Abstract
Premenstrual syndrome (PMS) is a clinical entity of concern in women of reproductive age group with its onset during the late luteal phase of the menstrual cycle that typically resolves within a few days after the onset of menstruation. Female reproductive hormones stimulate the gene promotor region of Gonadal steroids, which are modulators of the hypothalamic-pituitary axis, in association with the autonomic nervous system (ANS), form the stress system, which regulates the homeostatic mechanisms of the body. Disruption of this mechanism can lead to sympathovagal imbalance and cognitive deficits. Objectives: This study was aimed to compare the autonomic functions and cognition between PMS and control group. Methodology: This cross-sectional study was conducted as a pilot study with 20 subjects in each group. Autonomic function test and P300 were recorded. Study participants were also asked to answer Montreal cognitive assessment (MOCA) questionnaire. Results: On comparison of the test results between the two groups, individuals in PMS group were found to have increased sympathetic activity and reduced cognition when compared to the no PMS (control) group. Conclusion: The findings from this study proves a detrimental effect of gonadal steroids on autonomic nervous system and cognition.
Introduction
Premenstrual syndrome (PMS) is a clinical entity consisting of physical, behavioral, cognitive, and affective symptoms, with its onset during the late luteal phase of the menstrual cycle that typically resolves within a few days after the onset of menstruation [1]. Worldwide, around 90 % of women during the reproductive age suffer from PMS. The most common symptoms include headache, fatigue, bloating, breast tenderness, nausea, altered sleep pattern, mood swings, anxiety, and irritability [1]. In most women, these symptoms are self-limiting, with about 15% suffering moderate to severe symptoms which impair their routine activities [2]. Gonadal steroids, which are modulators of the hypothalamic-pituitary axis, in association with the autonomic nervous system (ANS), form the stress system, which regulates the homeostatic mechanisms of the body. Disruption of this mechanism can lead to sympathovagal imbalance and cognitive deficits [3,4]. The follicular phase of menstrual cycle is parasympathetic dominant and the luteal phase is sympathetic predominant [5,6], as the result of ovarian steroids affecting the hypothalamic-pituitary axis (HPA). These hormones also stimulate the gene promotor region of Corticotrophin Releasing Hormone (CRH) and the central noradrenergic system, thereby leading to sympathetic predominance in the premenstrual phase [5,6]. De Zambotti et. al in 2013 implicated the role of high progesterone levels during the late luteal phase of menstrual cycle to sympathovagal imbalance [7].
Sympathovagal imbalance is an important predictor of cardiovascular risk. Decreased vagal tone is deleterious for cardiovascular functions and increases the risk of cardiovascular diseases [8]. Conventional autonomic function test (CAFT) [9], power spectral analysis of heart rate variability (HRV) [10], and baroreflex sensitivity analysis by continuous blood pressure variability as recorded by Finapres [11], have been documented as sensitive measures of sympathovagal balance. Hence, in our current study we have used these measures as a tool to determine the sympathovagal balance.
In addition to sympathovagal imbalance, women with PMS often report various psychological symptoms [1], which include mood instability, depression, and lack of concentration. The etiopathogenesis of psychological symptoms is the increased sensitivity of the central nervous system to the cyclical fluctuations in sex hormones. Estrogen and progesterone receptors, being extensively present in the hypothalamus, are also found in other brain areas like the amygdala, hippocampus, and prefrontal cortex, areas involved in cognition. Estrogen and progesterone are lipophilic hormones and thus can cross the blood brain barrier and act upon these receptors [12]. Morgan et al., in 1996, showed significant impairment of cognition in individuals with PMS during the luteal phase of menstrual cycle [13]. In contrast to this finding, various studies have yielded inconsistent results in demonstrating an association of cognitive impairment and PMS [12]. In order to address these inconsistent findings, the current study also evaluated cognition by P300 of event related potentials (ERP) along with the Montreal cognitive assessment (MOCA) questionnaire. ERP are the brain evoked responses for evaluation of cognitive function [14,15]. There is also a paucity of literature associating cognitive function and cardiac autonomic function parameters in these women. Therefore, in the current study we have assessed the link between autonomic function test parameters with cognitive function. We hypothesized that women with PMS would have sympathetic overactivity and impaired cognition compared to those without PMS, and the reduced cognition might be associated with sympathovagal imbalance.
Materials and Methods
This cross-sectional study was conducted as a pilot analysis with 20 subjects in each group. The study was approved by scientific committee and ethics committee of the institute.
- Inclusion criteria:
Study Group (PMS group):
Women of 18 to 45 years old having regular 21-to-35- day menstrual cycles of 3 to 7 days duration [2], for at least 6 consecutive months, with normal body mass index (BMI), and diagnosed as moderate-to-severe PMS by the Premenstrual Syndrome Screening Tool (PSST) [16].
Control Group (Non-PMS Group):
Healthy women 18 to 45 years old having regular 21 to 35 days menstrual cycles of 3 to 7 days duration for at least 6 consecutive months, with normal BMI and having no PMS as inferred by the Premenstrual Syndrome Screening Tool (PSST).
- Exclusion criteria:
Both PMS and non-PMS group:
- omen diagnosed as Premenstrual Dysphoric Disorder (PMDD) by PSST questionnaire
- omen with irregular menstrual cycle
- Usage of Oral contraceptive pills
- History of:
- -
- Depression and/or other psychological disorders
- -
- Hypertension
- -
- Endocrine and metabolic disorders
- -
- Smoking, alcoholism
- On medications that affect autonomic nervous system and cognition.
Individuals who met the inclusion criteria were recruited into the study. After obtaining written informed consent from participants, age, height (cm) by stadiometer (BHH6, Easy Care, Mumbai, India), body weight measured with minimal clothing by digital weighing machine (MS 4900, Charder Electronics Co. Ltd, Taichung, Taiwan) were measured. BMI was calculated by ‘Quetelet’s index’ (BMI = weight (Kg)/height2 (m)2).
All individuals completed the PSST questionnaire and those who fulfilled the criteria for PMS were included in PMS group and others in non-PMS group. A brief menstrual history was obtained and participants were asked to report to the Department of Physiology in the late luteal phase of their menstrual cycle (5 to 7 days before the onset of regular menses), at around 10.00 am, 1 hour after a light breakfast. Subjects were asked to avoid caffeine intake at least 12 hours before recording. Basic demographic details such as education status, occupation, and so on, were obtained.
- AFT and HRV Recordings
The subject was asked to lie in a supine position and after 5 minutes of rest, lead II ECG was connected. Heart rate variability, complete battery of cardiac autonomic function tests which includes, lying-to-standing ratio (30:15 ratio), deep breathing ratio (E:I ratio), and diastolic blood pressure response to isometric hand grip test were recorded using BIOPAC MP100 data acquisition system (BIOPAC Inc., USA). Using the R-wave detector in the Acknowledge software, the R-R tachogram was extracted and the values were computed. HRV was analyzed using HRV analysis software (Version 2.0., Biosignal analysis group, University of Kuopio, Finland).
- BRS recording
BRS was recorded by Finapres (Finometer version 1.22a, Finapres Medical Systems, Amsterdam, The Netherlands). This is a non-invasive continuous blood pressure variability measurement method based on the principle of measurement of finger arterial pressure with the volume clamp technique of Penaz and the Physical criteria of Wesseling. In this technique, a brachial cuff and finger cuff are attached to the patient and the brachial artery pressure was measured by reconstructing the finger arterial pressure estimated through generalized waveform inverse modelling and generalized level correction [17].
- P300 recording
P300 was recorded using Nihon Khoden EP/EMG machine for the recording and Neuro pack software for analysis. P300 was recorded in the context of a standard auditory oddball paradigm. The evoked responses were picked up from scalp by placing reference electrode and ground electrode on both mastoids and recording electrode at Cz (Vertex). The P300 is a positive deflection, elicited in response to an Oddball paradigm, where the subject identifies the occasional stimuli (target stimuli). The peak latency of this wave in a healthy adult is 300ms and the latency varies with the accuracy in discriminating the target stimuli. The P300 wave of normal latency denotes that the subject is actively engaged in the task of detecting the targets. The latency in prolonged in individuals with poor cognition [18].
- MOCA
Subjects completed the Montreal Cognitive Assessment (MOCA) for cognitive testing. This questionnaire is scored for a total of 30. Cognitive functioning is tested by assessing visuospatial, naming, memory, attention, language, abstraction, delayed recall, and orientation components.
Results

Table 1.
Comparison of age, anthropometric parameters and basal blood pressure between PMS and non-PMS groups.
Table 1.
Comparison of age, anthropometric parameters and basal blood pressure between PMS and non-PMS groups.
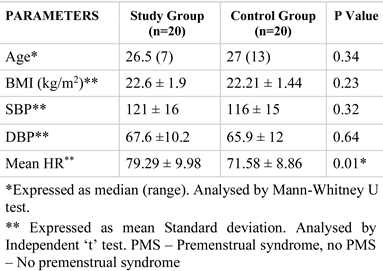

Table 2.
Comparison of heart rate variability, autonomic function test and baroreflex sensitivity parameters between PMS and non-PMS groups.
Table 2.
Comparison of heart rate variability, autonomic function test and baroreflex sensitivity parameters between PMS and non-PMS groups.
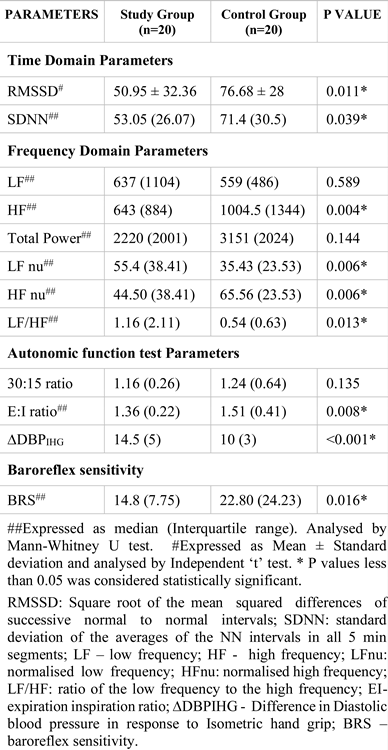

Table 3.
Comparison of cognitive parameters between PMS and non-PMS groups.
Table 3.
Comparison of cognitive parameters between PMS and non-PMS groups.
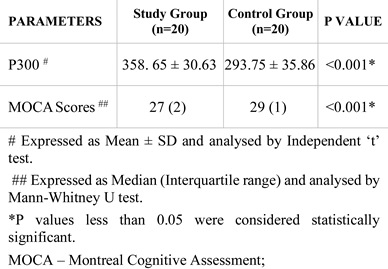

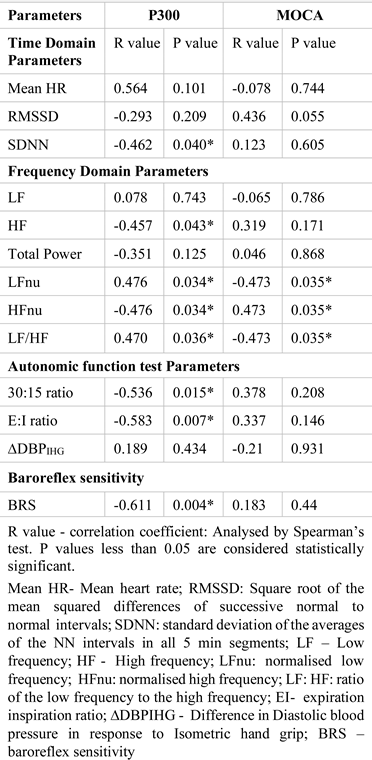
Table 4.
Correlation of P300 with heart rate variability, autonomic function test and baroreflex sensitivity in PMS group.
Table 4.
Correlation of P300 with heart rate variability, autonomic function test and baroreflex sensitivity in PMS group.
Discussion
In this study we compared the cognitive functioning and cardiac autonomic function between women with and without PMS. Since BMI and blood pressure are known to affect the autonomic function and cognition [19,20], these parameters were matched between the groups. Mean heart rate was found to be significantly increased in the PMS group. Resting heart rate is determined mainly by the parasympathetic action on the heart [21], indicating that women in PMS group have parasympathetic withdrawal.
Among the time domain parameters of HRV, RMSSD and SDNN are the most sensitive in short-term recording of HRV [22]. In our study, RMSSD and SDNN were found to be significantly reduced in the PMS group (Table 2).
RMSSD is one of the most sensitive parameters of parasympathetic tone in short-term recording of HRV, which denotes a decreased cardiac vagal tone over the heart [22]. Among the frequency domain parameters, HF and HFnu, the markers of parasympathetic activity, were significantly reduced; and LFnu, the marker of sympathetic activity, was significantly increased in the PMS group when compared to the control group (Table 2). LF:HF ratio that indicate sympathovagal imbalance [22,23] were also found to be significantly increased in PMS group. These findings suggest that in subjects with PMS, there is a sympathovagal imbalance with increased cardiac sympathetic drive and decreased parasympathetic drive. In comparing the cardiac autonomic functions between the two groups, E:I ratio, the measure of parasympathetic tone [24], was significantly reduced and the change in diastolic blood pressure in response to isometric hand grip (DBP IHG), which is a measure of sympathetic reactivity [24], was significantly increased in the PMS group. Thus, HRV was found to be decreased considerably and there is sympathovagal imbalance with sympathetic overactivity in the PMS group, indicating an increased risk of cardiovascular disease when compared with women without PMS.
The findings of the current study are consistent with a previous study reporting exaggerated sympathetic activity in PMS [3,24]. Sympathovagal balance can also be assessed by measuring baroreflex sensitivity (BRS). Increased BRS suggests predominant parasympathetic activity and vice versa. A study by Koifman et. al. showed reduced BRS during the late luteal phase in individuals with PMS [3]. The findings from our study are consistent with this study in that they show significantly reduced BRS in the PMS group, supporting the association of increased sympathetic activity with PMS.
PMS was also reported to be a risk factor for the development of hypertension for women in their early 40s. A recent study had also reported a 3-fold increased risk of hypertension in individuals with PMS [25,26]. Existence of sympathovagal imbalance in individuals with PMS during the late luteal phase of menstrual cycle can be attributed to the effect of gonadal hormones on ANS. Elevated and abnormal fluctuations of gonadal hormones, along with hyper-reactiveness of various systemic organs to gonadal hormones, is the key pathogenic mechanism in PMS [25,27]. Thus, the findings from the current study provide evidence that individuals with PMS have sympathovagal imbalance that, in turn, leads to long-term cardiovascular morbidity.
Regarding comparison of the cognitive parameters, P300, and MOCA between the study and control groups, cognition was significantly reduced (i.e., P300 latency is prolonged and MOCA scores are reduced) in PMS group (Table 3). This suggests an inhibitory effect of progesterone on cognition. Progesterone is shown to have inhibitory effects on most neuronal activity and it also responsible for negative psychological effects such as depression, anxiety, and mood swings in PMS [27]. Keenan et al. reported reduced learning ability in women with PMS when compared to the control group [28], but there are also studies showing opposite effects between cognition and PMS [13]. Though past studies show varied results in regard to cognition in PMS, our study yielded a highly significant result of p <0.001, supporting the idea of a neuro-inhibitory effect of progesterone. In addition to the highly significant P300 results, significant reduction in MOCA scores were found, further evidence for a decline in cognition among PMS women.
Correlations of P300 with HRV parameters, cardiac autonomic function test, and BRS parameters were significant in the PMS group (Table 4) where Mean RR, SDNN, HF, HF nu (30:15), E:I ratio, and BRS were found to have significant negative correlations with P300 latency. LF/HF ratio and LF nu were found to be significantly and positively correlated with P300. RMSSD and HF nu were found to have significant positive correlations with MOCA scores and LFnu and LF/HF ratio were found to have significant negative correlations with MOCA scores. There was no significant correlation between the cardiac autonomic function parameters and P300 or MOCA in the control group. These patterns support the idea that the sympathetic predominance in the PMS group may be related to impaired cognition, and is consistent with previous studies reporting a positive effect of parasympathetic nervous system on cognitive function and negative cognitive effect of sympathetic nervous system [29,30,31]. The findings from this study suggest a detrimental effect of gonadal steroids on autonomic nervous system and cognition. In PMS, the negative effects of gonadal hormones on cognition and neuropsychiatric symptoms like depression and anxiety may also add to cardiovascular risk, beyond the sympathovagal imbalance.
Limitations. Sample size was small. This was a nonfunded project. Hence the serum levels of sex steroids could not be done to strengthen the association between the study parameters.
Conclusions
We conclude that sympathovagal imbalance and impaired cognition exist in women with premenstrual syndrome. PMS, being one of the common disorders of women in reproductive age group, can lead to long term cardiovascular and neurological morbidity reducing the quality of life in women. Thus, living in a society where women’s reproductive health is given least importance, premenstrual syndrome has to be effectively addressed to alleviate symptoms, improve the quality of life, and to prevent the development of cardiovascular morbidities.
Conflict of interest disclosure
There are no known conflicts of interest in the publication of this article. The manuscript was read and approved by all authors.
Compliance with ethical standards
Any aspect of the work covered in this manuscript has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript.
Acknowledgments
We greatly acknowledge JIPMER, Puducherry for the resources used in this project.
References
- Zaka, M.; Mahmood, K.T. Pre-menstrual Syndrome- A review. J Pharm Sci & Res. 2012, 4, 1684–1691. [Google Scholar]
- Hoffman, B.L.; Schorge, J.O.; Bradshaw, K.D.; Halvorson, L.M.; Schaffer, J.I.; Corton, M.M. Williams’ Gynecology, 3rd ed.; The McGraw-Hill: 2016; ISBN-10: 9780071849081.
- Koifman, R.; Dayan, L.; Ablin, J.N.; Jacob, G. Cardiovascular Autonomic Profile in Women With Premenstrual Syndrome. Front. Physiol. 2018, 9, 9. [Google Scholar] [CrossRef]
- Agarwal, G.; Kumar, R.; Kumar, J.; Bijaraniya, K. Study of Sympathetic Function Tests during Different Phases of Men-strual Cycle. Sch J App Med Sci. 2015, 3, 1462–1466. [Google Scholar]
- Nilekar, A.; Vatve, M.S. Autonomic function in pre and post menstrual phases in young women. Pravara Med Rev. 2013, 5, 8–10. [Google Scholar]
- Nilekar, A.N.; Patil, V.V.; Kulkarni, S.; Vatve, M. Autonomic function tests during pre and post menstrual phases in young women. Pravara Med Rev. 2011, 3, 24–30. [Google Scholar]
- de Zambotti, M.; Nicholas, C.L.; Colrain, I.M.; Trinder, J.A.; Baker, F.C. Autonomic regulation across phases of the menstrual cycle and sleep stages in women with premenstrual syndrome and healthy controls. Psychoneuroendocrinology 2013, 38, 2618–2627. [Google Scholar] [CrossRef]
- Hadley, D.M.; Dewey, F.E.; Freeman, J.V.; Myers, J.N.; Froelicher, V.F. Prediction of Cardiovascular Death using a Novel Heart Rate Recovery Parameter. Med. Sci. Sports Exerc. 2008, 40, 1072–1079. [Google Scholar] [CrossRef]
- Pal, G.K.; Pal, P. Textbook of Practical Physiology, 3rd Ed., Universities Press; 2010. Chapter 41, Spectral analysis of Heart Rate Variability; pp. 291–297, ISBN- 13: 978-8173716713.
- Malliani, A. Heart rate variability: from bench to bedside. Eur. J. Intern. Med. 2005, 16, 12–20. [Google Scholar] [CrossRef]
- Parati, G.; Ochoa, J.E.; Lombardi, C.; Salvi, P.; Bilo, G. Assessment and interpretation of blood pressure variability in a clinical setting. Blood Press. 2013, 22, 345–354. [Google Scholar] [CrossRef]
- Le, J.; Thomas, N.; Gurvich, C. Cognition, The Menstrual Cycle, and Premenstrual Disorders: A Review. Brain Sci. 2020, 10, 198. [Google Scholar] [CrossRef]
- Morgan, M.; Rapkin, A.J.; D'Elia, L.; Reading, A.; Goldman, L. Cognitive functioning in premenstrual syndrome. Obstet. Gynecol. 1999, 88, 961–966. [Google Scholar] [CrossRef]
- Zhong, R.; Li, M.; Chen, Q.; Li, J.; Li, G.; Lin, W. The P300 Event-Related Potential Component and Cognitive Impairment in Epilepsy: A Systematic Review and Meta-analysis. Front. Neurol. 2019, 10, 943. [Google Scholar] [CrossRef]
- Rose, A.F.; Gilbertson, A.F.; Cottrell, C.; Tampi, R.R. Cognitive screening for adult psychiatric outpatients: Comparison of the Cognivue® to the Montreal Cognitive Assessment. World J. Psychiatry 2021, 11, 265–270. [Google Scholar] [CrossRef]
- Steiner, M.; Macdougall, M.; Brown, E. The premenstrual symptoms screening tool (PSST) for clinicians. Arch. Women's Ment. Heal. 2003, 6, 203–209. [Google Scholar] [CrossRef]
- Imholz, B.P.; Wieling, W.; van Montfrans, G.A.; Wesseling, K.H. Fifteen years experience with finger arterial pressure monitoring: assessment of the technology. Cardiovasc. Res. 1998, 38, 605–616. [Google Scholar] [CrossRef]
- Picton, T.W. The P300 Wave of the Human Event-Related Potential. J. Clin. Neurophysiol. 1992, 9, 456–479. [Google Scholar] [CrossRef]
- Pal, G.; Dutta, T.; Indumathy, J.; Pal, P. Assessment of heart rate variability indices in overweight and obese Indian population. Int. J. Clin. Exp. Physiol. 2014, 1, 192. [Google Scholar] [CrossRef]
- Veronese, N.; Facchini, S.; Stubbs, B.; Luchini, C.; Solmi, M.; Manzato, E.; Sergi, G.; Maggi, S.; Cosco, T.; Fontana, L. Weight loss is associated with improvements in cognitive function among overweight and obese people: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2017, 72, 87–94. [Google Scholar] [CrossRef]
- Subhashri, S.; Pal, P.; Pal, G.K.; Papa, D.; Nanda, N. Decreased baroreflex sensitivity is associated with cardiometabolic risks and prehypertension status in early-postmenopausal women. Clin. Exp. Hypertens. 2020, 43, 112–119. [Google Scholar] [CrossRef]
- Subhashri, S.; Pal, P.; Papa, D.; Nanda, N.; Pal, G.K.; Packirisamy, R.M. Assessment of Heart Rate Variability in Early Post-menopausal Women. Int. J. Clin. Exp. Physiol. 2019, 6, 11–14. [Google Scholar] [CrossRef]
- Ribeiro, T.; Azevedo, G.; Crescêncio, J.; Marães, V.; Papa, V.; Catai, A.; Verzola, R.; Oliveira, L.; de Sá, M.S.; Jr. , L.G.; et al. Heart rate variability under resting conditions in postmenopausal and young women. Braz. J. Med Biol. Res. 2001, 34, 871–877. [Google Scholar] [CrossRef]
- Popovici, I.-E.; Cozma, A.; Orasan, O.; Ciulei, G.; Poenar, A.; Buchman, C.; Tarmure, S.; Secara, S.; Sitar-Taut, A.; Alexescu, T.; et al. Biochemical and echocardiographic markers for the early detection of cardiotoxicity under monoclonal antibodies therapy. J. Mind Med Sci. 2021, 8, 34–43. [Google Scholar] [CrossRef]
- Manea, M.; Bratu, O.; Bacalbasa, N.; Diaconu, C. Diagnosis and management of pericardial effusion. J. Mind Med Sci. 2020, 7, 148–155. [Google Scholar] [CrossRef]
- Bertone-Johnson, E.R.; Whitcomb, B.W.; Rich-Edwards, J.W.; Hankinson, S.E.; Manson, J.E. Premenstrual Syndrome and Subsequent Risk of Hypertension in a Prospective Study. Am. J. Epidemiology 2015, 182, 1000–1009. [Google Scholar] [CrossRef]
- Halbreich, U. The etiology, biology, and evolving pathology of premenstrual syndromes. Psychoneuroendocrinology 2003, 28, 55–99. [Google Scholar] [CrossRef]
- Keenan, P.; Stern, R.; Janowsky, D.; Pedersen, C. Psychological aspects of premenstrual syndrome I: Cognition and memory. Psychoneuroendocrinology 1992, 17, 179–187. [Google Scholar] [CrossRef]
- Giuliano, R.J.; Karns, C.M.; Bell, T.A.; Petersen, S.; Skowron, E.A.; Neville, H.J.; Pakulak, E. Parasympathetic and sympathetic activity are associated with individual differences in neural indices of selective attention in adults. Psychophysiology 2018, 55, e13079. [Google Scholar] [CrossRef]
- Knight, E.L.; Giuliano, R.J.; Shank, S.W.; Clarke, M.M.; Almeida, D.M. Parasympathetic and sympathetic nervous systems interactively predict change in cognitive functioning in midlife adults. Psychophysiology 2020, 57, e13622–e13622. [Google Scholar] [CrossRef]
- Bassi, A.; Bozzali, M. Potential Interactions between the Autonomic Nervous System and Higher Level Functions in Neurological and Neuropsychiatric Conditions. Front. Neurol. 2015, 6, 182. [Google Scholar] [CrossRef]