Abstract
Older age renders individuals vulnerable during public emergency crises. Considering that older adults are a highly heterogeneous and continuously growing demographic subgroup, this study aimed to assess the mental health impact of COVID-19 on two groups of older patients: a group of chronic physical disease and a group of chronic mental disease. A total of 102 patients completed the Fear of COVID-19 Scale, the Generalized Anxiety Disorder scale, the Brief Patient Health Questionnaire (PHQ-9) and several questions regarding demographic characteristics. Suicidality was assessed by the 9th item of the PHQ-9. According to the results, older chronic disease patients showed higher levels of fear, whereas anxiety and depressive symptoms were present mainly in the group of older psychiatric patients. Suicidality was reported from a subtotal of 25.4% that was composed of 7.8% chronic disease patients and 17.6% psychiatric patients. Chronic physical disease and higher anxiety predicted more severe COVID-19-related fear.
Introduction
Older adults received particular attention during the coronavirus disease 2019 (COVID-19) pandemic. Intrinsic factors, such as the higher prevalence of chronic diseases as well as the age-related immunosenescence and frailty, rendered them more vulnerable to severe COVID-19 illness. In addition, extrinsic factors, such as limited access to healthcare facilities for COVID-19-unrelated conditions, the strict quarantine measures, as well as the possible limited acquaintance with communication technology, heightened the risk for physical and mental health deterioration [1].
Older age accounts for increased vulnerability to the stress imposed during public emergency crises [2] as it is related to both immunosenescence and increased prevalence of chronic conditions [3], factors raising the risk for severe COVID-19 and increasing mortality. In addition, older people may be in need of more care due to other disabilities or unpropitious psychosocial conditions [4].
Older individuals with underlying health conditions comprise the most vulnerable age group for life-threatening complications and death from COVID-19. In particular, oncology patients being immunocompromised are exposed to greater danger of suffering from Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) infection, due to both the underlying malignancy and anticancer treatments [5]. Oncologic patients are also particularly vulnerable to increased stress, due to fear of being contaminated by the virus, the agony of cancer’s progression and the health insecurities resulting from the gaps related to clinical care services [6].
Likewise, although cardiovascular comorbidity in COVID-19 patients increases mortality, similar fears kept heart disease patients away from seeking urgent health care, despite having symptoms [7]. In fact, the number of patients with heart attack who were admitted for urgent care has dropped by more than 50% during the COVID-19 outbreak, according to an extensive worldwide survey by the European Society of Cardiology [8]. Similarly, recent research has highlighted the consequences that chronic kidney disease patients are facing from skipping hemodialysis sessions due to fear of coronavirus infection and/or difficulties in transportation [9]. Limited access to both primary and emergency health care for non-COVID-19-related conditions probably affected older patients to a greater extent [1]. On top of the alarming implications on physical health, there is also concern about the pandemic’s impact on mental health. In a recent meta-analysis, chronic disease patients had a higher risk of depression and anxiety than other populations [10].
Aging is also associated with a high prevalence of cognitive and mood disorders, which have a negative impact on physical health and wellbeing [11]. Older individuals with a mental disorder prior to the beginning of the pandemic crisis are more susceptible to stress and more vulnerable to relapse [12].
The pandemic’s social consequences added to the frustration in older people with mental disorders as social distancing measures and isolation may exacerbate existing mental health conditions [13]. On top of that, according to a recent survey, the COVID-19 pandemic disrupted mental health services in 130 countries while the demand for mental health care services was on the rise due to uncertainty and fear [14]. Over 70% of the mental health services’ representatives reported disruptions in mental health care for older adults with a psychiatric condition.
Furthermore, psychiatric patients constitute a major challenge to the system, as they are potentially super-spreaders, struggling to properly appreciate the risks of the disease or stick to the necessary medical precautions [15]. According to a recent study of older bipolar patients, increased depressive and anxiety symptoms were significantly associated with fear for the virus and loneliness [16].
The many faces of fear during the current pandemic, e.g fear of becoming severely ill or dying, fear of transmitting the virus, fear of health deterioration due to the significant changes in health care delivery, fear of disconnecting with the close ones, add an additional burden to older adults [17]. Both positive and negative behavioral consequences arise from fear such as greater adherence to protective measures and control strategies or avoiding health care settings [18] and being hesitant to return to old habits [19].
Considering that older adults are a continuously growing demographic subgroup of particular research interest [20], and taking into account that the impact of COVID-19 on older adults may be uneven depending on sociocultural and other individual factors [21], this study aimed to assess fear of COVID-19 in two subgroups of older adults, i.e., a group of older patients with chronic physical disease and a group of older patients with chronic mental disease.
Materials and Methods
Participants and survey procedure
The study included 102 older adults who were divided into two groups: the first group (Chronic Disease Patients, CDP) included 50 participants undergoing treatment for a chronic physical condition (16 patients with cardiovascular disease, 21 patients with different types of cancer, and 13 patients undergoing hemodialysis due to chronic kidney disease) and the second group (Psychiatric Patients, PP) included 52 patients with a chronic psychiatric condition (18 patients with psychotic disorder and 34 with affective disorder), all recruited from the hospital’s outpatient clinics.
Inclusion criteria were age over 60 years, receiving treatment for a chronic physical or mental disease, and acceptance to participate. Exclusion criteria were confirmed SARS-CoV-2 infection and current diagnosis of any neurocognitive disorder. Clinical interviews were held by a trained psychiatrist who acquainted patients with the study goals, the voluntary nature of participation, the right to withdraw at any moment, and the assurance that data would be kept anonymous, once submitted. Written consent was obtained from each participant before data collection. Ethical approval was granted from the Papageorgiou General Hospital Review Board (563/2020) prior to data collection.
Measures
Sociodemographic information was obtained from medical records and a sociodemographic form. In addition, patients completed the Greek versions of the following psychometric scales:
- The Fear of COVID-19 scale (FCV-19S) [22,23] contains 7 items (e.g., item 1, “I am most afraid of coronavirus-19”) assessing fear of COVID-19 on a 5-item Likert-type response scale from 1 (strongly disagree) to 5 (strongly agree). The total score ranges from a minimum of 7 to a maximum of 35 and it is obtained by summing all items. The scale is widely used and validated in many languages and different age groups [24,25]. A cut-off point score of 16.5 or higher was proposed to discriminate high levels of fear from normal fear reactions [26]. The Cronbach’s alpha internal consistency coefficient of the scale in the current study was .86.
- The Generalized Anxiety Disorder (GAD-7) [27,28] contains 7 items (e.g., item 1, “Feeling nervous, anxious or on edge”) assessing anxiety symptoms on a 4-point Likert-type scale from 0 (not at all) to 3 (nearly every day). The total score ranges from a minimum of 0 to a maximum of 21 and it is obtained by summing all items. A cut-off point score of 10 or higher indicates clinically significant anxiety [27]. The Cronbach’s alpha internal consistency coefficient of the scale in the current study was .87.
- The Brief Patient Health Questionnaire (PHQ-9) Depression scale [29,30] contains 9 items (e.g., item 1, “Little interest or pleasure in doing things”) assessing depressive symptoms on a 4-point Likert type scale from 0 (not at all) to 3 (nearly every day). The total score ranges from a minimum of 0 to a maximum of 27, and it is obtained by summing all items. A cut-off point score of 10 or higher indicates clinically significant depressive symptomatology. The Cronbach’s alpha internal consistency coefficient of the scale in the current study was .83.
- The last item of PHQ-9 was used to explore suicidal thoughts (i.e., “Over the last two weeks, how often have you been bothered by thoughts that you would be better off dead or of hurting yourself in some way?”). Previous studies have assessed the validity of item 9 by comparisons with clinical interviewing results [31,32]. The item was proved to be a strong predictor of suicidality in different age groups [33] and it was used in the current study to explore suicidal ideation.
Data analysis
All statistical analyses were performed using SPSS 26.0 (IBM Corp), with p<.05 as the level of statistical significance. Data were presented as mean values (M), standard deviations (SD), numbers and percentages. One-way analysis of variance was used to ascertain the presence of FCV-19S differences among type of disease. To analyze the differences in levels of fear, anxiety, depression and suicidality, independent sample t-tests were used to compare the mean scores between the two groups. Effect sizes are reported as Cohen’s d. Finally, to identify significant predictors of fear, a three-stage hierarchical regression was conducted with FCV-19S as the dependent variable.
Results
Sociodemographic data
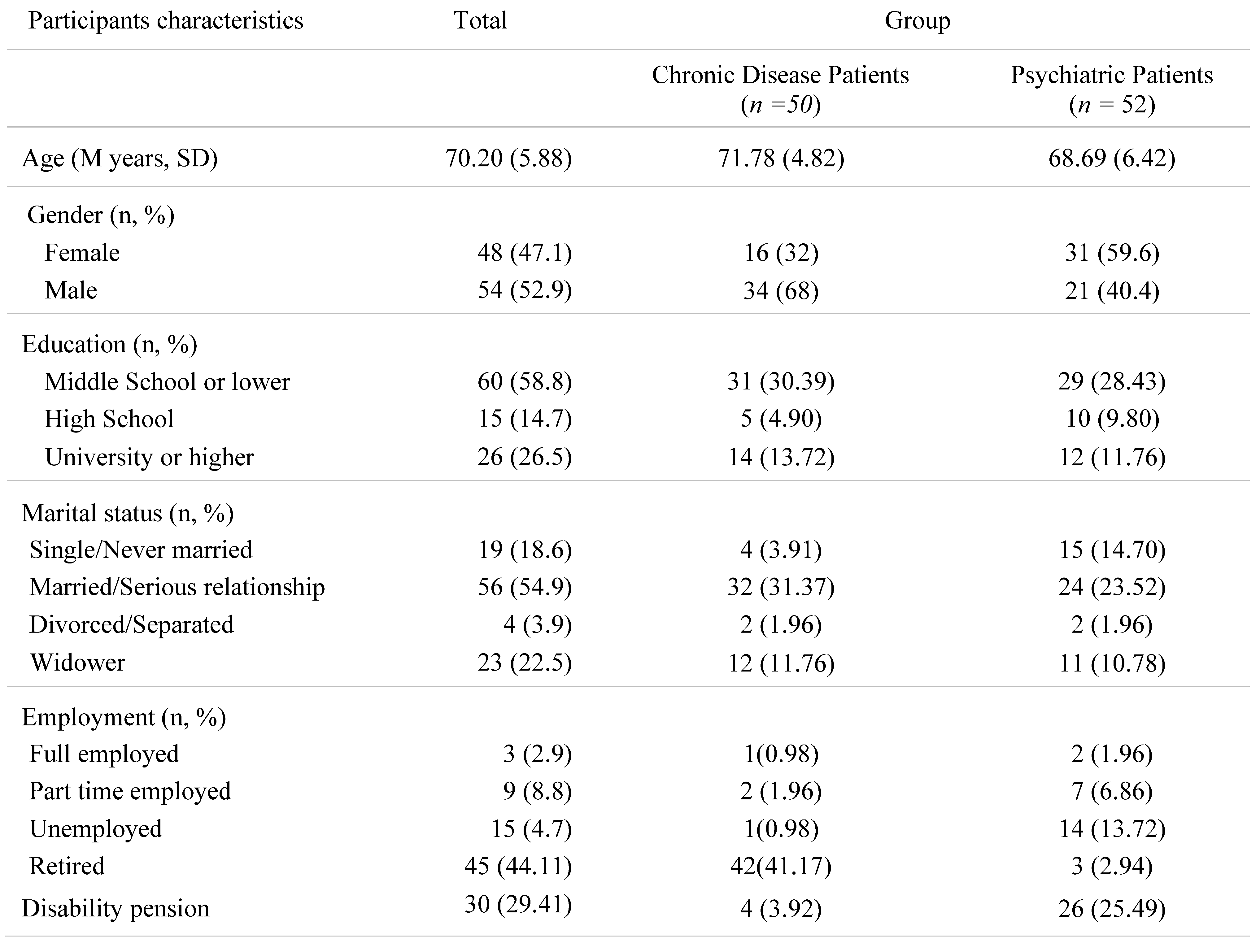
A total of 102 patients [47 females (46.07%) and 55 males (53.93%)] met the study inclusion criteria and were included in the study. Most of the participants completed 12 years of education or less, were married and retired. A significant percentage, mostly derived from the mental disease group, lived on a disability pension (Table 1).

Table 1.
Sociodemographic Characteristics.
Psychometric scales
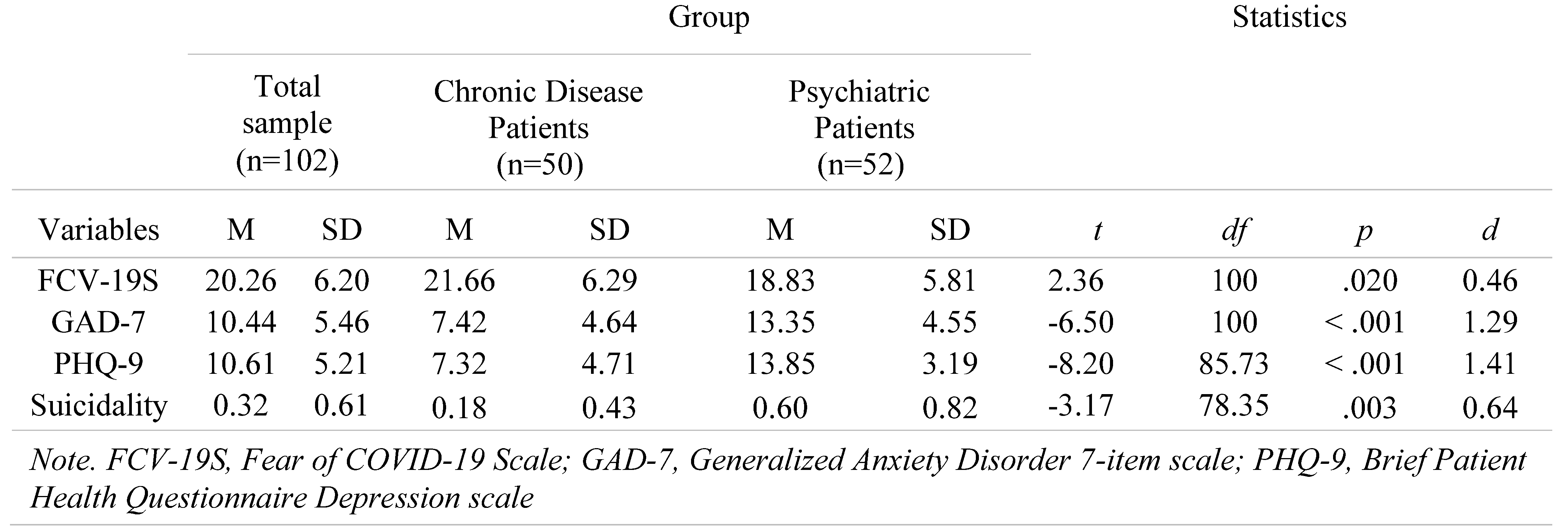
The mean FCV-19S total score for the chronic disease group was 21.66 (SD=6.29), which is statistically different [t(100)=2.36,p=.020,d=0.46] from the values obtained for the psychiatric disease group (M=18.83, SD=5.81) (Table 2).

Table 2.
Group Differences in Fear of COVID-19, Anxiety, Depression and Suicidality Scores.
High fear (FCV-19S scores >16.5) was reported from a subtotal of 72.5% composed of 38.23% chronic disease patients and 34.32% psychiatric patients. High anxiety (GAD-7 scores >10) was reported from a subtotal of 49.0% composed of 10.0% chronic disease patients and 39.0% psychiatric patients. High depressive symptomatology (PHQ-9 scores>10) was reported from a subtotal of 55% composed of 11% chronic disease patients and 44.0% psychiatric patients. Suicidality (PHQ-9 item 9 >0) was reported from a subtotal of 25.5% composed of 7.8% chronic disease patients and 17.6% psychiatric patients.
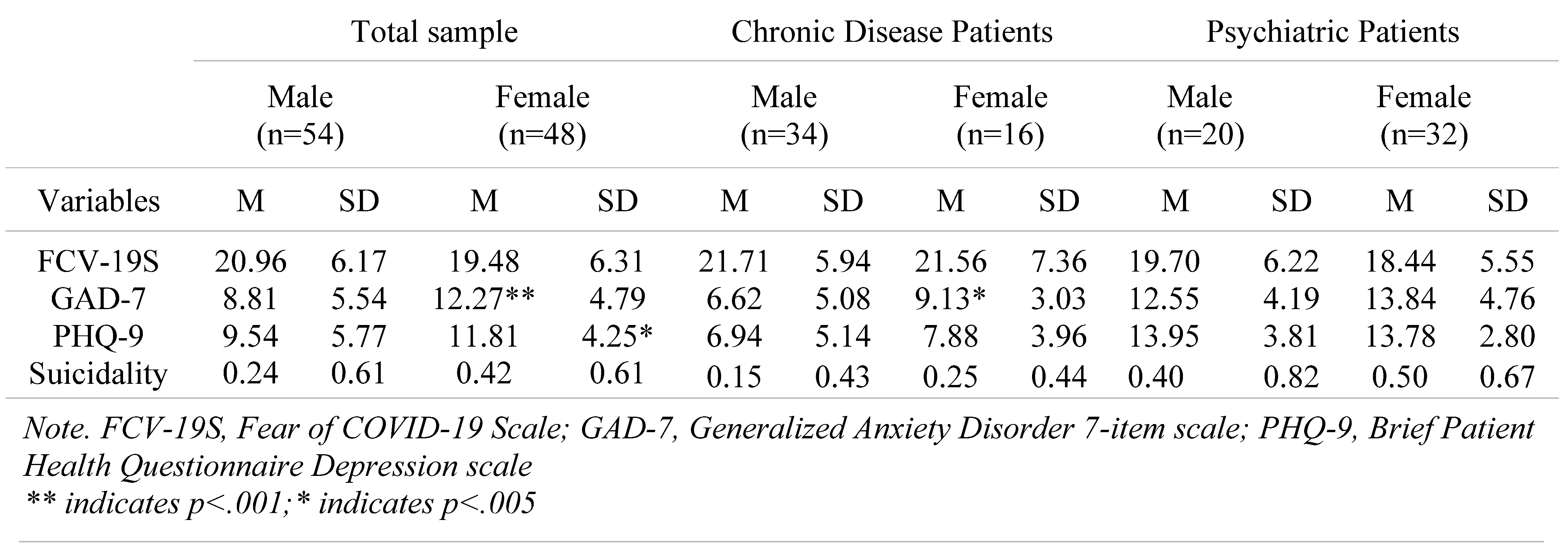
Gender comparisons
Gender comparisons in the total sample revealed statistically significant differences in anxiety as measured by GAD-7 [t(100)=-3.347, p=.001, d=.66] and in depression as measured by PHQ-9 [t(100)=-2.242, p=.025, d=.44]. Regarding FCV-19S, the result of the two-tailed independent samples t-test was not significant [t(100)=1.109, p=.230]. Similarly, regarding suicidality the result was also not significant [t(100)=-1.447, p=.151] (Table 3).

Table 3.
Gender Differences in Fear of COVID-19, Anxiety, Depression and Suicidality Scores.
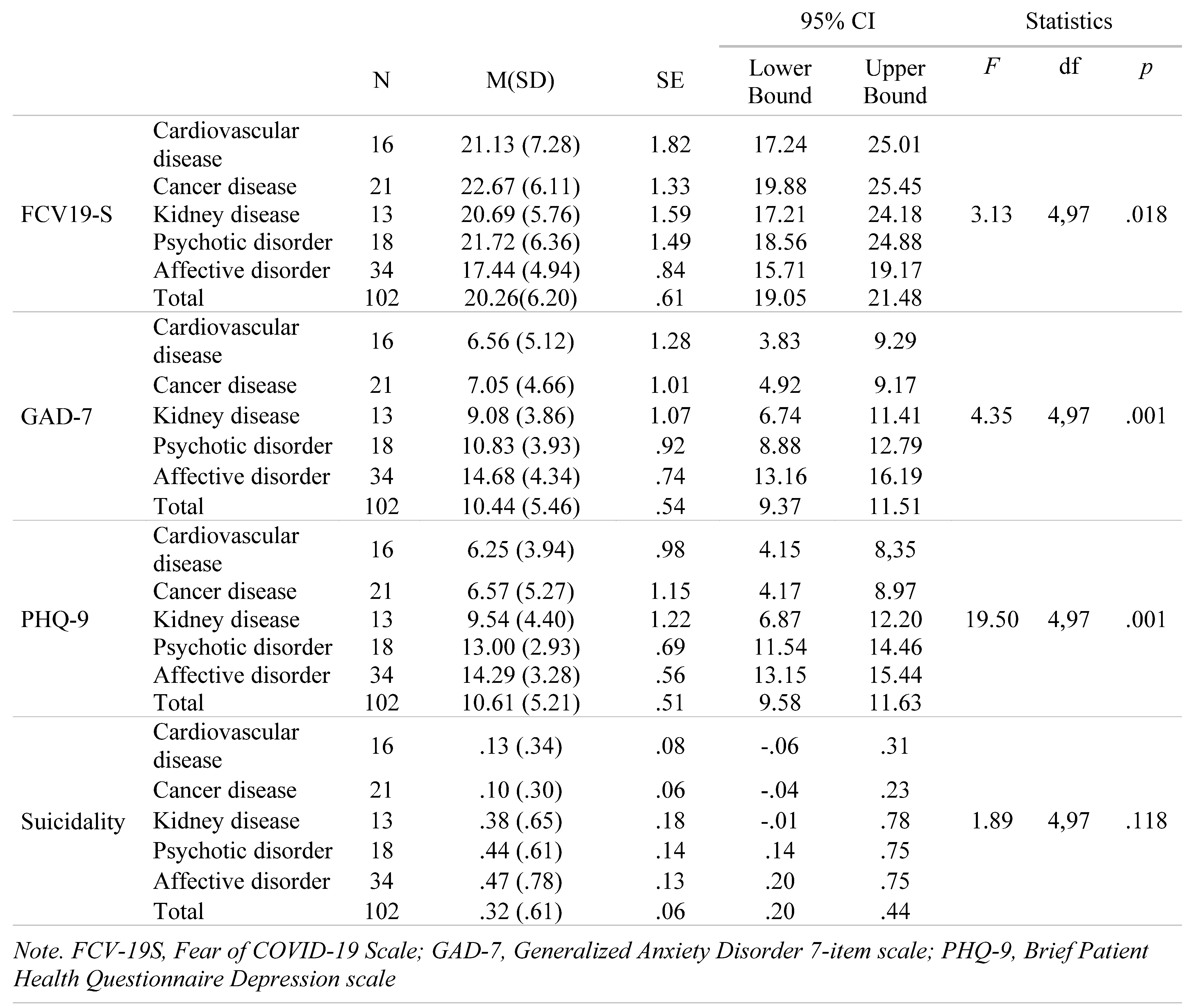
Type of disease
The participants with Cancer disease had the highest FCV-19S score and the 34 participants with Affective Disorder the lowest. The effect of type of disease was significant [F(4,97)=3.13, p=.018]. Patients with Cardiovascular disease, kidney disease and Psychotic disorder have also exceeded the cut-off score of 16.5, showing high levels of Fear of COVID-19 (Table 4).

Table 4.
Differences in Fear of COVID-19, Anxiety, Depression and Suicidality Scores by Disease.
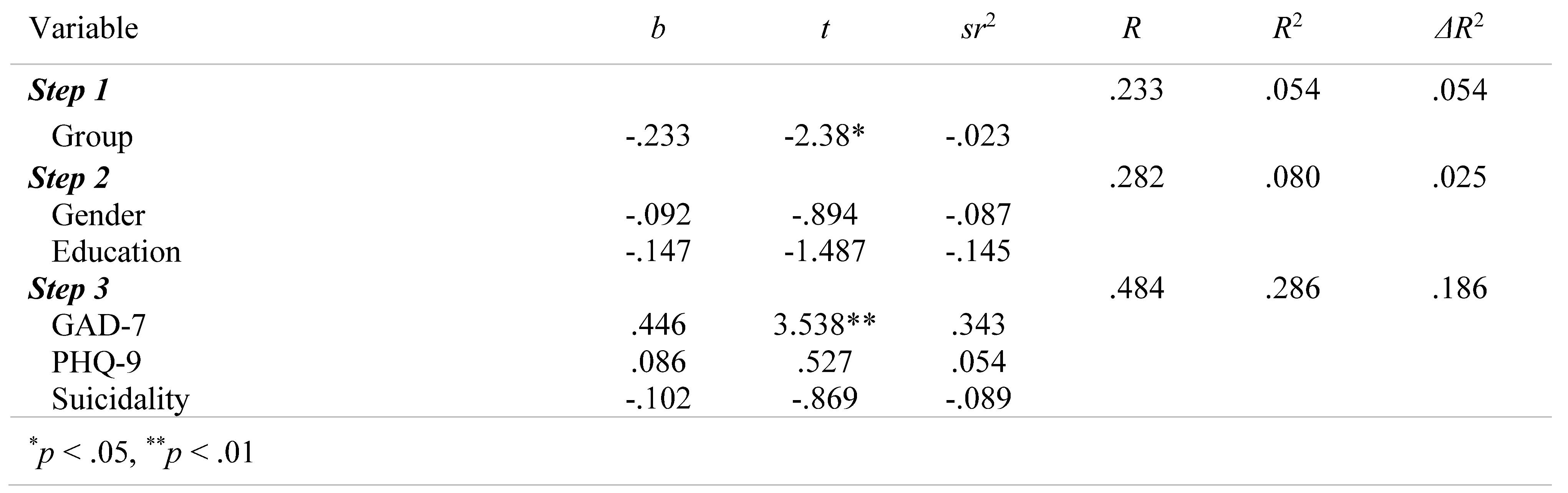
Linear regression analysis was performed to identify significant predictors of FCV-19S. All needed transformation was completed before the analysis and relevant statistical assumptions were met. A three-stage hierarchical regression was conducted with FCV-19S as the dependent variable. Group was entered at stage one of the regression. Gender and Education were entered at stage two, and GAD-7, PHQ-9 and suicidality at stage three.
Results revealed that at stage one, group contributed significantly to the regression model [F(1, 99)=5.67, p=.019, ΔR2=.54], accounting for 54.0% of the variation in FCV-19S.
The addition of Gender and Education resulted in a non-significant change in R2 [F (2,97)=5.67, p=.267]. Adding GAD-7, PHQ-9 and suicidality to the regression model explained an additional 15.5% of the variation in FCV-19S and this change in R² was significant [F (3,94)=6.34, p=.001] (Table 5).

Table 5.
Summary of Hierarchical Regression Analysis for Variables Predicting Fear of COVID-19.
Discussion
This study explored fear of COVID-19, anxiety, depressive symptoms and suicidality in two specific older subpopulations, that is, in older adults with chronic physical or mental disease, both conditions that may contribute to additional risk for mental health deterioration during the pandemic.
Both groups presented elevated fear of COVID-19 according to the proposed cut-off score [26]. High fear of COVID-19 among older adults is reported by several studies using the same measurement scale [17,34,35]. In a different study among 315 older adults in Turkey the mean FCV-19S score was somewhat below indicating mild fear reactions [36]. Using the COVID-19 Fear Inventory, some authors found highest fear levels among the oldest-old probably due to the higher health risks posed to this age group [37]. Increased fear of COVID-19 has been linked with higher anxiety and depression [38].
Patients with chronic physical diseases
Patients with chronic diseases reported significantly higher levels of fear than those with mental diseases. This result is in line with recent research among immunocompromised patients during the COVID-19 outbreak reporting that they were more likely to experience high levels of fear of COVID-19 [39,40]. In the current study cancer patients presented more fearful than other patients probably due to their state of immunosuppression or disruptions in treatment [41]. In a study of cancer patients, two months after the beginning of the pandemic lockdown in Poland, FCV-19S mean was 18.50 (SD=7.44), also indicating high levels of fear [42]. Contrary to this result, in a different study, although reporting high mean scores in FCV-19S cancer patients did not differ from healthy controls who also reported elevated fear of COVID-19 [43].
Participants with chronic physical disease reported mild anxiety and depressive symptoms. Only a 10% of the participants in this group reported anxiety symptoms and another 11% reported depressive symptomatology. This result is in line with a recent study among participants with chronic conditions (i.e., cancer, diabetes, obesity, and heart conditions), with a percentage of 14% presenting high levels of anxiety and 19% reporting depressive symptomatology [44]. In a comprehensive literature search of research articles assessing the mental health impact of COVID-19 on older adults it was shown that older adults were less distressed than younger ones, but they are exhibiting more severe anxiety and depressive symptoms during the pandemic than before [21].
Patients with chronic mental health diseases
In the current study patients with a pre-existing mental health condition showed elevated levels of fear of COVID-19 and high anxiety and depressive symptoms. Some reports have highlighted the psychological consequences of COVID-19 on patients with a mental health disorder, reporting relapses, fear of transmitting the virus, or symptoms centered around the pandemic [45]. At the beginning of the pandemic’s lockdown, individuals with pre-existing mental health conditions reported increased levels of anxiety and depressive symptomatology [46]. A longitudinal study that assessed symptoms of patients with mental health conditions, both before and during the COVID-19 pandemic, reported that for those with severe or chronic mental health disorders, the COVID-19 pandemic did not exacerbate their pre-existing symptoms, but individuals with less severe mental health conditions experienced increased levels of worry, anxiety and depressive symptomatology [47]. In a multisite comparative effectiveness study of 73 older adults (age >60) with pre-existing diagnosis of depression, no changes were found in regard to symptoms of clinical depression, anxiety, or suicidal thoughts compared to symptoms assessed before the pandemic [48]. Finally, compared to those with no mental disorder, respondents with a mood disorder were more likely to express concern for access to appropriate medical care, and were less likely to be concerned about dying of COVID-19 themselves [49].
Concerning suicidal ideation, only a small percentage of respondents reported suicidal thoughts mainly from the mental disease group. This result is in line with a web study that investigated the prevalence of suicidal ideation in the community during restriction measures in Greece. According the results, out of 5,116 adults a subtotal of 5.20% reported suicidal thoughts [50].
Gender
No differences were found between males and females regarding FCV-19S. Several studies measuring fear of COVID-19 in older adults reported significantly higher scores in females [51,52,53], but this result may reflect the over-representation of females in their samples or the wide age range explored.
Taken together, the pandemic probably disproportionately affected older adults across different countries depending on case fatality rates, availability of healthcare resources, and sociocultural factors. Although there was evidence that the prevalence of mental health symptoms may have increased in older adults [17], several studies indicated that older adults were able to tolerate the stress imposed by the pandemic, possibly due to previous experiences with traumatic events. As such, they proved to be adaptable to the new circumstances and resilient against psychological distress [54,55].
Older adults are considered to be a vulnerable population during public health crises, but the 21st century is a century related with progress in healthcare provision, medical and communication technology. The COVID-19 vaccine was timely developed and, in several countries, including Greece, older adults were the first to receive it showing high levels of vaccine acceptance [56]. In addition, although there was evidence that older adults among the general population may express higher levels of COVID-19-related fear and worry [57], they may be resilient against the psychological strain imposed by the pandemic [58,59].
Limitations
Although most research on the impact of the COVID-19 pandemic on mental health is based on online studies and convenience samples, this study based its findings on clinical interviews. Qualitative data derived from these interviews will be presented separately, to further describe how outcomes of the fear of COVID-19 on mental health could differ between population groups. However, limitations need to be addressed as the data were driven from a cross-sectional study design, reporting results from self-completed questionnaires, therefore jeopardizing the opportunity to report causal conclusions and being prone to social convenience biases.
Conclusions
Fear of COVID-19 seems to trouble older adults, especially those with a chronic physical disease, as they try to address the challenges imposed from the global medical crisis. At the beginning of the pandemic there were voices predicting an increase in mental health disorders, such as anxiety depression, and suicidality. Despite these predictions, in Greece the “mental health pandemic” with increased suicidality rates is not yet verified. That does not mean that researchers’ predictions should be taken lightly since the pandemic is still ongoing and severe consequences may become apparent in a later time.
Conflict of interest disclosure
There are no known conflicts of interest in the publication of this article. The manuscript was read and approved by all authors.
Compliance with ethical standards
Any aspect of the work covered in this manuscript has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript.
References
- United Nations. Policy Brief: The impact of COVID-19 on older persons. 2020. Available online: https://www.paho.org/en/documents/policy-brief-impact-covid-19-older-persons.
- Hutton David & World Health Organization. Ageing and Life Course Unit. Older people in emergencies: considerations for action and policy development. World Health Organization. 2008, pp. 44. Available online: https://apps.who.int/iris/handle/10665/43817.
- Clark, A.; Jit, M.; Warren-Gash, C.; Guthrie, B.; Wang, H.H.X.; Mercer, S.W.; Sanderson, C.; McKee, M.; Troeger, C.; Ong, K.L.; Checchi, F.; Perel, P.; Joseph, S.; Gibbs, H.P.; Banerjee, A.; Eggo, R.M.; Centre for the Mathematical Modelling of Infectious Diseases COVID-19 working group. Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study. Lancet Glob Health. 2020, 8, e1003–e1017. [Google Scholar] [CrossRef]
- Kar, N. Care of older persons during and after disasters: Meeting the challenge. Journal of Geriatric Care and Research 2016, 3, 7–12. [Google Scholar]
- Tsamakis, K.; Gavriatopoulou, M.; Schizas, D.; Stravodimou, A.; Mougkou, A.; Tsiptsios, D.; Sioulas, V.; Spartalis, E.; Sioulas, A.D.; Tsamakis, C.; Charalampakis, N.; Mueller, C.; Arya, D.; Zarogoulidis, P.; Spandidos, D.A.; Dimopoulos, M.A.; Papageorgiou, C.; Rizos, E. Oncology during the COVID-19 pandemic: challenges, dilemmas and the psychosocial impact on cancer patients. Oncol Lett. 2020, 20, 441–447. [Google Scholar] [CrossRef] [PubMed]
- Bandinelli, L.; Ornell, F.; von Diemen, L.; Kessler, F.H.P. The Sum of Fears in Cancer Patients Inside the Context of the COVID-19. Front Psychiatry. 2021, 12, 557834. [Google Scholar] [CrossRef] [PubMed]
- Nouskas, I.; Holeva, V.; Parlapani, E.; Nikopoulou, V.A.; Diakogiannis, I. A COVID-19 Patient Presenting With Paroxysmal Atrial Fibrillation. Cureus. 2021, 13, e17569. [Google Scholar] [CrossRef]
- Pessoa-Amorim, G.; Camm, C.F.; Gajendragadkar, P.; De Maria, G.L.; Arsac, C.; Laroche, C.; Zamorano, J.L.; Weidinger, F.; Achenbach, S.; Maggioni, A.P.; Gale, C.P.; Poppas, A.; Casadei, B. Admission of patients with STEMI since the outbreak of the COVID-19 pandemic: a survey by the European Society of Cardiology. Eur Heart J Qual Care Clin Outcomes. 2020, 6, 210–216. [Google Scholar] [CrossRef]
- Lee, J.; Steel, J.; Roumelioti, M.E.; Erickson, S.; Myaskovsky, L.; Yabes, J.G.; Rollman, B.L.; Weisbord, S.; Unruh, M.; Jhamb, M. Psychosocial Impact of COVID-19 Pandemic on Patients with End-Stage Kidney Disease on Hemodialysis. Kidney360. 2020, 1, 1390–1397. [Google Scholar] [CrossRef]
- Wu, T.; Jia, X.; Shi, H.; Niu, J.; Yin, X.; Xie, J.; Wang, X. Prevalence of mental health problems during the COVID-19 pandemic: A systematic review and meta-analysis. J Affect Disord. 2021, 281, 91–98. [Google Scholar] [CrossRef]
- Jordan, W.J. Mental Health & Drugs; A Map the Mind. J Mind Med Sci. 2020, 7, 133–140. [Google Scholar] [CrossRef]
- Yao, H.; Chen, J.H.; Xu, Y.F. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry. 2020, 7, e21. [Google Scholar] [CrossRef]
- Grolli, R.E.; Mingoti, M.E.D.; Bertollo, A.G.; Luzardo, A.R.; Quevedo, J.; Réus, G.Z.; Ignácio, Z.M. Impact of COVID-19 in the Mental Health in Elderly: Psychological and Biological Updates. Mol Neurobiol. 2021, 58, 1905–1916. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The impact of COVID-19 on mental, neurological and substance use services. Results of a rapid assessment. 2020. Available online: https://www.who.int/publications/i/item/978924012455.
- Brown, C.; Ruck Keene, A.; Hooper, C.R.; O'Brien, A. Isolation of patients in psychiatric hospitals in the context of the COVID-19 pandemic: An ethical, legal, and practical challenge. Int J Law Psychiatry. 2020, 71, 101572. [Google Scholar] [CrossRef] [PubMed]
- Orhan, M.; Korten, N.; Paans, N.; de Walle, B.; Kupka, R.; van Oppen, P.; Kok, A.; Sonnenberg, C.; Schouws, S.; Dols, A. Psychiatric symptoms during the COVID-19 outbreak in older adults with bipolar disorder. Int J Geriatr Psychiatry. 2021, 36, 892–900. [Google Scholar] [CrossRef] [PubMed]
- Parlapani, E.; Holeva, V.; Nikopoulou, V.A.; Sereslis, K.; Athanasiadou, M.; Godosidis, A.; Stephanou, T.; Diakogiannis, I. Intolerance of Uncertainty and Loneliness in Older Adults During the COVID-19 Pandemic. Front Psychiatry. 2020, 11, 842. [Google Scholar] [CrossRef]
- Harper, C.A.; Satchell, L.P.; Fido, D.; Latzman, R.D. Functional Fear Predicts Public Health Compliance in the COVID-19 Pandemic. Int J Ment Health Addict. 2021, 19, 1875–1888. [Google Scholar] [CrossRef]
- Holeva, V.; Parlapani, E.; Nikopoulou, V.A.; Kostikidou, S.; Diakogiannis, I. Hesitancy to Return to the Pre-pandemic Routine. J Ration Emot Cogn Behav Ther. 2022, 40, 23–39. [Google Scholar] [CrossRef]
- United Nations. World Population Ageing 2019: Highlights (ST/ESA/SER.A/430). 2019. Available online: https://www.un.org/en/development/desa/population/p ublications/pdf/ageing/WorldPopulationAgeing2019-Highlights.pdf.
- Parlapani, E.; Holeva, V.; Nikopoulou, V.A.; Kaprinis, S.; Nouskas, I.; Diakogiannis, I. A review on the COVID-19-related psychological impact on older adults: vulnerable or not? Aging Clin Exp Res. 2021, 33, 1729–1743. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Lin, C.Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The Fear of COVID-19 Scale: Development and Initial Validation. Int J Ment Health Addict. 2022, 20, 1537–1545. [Google Scholar] [CrossRef]
- Tsipropoulou, V.; Nikopoulou, V.A.; Holeva, V.; Nasika, Z.; Diakogiannis, I.; Sakka, S.; Kostikidou, S.; Varvara, C.; Spyridopoulou, E.; Parlapani, E. Psychometric Properties of the Greek Version of FCV-19S. Int J Ment Health Addict. 2021, 19, 2279–2288. [Google Scholar] [CrossRef]
- Muller, A.E.; Himmels, J.P.W.; Van de Velde, S. Instruments to measure fear of COVID-19: a diagnostic systematic review. BMC Med Res Methodol. 2021, 21, 82. [Google Scholar] [CrossRef]
- Voitsidis, P.; Kerasidou, M.D.; Nikopoulou, A.V.; Tsalikidis, P.; Parlapani, E.; Holeva, V.; Diakogiannis, I. A systematic review of questionnaires assessing the psychological impact of COVID-19. Psychiatry Res. 2021, 305, 114183. [Google Scholar] [CrossRef] [PubMed]
- Nikopoulou, V.A.; Holeva, V.; Parlapani, E.; Karamouzi, P.; Voitsidis, P.; Porfyri, G.N.; Blekas, A.; Papigkioti, K.; Patsiala, S.; Diakogiannis, I. Mental Health Screening for COVID-19: a Proposed Cutoff Score for the Greek Version of the Fear of COVID-19 Scale (FCV-19S). Int J Ment Health Addict. 2022, 20, 907–920. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- Skapinakis, P. The 2-item Generalized Anxiety Disorder scale had high sensitivity and specificity for detecting GAD in primary care. Evid Based Med. 2007, 12, 149. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Hyphantis, T.; Kotsis, K.; Voulgari, P.V.; Tsifetaki, N.; Creed, F.; Drosos, A.A. Diagnostic accuracy, internal consistency, and convergent validity of the Greek version of the patient health questionnaire 9 in diagnosing depression in rheumatologic disorders. Arthritis Care Res (Hoboken). 2011, 63, 1313–1321. [Google Scholar] [CrossRef]
- Razykov, I.; Hudson, M.; Baron, M.; Thombs, B.D.; Canadian Scleroderma Research Group. Utility of the Patient Health Questionnaire-9 to assess suicide risk in patients with systemic sclerosis. Arthritis Care Res (Hoboken). 2013, 65, 753–758. [Google Scholar] [CrossRef]
- Walker, J.; Hansen, C.H.; Hodges, L.; Thekkumpurath, P.; O'Connor, M.; Sharma, N.; Kleiboer, A.; Murray, G.; Kroenke, K.; Sharpe, M. Screening for suicidality in cancer patients using Item 9 of the nine-item patient health questionnaire; does the item score predict who requires further assessment? Gen Hosp Psychiatry. 2010, 32, 218–220. [Google Scholar] [CrossRef]
- Rossom, R.C.; Coleman, K.J.; Ahmedani, B.K.; Beck, A.; Johnson, E.; Oliver, M.; Simon, G.E. Suicidal ideation reported on the PHQ9 and risk of suicidal behavior across age groups. J Affect Disord. 2017, 215, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Mistry, S.K.; Ali, A.R.M.M.; Akther, F.; Yadav, U.N.; Harris, M.F. Exploring fear of COVID-19 and its correlates among older adults in Bangladesh. Global Health. 2021, 17, 47. [Google Scholar] [CrossRef]
- Yadav, U.N.; Yadav, O.P.; Singh, D.R.; Ghimire, S.; Rayamajhee, B.; Kanti Mistry, S.; Rawal, L.B.; Ali, A.M.; Kumar Tamang, M.; Mehta, S. Perceived fear of COVID-19 and its associated factors among Nepalese older adults in eastern Nepal: A cross-sectional study. PLoS One. 2021, 16, e0254825. [Google Scholar] [CrossRef] [PubMed]
- Gokseven, Y.; Ozturk, G.Z.; Karadeniz, E.; Sarı, E.; Tas, B.G.; Ozdemir, H.M. The Fear of COVID-19 Infection in Older People. J Geriatr Psychiatry Neurol. 2022, 35, 460–466. [Google Scholar] [CrossRef] [PubMed]
- Stroe, A.Z.; Stuparu, A.F.; Axelerad, S.D.; Axelerad, D.D.; Moraru, A. Neuropsychological symptoms related to the COVID-19 pandemic experienced by the general population and particularly by the healthcare personnel. J Mind Med Sci. 2021, 8, 197–208. [Google Scholar] [CrossRef]
- Voitsidis, P.; Nikopoulou, V.A.; Holeva, V.; Parlapani, E.; Sereslis, K.; Tsipropoulou, V.; Karamouzi, P.; Giazkoulidou, A.; Tsopaneli, N.; Diakogiannis, I. The mediating role of fear of COVID-19 in the relationship between intolerance of uncertainty and depression. Psychol Psychother. 2021, 94, 884–893. [Google Scholar] [CrossRef]
- Al-Rahimi, J.S.; Nass, N.M.; Hassoubah, S.A.; Wazqar, D.Y.; Alamoudi, S.A. Levels and predictors of fear and health anxiety during the current outbreak of COVID-19 in immunocompromised and chronic disease patients in Saudi Arabia: A cross-sectional correlational study. PLoS One. 2021, 16, e0250554. [Google Scholar] [CrossRef]
- Kohler, H.; Bäuerle, A.; Schweda, A.; Weismüller, B.; Fink, M.; Musche, V.; Robitzsch, A.; Pfeiffer, C.; Benecke, A.V.; Dörrie, N.; Führer, D.; Taube, C.; Rassaf, T.; Teufel, M.; Skoda, E.M. Increased COVID-19-related fear and subjective risk perception regarding COVID-19 affects behavior in individuals with internal high-risk diseases. J Prim Care Community Health. 2021, 12, 2150132721996898. [Google Scholar] [CrossRef]
- Guven, D.C.; Sahin, T.K.; Aktepe, O.H.; Yildirim, H.C.; Aksoy, S.; Kilickap, S. Perspectives, Knowledge, and Fears of Cancer Patients About COVID-19. Front Oncol. 2020, 10, 1553. [Google Scholar] [CrossRef]
- Sigorski, D.; Sobczuk, P.; Osmola, M.; Kuć, K.; Walerzak, A.; Wilk, M.; Ciszewski, T.; Kopeć, S.; Hryń, K.; Rutkowski, P.; Stec, R.; Szczylik, C.; Bodnar, L. Impact of COVID-19 on anxiety levels among patients with cancer actively treated with systemic therapy. ESMO Open. 2020, 5, e000970. [Google Scholar] [CrossRef]
- Musche, V.; Bäuerle, A.; Steinbach, J.; Schweda, A.; Hetkamp, M.; Weismüller, B.; Kohler, H.; Beckmann, M.; Herrmann, K.; Tewes, M.; Schadendorf, D.; Skoda, E.M.; Teufel, M. COVID-19-Related Fear and Health-Related Safety Behavior in Oncological Patients. Front Psychol. 2020, 11, 1984. [Google Scholar] [CrossRef]
- Budu, M.O.; Rugel, E.J.; Nocos, R.; Teo, K.; Rangarajan, S.; Lear, S.A. Psychological Impact of COVID-19 on People with Pre-Existing Chronic Disease. Int J Environ Res Public Health. 2021, 18, 5972. [Google Scholar] [CrossRef] [PubMed]
- Grover, S.; Suman, A.; Naskar, C.; Jagota, G.; Sahoo, S.; Mehra, A. Fear of spreading COVID-19 infection in a female with psychotic illness leading to suicidal and homicidal attempt: A case report. Asian J Psychiatr. 2021, 61, 102692. [Google Scholar] [CrossRef] [PubMed]
- Fancourt, D.; Steptoe, A.; Bu, F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry. 2021, 8, 141–149. [Google Scholar] [CrossRef]
- Pan, K.Y.; Kok, A.A.L.; Eikelenboom, M.; Horsfall, M.; Jörg, F.; Luteijn, R.A.; Rhebergen, D.; Oppen, P.V.; Giltay, E.J.; Penninx, B.W.J.H. The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: a longitudinal study of three Dutch case-control cohorts. Lancet Psychiatry. 2021, 8, 121–129. [Google Scholar] [CrossRef]
- Hamm, M.E.; Brown, P.J.; Karp, J.F.; Lenard, E.; Cameron, F.; Dawdani, A.; Lavretsky, H.; Miller, J.P.; Mulsant, B.H.; Pham, V.T.; Reynolds, C.F.; Roose, S.P.; Lenze, E.J. Experiences of American Older Adults with Pre-existing Depression During the Beginnings of the COVID-19 Pandemic: A Multicity, Mixed-Methods Study. Am J Geriatr Psychiatry. 2020, 28, 924–932. [Google Scholar] [CrossRef] [PubMed]
- Van Rheenen, T.E.; Meyer, D.; Neill, E.; Phillipou, A.; Tan, E.J.; Toh, W.L.; Rossell, S.L. Mental health status of individuals with a mood-disorder during the COVID-19 pandemic in Australia: Initial results from the COLLATE project. J Affect Disord. 2020, 275, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulou, A.; Efstathiou, V.; Yotsidi, V.; Pomini, V.; Michopoulos, I.; Markopoulou, E.; Papadopoulou, M.; Tsigkaropoulou, E.; Kalemi, G.; Tournikioti, K.; Douzenis, A.; Gournellis, R. Suicidal ideation during COVID-19 lockdown in Greece: Prevalence in the community, risk and protective factors. Psychiatry Res. 2021, 297, 113713. [Google Scholar] [CrossRef]
- Caycho-Rodríguez, T.; Tomás, J.M.; Barboza-Palomino, M.; Ventura-León, J.; Gallegos, M.; Reyes-Bossio, M.; Vilca, L.W. Assessment of Fear of COVID-19 in Older Adults: Validation of the Fear of COVID-19 Scale. Int J Ment Health Addict. 2022, 20, 1231–1245. [Google Scholar] [CrossRef]
- Lin, C.Y.; Hou, W.L.; Mamun, M.A.; Aparecido da Silva, J.; Broche-Pérez, Y.; Ullah, I.; Masuyama, A.; Wakashima, K.; Mailliez, M.; Carre, A.; Chen, Y.P.; Chang, K.C.; Kuo, Y.J.; Soraci, P.; Scarf, D.; Broström, A.; Griffiths, M.D.; Pakpour, A.H. Fear of COVID-19 Scale (FCV-19S) across countries: Measurement invariance issues. Nurs Open. 2021, 8, 1892–1908. [Google Scholar] [CrossRef]
- Pierce, M.; McManus, S.; Hope, H.; Hotopf, M.; Ford, T.; Hatch, S.L.; John, A.; Kontopantelis, E.; Webb, R.T.; Wessely, S.; Abel, K.M. Mental health responses to the COVID-19 pandemic: a latent class trajectory analysis using longitudinal UK data. Lancet Psychiatry. 2021, 8, 610–619. [Google Scholar] [CrossRef]
- Fuller, H.R.; Huseth-Zosel, A. Lessons in Resilience: Initial Coping Among Older Adults During the COVID-19 Pandemic. Gerontologist. 2021, 61, 114–125. [Google Scholar] [CrossRef]
- Röhr, S.; Reininghaus, U.; Riedel-Heller, S.G. Mental wellbeing in the German old age population largely unaltered during COVID-19 lockdown: results of a representative survey. BMC Geriatr. 2020, 20, 489. [Google Scholar] [CrossRef]
- Holeva, V.; Parlapani, E.; Nikopoulou, V.A.; Nouskas, I.; Diakogiannis, I. COVID-19 vaccine hesitancy in a sample of Greek adults. Psychol Health Med. 2022, 27, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Maxfield, M.; Pituch, K.A. COVID-19 worry, mental health indicators, and preparedness for future care needs across the adult lifespan. Aging Ment Health. 2021, 25, 1273–1280. [Google Scholar] [CrossRef] [PubMed]
- Bruine de Bruin, W. Age Differences in COVID-19 Risk Perceptions and Mental Health: Evidence From a National U.S. Survey Conducted in March 2020. J Gerontol B Psychol Sci Soc Sci. 2021, 76, e24–e29. [Google Scholar] [CrossRef]
- López, J.; Perez-Rojo, G.; Noriega, C.; Carretero, I.; Velasco, C.; Martinez-Huertas, J.A.; López-Frutos, P.; Galarraga, L. Psychological well-being among older adults during the COVID-19 outbreak: a comparative study of the young-old and the old-old adults. Int Psychogeriatr. 2020, 32, 1365–1370. [Google Scholar] [CrossRef]
© 2022 by the author. 2022 Oana Denisa Bălălău, Mihai George Loghin, Delia Maria Bogheanu, Nicolae Bacalbasa, Anca Daniela Stănescu, Daniela Gabriela Bălan, Ioana Păunică, Octavian Gabriel Olaru