Congenital Epulis: A Two-Case Report
Abstract
Introduction
Case Presentation
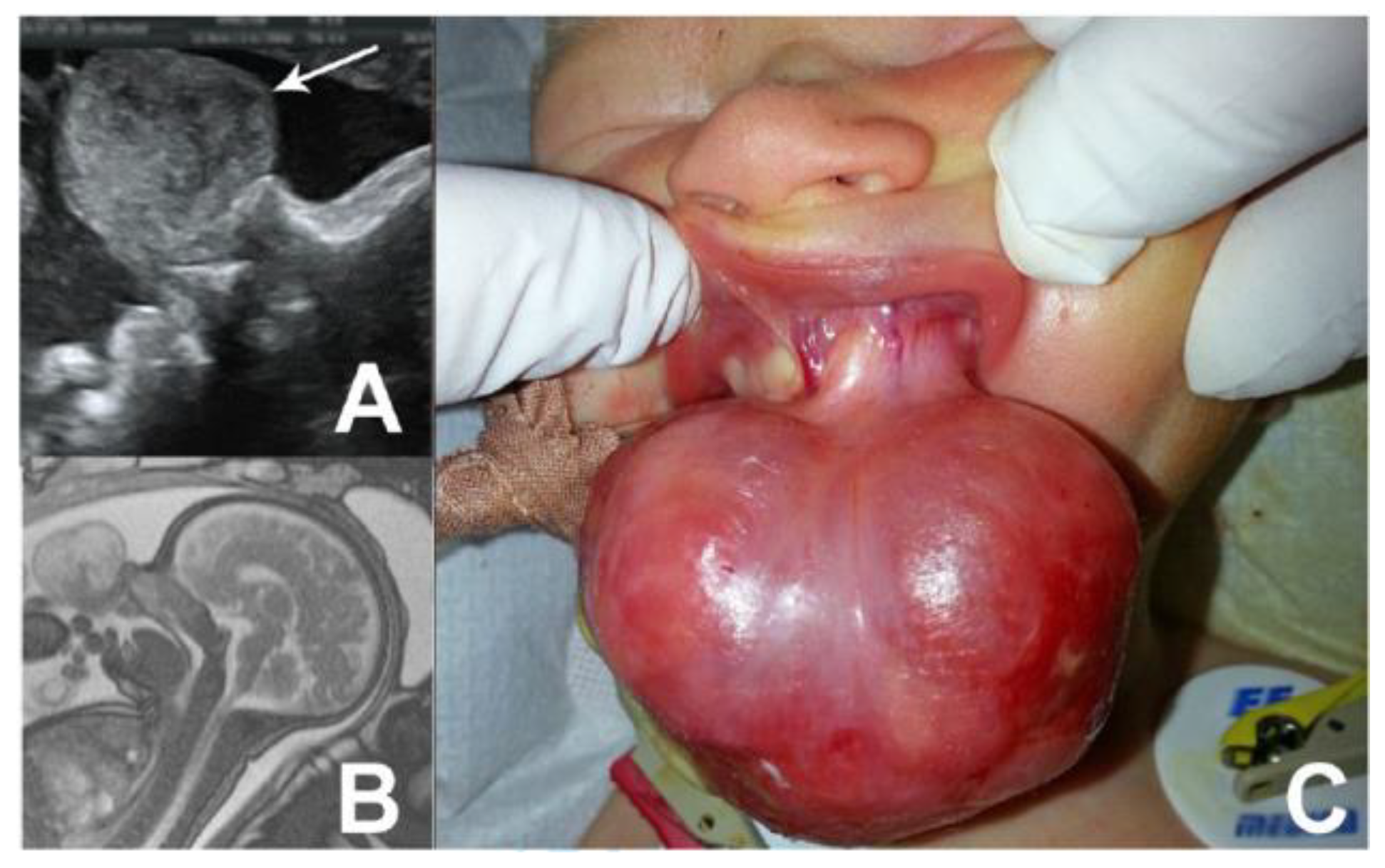
Case no. 1
Case no. 2.
Discussions
Highlights
- ✓
- Congenital epulis is a rare oral tumor of the newborn.
- ✓
- The size and position of congenital epulis make the tumor at risk for airway obstruction of the newborn or bleeding during delivery or shortly after.
- ✓
- Prenatal diagnosis of oral tumors in the newborn is essential to consider to build-up perinatal multidisciplinary management plan.
Conclusions
Conflicts of Interest disclosure
Compliance with ethical standards
References
- Küpers, A.M.; Andriessen, P.; van Kempen, M.J.; van der Tol, I.G.; Baart, J.A.; Dumans, A.G.; van der Waal, I. Congenital epulis of the jaw: a series of five cases and review of literature. Pediatr Surg Int. 2009, 25, 207–210. [Google Scholar] [CrossRef] [PubMed]
- Evans, D.A. Congenital epulis. Otolaryngol Head Neck Surg. 2001, 125, 283–284. [Google Scholar] [CrossRef] [PubMed]
- Merrett, S.J.; Crawford, P.J. Congenital epulis of the newborn: a case report. Int J Paediatr Dent. 2003, 13, 127–129. [Google Scholar] [CrossRef]
- Lee, J.M.; Kim, U.K.; Shin, S.H. Multiple congenital epulis of the newborn: a case report and literature review. J Ped Surg Case Reports. 2013, 1, 32–33. [Google Scholar] [CrossRef][Green Version]
- Roy, S.; Sinsky, A.; Williams, B.; Desilets, V.; Patenaude, Y.G. Congenital epulis: prenatal imaging with MRI and ultrasound. Pediatr Radiol. 2003, 33, 800–803. [Google Scholar] [CrossRef]
- Kumar, B.; Sharma, S.B. Neonatal oral tumors: congenital epulis and epignathus. J Pediatr Surg. 2008, 43, e9–e11. [Google Scholar] [CrossRef]
- Suciu, N.; Serban, A.; Toader, O.; Oprescu, D.; Spataru, R.I. Case report of fetal lingual tumor—perinatal care and neonatal surgical intervention. J Matern Fetal Neonatal Med. 2014, 27, 314–319. [Google Scholar] [CrossRef]
- Kumar, P.; Kim, H.H.; Zahtz, G.D.; Valderrama, E.; Steele, A.M. Obstructive congenital epulis: prenatal diagnosis and perinatal management. Laryngoscope. 2002, 112, 1935–1939. [Google Scholar] [CrossRef]
- Serban, D.; Smarandache, C.G.; Tudor, C.; Duta, L.N.; Dascalu, A.M.; Aliuș, C. Laparoscopic Surgery in COVID-19 Era- Safety and Ethical Issues. Diagnostics (Basel). 2020, 10, 673. [Google Scholar] [CrossRef]
- Serban, D.; Spataru, R.I.; Vancea, G.; Balasescu, S.A.; Socea, B.; Tudor, C.; Dascalu, A.M. Informed consent in all surgical specialties: from legal obligation to patient satisfaction. Rom J Leg Med. 2020, 28, 317–321. [Google Scholar] [CrossRef]
- Ritwik, P.; Brannon, R.B.; Musselman, R.J. Spontaneous regression of congenital epulis: a case report and review of the literature. J Med Case Rep. 2010, 4, 331. [Google Scholar] [CrossRef] [PubMed]
- Popescu, B.; Oașă, I.D.; Curcă, C.; et al. First impressions on TOUSS approach of the oral cavity and pharyngeal malignant tumors. J Clin Invest Surg. 2019, 4, 72–76. [Google Scholar] [CrossRef]
- Jain, N.; Sinha, P.; Singh, L. Large Congenital Epulis in a Newborn: Diagnosis and Management. Ear Nose Throat, J. 2020, 99, NP79–NP81. [Google Scholar] [CrossRef]
- Sharma, D.; Murki, S.; Pratap, T.; Leelakumar, V. Twin congenital epulis in the alveolar ridge of the maxilla and mandible in a newborn: a rare and interesting case. BMJ Case Rep. 2014, 2014, bcr2014206490. [Google Scholar] [CrossRef]
- Kayıran, S.M.; Buyukunal, C.; Ince, U.; Gürakan, B. Congenital epulis of the tongue: A case report and review of the literature. JRSM Short Rep. 2011, 2, 62. [Google Scholar] [CrossRef]
- Rafique, A.; Habib, H.; Rehman, F.A.; Arshi, S. Impact of rational and experiential thinking styles on interpersonal conflict resolution among young adults. J Mind Med Sci. 2020, 7, 69–78. [Google Scholar] [CrossRef]
- Bang, K.O.; Bodhade, A.S.; Dive, A.M. Congenital granular cell epulis of a newborn. Dent Res J (Isfahan). 2012, 9 (Suppl 1), S136–S138. [Google Scholar]
- Vered, M.; Dobriyan, A.; Buchner, A. Congenital granular cell epulis presents an immunohistochemical profile that distinguishes it from the granular cell tumor of the adult. Virchows Arch. 2009, 454, 303–310. [Google Scholar] [CrossRef]
- Spataru, R.I.; Sirbu, A.; Sirbu, D. Forensic ramifications in diagnosing and treating high forms of the Hirschsprung’s disease. Rom J Leg Med. 2013, 21, 105–110. [Google Scholar]
- Serban, D.; Smarandache, A.M.; Cristian, D.; Tudor, C.; Duta, L.; Dascalu, A.M. Medical errors and patient safety culture—shifting the healthcare paradigm in Romanian hospitals. Rom J Leg Med. 2020, 28, 195–201. [Google Scholar] [CrossRef]
- Popescu, B.; Oașă, I.D.; Bertesteanu, S.V.; Balalau, C.; Manole, F.; Domuta, M.; Oancea, A.L. Strategies to improve activity and results of the head and neck tumor board. J Clin Invest Surg. 2020, 5, 9–12. [Google Scholar] [CrossRef]
- Narasimhan, K.; Arneja, J.S.; Rabah, R. Treatment of congenital epulis (granular cell tumour) with excision and gingivoperiosteoplasty. Can J Plast Surg. 2007, 15, 215–218. [Google Scholar] [CrossRef] [PubMed]
- Adeyemi, B.F.; Oluwasola, A.O.; Adisa, A.O. Congenital epulis. Indian J Dent Res. 2010, 21, 292–294. [Google Scholar] [CrossRef]
- Kaiserling, E.; Ruck, P.; Xiao, J.C. Congenital epulis and granular cell tumor: a histologic and immunohistochemical study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995, 80, 687–697. [Google Scholar] [CrossRef]
- Karamchandani, J.R.; Nielsen, T.O.; van de Rijn, M.; West, R.B. Sox10 and S100 in the diagnosis of soft-tissue neoplasms. Appl Immunohistochem Mol Morphol. 2012, 20, 445–450. [Google Scholar] [CrossRef]
- Truschnegg, A.; Acham, S.; Kiefer, B.A.; Jakse, N.; Beham, A. Epulis: a study of 92 cases with special emphasis on histopathological diagnosis and associated clinical data. Clin Oral Investig. 2016, 20, 1757–1764. [Google Scholar] [CrossRef]
- Orosz, M.; Szende, B.; Gábris, K. The clinical and pathological symptoms of pregnancy epulis. Fogorv Sz. 2007, 100, 237–241. [Google Scholar]
- Spataru, R.I.; Popoiu, M.C.; Ivanov, M. Foregut duplication cyst associated with esophageal atresia-one-stage neonatal surgical repair. Indian J Surg. 2015, 77 (Suppl 1), 52–55. [Google Scholar] [CrossRef][Green Version]
- Spătaru, R.I.; Martius, E.; Ivan, L.E.; Sirbu, D.; Hostiuc, S. Pseudomembranous colitis complicating the natural course of Crohn’s disease in a pediatric patient. Rom J Legal Med. 2014, 22, 161–166. [Google Scholar] [CrossRef][Green Version]
- Aparna, H.G.; Jayanth, B.S.; Shashidara, R.; Jaishankar, P. Congenital epulis in a newborn: a case report, immunoprofiling and review of literature. Ethiop J Health Sci. 2014, 24, 359–362. [Google Scholar] [CrossRef]
- Miulescu, R.E.; Guja, L.; Socea, B.; Dumitriu, A.; Paunica, S.; Ștefănescu, E. Oral pathology induced by excess or deficiency of glucocorticoids in adults. J Mind Med Sci. 2020, 7, 141–147. [Google Scholar] [CrossRef]
- Spataru, R. The use of mechanical suture in the treatment of Hirschsprung’s disease: experience of 17 cases. Chirurgia (Bucur). 2014, 109, 208–212. [Google Scholar]

Share and Cite
Ivanov, M.; Stroe, B.; Ardeleanu, V.; Hainarosie, R.; Constantin, V.D.; Dumitriu, A.S.; Paunica, S.; Kadar, A. Congenital Epulis: A Two-Case Report. J. Mind Med. Sci. 2021, 8, 336-340. https://doi.org/10.22543/7674.82.P336340
Ivanov M, Stroe B, Ardeleanu V, Hainarosie R, Constantin VD, Dumitriu AS, Paunica S, Kadar A. Congenital Epulis: A Two-Case Report. Journal of Mind and Medical Sciences. 2021; 8(2):336-340. https://doi.org/10.22543/7674.82.P336340
Chicago/Turabian StyleIvanov, Monica, Bianca Stroe, Valeriu Ardeleanu, Razvan Hainarosie, Vlad Denis Constantin, Anca Silvia Dumitriu, Stana Paunica, and Anna Kadar. 2021. "Congenital Epulis: A Two-Case Report" Journal of Mind and Medical Sciences 8, no. 2: 336-340. https://doi.org/10.22543/7674.82.P336340
APA StyleIvanov, M., Stroe, B., Ardeleanu, V., Hainarosie, R., Constantin, V. D., Dumitriu, A. S., Paunica, S., & Kadar, A. (2021). Congenital Epulis: A Two-Case Report. Journal of Mind and Medical Sciences, 8(2), 336-340. https://doi.org/10.22543/7674.82.P336340


