Psychological and Psychiatric Characterization of Various Groups of Drugs Users
Abstract
:Introduction
Materials and Methods
Statistical analysis
Results
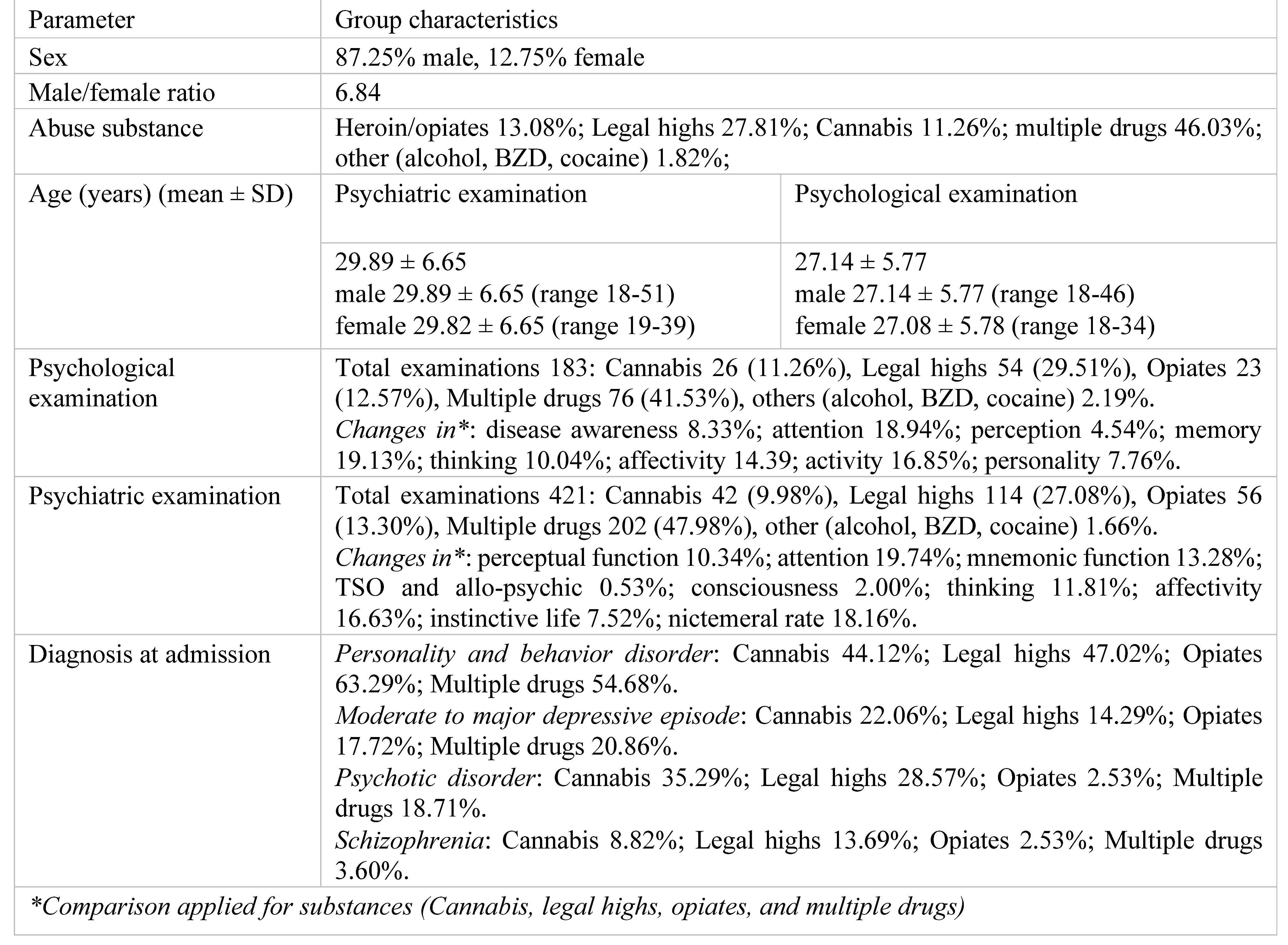
Group characteristics
- 1.
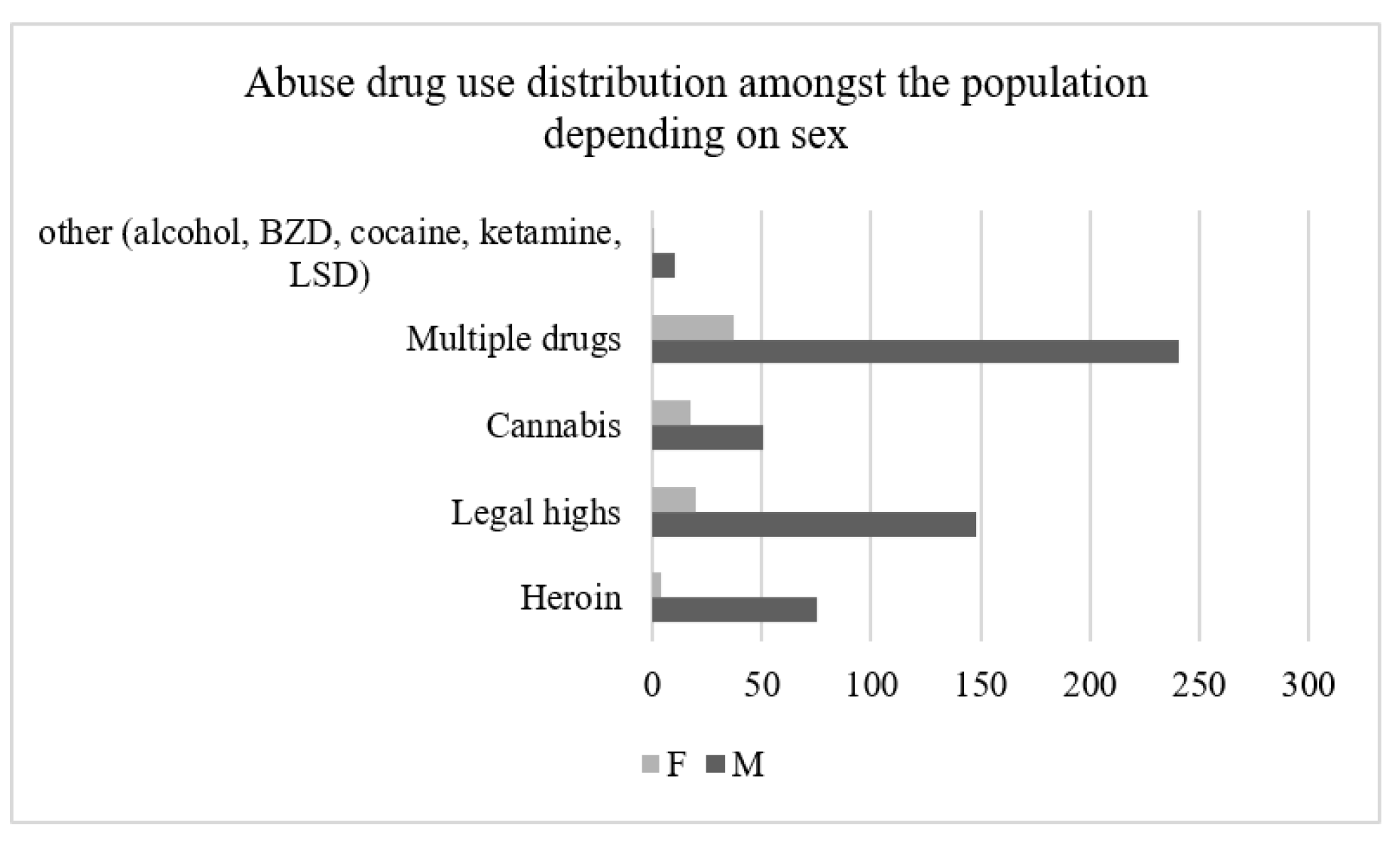
- Indicator: age and sex
- 2.
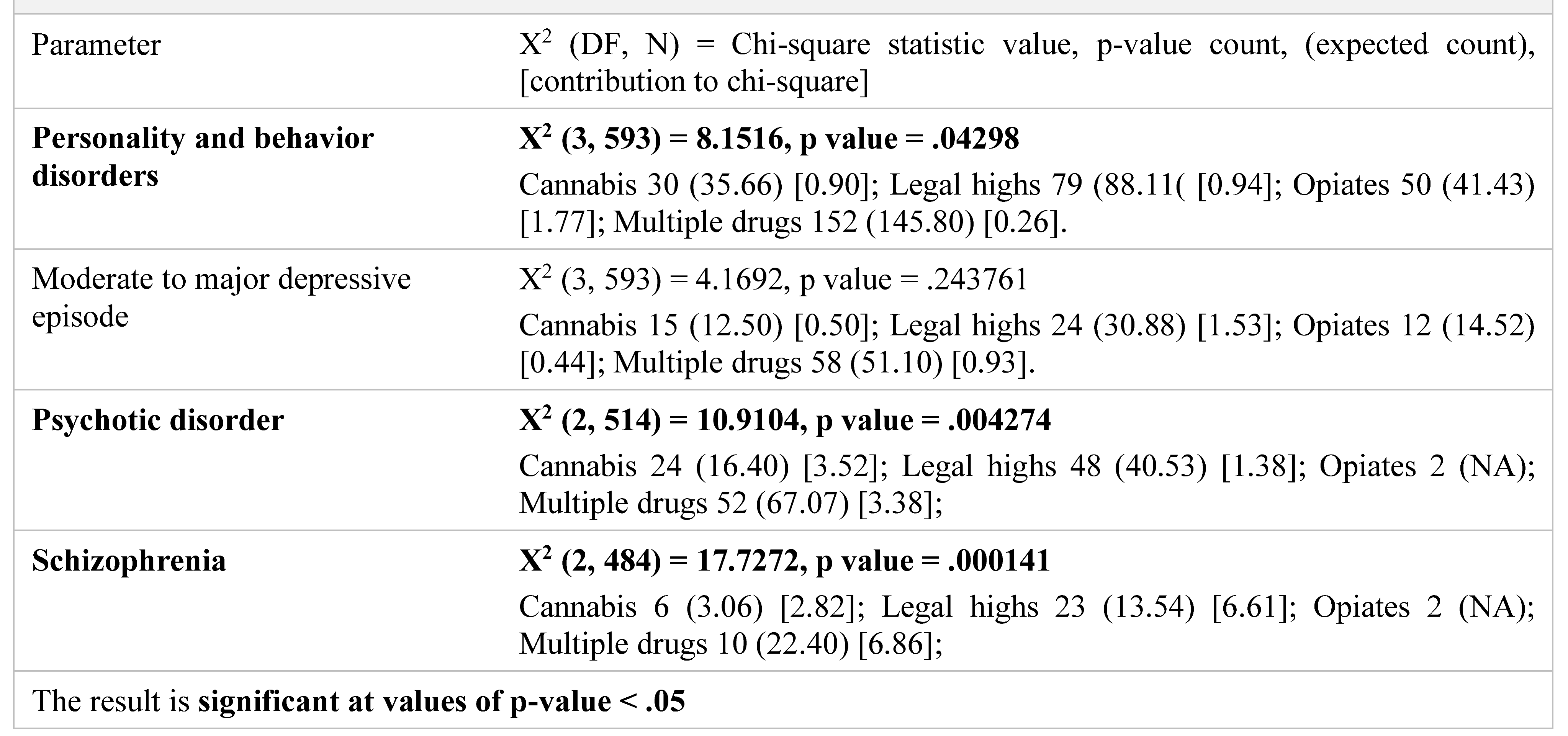
- Indicator: diagnosis at admission
- 3.
- Indicator: type of abuse substance
- 4.
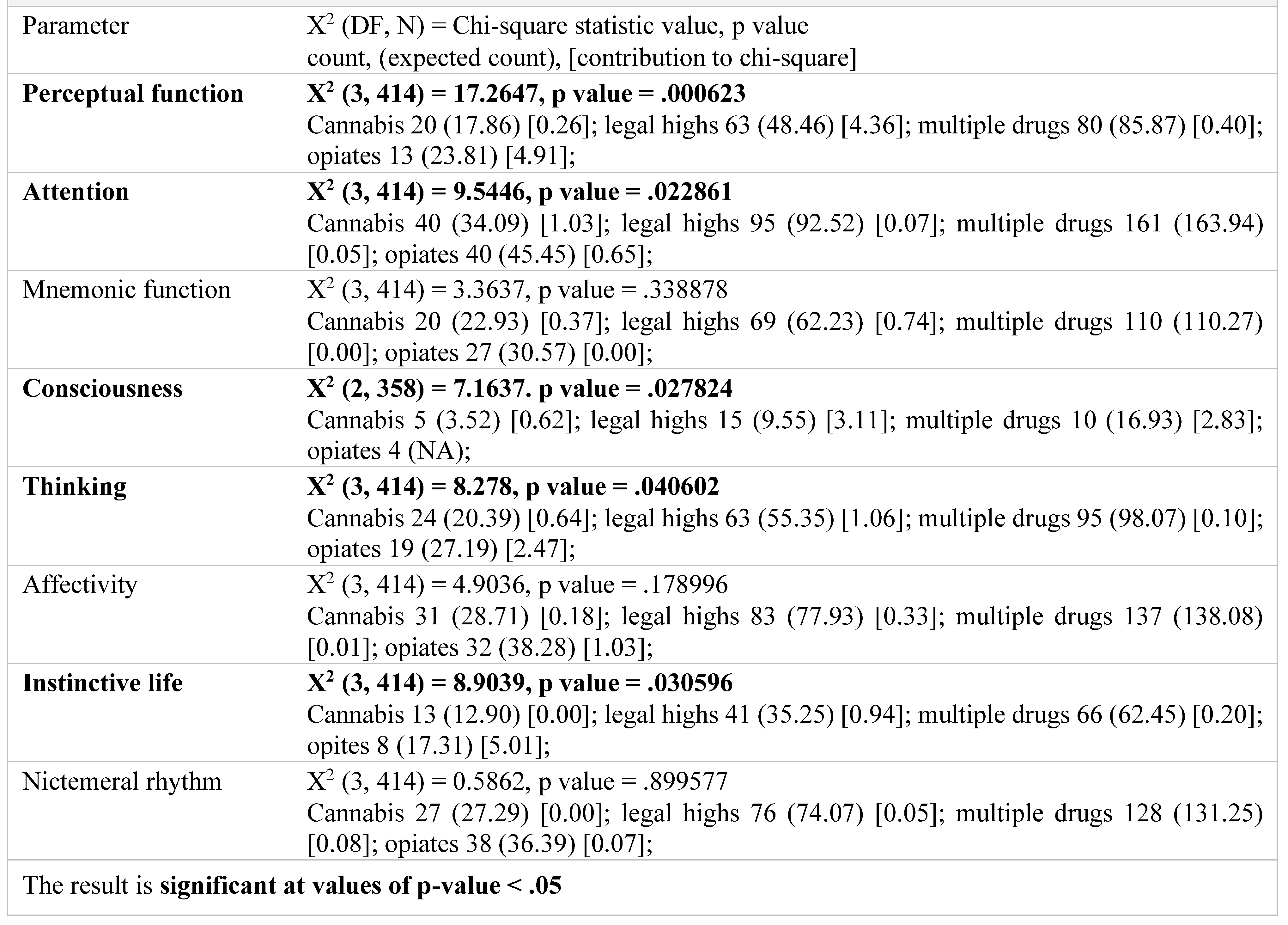
- Assessment of mental state
- Psychiatric examination
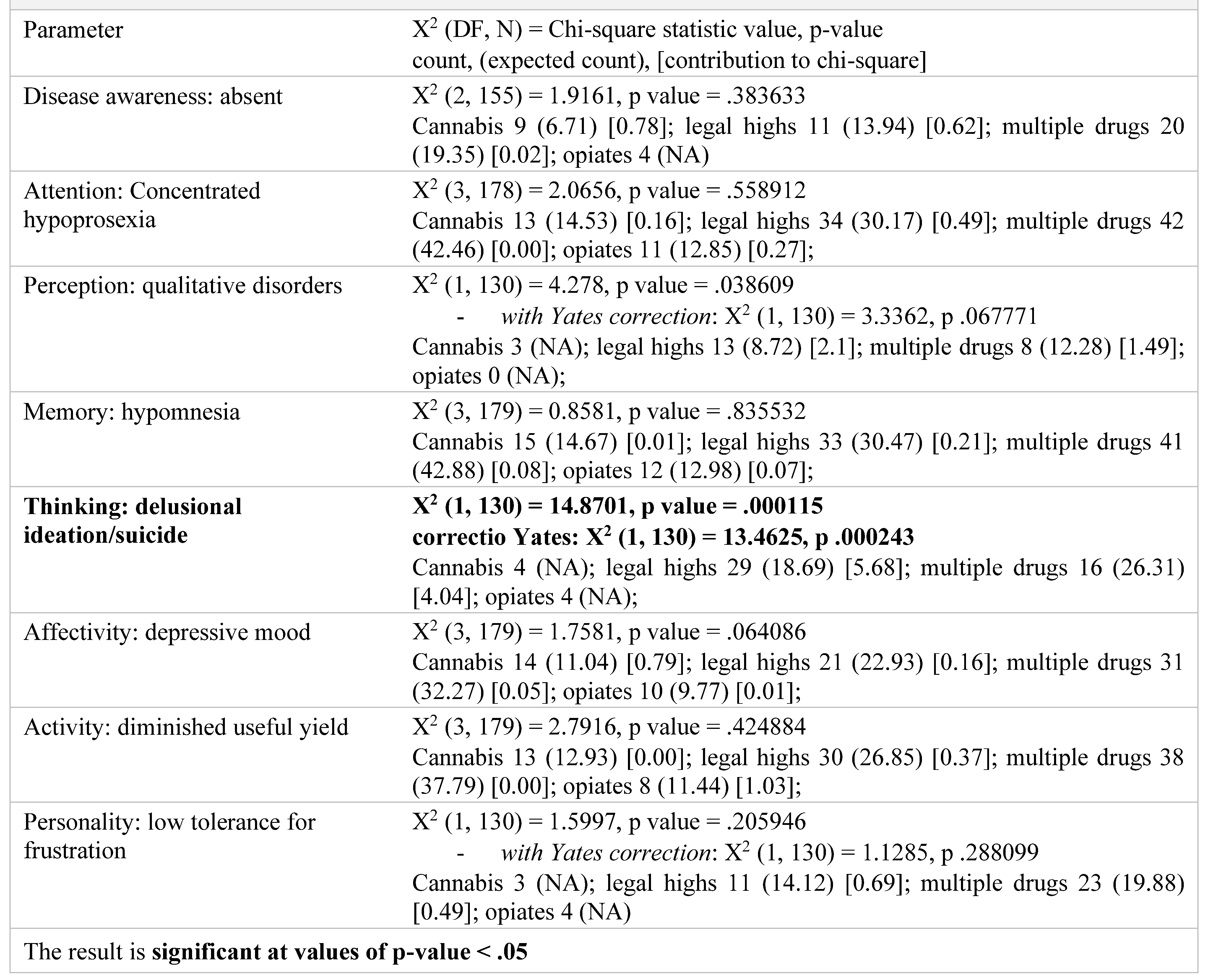
- Psychological examination
Group characteristics
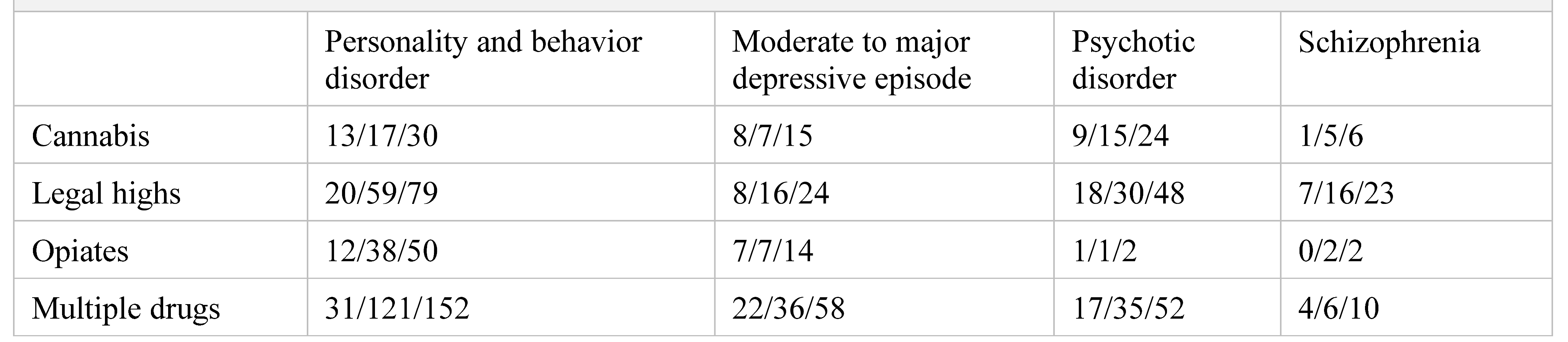
Diagnosis at admission
Assessment of mental state
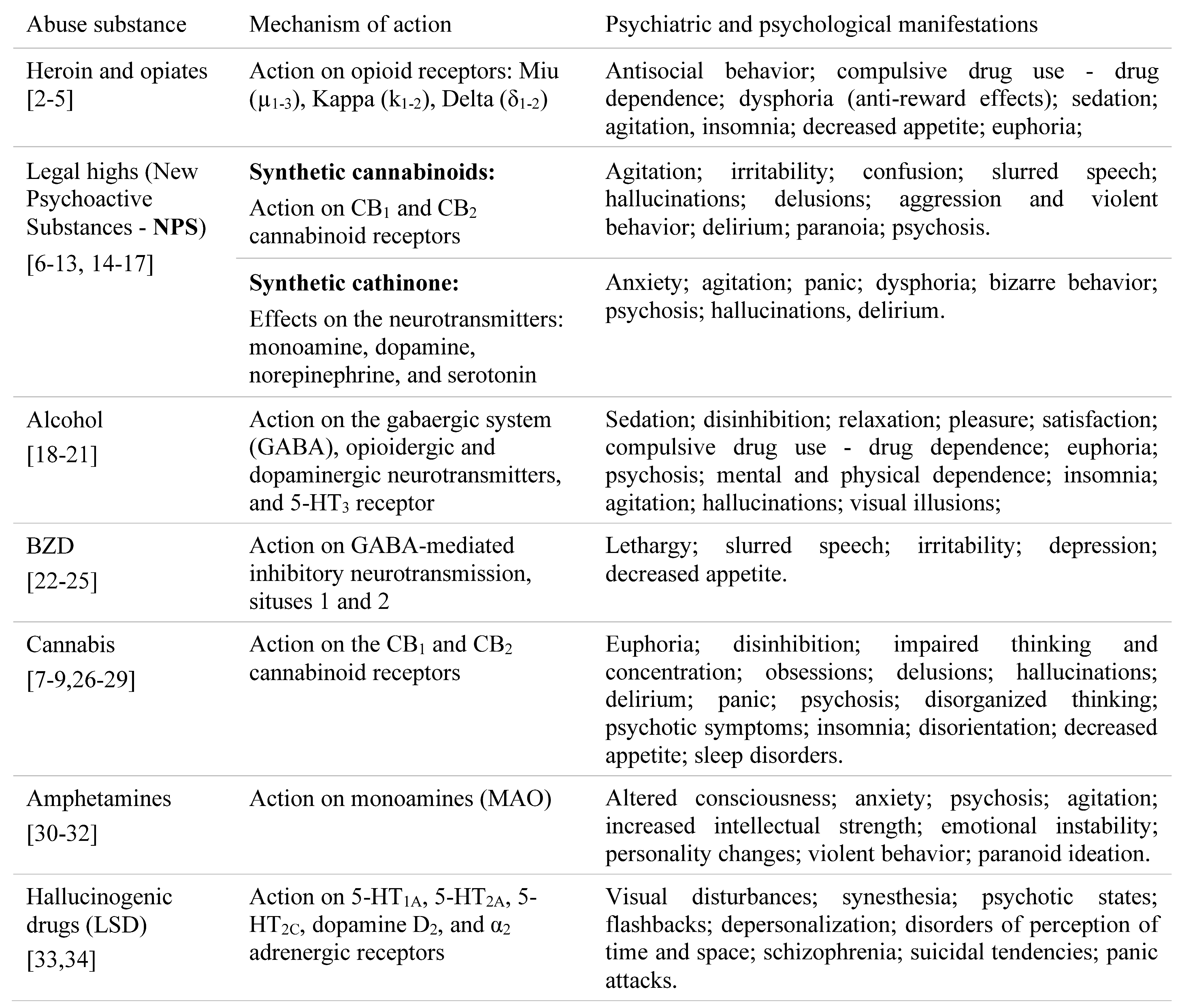
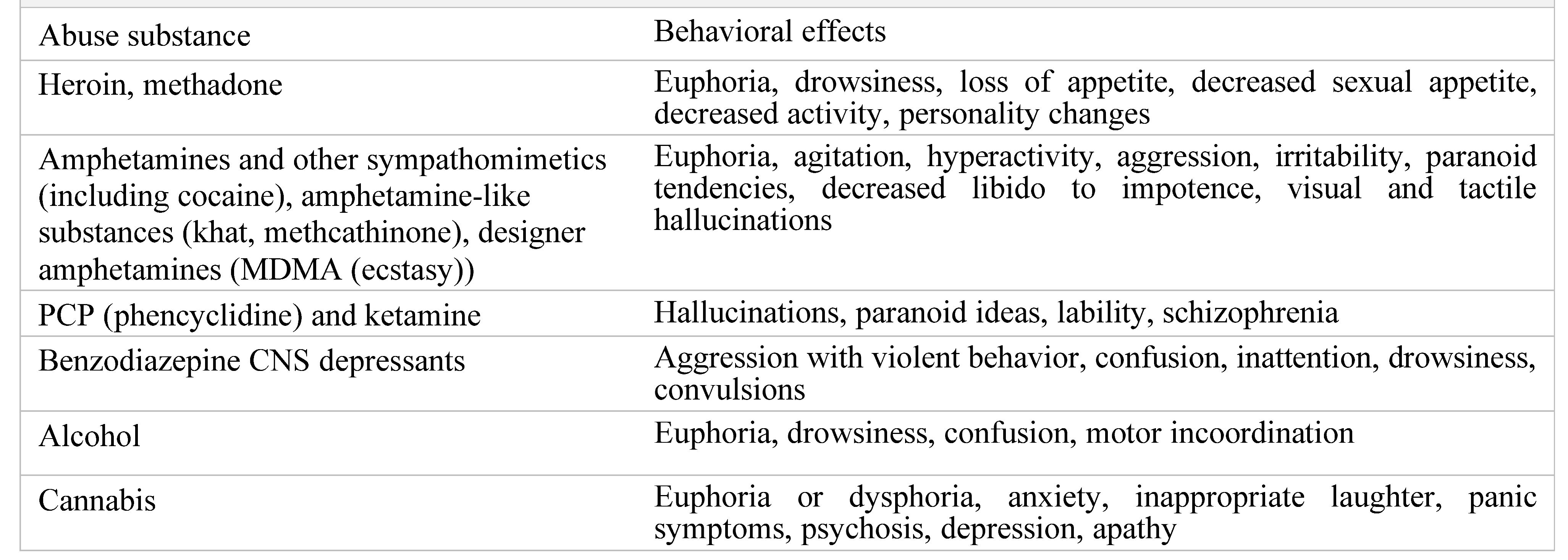
Discussion
Psychiatric examination
Psychological examinations
Conclusions
Limitations
- ✓
- A wide range of symptoms appears after substances of abuse intake because most drugs cause non-specific symptoms, especially in the psychiatric and psychological sphere.
- ✓
- Most the substances of abuse determine multiple changes in the consumers’ personalities.
- ✓
- The collaboration between pharmacists, chemists, and psychologists is essential in assessing a possible correlation between the changes in one’s personality and the specific chemical structures of different drugs.
Conflict of interest disclosure
Compliance with ethical standards
References
- United Nations Office on Drugs and Crime (UNODC). World Drug Report. New York: United Nations Publication; (2015). Sales No. E.15.XI. Available online: https://www.unodc.org/documents/wdr2015/World_D rug_Report_2015.pdf.
- Brown, R. Heroin dependence. WMJ. 2004, 103, 20–26. [Google Scholar] [PubMed]
- Hosztafi, S. A heroin addikció [Heroin addiction]. Acta Pharm Hung. 2011, 81, 173–183. [Google Scholar] [PubMed]
- Wang, S. Historical Review: Opiate Addiction and Opioid Receptors. Cell Transplant. 2019, 28, 233–238. [Google Scholar] [CrossRef]
- Baconi, D.; Bălălău, D.; Abraham, P. Abuzul și toxicodependența. Mecanisme, manifestări, tratament, legislație, Editura medicală, 2008.
- Gunderson, E.W.; Haughey, H.M.; Ait-Daoud, N.; Joshi, A.S.; Hart, C.L. "Spice" and "K2" herbal highs: a case series and systematic review of the clinical effects and biopsychosocial implications of synthetic cannabinoid use in humans. Am J Addict. 2012, 21, 320. [Google Scholar] [CrossRef]
- Ashton, J.C.; Friberg, D.; Darlington, C.L.; Smith, P.F. Expression of the cannabinoid CB2 receptor in the rat cerebellum: an immunohistochemical study. Neurosci Lett. 2006, 396, 113–116. [Google Scholar] [CrossRef] [PubMed]
- Pertwee, R.G. Receptors and channels targeted by synthetic cannabinoid receptor agonists and antagonists. Curr Med Chem. 2010, 17, 1360–1381. [Google Scholar] [CrossRef]
- Howlett, A.C.; Barth, F.; Bonner, T.I.; Cabral, G.; Casellas, P.; Devane, W.A.; Felder, C.C.; Herkenham, M.; Mackie, K.; Martin, B.R.; Mechoulam, R.; Pertwee, R.G. International Union of Pharmacology. XXVII. Classification of cannabinoid receptors. Pharmacol Rev. 2002, 54, 161–202. [Google Scholar] [CrossRef]
- Howlett, A.C.; Johnson, M.R.; Melvin, L.S.; Milne, G.M. Nonclassical cannabinoid analgetics inhibit adenylate cyclase: development of a cannabinoid receptor model. Mol Pharmacol. 1988, 33, 297–302. [Google Scholar] [PubMed]
- Weinstein, A.M.; Rosca, P.; Fattore, L.; London, E.D. Synthetic Cathinone and Cannabinoid Designer Drugs Pose a Major Risk for Public Health. Front Psychiatry. 2017, 8, 156. [Google Scholar] [CrossRef]
- Castaneto, M.S.; Gorelick, D.A.; Desrosiers, N.A.; Hartman, R.L.; Pirard, S.; Huestis, M.A. Synthetic cannabinoids: epidemiology, pharmacodynamics, and clinical implications. Drug Alcohol Depend. 2014, 144, 12–41. [Google Scholar] [CrossRef]
- Baumann, M.H.; Walters, H.M.; Niello, M.; Sitte, H.H. Neuropharmacology of Synthetic Cathinones. Handb Exp Pharmacol. 2018, 252, 113–142. [Google Scholar] [CrossRef]
- Reynaud, M.; Schwan, R.; Loiseaux-Meunier, M.N.; Albuisson, E.; Deteix, P. Patients admitted to emergency services for drunkenness: moderate alcohol users or harmful drinkers? Am J Psychiatry. 2001, 158, 96–99. [Google Scholar] [CrossRef] [PubMed]
- Chikritzhs, T.; Livingston, M. Alcohol and the Risk of Injury. Nutrients. 2021, 13, 2777. [Google Scholar] [CrossRef] [PubMed]
- Martel, M.L.; Klein, L.R.; Lichtenheld, A.J.; Kerandi, A.M.; Driver, B.E.; Cole, J.B. Etiologies of altered mental status in patients with presumed ethanol intoxication. Am J Emerg Med. 2018, 36, 1057–1059. [Google Scholar] [CrossRef]
- Costardi, J.V.; Nampo, R.A.; Silva, G.L.; Ribeiro, M.A.; Stella, H.J.; Stella, M.B.; Malheiros, S.V. A review on alcohol: from the central action mechanism to chemical dependency. Rev Assoc Med Bras (1992). 2015, 61, 381–387. [Google Scholar] [CrossRef] [PubMed]
- Pétursson, H. The benzodiazepine withdrawal syndrome. Addiction. 1994, 89, 1455–1459. [Google Scholar] [CrossRef]
- Nelson, J.; Chouinard, G. Guidelines for the clinical use of benzodiazepines: pharmacokinetics, dependency, rebound and withdrawal. Canadian Society for Clinical Pharmacology. Can J Clin Pharmacol. 1999, 6, 69–83. [Google Scholar]
- Howard, P.; Twycross, R.; Shuster, J.; Mihalyo, M.; Wilcock, A. Benzodiazepines. J Pain Symptom Manage. 2014, 47, 955–64. [Google Scholar] [CrossRef]
- Hasin, D. Long-term cannabis use and preparedness for ageing. Lancet Healthy Longev. 2022, 3, e645–e646. [Google Scholar] [CrossRef]
- Jett, J.; Stone, E.; Warren, G.; Cummings, K.M. Cannabis Use, Lung Cancer, and Related Issues. J Thorac Oncol. 2018, 13, 480–487. [Google Scholar] [CrossRef]
- Wøien, V.A.; Horwitz, H.; Høgberg, L.C.; Askaa, B.; Jürgens, G. Cannabismisbrug og dets konsekvenser [Cannabis--abuse and consequences]. Ugeskr Læger. 2015, 177, 241–245. Available online: https://ugeskriftet.dk/files/scientific_article_files/2015-01/artikel_13425.pdf.
- Mashhoon, Y.; Sagar, K.A.; Gruber, S.A. Cannabis Use and Consequences. Pediatr Clin North Am. 2019, 66, 1075–1086. [Google Scholar] [CrossRef] [PubMed]
- Iyalomhe, G.B. Cannabis abuse and addiction: a contemporary literature review. Niger J Med. 2009, 18, 128–133. [Google Scholar] [CrossRef] [PubMed]
- Heal, D.J.; Smith, S.L.; Gosden, J.; Nutt, D.J. Amphetamine, past and present--a pharmacological and clinical perspective. J Psychopharmacol. 2013, 27, 479–496. [Google Scholar] [CrossRef]
- Harro, J. Neuropsychiatric Adverse Effects of Amphetamine and Methamphetamine. Int Rev Neurobiol. 2015, 120, 179–204. [Google Scholar] [CrossRef]
- Steinkellner, T.; Freissmuth, M.; Sitte, H.H.; Montgomery, T. The ugly side of amphetamines: short-and long-term toxicity of 3,4-methylenedioxymethamphetamine (MDMA, 'Ecstasy'), methamphetamine and D-amphetamine. Biol Chem. 2011, 392, 103–115. [Google Scholar] [CrossRef]
- Nichols, D.E. Hallucinogens. Pharmacol Ther. 2004, 101, 131–181. [Google Scholar] [CrossRef]
- Liechti, M.E. Modern Clinical Research on LSD. Neuropsychopharmacology. 2017, 42, 2114–2127. [Google Scholar] [CrossRef]
- Adamowicz, P.; Gieroń, J. Acute intoxication of four individuals following use of the synthetic cannabinoid MAB-CHMINACA. Clin Toxicol (Phila). 2016, 54, 650–654. [Google Scholar] [CrossRef]
- Katz, K.D.; Leonetti, A.L.; Bailey, B.C.; Surmaitis, R.M.; Eustice, E.R.; Kacinko, S.; Wheatley, S.M. Case Series of Synthetic Cannabinoid Intoxication from One Toxicology Center. West J Emerg Med. 2016, 17, 290–294. [Google Scholar] [CrossRef]
- Armenian, P.; Darracq, M.; Gevorkyan, J.; Clark, S.; Kaye, B.; Brandehoff, N.P. Intoxication from the novel synthetic cannabinoids AB-PINACA and ADB-PINACA: A case series and review of the literature. Neuropharmacology. 2018, 134 Pt A, 82–91. [Google Scholar] [CrossRef]
- Hermanns-Clausen, M.; Müller, D.; Kithinji, J.; Angerer, V.; Franz, F.; Eyer, F.; Neurath, H.; Liebetrau, G.; Auwärter, V. Acute side effects after consumption of the new synthetic cannabinoids AB-CHMINACA and MDMB-CHMICA. Clin Toxicol (Phila). 2018, 56, 404–411. [Google Scholar] [CrossRef] [PubMed]
- Sadock, B.J.; Sadock, V.A. Kaplan & Sadock's comprehensive textbook of psychiatry (7th ed.). Lippincott Williams & Wilkins Publishers, (Eds.). (2000).
- Skelton, K.R.; Young-Wolff, K.C. Preconception cannabis use: An important but overlooked public health issue. Womens Health (Lond). 2022, 18, 17455057221124071. [Google Scholar] [CrossRef] [PubMed]
- Mititelu, M.; Hîncu, L.; Ozon, E.A.; Baconi, D.L.; Paunica, I.; Bălălău, O.D. Analysis of potentially toxic contaminants in milk powder. J Mind Med Sci. 2021, 8, 237–244. [Google Scholar] [CrossRef]
- Yazıcı, S.; Karabulut, M.; Baysal, A.; Zeybek, R. The effects of levosimendan on renal functions in open-heart surgery patients with a low ejection fraction. J Clin Investig Surg. 2021, 6, 121–130. [Google Scholar] [CrossRef]
- Georgescu, S.R.; Tampa, M.; Paunica, S.; Balalau, C.; Constantin, V.; Paunica, G.; Motofei, I. Distribution of post-finasteride syndrome in men with androgenic alopecia. ESDR-Congress 2015. Journal of Investigative Dermatology (Meeting Abstract 228); 2015, 135, S40. [Google Scholar]
- Motofei, I.G.; Rowland, D.L.; Baconi, D.L.; Georgescu, S.R.; Paunică, S.; Constantin, V.D.; Bălălău, D.; Paunică, I.; Bălălău, C.; Baston, C.; Sinescu, I. Therapeutic considerations related to finasteride administration in male androgenic alopecia and benign prostatic hyperplasia. Farmacia. 2017, 65, 660–666. [Google Scholar]
- Velikova, M.; Galunska, B.; Dimitrova, R.; Stoyanov, Z. Alcohol consumption and cognitive aging: can it be beneficial? J Mind Med Sci. 2021, 8, 5–16. [Google Scholar] [CrossRef]
- Bălălău, C.; Voiculescu, Ș.; Motofei, I.; Scăunașu, R.V.; Negrei, C. Low dose tamoxifen as treatment of benign breast proliferative lesions. Farmacia. 2015, 63, 371–375. [Google Scholar]
- Inanc, I.H.; Polat, E.; Coskun, F.Y. One-year clinical follow-up and outcomes in patients after drug-eluting stent implantation for unprotected left main coronary stenosis: A single center study from Turkey. J Clin Investig Surg. 2020, 5, 43–50. [Google Scholar] [CrossRef]
- Ardeleanu, V.; Andronache, L.F.; Gherghiceanu, F.; Paunica, S.; Balalau, C.; Pantea Stoian, A. Treatment of lipomas and diffuse lipomatosis with NDYAG 1064 NM laser and their impact on the quality of life. J Mind Med Sci. 2020, 7, 16–22. [Google Scholar] [CrossRef]
- John, S. Does In-Hospital Depressed Level of Consciousness Impact Outcomes in Critically Ill Patients? Crit Care Med. 2022, 50, 1681–1682. [Google Scholar] [CrossRef]
- Yi, L.; Li, T. Effective Strategies to Promote the Cultivation of Public Legal Consciousness from the Perspective of Social Psychology. J Environ Public Health. 2022, 2022, 8275938. [Google Scholar] [CrossRef]
- Michel, M. Confidence in consciousness research. Wiley Interdiscip Rev Cogn Sci. 2022, e1628. [Google Scholar] [CrossRef] [PubMed]
- Bacinschi, N.; Pogonea, I.; Podgurschi, L.; Mihalachi-Anghel, M.; Ștefănescu, E.; Socea, B.; Chianu, M. The role of biotransformation processes in mediating interactions between psychotropic drugs and natural products. J Mind Med Sci. 2020, 7, 9–15. [Google Scholar] [CrossRef]
- Koculak, M.; Wierzchoń, M. How much consciousness is there in complexity? Front Psychol. 2022, 13, 983315. [Google Scholar] [CrossRef]
- Motofei, I.G.; Rowland, D.L.; Popa, F.; Bratucu, E.; Straja, D.; Manea, M.; Georgescu, S.R.; Paunica, S.; Bratucu, M.; Balalau, C.; Constantin, V.D. A Pilot Study on Tamoxifen Sexual Side Effects and Hand Preference in Male Breast Cancer. Arch Sex Behav. 2015, 44, 1589–1594. [Google Scholar] [CrossRef]
- Elboukhani, I.; Essadouni, C.; Mchachi, A.; Benhmidoune, L.; Chakib, A.; Rachid, R.; Elbelhadji, M. Topical anesthesia versus peribulbar anesthesia in phacoemulsification cataract surgery and intraocular lens implantation. J Clin Investig Surg 2020, 5, 100–103. [Google Scholar] [CrossRef]
- Adineh, M.; Elahi, N.; Molavynejad, S.; Jahani, S.; Savaie, M. Impact of a sensory stimulation program conducted by family members on the consciousness and pain levels of ICU patients: A mixed method study. Front Med (Lausanne). 2022, 9, 931304. [Google Scholar] [CrossRef]
- Mortaheb, S.; Van Calster, L.; Raimondo, F.; Klados, M.A.; Boulakis, P.A.; Georgoula, K.; Majerus, S.; Van De Ville, D.; Demertzi, A. Mind blanking is a distinct mental state linked to a recurrent brain profile of globally positive connectivity during ongoing mentation. Proc Natl Acad Sci U S A. 2022, 119, e2200511119. [Google Scholar] [CrossRef] [PubMed]
- Colman, W. Thinking the unthinkable: trauma, defence and early states of mind in the work of Alessandra Cavalli. J Anal Psychol. 2022, 67, 919–938. [Google Scholar] [CrossRef]
- Preiss, D.D. Metacognition, Mind Wandering, and Cognitive Flexibility: Understanding Creativity. J Intell. 2022, 10, 69. [Google Scholar] [CrossRef]
- De Calheiros Velozo, J.; Lafit, G.; Viechtbauer, W.; van Amelsvoort, T.; Schruers, K.; Marcelis, M.; et al. Delayed affective recovery to daily-life stressors signals a risk for depression. J Affect Disord, 2022; S0165-0327(22)01149-1. [Google Scholar] [CrossRef]
- Schoeller, F.; Perlovsky, L.; Arseniev, D. Physics of mind: Experimental confirmations of theoretical predictions. Phys Life Rev. 2018, 25, 45–68. [Google Scholar] [CrossRef] [PubMed]
- Aliuș, C.; Bacalbașa, N.; Bălălău, C. Innovative Device for Indocianyne Green Navigational Surgery. J Mind Med Sci. 2020, 7, 40–45. [Google Scholar] [CrossRef]
- Custal, M.; Torguet, P.; Vallés, M.; Bronsoms, J.; Maté, G.; Mauri, J. Nefropatía, ritmo nictemeral y presión de pulso en la diabetes mellitus tipo 2 [Nephropathy, nycthemeral variability and pulse pressure in patients with type 2 diabetes mellitus]. Med Clin (Barc). 2001, 116, 454–456. [Google Scholar] [CrossRef]
- Wallis, D.; Coatsworth, J.D.; Mennis, J.; Riggs, N.R.; Zaharakis, N.; Russell, M.A.; Brown, A.R.; Rayburn, S.; Radford, A.; Hale, C.; Mason, M.J. Predicting Self-Medication with Cannabis in Young Adults with Hazardous Cannabis Use. Int J Environ Res Public Health. 2022, 19, 1850. [Google Scholar] [CrossRef]
- Micu, S.I.; Musat, M.; Dumitru, A.; Paduraru, D.N.; Rogoveanu, A.; Dumitriu, A.S.; Paunica, S.; Balalau, C.; Popoiag, R.E. Hepatitis C virus: host, environmental and viral factors promoting spontaneous clearance. J Mind Med Sci. 2020, 7, 156–161. [Google Scholar] [CrossRef]
- Ismail, Z.; Gatchel, J.; Bateman, D.R.; Barcelos-Ferreira, R.; Cantillon, M.; Jaeger, J.; Donovan, N.J.; Mortby, M.E. Affective and emotional dysregulation as pre-dementia risk markers: exploring the mild behavioral impairment symptoms of depression, anxiety, irritability, and euphoria. Int Psychogeriatr. 2018, 30, 185–196. [Google Scholar] [CrossRef]
- Chen, X.; Mo, Q.; Yu, B.; Bai, X.; Jia, C.; Zhou, L.; Ma, Z. Hierarchical and nested associations of suicide with marriage, social support, quality of life, and depression among the elderly in rural China: Machine learning of psychological autopsy data. Front Psychiatry. 2022, 13, 1000026. [Google Scholar] [CrossRef]
- Joseph, V.A.; Martínez-Alés, G.; Olfson, M.; Shaman, J.; Gould, M.S.; Keyes, K.M. Temporal Trends in Suicide Methods Among Adolescents in the US. JAMA Netw Open. 2022, 5, e2236049. [Google Scholar] [CrossRef]
- Meteliuk, A.; Galvez, S.; Fomenko, T.; et al. Successful transfer of stable patients on opioid agonist therapies from specialty addiction treatment to primary care settings in Ukraine: A pilot study. J Subst Abuse Treat. 2022, 134, 108619. [Google Scholar] [CrossRef] [PubMed]
- Brunette, M.F.; Mueser, K.T.; Babbin, S.; Meyer-Kalos, P.; Rosenheck, R.; Correll, C.U.; Cather, C.; Robinson, D.G.; Schooler, N.R.; Penn, D.L.; Addington, J.; Estroff, S.E.; Gottlieb, J.; Glynn, S.M.; Marcy, P.; Robinson, J.; Kane, J.M. Demographic and clinical correlates of substance use disorders in first episode psychosis. Schizophr Res. 2018, 194, 4–12. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Bagge, C.L.; Schumacher, J.A.; Coffey, S.F. Does comorbid substance use disorder exacerbate borderline personality features? A comparison of borderline personality disorder individuals with vs. without current substance dependence. Personal Disord. 2010, 1, 239–249. [Google Scholar] [CrossRef] [PubMed]
 |
 |
 |
 |
 |
 |
 |
 |
© 2022 by the author. 2022 Daniela-Mădălina Ciucă Anghel, Elena-Elisabeta Anghe, Miriana Stan, Gheorghe Tudor, Anca Silvia Dumitriu, Stana Paunica, Daniela Luiza Baconi
Share and Cite
Ciucă Anghel, D.-M.; Anghel, E.-E.; Stan, M.; Tudor, G.; Dumitriu, A.S.; Paunica, S.; Baconi, D.L. Psychological and Psychiatric Characterization of Various Groups of Drugs Users. J. Mind Med. Sci. 2022, 9, 255-265. https://doi.org/10.22543/2392-7674.1356
Ciucă Anghel D-M, Anghel E-E, Stan M, Tudor G, Dumitriu AS, Paunica S, Baconi DL. Psychological and Psychiatric Characterization of Various Groups of Drugs Users. Journal of Mind and Medical Sciences. 2022; 9(2):255-265. https://doi.org/10.22543/2392-7674.1356
Chicago/Turabian StyleCiucă Anghel, Daniela-Mădălina, Elena-Elisabeta Anghel, Miriana Stan, Gheorghe Tudor, Anca Silvia Dumitriu, Stana Paunica, and Daniela Luiza Baconi. 2022. "Psychological and Psychiatric Characterization of Various Groups of Drugs Users" Journal of Mind and Medical Sciences 9, no. 2: 255-265. https://doi.org/10.22543/2392-7674.1356
APA StyleCiucă Anghel, D.-M., Anghel, E.-E., Stan, M., Tudor, G., Dumitriu, A. S., Paunica, S., & Baconi, D. L. (2022). Psychological and Psychiatric Characterization of Various Groups of Drugs Users. Journal of Mind and Medical Sciences, 9(2), 255-265. https://doi.org/10.22543/2392-7674.1356



