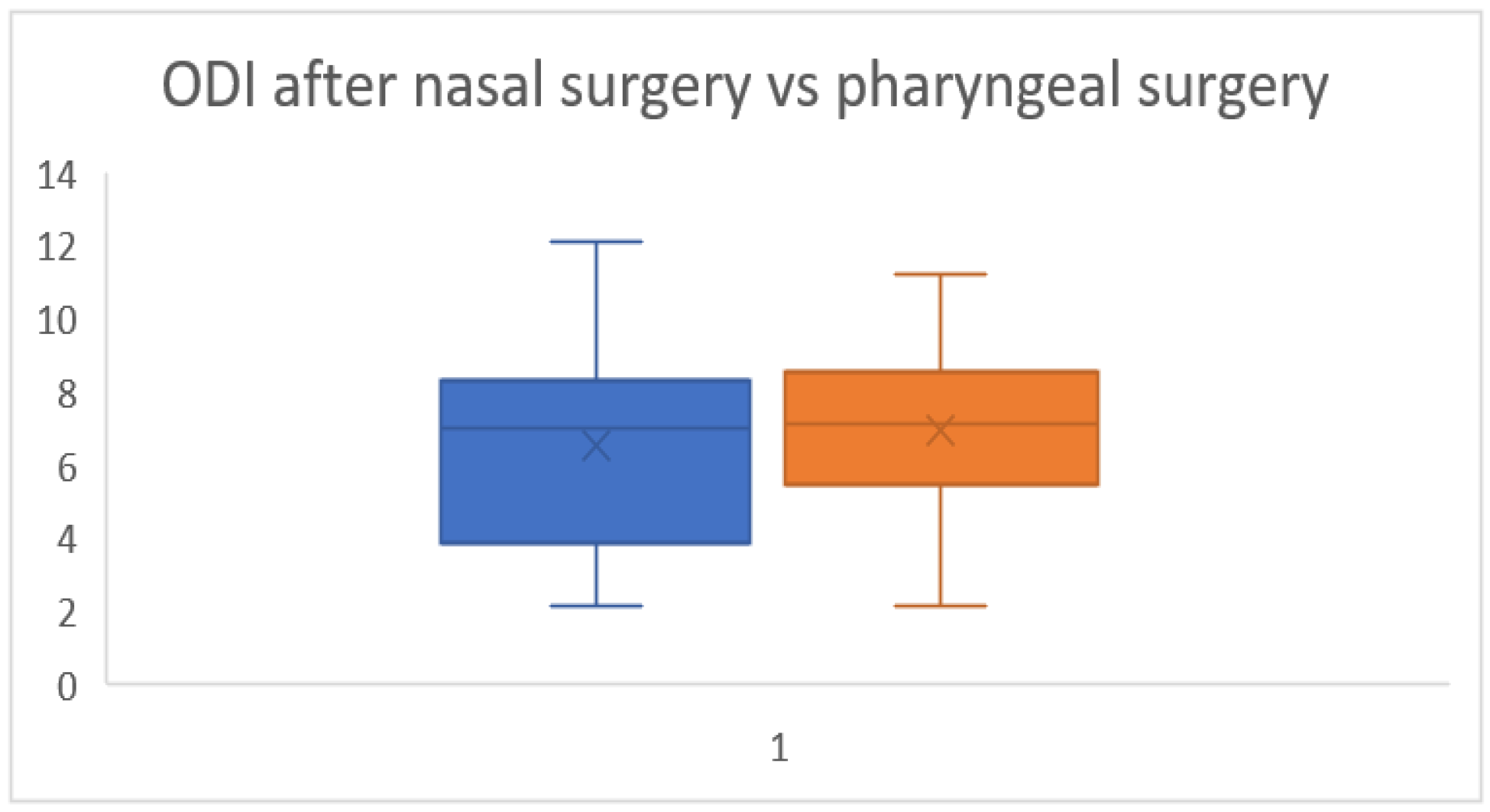
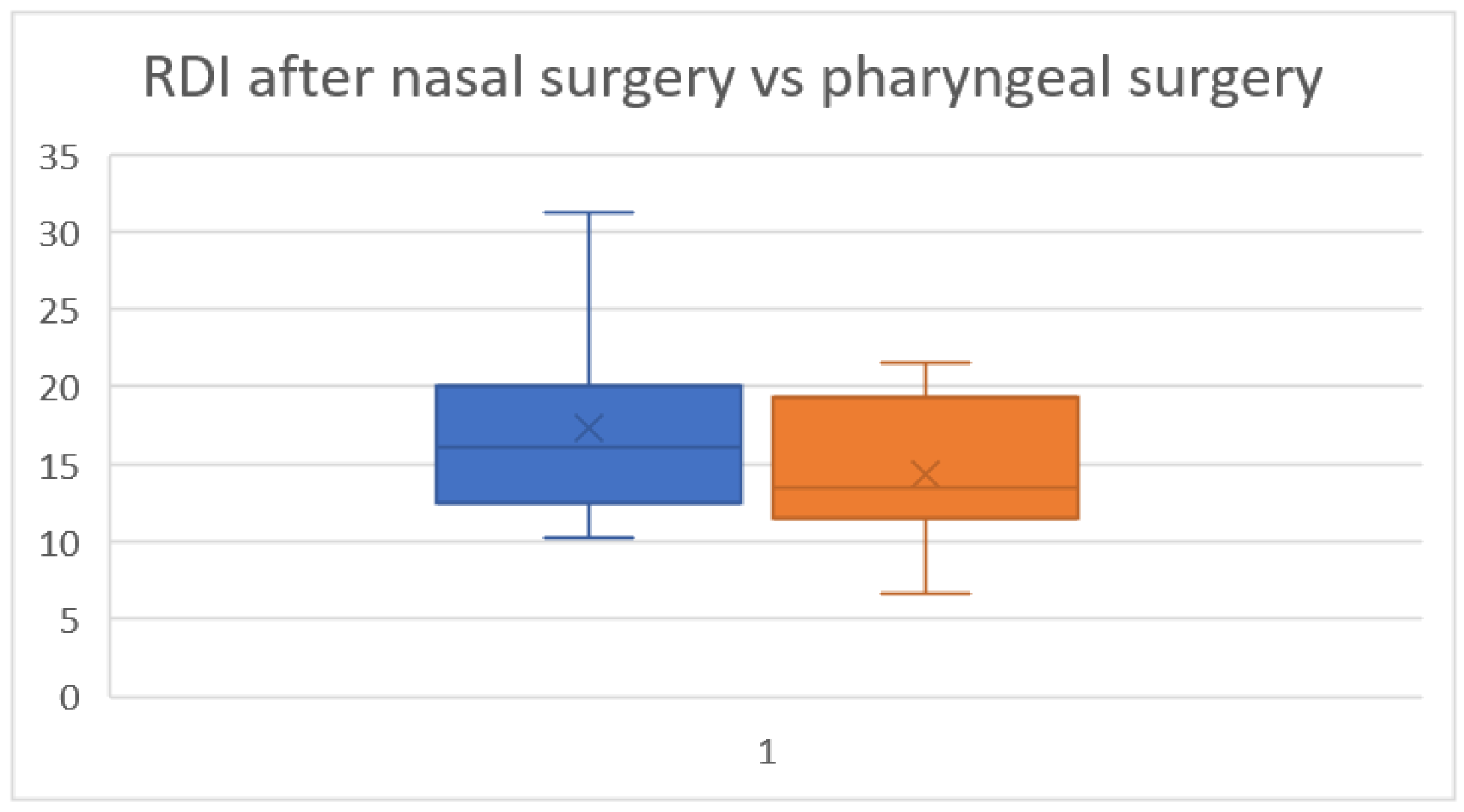
- Comparing the impact of nasal surgery and pharyngeal surgery on AHI, ODI and RDI it results in similar outcomes. Further larger studies are needed in order to obtain higher statistical power.
Conflict of Interest disclosure
Compliance with ethical standards
References
- Benjafield, A.V.; Ayas, N.T.; Eastwood, P.R.; Heinzer, R.; Ip, M.S.M.; Morrell, M.J.; Nunez, C.M.; Patel, S.R.; Penzel, T.; Pépin, J.L.; Peppard, P.E.; Sinha, S.; Tufik, S.; Valentine, K.; Malhotra, A. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. 2019, 7, 687–698. [Google Scholar] [CrossRef] [PubMed]
- Gami, A.S.; Olson, E.J.; Shen, W.K.; Wright, R.S.; Ballman, K.V.; Hodge, D.O.; Herges, R.M.; Howard, D.E.; Somers, V.K. Obstructive sleep apnea and the risk of sudden cardiac death: a longitudinal study of 10,701 adults. J Am Coll Cardiol. 2013, 62, 610–616. [Google Scholar] [CrossRef] [PubMed]
- Peppard, P.E.; Young, T.; Palta, M.; Skatrud, J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000, 342, 1378–1384. [Google Scholar] [CrossRef]
- Yaggi, H.K.; Concato, J.; Kernan, W.N.; Lichtman, J.H.; Brass, L.M.; Mohsenin, V. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005, 353, 2034–2041. [Google Scholar] [CrossRef] [PubMed]
- Reichmuth, K.J.; Austin, D.; Skatrud, J.B.; Young, T. Association of sleep apnea and type II diabetes: a population-based study. Am J Respir Crit Care Med. 2005, 172, 1590–1595. [Google Scholar] [CrossRef]
- Chiu, F.H.; Chang, Y.; Liao, W.W.; Yeh, Y.L.; Lin, C.M.; Jacobowitz, O.; Hsu, Y.S. Post-Operative Sleep Endoscopy with Target-Controlled Infusion After Palatopharyngoplasty for Obstructive Sleep Apnea: Anatomical and Polysomnographic Outcomes. Nat Sci Sleep. 2021, 13, 1181–1193. [Google Scholar] [CrossRef]
- Suceveanu, A.I.; Mazilu, L.; Katsiki, N.; Parepa, I.; Voinea, F.; Pantea-Stoian, A.; Rizzo, M.; Botea, F.; Herlea, V.; Serban, D.; Suceveanu, A.P. NLRP3 Inflammasome Biomarker-Could Be the New Tool for Improved Cardiometabolic Syndrome Outcome. Metabolites. 2020, 10, 448. [Google Scholar] [CrossRef]
- Rotenberg, B.W.; Vicini, C.; Pang, E.B.; Pang, K.P. Reconsidering first-line treatment for obstructive sleep apnea: a systematic review of the literature. J Otolaryngol Head Neck Surg. 2016, 45, 23. [Google Scholar] [CrossRef]
- Lin, C.M.; Davidson, T.M.; Ancoli-Israel, S. Gender differences in obstructive sleep apnea and treatment implications. Sleep Med Rev. 2008, 12, 481–496. [Google Scholar] [CrossRef]
- Deng, X.; Gu, W.; Li, Y.; Liu, M.; Li, Y.; Gao, X. Age-group-specific associations between the severity of obstructive sleep apnea and relevant risk factors in male and female patients. PLoS One. 2014, 9, e107380. [Google Scholar] [CrossRef]
- Ioacara, S.; Tiu, C.; Panea, C.; Nicolae, H.; Sava, E.; Martin, S.; Fica, S. Stroke Mortality Rates and Trends in Romania, 1994-2017. J Stroke Cerebrovasc Dis. 2019, 28, 104431. [Google Scholar] [CrossRef]
- Gurgu, R.S.; Ciobanu, A.M.; Danasel, R.I.; Panea, C.A. Psychiatric comorbidities in adult patients with epilepsy (A systematic review). Exp Ther Med. 2021, 22, 909. [Google Scholar] [CrossRef] [PubMed]
- Nitipir, C.; Baetu, A.; Voinea, A.; Pietrosanu, C.; Iaciu, C.; Voichitescu, M.; et al. Peripheral Neurotoxicity Induced by Taxanes, Cisplatin, Oxaliplatin, Fluoropyrimidines and Vinorelbine. A clinical perspective. Revista de Chimie (Rev. Chim.) 2018, 69, 3427–3432. [Google Scholar] [CrossRef]
- Bostan, M.; Petrică-Matei, G.G.; Ion, G.; Radu, N.; Mihăilă, M.; Hainăroşie, R.; Braşoveanu, L.I.; Roman, V.; Constantin, C.; Neagu, M.T. Cisplatin effect on head and neck squamous cell carcinoma cells is modulated by ERK1/2 protein kinases. Exp Ther Med. 2019, 18, 5041–5051. [Google Scholar] [CrossRef]
- Drăgoi, C.M.; Moroşan, E.; Dumitrescu, I.B.; Nicolae, A.C.; et al. Insights into chrononutrition: the innermost interplay amongst nutrition, metabolism and the circadian clock, in the context of epigenetic reprogramming. Farmacia. 2019, 67, 557–571. [Google Scholar] [CrossRef]
- Pang, K.P.; Montevecchi, F.; Vicini, C.; Carrasco-Llatas, M.; Baptista, P.M.; et al. Does nasal surgery improve multilevel surgical outcome in obstructive sleep apnea: A multicenter study on 735 patients. Laryngoscope Investig Otolaryngol. 2020, 5, 1233–1239. [Google Scholar] [CrossRef]
- Popescu, B.; Doinița, O.I.; Bălălău, C.; Scăunașu, R.; Manole, F.; Domuța, M.; Oancea, A.L.A. Fibroscopic examination on ENT patients in COVID-19 era. J Clin Investig Surg. 2020, 5, 63–65. [Google Scholar] [CrossRef]
- Deegan, P.C.; McNicholas, W.T. Predictive value of clinical features for the obstructive sleep apnoea syndrome. Eur Respir J. 1996, 9, 117–124. [Google Scholar] [CrossRef]
- Young, T.; Finn, L.; Kim, H. Nasal obstruction as a risk factor for sleep-disordered breathing. The University of Wisconsin Sleep and Respiratory Research Group. J Allergy Clin Immunol. 1997, 99, S757–S762. [Google Scholar] [CrossRef]
- Silvoniemi, P.; Suonpää, J.; Sipilä, J.; et al. Sleep disorders in patients with severe nasal obstruction due to septal deviation. Acta Otolaryngol Suppl. 1997, 529, 199–201. [Google Scholar] [CrossRef]
- Nakata, S.; Noda, A.; Yasuma, F.; Morinaga, M.; Sugiura, M.; Katayama, N.; Sawaki, M.; Teranishi, M.; Nakashima, T. Effects of nasal surgery on sleep quality in obstructive sleep apnea syndrome with nasal obstruction. Am J Rhinol. 2008, 22, 59–63. [Google Scholar] [CrossRef]
- Bican, A.; Kahraman, A.; Bora, I.; Kahveci, R.; Hakyemez, B. What is the efficacy of nasal surgery in patients with obstructive sleep apnea syndrome? J Craniofac Surg. 2010, 21, 1801–1806. [Google Scholar] [CrossRef]
- Verse, T.; Pirsig, W. Impact of impaired nasal breathing on sleep-disordered breathing. Sleep Breath. 2003, 7, 63–76. [Google Scholar] [CrossRef]
- Iozsa, D.A.; Costea, A.C.; Ionescu, N.S. Esophageal atresia associating gastrointestinal malformations: a study of clinical approach. J Mind Med Sci. 2021, 8, 273–279. [Google Scholar] [CrossRef]
- Popescu, B.; Oașă, I.D.; Bertesteanu, S.V.; Balalau, C.; Scaunasu, R.; et al. Emergency tracheostomy protocols in Coltea Clinical Hospital in patients with SARS-CoV-2 infection. J Clin Investig Surg. 2020, 5, 34–38. [Google Scholar] [CrossRef]
- Rama, A.N.; Tekwani, S.H.; Kushida, C.A. Sites of obstruction in obstructive sleep apnea. Chest. 2002, 122, 1139–1147. [Google Scholar] [CrossRef] [PubMed]
- Aliuș, C.; Bacalbașa, N.; Bălălău, C. Innovative Device for Indocianyne Green Navigational Surgery. J Mind Med Sci. 2020, 7, 40–45. [Google Scholar] [CrossRef]
- Marques, M.; Genta, P.R.; Azarbarzin, A.; Sands, S.A.; Taranto-Montemurro, L.; Messineo, L.; White, D.P.; Wellman, A. Retropalatal and retroglossal airway compliance in patients with obstructive sleep apnea. Respir Physiol Neurobiol. 2018, 258, 98–103. [Google Scholar] [CrossRef]
- Vroegop, A.V.; Vanderveken, O.M.; Boudewyns, A.N.; Scholman, J.; Saldien, V.; Wouters, K.; Braem, M.J.; Van de Heyning, P.H.; Hamans, E. Drug-induced sleep endoscopy in sleep-disordered breathing: report on 1,249 cases. Laryngoscope. 2014, 124, 797–802. [Google Scholar] [CrossRef]
- Vroegop, A.V.; Vanderveken, O.M.; Dieltjens, M.; Wouters, K.; Saldien, V.; Braem, M.J.; Van de Heyning, P.H. Sleep endoscopy with simulation bite for prediction of oral appliance treatment outcome. J Sleep Res. 2013, 22, 348–355. [Google Scholar] [CrossRef]
- Khan, A.; Ramar, K.; Maddirala, S.; Friedman, O.; Pallanch, J.F.; Olson, E.J. Uvulopalatopharyngoplasty in the management of obstructive sleep apnea: the mayo clinic experience. Mayo Clin Proc. 2009, 84, 795–800. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Guan, S.; Zhang, C.; Du, X.; Li, T.; Xiao, S. Nasopharyngeal tube effects on alleviating sleep hypoxemia during the first night following velopharyngeal surgery in patients with obstructive sleep apnea syndrome. J Clin Sleep Med. 2022. [Google Scholar] [CrossRef]
- Lechat, B.; Loffler, K.A.; Wallace, D.M.; Reynolds, A.; Appleton, S.L.; Scott, H.; Vakulin, A.; Lovato, N.; Adams, R.; Eckert, D.J.; Catcheside, P.G.; Sweetman, A. All-Cause Mortality in People with Co-Occurring Insomnia Symptoms and Sleep Apnea: Analysis of the Wisconsin Sleep Cohort. Nat Sci Sleep. 2022, 14, 1817–1828. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Liang, C.; Zhang, X.; Yu, H.; Yan, X.; Wang, L.; et al. Factors influencing patient delay in individuals with obstructive sleep apnoea: a study based on an integrated model. Ann Med. 2022, 54, 2828–2840. [Google Scholar] [CrossRef]
- Steward, K.A.; Silva, M.A.; Maduri, P.; Tang, X.; Wittine, L.; Dams-O'Connor, K.; Nakase-Richardson, R. Obstructive sleep apnea is associated with worse cognitive outcomes in acute moderate-to-severe traumatic brain injury: A TBI Model Systems study. Sleep Med. 2022, 100, 454–461. [Google Scholar] [CrossRef]
- Cunningham, T.J.; Kishore, D.; Guo, M.; Igue, M.; Malhotra, A.; Stickgold, R.; Djonlagic, I. The Effect of Obstructive Sleep Apnea on Sleep-Dependent Emotional Memory Consolidation. Ann Am Thorac Soc. 2022. [Google Scholar] [CrossRef]
- Zeng, Y.; Shu, Y.; Liu, X.; Li, P.; Kong, L.; Li, K.; Xie, W.; Zeng, L.; Long, T.; Huang, L.; Li, H.; Peng, D. Frequency-specific alterations in intrinsic low-frequency oscillations in newly diagnosed male patients with obstructive sleep apnea. Front Neurosci. 2022, 16, 987015. [Google Scholar] [CrossRef]
© 2022 by the author. 2022 Ruxandra Oana Alius, Viorel Zainea, Catalina Voiosu, Irina Gabriela Ionita, Andreea Rusescu, Oana Denisa Balalau, Catalin Alius, Raluca Oana Pulpa, Razvan Hainarosie
Share and Cite
Alius, R.O.; Zainea, V.; Voiosu, C.; Ionita, I.G.; Rusescu, A.; Balalau, O.D.; Alius, C.; Pulpa, R.O.; Hainarosie, R. Nasal Surgery Versus Pharyngeal Surgery in the Treatment of Obstructive Sleep Apnea. J. Mind Med. Sci. 2022, 9, 318-323. https://doi.org/10.22543/2392-7674.1347
Alius RO, Zainea V, Voiosu C, Ionita IG, Rusescu A, Balalau OD, Alius C, Pulpa RO, Hainarosie R. Nasal Surgery Versus Pharyngeal Surgery in the Treatment of Obstructive Sleep Apnea. Journal of Mind and Medical Sciences. 2022; 9(2):318-323. https://doi.org/10.22543/2392-7674.1347
Chicago/Turabian StyleAlius, Ruxandra Oana, Viorel Zainea, Catalina Voiosu, Irina Gabriela Ionita, Andreea Rusescu, Oana Denisa Balalau, Catalin Alius, Raluca Oana Pulpa, and Razvan Hainarosie. 2022. "Nasal Surgery Versus Pharyngeal Surgery in the Treatment of Obstructive Sleep Apnea" Journal of Mind and Medical Sciences 9, no. 2: 318-323. https://doi.org/10.22543/2392-7674.1347
APA StyleAlius, R. O., Zainea, V., Voiosu, C., Ionita, I. G., Rusescu, A., Balalau, O. D., Alius, C., Pulpa, R. O., & Hainarosie, R. (2022). Nasal Surgery Versus Pharyngeal Surgery in the Treatment of Obstructive Sleep Apnea. Journal of Mind and Medical Sciences, 9(2), 318-323. https://doi.org/10.22543/2392-7674.1347


