Abstract
Klebsiella pneumoniae has emerged as the predominant pathogenic agent of liver abscess in Asia, and the incidence is increasing worldwide. Hypervirulent strains are associated with septic metastatic dissemination in the eyes, lungs, and central nervous system, causing severe morbidity. We present the case of a 54year old man, with no previous comorbidities, admitted in emergency for the blind red painful eye. Further investigation documented septic endophthalmitis with transscleral extension and orbital cellulitis. Thoraco-abdominal computed tomography evidenced a hepatic abscess as the locus of the primary infection. Intravenous antibiotherapy with cefuroxime, followed by meropenem and vancomycin were efficient for managing the hepatic abscess. However, as the eyeball was perforated at the admission, evisceration was performed. The vitreous sample revealed Klebsiella pneumoniae, with a positive string test as the etiologic agent. The diagnostic and therapeutic management required a permanent collaboration between an ophthalmologist, infectious diseases specialist, surgeon, and radiologist.
Introduction
Liver abscess is a relatively infrequent clinical entity which may be caused by a wide variety of bacteria, fungi and parasites. The reported annual incidence varies between 3-4 cases per 100,000 in the Europe United States, up to 17.6 per 100,000 in Taiwan [1].
Classically, most of the abscess liver encountered in clinical practice are plurimicrobial, being in 50-70% of cases a complication of septic process located at the biliary ducts, portal system or less frequently, hematogenic dissemination via hepatic artery [2,3]. Less frequently, there are cases of liver abscesses after duodeno-pancreatic surgery, which involve operative times in the main bile duct, post-alcoholization of primary or metastatic liver tumors, by superinfection of pre-existing liver cysts or as a postoperative complication of segmental liver transplants [3,4].
Clinical and epidemiological studies evidenced that Klebsiella pneumonia has emerged as the predominant pathogen of pyogenic liver abscesses, surpassing Escherichia coli, with the prevalence growing from 30% in the 1980s to more than 80% in the 1990s in Taiwan (30), and accounting for 63.9% of cases of pyogenic liver abscesses in China according to Qian et al, in a 21 years study period, during 1994-2005 [5]. There are increasing evidences of the worldwide dissemination of the hypervirulent strains of Klebsiella pneumoniae which cause community acquired cryptogenic liver abscess, with possible secondary hematogenous disseminations in eyes, lungs and central nervous system, requiring a multidisciplinary approach.
Case Presentation
We report the case of a 54 years old man, with no previously known chronic comorbidities and no recent history of ocular trauma, who presented in Emergency at the Ophthalmology ward with decreased vision, and severe ocular pain, photophobia and tearing in his right eye, with progressive onset during the last 10 days. The patient was consulted on ambulatory basis and diagnosed with acute uveitis. As he initially refused hospitalization, he was prescribed topic mydriatics, antibiotics (tobramycin), corticosteroid and non-corticosteroid anti-inflammatory eyedrops. As the symptoms were getting worse under local treatment, he presented in emergency for further investigation and therapy.
Physical exam at admission revealed subfebrility (37.8⁰C), loss of appetite, nausea and a ponderal loss of 7 kg during the last 2 weeks
Ophthalmological exam showed a red painful eye, with a visual acuity of no light perception. The ocular tonus was increased at digital evaluation. The biomicroscopic examination evidenced chemosis, periorbital cellulitis, intense corneal edema, hypopyon, circumferential irido- lenticular synechiae and a dense fibrinous exudate in the pupillary area and limited painful ocular motility. The opacification of the lens and edema of the cornea impended the direct examination of the posterior segment. The left eye was of normal clinical appearance. After being tested for COVID-19, the patient was admitted in the Ophthalmology department with a presumed diagnosis of endophthalmitis of the right eye, following the strict protocol for COVID-19 preventing of intrahospital dissemination [6,7,8].
Imagistic evaluation was further performed to evaluate the extension of the inflammatory process at the level of the posterior segment of the right eye.
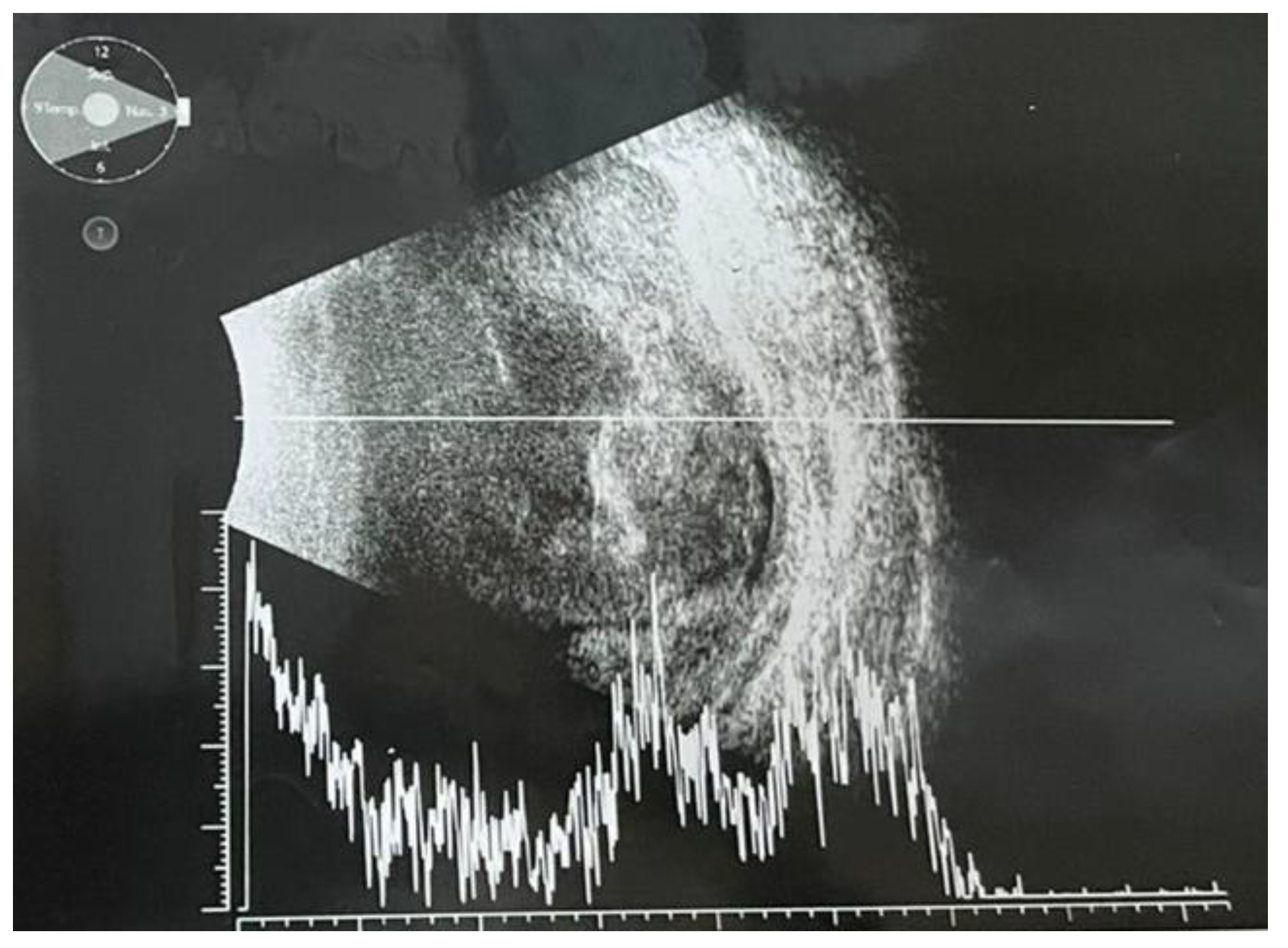
Ultrabiomicroscopy (UBM) confirmed posterior irido- lenticular synechiae on 360⁰ and thickening of the ciliary body (Figure 1). Ocular ultrasound exam revealed total retinal detachment, multiple fine vitreous echoes suggestive for vitritis, homogeneous thickening of the choroid and a 3mm diameter hyperechogenic mass invading sclera (Figure 2). A differential diagnosis between an extrascleral extension of an endophthalmitis and a possible intraocular tumor with scleral penetration was considered.

Figure 1.
Ultrabiomicroscopy: circumferentially posterior synechiae and ciliary body thickening.
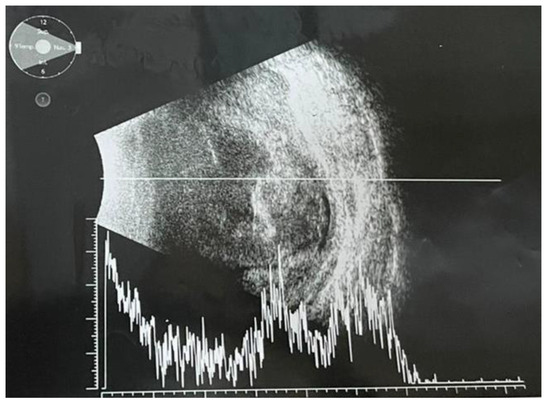
Figure 2.
Ocular ultrasonography (mode A/B): total retinal detachment, retinal and choroidal thickening; multiple densities in the vitreous body suggestive for vitritis; in the superior sector, a hypodense mass with loss of scleral echo and deformed ocular contour.
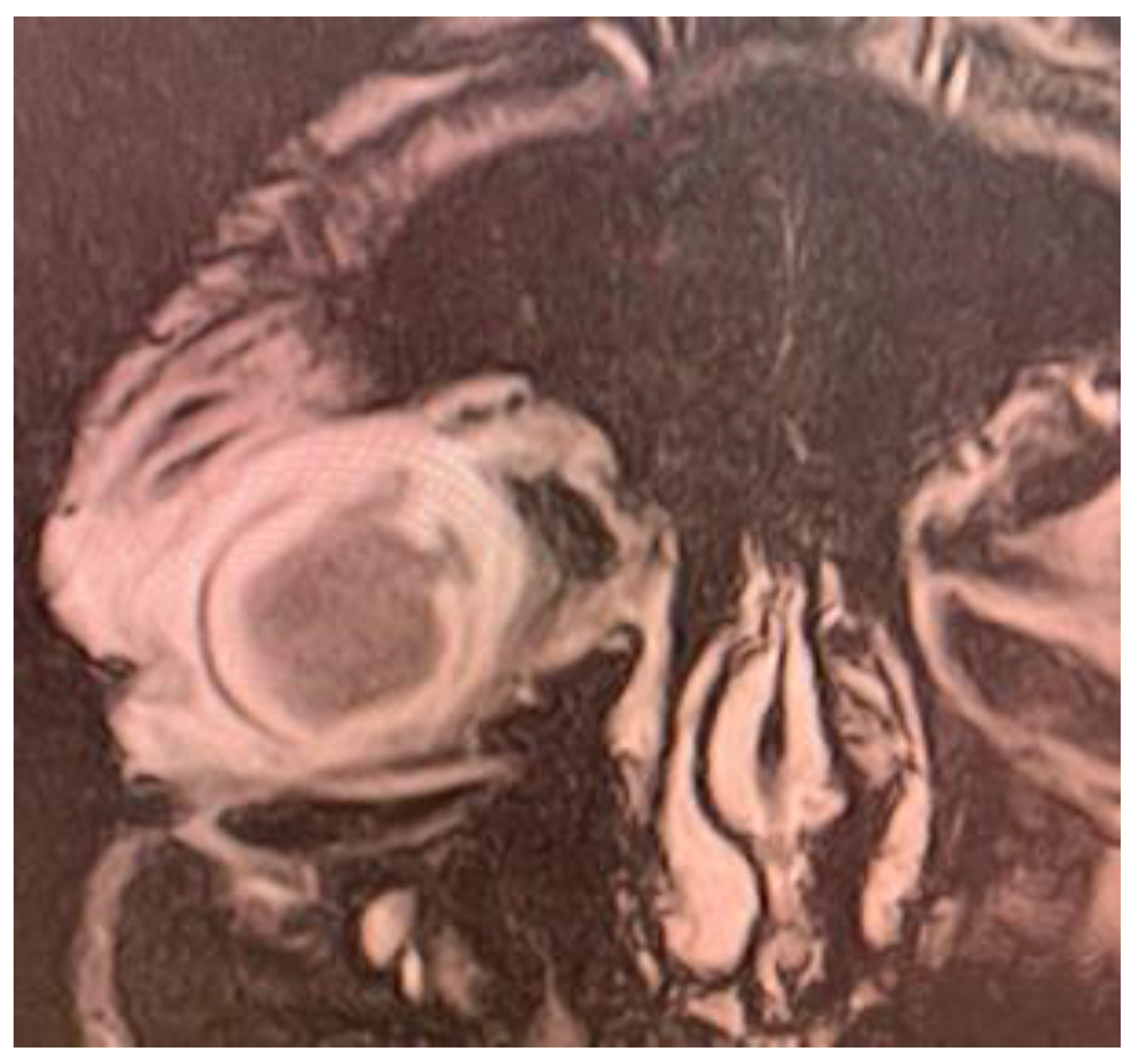
Magnetic resonance imaging (MRI) exam showed deformed right eyeball of reduced volume, with irregulated contour at the level of the medial convexity, at which level the scleral contour appeared interrupted, with underlying thickened choroid and vitreous body prolapse. Posterior lens luxation and increased hematogenous density of vitreous body were evidenced. Moderate inflammation of the preseptal and postseptal soft tissue was noticed (Figure 3).
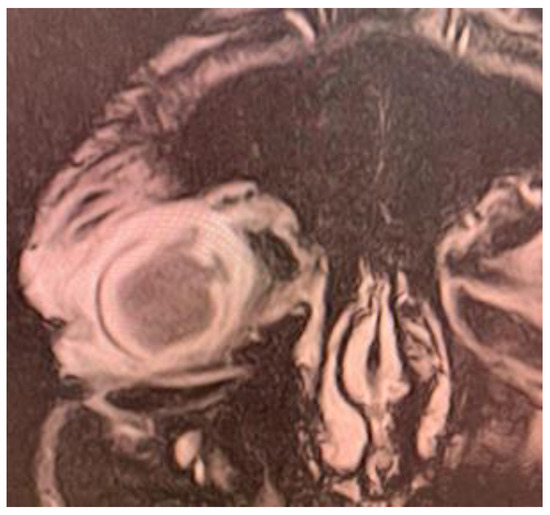
Figure 3.
MRI exam: Right eye endophthalmitis with scleral abscess and perforation; increased density of vitreous body, deformed eye contour, with 2 area of scleral perforation in the superior and internal part; exophthalmia with inflammatory changes of the periorbital soft tissue.
Based on the clinical and imagistic examination, the diagnosis of endogenous endophthalmitis, with scleral perforation and subconjunctival abscess was established.
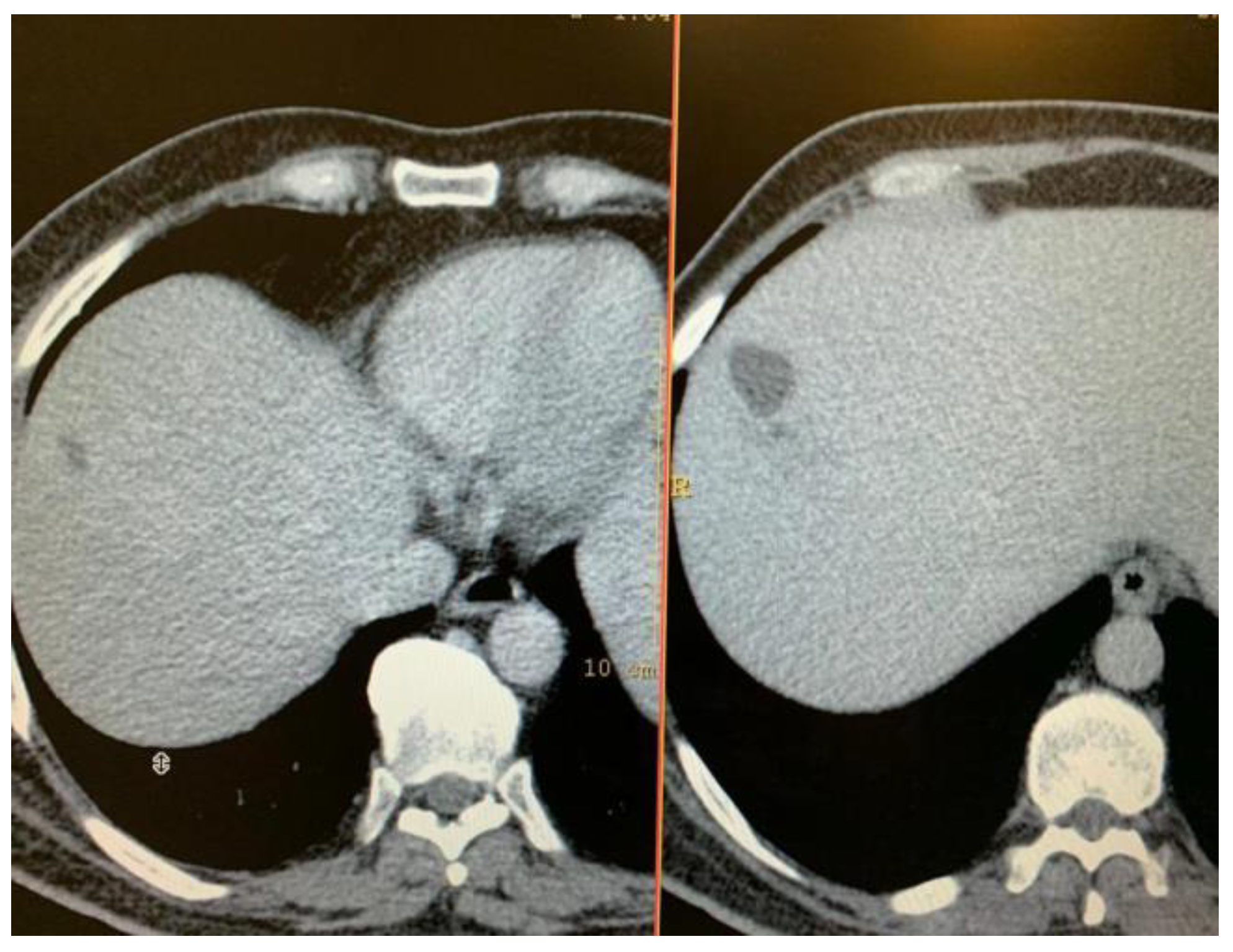
Thoraco-abdominal computer tomography was performed to identify the focus of the primary infection, in a patient with no other organ specific symptomatology. A multiloculated, non-homogenous hepatic abscess located in the right lobe, segment VIII, of 50/32/57 mm diameter, surrounded by a hypodense area. The paraclinical data confirmed the general inflammatory syndrome, with and ESR (12 mm/h), leukocytosis 15.7/30*3/microL with neutrophilia 84.2%, and showed mild increase of hepatic enzymes: AST (85UI/L), GGT (113 UI/l). Blood culture were obtained, but could not identify any pathogenic agent. IG ELISA for Echinococcosis was negative. Infectious disease and general surgery evaluation recommended empiric general antibiotherapy was initiated with intravenous Ceftriaxone 1 g/day, switched after 5 days to meropenem 1g at 8 hours and Vancomycin 1 g at 12 hours for, for 14 day. Progressive remission of the hepatic liver abscess was observed on serial computer tomography (Figure 4).
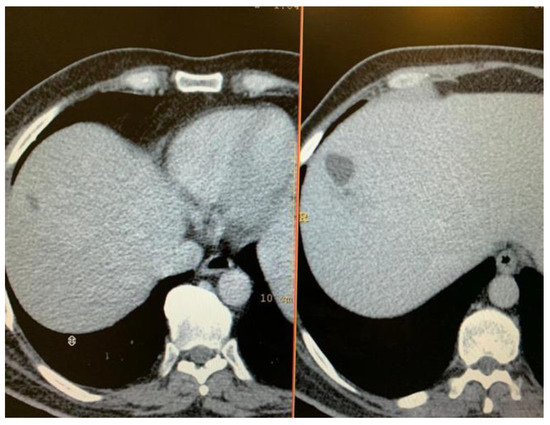
Figure 4.
Serial CT exam: diminished size of the right lobe hepatic abscess: a) after intravenous therapy; b) at admission.
Local ophthalmic therapy was started with mydriatics (cyclopentolate, phenylephrine, tropicamide), antibiotics (ceftriaxone, ciprofloxacin, vancomycin) and dexamethasone. However, due to delayed presentation, with perforated eyeball at the admission, evisceration was performed. During surgery, vitreous samples were taken and send to bacteriology examination. Klebsiella pneumoniae, with positive string test, of >5mm, and “wild- type” antibiotic resistance, sensitive to cephalosporins, carbapenems, amikacin and fluoroquinolones was identified as the etiologic agent.
The patient was discharged after 20 days of hospitalization, with the indication to continue the topical ocular treatment with ciprofloxacin and general antibiotic therapy with levofloxacin 500 mg/day and cefuroxime 500mg twice per day for 14 days. Follow-up at 14 days and 1 months showed a favorable evolution, with total remission of the hepatic abscess and no local or systemic recurrences.
Discussions
Klebsiella pneumoniae is a Gram-negative microorganism, which has attracted special attention due to lung, urinary and bloodstream infections, acquired both intra-community and hospital acquired. Therapeutic management is threatened by the complex mechanisms of multidrug resistance, mainly due to extended spectrum beta-lactamases (ESBL), AmpC beta lactamases or carbapenamases [9], of the strains encountered in hospital environment. The increasing incidence of metastatic infection by K. pneumoniae in the East Asia in the recent decade may be explained by the emergence of hypervirulent strains of Klebsiella. Presentation signs of Klebiella pneumoniae liver abscess are generally non- specific, with nausea, vomiting, right upper quadrant tenderness and fever. A differential diagnosis should take into account acute biliary pathology, echinococcosis, hepatocarcinoma, infectious and toxic hepatitis, especially in cases with occupational increased risk [10,11,12].
“Invasive Klebsiella pneumoniae liver abscess syndrome” is encountered in 5-16% cases of Klebsiella pneumoniae liver abscess (KPLA) [13,14,15], but it is estimated to be up to 45% in infections with hypervirulent serotypes of KP [16]. Endophthalmitis is the most common (as many as 60% of cases) and serious septic lesion of this syndrome, followed by lung septic nodules (40%), meningitis (25%), and less frequently, necrotizing fasciitis, prostatic abscess, skin or osteoarticular nodules [17,18,19,20]. Presence of metastatic infection is associated 17% mortality and serious morbidity, mainly due to vision loss and permanent neurologic sequelae [21]. It is associated microbiologically with the presence of hypervirulent strain, K1 and less frequent K2, and clinically with diabetes and impaired glucose metabolism. Chronic hyperglycemia leads to the maintenance of low-level chronic inflammation, and defective phagocytosis, increased retinal-blood barrier and delayed healing [21]. Gut dysbiosis in diabetes may also favor the pathogenic agent translocation at the level of the intestinal wall [22,23].
The KPLA is a well define pathological entity, characterized by the fact that is community acquired, lack of associated hepato-biliary disease, with an increased potential of metastatic spread, varying between 11-45% in clinical studies [24,25,26]. Clinical signs are fever, nausea, vomiting, right upper quadrant pain and occasionally jaundice imposing differential diagnosis with acute cholecystitis [27].
The KPLA are frequent multilobulated, with solid appearance due to high viscosity of the pus, and often bigger than 5 cm in diameter. Specific characteristics of the KPLA are related with increase chance of metastatic dissemination of the infection: abscess of more than 5 cm in diameter, right lobe location, especially upper segments (VII and VIII), and the thrombosis of the suprahepatic vein, favoring the systemic spread via inferior vena cava [28,29,30].
Management of the KPLA is based on intravenous antibiotics with 3rd generation cephalosporins and/or carbapenems, followed by long term oral fluoroquinolones to prevent recurrences. Long term supportive antioxidant treatment may be helpful to prevent chronic inflammation and fibrosis [28,29]. In non-responders, percutaneous drainage may be performed, under CT or ultrasound guidance. However, surgeons have to take into account the high viscosity of the pus and the possibility of multiloculated lesions. Upper locations are considered a contraindication for percutaneous drainage due to the increased risk of accidentally pneumoperitoneum. In case of imminence of perforation, surgical drainage, under general anesthesia should be performed, but taking into account the anesthetic-surgical risk in sepsis, especially in elderly patients, with multiple comorbidities [31,32,33].
Mortality is relatively low, of 5-6%, similar to the one of non-KPLA [14], due to the “wild type” antibiotic resistance encountered in most cases. Death may appear due to spontaneous abscess rupture, septic shock, intravascular disseminated coagulation or septic dissemination in vital organs [34,35,36,37,38].
The endophthalmitis-liver abscess association was first described in 1986 in Taiwan, the etiologic agent encountered being Klebsiella pneumoniae [39]. In the following decades, the case reports on this unusual encounter became more and more frequent and further clinical studies developed in the next decades evidenced a growing incidence of this infectious pathology. Endogenous endophthalmitis is generally uncommon, but is the most frequent serious septic complication of KPLA and the outcome is usually extremely severe [40]. Early diagnosis, before vision loss and intensive intravitreal antibiotic injections could preserve some vision in affected eyes [28,29,30].
Highlights
- ✓
- Hypervirulent Klebsiella pneumoniae may cause cryptogenic hepatic abscess in previously healthy adults, with metastatic septic determinations, such as endophthalmitis.
- ✓
- Ophthalmic signs may precede hepatic ones and searching for the foculs of the iniatial infection may be challenging.
- ✓
- The therapeutic management is based on necessary interdisciplinary collaboration between several specialists such as ophthalmologist, infectious diseases specialist, surgeon and radiologist.
Conclusions
The particularity of the case was the fact that ocular symptoms preceded the hepatic ones, which was one of the causes of delayed diagnosis. The ophthalmic signs brought the patient to the emergency department and prevent other life-threatening complications, such as central nervous system dissemination and meningitis. The diagnostic and therapeutic management required a permanent collaboration between ophthalmologist, infectious diseases specialist, surgeon and radiologist. The case proves the community presence and dissemination of the hypervirulent Klebsiella pneumoniae strains in our country and the devastating potential of this pathogenic agent even in previously healthy adults.
Abbreviations
hvKp: hypervirulent Klebsiella pneumoniae; KPLA: Klebsiella pneumoniae liver abscess.
Conflicts of Interest disclosure
There are no known conflicts of interest in the publication of this article. The manuscript was read and approved by all authors.
Compliance with ethical standards
Any aspect of the work covered in this manuscript has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript.
References
- Tsai, F.C.; Huang, Y.T.; Chang, L.Y.; Wang, J.T. Pyogenic liver abscess as endemic disease, Taiwan. Emerg Infect Dis. 2008, 14, 1592–1600. [Google Scholar] [CrossRef] [PubMed]
- Jun, J.B. Klebsiella pneumoniae Liver Abscess. Infect Chemother. 2018, 50, 210–218. [Google Scholar] [CrossRef] [PubMed]
- Han, S.H. Review of hepatic abscess from Klebsiella pneumoniae. An association with diabetes mellitus and septic endophthalmitis. West J Med. 1995, 162, 220–224. [Google Scholar]
- Maggi, U.; Formiga, A.; Lauro, R. Hepatic abscess as a complication of duodenal-jejunal bypass sleeve system and review of the literature. Surg Obes Relat Dis. 2016, 12, e47–e50. [Google Scholar] [CrossRef]
- Qian, Y.; Wong, C.C.; Lai, S.C.; Lin, Z.H.; Zheng, W.L.; Zhao, H.; Pan, K.H.; Chen, S.J.; Si, J.M. Klebsiella pneumoniae invasive liver abscess syndrome with purulent meningitis and septic shock: A case from mainland China. World J Gastroenterol. 2016, 22, 2861–2866. [Google Scholar] [CrossRef]
- Dascalu, A.M.; Tudosie, M.S.; Smarandache, G.C.; Serban, D. Impact of COVID-19 pandemic upon ophthalmological clinical practice. Rom J Leg Med. 2020, 28, 96–100. [Google Scholar] [CrossRef]
- Popescu, B.; Doinița, O.I.; Bălălău, C.; Scăunașu, R.; Manole, F.; Domuța, M.; Oancea, A.L. Fibroscopic examination on ENT patients in COVID-19 era. J Clin Invest Surg. 2020, 5, 63–65. [Google Scholar] [CrossRef]
- Marina, C.N.; Gheoca-Mutu, D.E.; Răducu, L.; Avino, A.; Brîndușe, L.A.; Stefan, C.M.; Scaunasu, R.V.; Jecan, C.R. COVID-19 outbreak impact on plastic surgery residents from Romania. J Mind Med Sci. 2020, 7, 212–216. [Google Scholar] [CrossRef]
- Pichler, C.; Büchsel, M.; Rossen, J.W.; Vavra, M.; Reuter, S.; Kern, W.V.; Thimme, R.; Mischnik, A. First report of invasive liver abscess syndrome with endophthalmitis caused by a K2 serotype ST2398 hypervirulent Klebsiella pneumoniae in Germany, 2016. New Microbes and New Infections. 2017, 17, 77–80. [Google Scholar] [CrossRef]
- Oikonomou, K.G.; Aye, M. Klebsiella Pneumoniae Liver Abscess: A Case Series of Six Asian Patients. Am J Case Rep 2017, 18, 1028–1033. [Google Scholar] [CrossRef]
- Kamal, F.; Williams, G.; Akbar, H.; Khan, M.A.; Kadaria, D. Klebsiella Pneumoniae Liver Abscess: a Case Report and Review of Literature. Cureus. 2017, 9, e970. [Google Scholar] [CrossRef] [PubMed]
- Stefan, D.S.; Constantinescu, R.R.; Meghea, A.; Anghel, R.; Stefan, M.; Tudosie, M.S. Obtaining of Biofertilisers Using Pelt Skin Wastes. Rev. Chim. (Bucharest). 2016, 67, 1401–1405. [Google Scholar]
- Chiu, C.T.; Lin, D.Y.; Liaw, Y.F. Metastatic Septic Endophthalmitis in Pyogenic Liver Abscess. Journal of Clinical Gastroenterology. 1988, 10, 524–527. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.J.; Liu, Y.C.; Lee, S.S.J.; Yen, M.Y.; Chen, Y.S.; Wang, J.H.; Wann, S.R.; Lin, H.H. Primary Liver Abscess Due to Klebsiella pneumoniae in Taiwan. Clinical Infectious Diseases. 1998, 26, 1434–1438. [Google Scholar] [CrossRef]
- Kashani, A.H.; Eliott, D. The emergence of Klebsiella pneumoniae endogenous endophthalmitis in the USA: basic and clinical advances. J Ophthal Inflamm Infect. 2013, 3, 28. [Google Scholar] [CrossRef]
- Jun, J.B. Klebsiella pneumoniae Liver Abscess. Infect Chemother. 2018, 50, 210–218. [Google Scholar] [CrossRef]
- Cheng, D.L.; Liu, Y.C.; Yen, M.; Liu, Y.C.; Wang, R.S. Septic metastatic lesions of pyogenic liver abscess. Their association with Klebsiella pneumoniae bacteremia in diabetic patients. Arch Intern Med 1991, 151, 1557–1559. [Google Scholar] [CrossRef]
- Tudorachi, N.-B.; Eva, I.; Dascalu, C.G.; AL-Hiary, R.; Barbieru, B.; Paunica, M.; Motofei, C.; Moraru, A.-C. The influence of serum calcium and magnesium levels in the radiological evolution of knee osteoarthritis. J Mind Med Sci. 2020, 7, 217–226. [Google Scholar] [CrossRef]
- Braiteh, F.; Golden, M.P. Cryptogenic invasive Klebsiella pneumoniae liver abscess syndrome. Int J Infect Dis. 2007, 11, 16–22. [Google Scholar] [CrossRef]
- García-Cruz, E.; Otero, J.R.; Ineva, P.A.; Pérez, L.M.M.; Elías, L.P.; Asensio, A.A. Robot-assisted aquablation for resection of benign prostatic hyperplasia: A series of cases. J Clin Invest Surg. 2020, 5, 18–23. [Google Scholar] [CrossRef]
- Serban, D.; Papanas, N.; Dascalu, A.M.; et al. Diabetic Retinopathy in Patients with Diabetic Foot Ulcer: A Systematic Review. The International Journal of Lower Extremity Wounds. 2021, 20, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Suceveanu, A.I.; Stoian, A.P.; Parepa, I.; Voinea, C.; Hainarosie, R.; Manuc, D.; Nitipir, C.; Mazilu, L.; Suceveanu, A.P. Gut Microbiota Patterns in Obese and Type 2 Diabetes (T2D) Patients from Romanian Black Sea Coast Region. Rev Chim. 2018, 69, 2260–2267. [Google Scholar] [CrossRef]
- Moraru, D.; Dumitru, A.; Micu, S.I.; Musat, M.; Preda, G.; Popoiag, R.E. The burden of clostridium difficile infection in patients with liver cirrhosis. J Mind Med Sci. 2019, 6, 237–242. [Google Scholar] [CrossRef]
- Yang, C.S.; Tsai, H.Y.; Sung, C.S.; Lin, K.H.; Lee, F.L.; Hsu, W.M. Endogenous Klebsiella Endophthalmitis Associated with Pyogenic Liver Abscess. Ophthalmology. 2007, 114, 876–880. [Google Scholar] [CrossRef]
- Pastagia, M.; Arumugam, V. Klebsiella pneumoniae liver abscesses in a public hospital in Queens, New York. Travel Med Infect Dis. 2008, 6, 228–233. [Google Scholar] [CrossRef]
- Wang, H.; Ren, Y.; Chang, Z.; Liu, Z. The increased recurrence rate of liver abscess caused by extended-spectrum β-lactamase-producing Klebsiella pneumoniae. Eur J Clin Microbiol Infect Dis. 2020, 39, 1315–1320. [Google Scholar] [CrossRef]
- Serban, D.; Socea, B.; Balasescu, S.A.; Badiu, C.D.; Tudor, C.; Dascalu, A.M.; Vancea, G.; Spataru, R.I.; Sabau, A.D.; Sabau, D.; Tanasescu, C. Safety of Laparoscopic Cholecystectomy for Acute Cholecystitis in the Elderly: A Multivariate Analysis of Risk Factors for Intra and Postoperative Complications. Medicina. 2021, 57, 230. [Google Scholar] [CrossRef]
- Park, I.H.; Jun, C.H.; Wi, J.W.; Park, S.Y.; Lee, W.S.; Jung, S.I.; Park, C.H.; Joo, Y.E.; Kim, H.S.; Choi, S.K.; Rew, J.S. Prevalence of and risk factors for endogenous endophthalmitis in patients with pyogenic liver abscesses. Korean J Intern Med. 2015, 30, 453–459. [Google Scholar] [CrossRef]
- Lee, J.Y.; Kim, K.H. Endogenous Endophthalmitis Complicated by Pyogenic Liver Abscess: A Review of 17 Years' Experience at a Single Center. Digestion. 2014, 90, 116–121. [Google Scholar] [CrossRef]
- Lin, J.C.; Siu, L.K.; Fung, C.P.; Tsou, H.H.; Wang, J.J.; Chen, C.T.; Wang, S.C.; Chang, F.Y. Impaired phagocytosis of capsular serotypes K1 or K2 Klebsiella pneumoniae in type 2 diabetes mellitus patients with poor glycemic control. J Clin Endocrinol Metab. 2006, 91, 3084–3087. [Google Scholar] [CrossRef]
- Gheorghe, G.; Stoian, A.P.; Gaman, M.; Socea, B.; Neagu, T.P.; Stanescu, A.M.A.; Bratu, O.G.; Mischianu, D.L.D.; Suceveanu, A.I.; Diaconu, C.C. The Benefits and Risks of Antioxidant Treatment in Liver Diseases. Rev Chim. 2019, 70, 651–655. [Google Scholar] [CrossRef]
- Radu, N.; Voicescu, M.; Radu, E.; Tanasescu, C. Biomaterial with antioxidant and antifungal activities, obtained from romanian indigenous plants. Molecular Crystals and Liquid Crystals. 2017, 655, 243–249. [Google Scholar] [CrossRef]
- Șerban, D.; Brănescu, C.M.; Smarandache, G.C.; Tudor, C.; Tănăsescu, C.; Tudosie, M.S.; Stana, D.; Costea, D.O.; Dascălu, A.M.; Spătaru, R.I. Safe surgery in day care centers: focus on preventing medical legal issues. Rom J Leg Med. 2021, 29, 60–64. [Google Scholar] [CrossRef]
- Fung, C.P.; Chang, F.Y.; Lee, S.C.; Hu, B.S.; Kuo, B.I.; Liu, C.Y.; Ho, M.; Siu, L.K. A global emerging disease of Klebsiella pneumoniae liver abscess: is serotype K1 an important factor for complicated endophthalmitis? Gut. 2002, 50, 420–424. [Google Scholar] [CrossRef]
- Cheng, D.L.; Liu, Y.C.; Yen, M.; Liu, Y.C.; Wang, R.S. Septic metastatic lesions of pyogenic liver abscess. Their association with Klebsiella pneumoniae bacteremia in diabetic patients. Arch Intern Med. 1991, 151, 1557–1559. [Google Scholar]
- Fang, C.T.; Lai, S.Y.; Yi, W.C.; Hsueh, P.R.; Liu, K.L.; Chang, S.C. Klebsiella pneumoniae genotype K1: an emerging pathogen that causes septic ocular or central nervous system complications from pyogenic liver abscess. Clin Infect Dis. 2007, 45, 284–293. [Google Scholar] [CrossRef]
- Chung, C.Y.; Wong, E.S.; Liu, C.C.H.; Wong, M.O.M.; Li, K.K.W. Clinical features and prognostic factors of Klebsiella endophthalmitis-10-year experience in an endemic region. Eye 2017, 31, 1569–1575. [Google Scholar] [CrossRef]
- Wells, J.T.; Lewis, C.R.; Danner, O.K.; Wilson, K.L.; Matthews, L.R. Klebsiella pneumoniae Liver Abscess and Metastatic Endophthalmitis. J Investig Med High Impact Case Rep. 2015, 4, 2324709615624125. [Google Scholar] [CrossRef]
- Liu, Y.C.; Cheng, D.L.; Lin, C.L. Klebsiella pneumoniae liver abscess associated with septic endophthalmitis. Arch Intern Med. 1986, 146, 1913–1916. [Google Scholar]
- Sheu, S.J. Endophthalmitis. Korean J Ophthalmol. 2017, 31, 283–289. [Google Scholar] [CrossRef]