A Rare Complication in a COVID-19 Positive Patient with Sigmoid Colon Cancer-Hemoperitoneum Due to Gallbladder Necrosis Following Micro-Thrombosis
Abstract
:Introduction
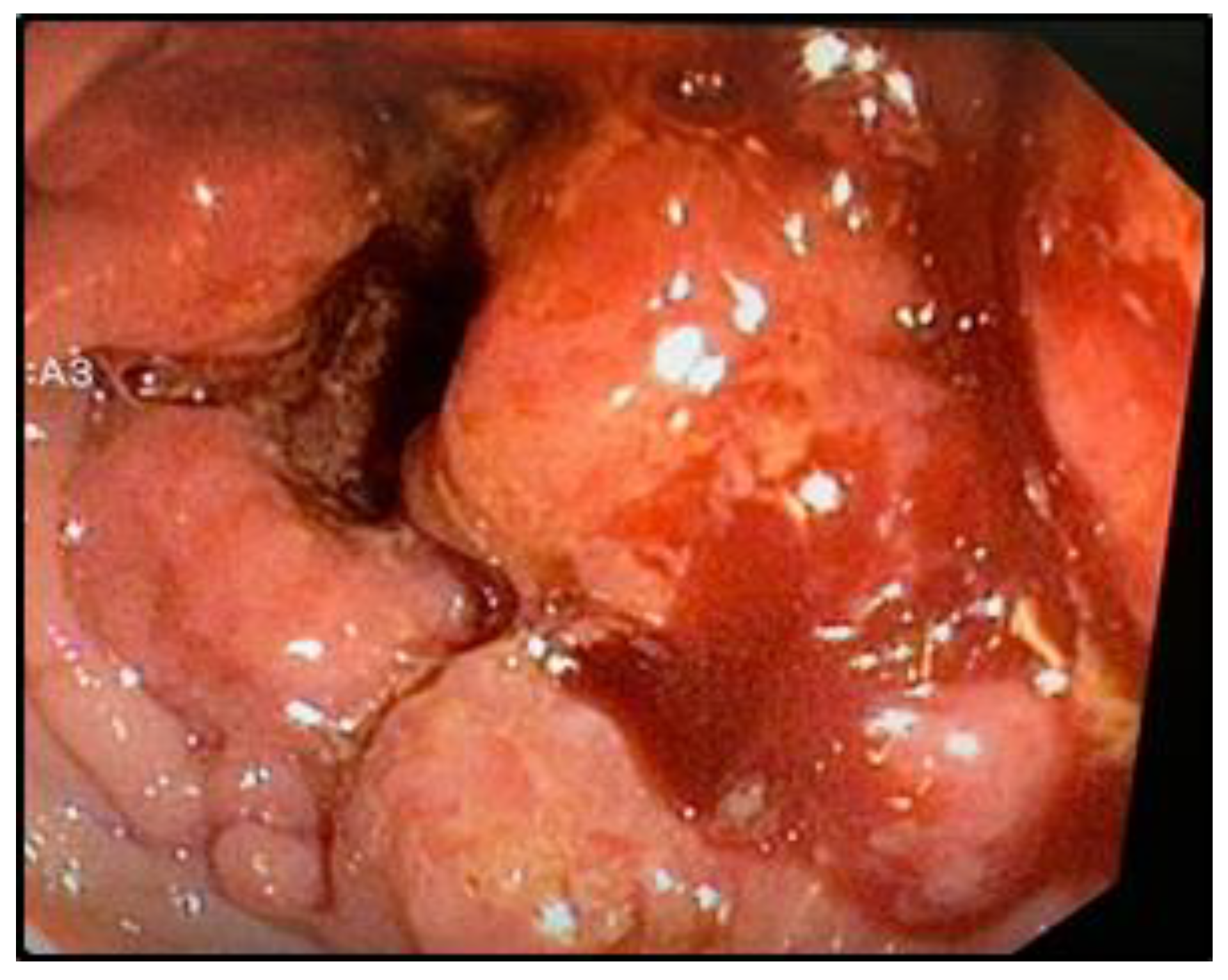
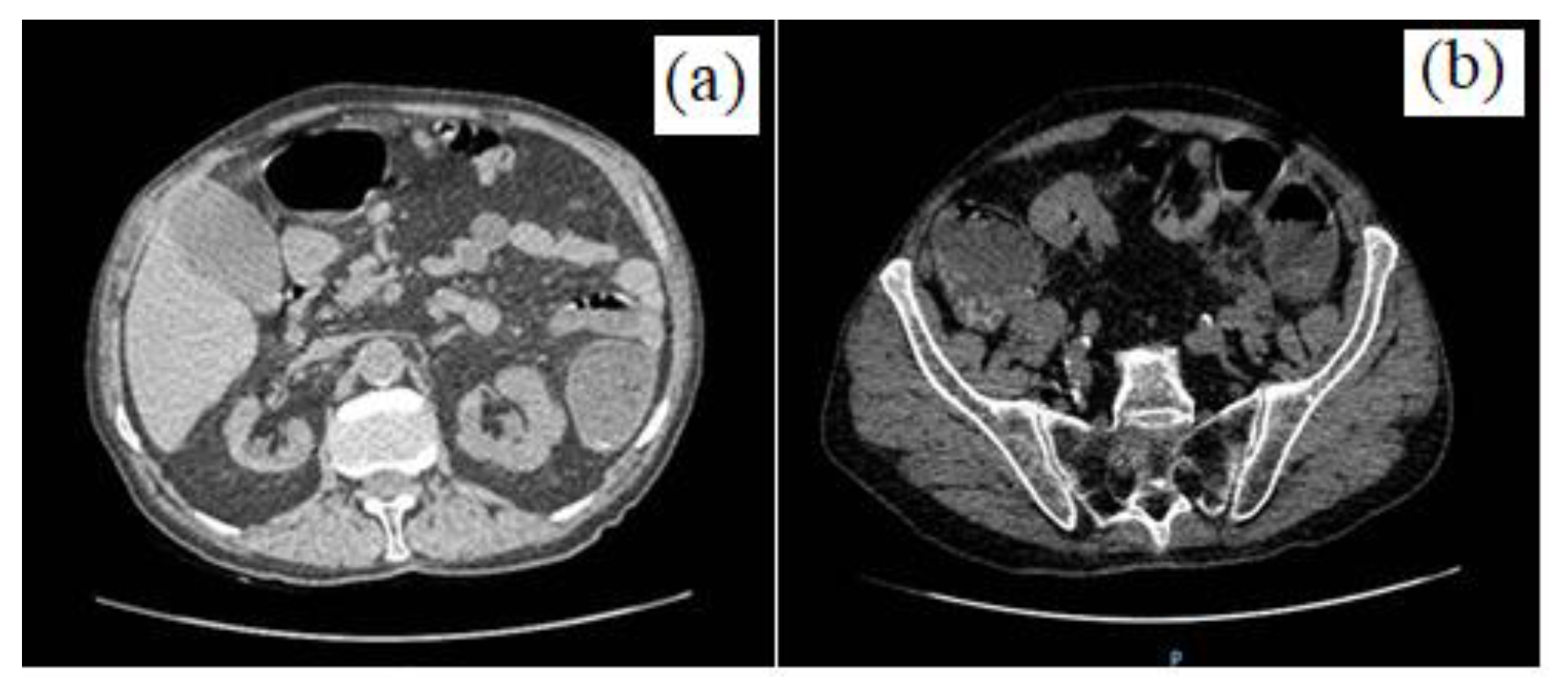
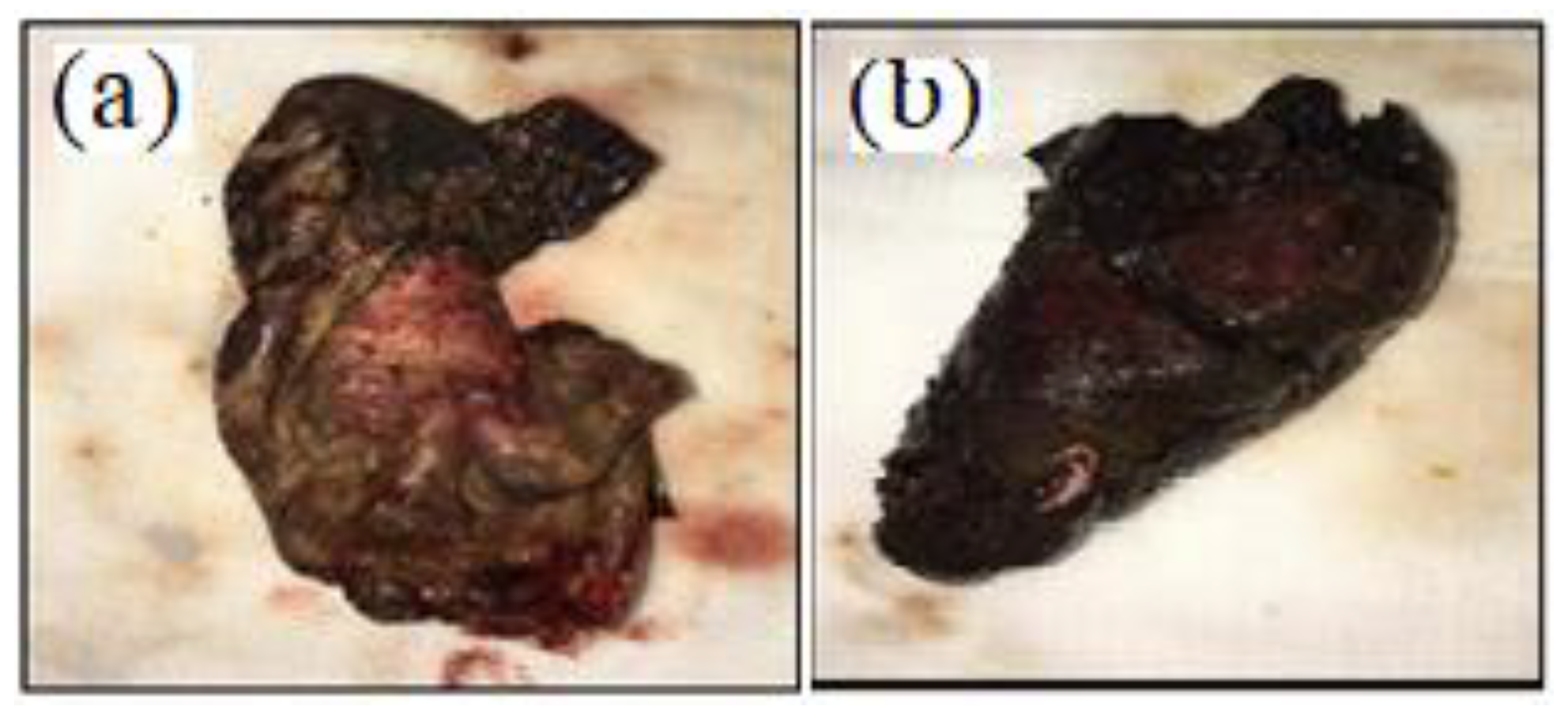
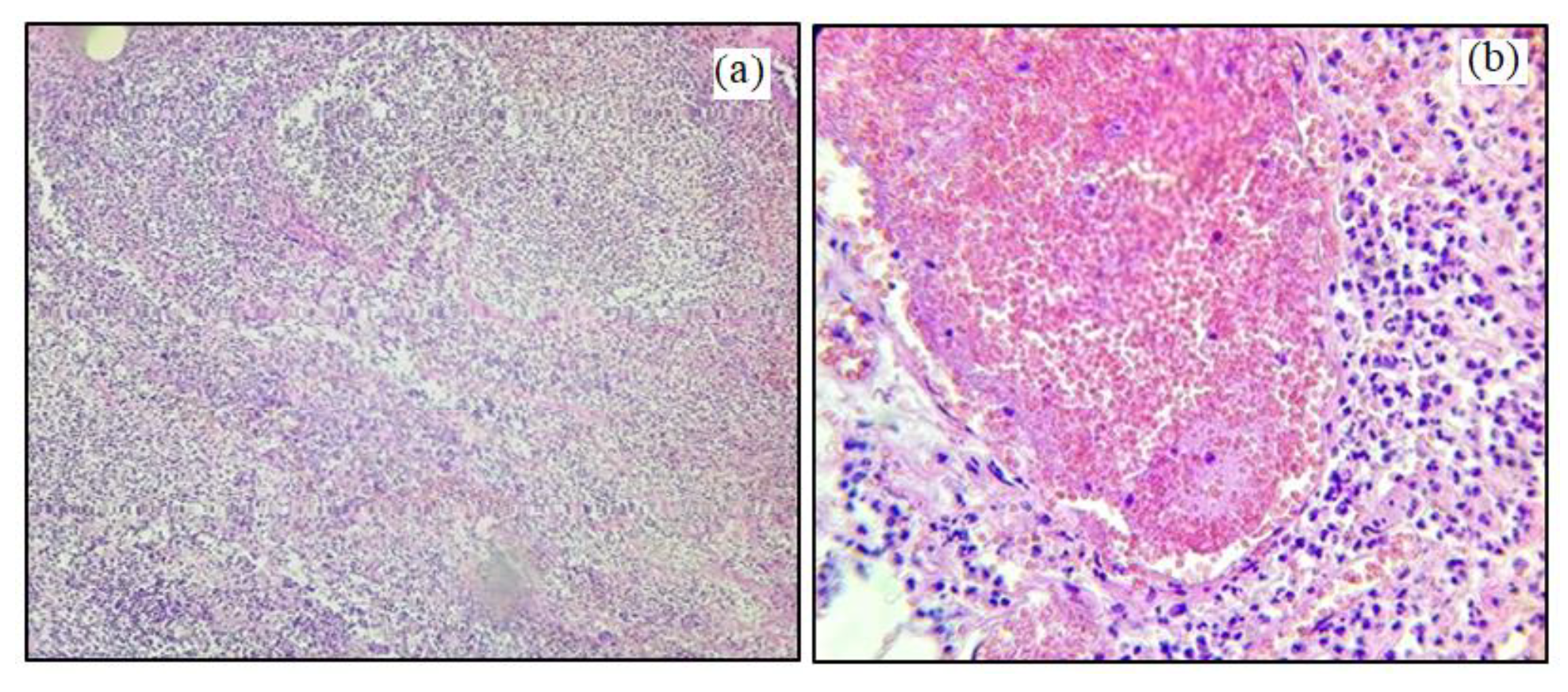
Case Presentation
Discussions
Highlights
- ✓
- SARS-Cov2 infection in an oncological patient changes the therapeutic approach not only in terms of anesthesia, but also of surgery, due to the resulting intraoperative and postoperative complications.
- ✓
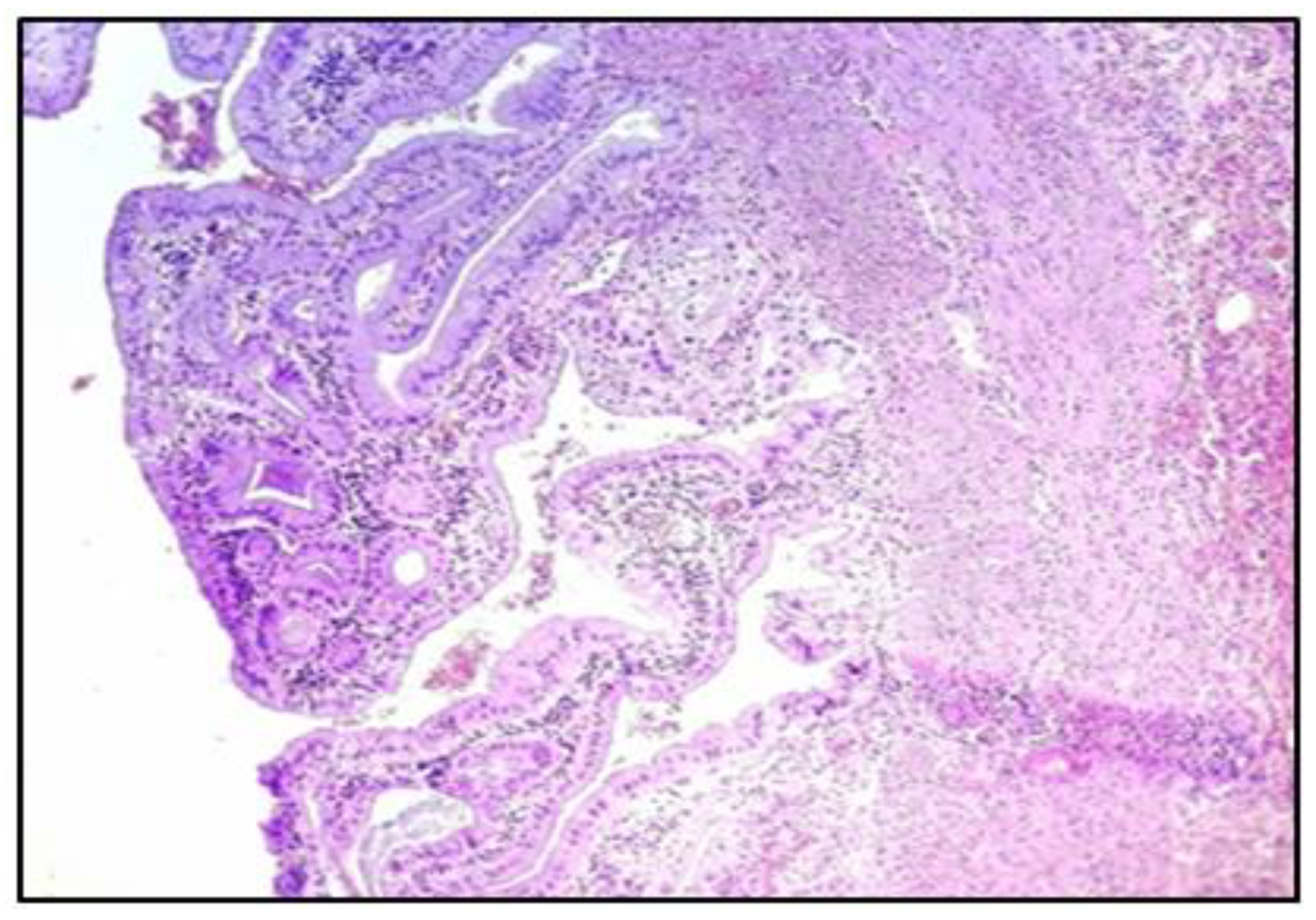
- The confirmation by histopathological examination of the existence of micro-thrombi in the gallbladder vasculature, with necrosis and its perforation, supports the recent studies that mention the occurrence of coagulation disorders in Covid-19-positive patients.
Conclusions
Conflicts of Interest disclosure
Compliance with ethical standards
References
- Coronaviridae Study Group of the International Committee on Taxonomy of Viruses. The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020, 5, 536–544. [Google Scholar] [CrossRef]
- Dascalu, A.M.; Tudosie, M.S.; Smarandache, G.C.; Serban, D. Impact of the Covid-19 pandemic upon the ophthalmological clinical practice. Rom J Leg Med. 2020, 28, 96–100. [Google Scholar] [CrossRef]
- Dhand, R.; Li, J. Coughs and Sneezes: Their Role in Transmission of Respiratory Viral Infections, Including SARS-CoV-2. Am J Respir Crit Care Med. 2020, 202, 651–659. [Google Scholar] [CrossRef] [PubMed]
- Serban, D.; Smarandache, C.G.; Tudor, C.; Duta, L.N.; Dascalu, A.M.; Aliuș, C. Laparoscopic Surgery in COVID-19 Era-Safety and Ethical Issues. Diagnostics (Basel). 2020, 10, 673. [Google Scholar] [CrossRef]
- Lauer, S.A.; Grantz, K.H.; Bi, Q.; Jones, F.K.; Zheng, Q.; Meredith, H.R.; Azman, A.S.; Reich, N.G.; Lessler, J. The Incubation Period of Coronavirus Disease 2019 (COVID-19) From Publicly Reported Confirmed Cases: Estimation and Application. Ann Intern Med. 2020, 172, 577–582. [Google Scholar] [CrossRef]
- Alene, M.; Yismaw, L.; Assemie, M.A.; Ketema, D.B.; Gietaneh, W.; Birhan, T.Y. Serial interval and incubation period of COVID-19: a systematic review and meta- analysis. BMC Infect Dis. 2021, 21, 257. [Google Scholar] [CrossRef]
- Yi, Y.; Lagniton, P.N.P.; Ye, S.; Li, E.; Xu, R.H. COVID-19: what has been learned and to be learned about the novel coronavirus disease. Int J Biol Sci. 2020, 16, 1753–1766. [Google Scholar] [CrossRef]
- Serban, D.; Socea, B.; Badiu, C.D.; Tudor, C.; Balasescu, S.A.; Dumitrescu, D.; Trotea, A.M.; Spataru, R.I.; Vancea, G.; Dascalu, A.M.; Tanasescu, C. Acute surgical abdomen during the COVID-19 pandemic: Clinical and therapeutic challenges. Exp Ther Med. 2021, 21, 519. [Google Scholar] [CrossRef]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y.; Xia, J.; Yu, T.; Zhang, X.; Zhang, L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020, 395, 507–513. [Google Scholar] [CrossRef]
- Mehta, P.; McAuley, D.F.; Brown, M.; Sanchez, E.; Tattersall, R.S.; Manson, J.J.; HLH Across Speciality Collaboration, UK. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020, 395, 1033–1034. [Google Scholar] [CrossRef]
- Lei, S.; Jiang, F.; Su, W.; Chen, C.; Chen, J.; Mei, W.; Zhan, L.Y.; Jia, Y.; Zhang, L.; Liu, D.; Xia, Z.Y.; Xia, Z. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine 2020, 21, 100331. [Google Scholar] [CrossRef] [PubMed]
- Thyagarajan, R.; Mondy, K. Timing of surgery after recovery from coronavirus disease 2019 (COVID-19) infection. Infect Control Hosp Epidemiol. 2021, 42, 790–791. [Google Scholar] [CrossRef] [PubMed]
- Serban, D.; Spataru, R.I.; Vancea, G.; Balasescu, S.A.; Socea, B.; Tudor, C.; Dascalu, A.M. Informed consent in all surgical specialties: from legal obligation to patient satisfaction. Rom J Leg Med. 2020, 28, 317–321. [Google Scholar] [CrossRef]
- Radu, N.; Voicescu, M.; Radu, E.; Tanasescu, C. Biomaterial with antioxidant and antifungal activities, obtained from Romanian indigenous plants. Molecular Crystals and Liquid Crystals. 2017, 655, 243–249. [Google Scholar] [CrossRef]
- Alius, C.; Tudor, C.; Badiu, C.D.; Dascalu, A.M.; Smarandache, C.G.; Sabau, A.D.; Tanasescu, C.; Balasescu, S.A.; Serban, D. Indocyanine Green-Enhanced Colorectal Surgery-between Being Superfluous and Being a Game-Changer. Diagnostics (Basel). 2020, 10, 742. [Google Scholar] [CrossRef]
- Suceveanu, A.I.; Pantea-Stoian, A.; Mazilu, L.; Voinea, F.; et al. Interferon-free therapy is not a trigger for hepatocellular carcinoma in patients with chronic infection with hepatitis C virus. Farmacia. 2018, 66, 904–908. [Google Scholar] [CrossRef]
- Tofolean, D.E.; Mazilu, L.; Stăniceanu, F.; Mocanu, L.; Suceveanu, A.I.; Baz, R.O.; Parepa, R.I.; Suceveanu, A.P.; Bondari, S.; Bondari, D.; Voinea, F. Clinical presentation of a patient with cutis laxa with systemic involvement: a case report. Rom J Morphol Embryol. 2015, 56, 1205–10. [Google Scholar]
- Serban, D.; Branescu, C.M.; Smarandache, C.G.; Tudor, C.; Tanasescu, C.; Tudosie, M.S.; Stana, D.; Comandasu, M.; Costea, D.O.; Dascalu, A.M. Safe surgery in Day Care Centers - Focus on preventing medico-legal issues. Rom J Leg Med. 2021, 29, 60–64. [Google Scholar] [CrossRef]
- Tănăsescu, C.; Faur, M.; Sabău, D. Day-case Surgery in the Context of Inguinal Hernia Repair by the Modified Lichtenstein Technique - A Single Centre Experience. Chirurgia (Bucur). 2019, 114, 115–120. [Google Scholar] [CrossRef]
- Cook, T.M. Combined spinal-epidural techniques. Anaesthesia. 2000, 55, 42–64. [Google Scholar] [CrossRef]
- Serban, D.; Socea, B.; Balasescu, S.A.; Badiu, C.D.; Tudor, C.; Dascalu, A.M.; Vancea, G.; Spataru, R.I.; Sabau, A.D.; Sabau, D.; Tanasescu, C. Safety of Laparoscopic Cholecystectomy for Acute Cholecystitis in the Elderly: A Multivariate Analysis of Risk Factors for Intra and Postoperative Complications. Medicina (Kaunas). 2021, 57, 230. [Google Scholar] [CrossRef]
- Dimitriu, M.C.T.; Pantea-Stoian, A.; Smaranda, A.C.; Nica, A.A.; Carap, A.C.; Constantin, V.D.; Davitoiu, A.M.; Cirstoveanu, C.; Bacalbasa, N.; Bratu, O.G.; Jacota-Alexe, F.; Badiu, C.D.; Smarandache, C.G.; Socea, B. Burnout syndrome in Romanian medical residents in time of the COVID-19 pandemic. Med Hypotheses 2020, 144, 109972. [Google Scholar] [CrossRef]
- Costea, D.O.; Enache, F.D.; Baz, R.; Suceveanu, A.P.; Suceveanu, A.I.; Ardeleanu, A.; Mazilu, L.; Costea, A.C.; Botea, F.; Voinea, F. Confirmed child patient with Covid-19 infection, operated for associated surgical pathology – first pediatric case in Romania. Rom Biotechnol Lett. 2020, 25, 2107–2110. [Google Scholar] [CrossRef]
- Tang, N.; Li, D.; Wang, X.; Sun, Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020, 18, 844–847. [Google Scholar] [CrossRef]
- Tang, N.; Bai, H.; Chen, X.; Gong, J.; Li, D.; Sun, Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020, 18, 1094–1099. [Google Scholar] [CrossRef]
- Tudosie, M.; Miulescu, R.; Negulescu, V.; Ionica, M.; Stefan, S.; Corlan, G.; Macovei, R. Evaluation and modeling of pharmacokinetics of copper ion during hemodialysis. Farmacia. 2013, 61, 53–65. [Google Scholar]
- Han, H.; Yang, L.; Liu, R.; Liu, F.; Wu, K.L.; Li, J.; Liu, X.H.; Zhu, C.L. Prominent changes in blood coagulation of patients with SARS-CoV-2 infection. Clin Chem Lab Med. 2020, 58, 1116–1120. [Google Scholar] [CrossRef]
- Radu, N.; Roman, V.; Tănăsescu, C. Biomaterials obtained from probiotic consortia of microorganisms. Potential applications in regenerative medicine. Molecular Crystals and Liquid Crystals. 2016, 628, 115–123. [Google Scholar] [CrossRef]
- Mazilu, L.; Katsiki, N.; Nikolouzakis, T.K.; Aslanidis, M.I.; Lazopoulos, G.; Kouretas, D.; Tsatsakis, A.; Suceveanu, A.I.; Stoian, A.P.; Parepa, I.R.; Voinea, F.; Suceveanu, A.P.; Arsene, A.L.; Velescu, B.Ș.; Vesa, C.; Nitipir, C. Thrombosis and Haemostasis challenges in COVID-19 - Therapeutic perspectives of heparin and tissue-type plasminogen activator and potential toxicological reactions-a mini review. Food Chem Toxicol 2021, 148, 111974. [Google Scholar] [CrossRef]
- Pantea Stoian, A.; Pricop-Jeckstadt, M.; Pana, A.; Ileanu, B.V.; Schitea, R.; Geanta, M.; Catrinoiu, D.; Suceveanu, A.I.; Serafinceanu, C.; Pituru, S.; Poiana, C.; Timar, B.; Nitipir, C.; Parvu, S.; Arsene, A.; Mazilu, L.; Toma, A.; Hainarosie, R.; Ceriello, A.; Rizzo, M.; Jinga, V. Death by SARS-CoV 2: a Romanian COVID-19 multi-centre comorbidity study. Sci Rep. 2020, 10, 21613. [Google Scholar] [CrossRef]
- Ciocirlan, M.; Draghia, L.; Manuc, D.; et al. Nutritional status of patients with digestive cancers. Conference: 3rd International Conference on Interdisciplinary Management of Diabetes Mellitus and its Complications (INTERDIAB) Location: Bucharest, ROMANIA Date: MAR 02-04,2017. Sponsor(s): Assoc Renal Metab & Nutrit Studies; AstraZeneca Diabetes; MSD Diabetes; novo nordisk; SANOFI.INTERDIAB 2017: DIABETES MELLITUS IN INTERNAL MEDICINE Book Series: International Conference on Interdisciplinary Management of Diabetes Mellitus and its Complications, 2017:132-138.
- Liu, Q.; Wang, R.S.; Qu, G.Q.; Wang, Y.Y.; Liu, P.; Zhu, Y.Z.; Fei, G.; Ren, L.; Zhou, Y.W.; Liu, L. Gross examination report of a COVID-19 death autopsy. Fa Yi Xue Za Zhi. 2020, 36, 21–23. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Shi, L.; Wang, Y.; Zhang, J.; Huang, L.; Zhang, C.; Liu, S.; Zhao, P.; Liu, H.; Zhu, L.; Tai, Y.; Bai, C.; Gao, T.; Song, J.; Xia, P.; Dong, J.; Zhao, J.; Wang, F.S. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020, 8, 420–422. [Google Scholar] [CrossRef] [PubMed]
- Vinayagam, S.; Sattu, K. SARS-CoV-2 and coagulation disorders in different organs. Life Sci 2020, 260, 118431. [Google Scholar] [CrossRef]
- Zhou, B.; Zhao, W.; Feng, R.; Zhang, X.; Li, X.; Zhou, Y.; Peng, L.; Li, Y.; Zhang, J.; Luo, J.; Li, L.; Wu, J.; Yang, C.; Wang, M.; Zhao, Y.; Wang, K.; Yu, H.; Peng, Q.; Jiang, N. The pathological autopsy of coronavirus disease 2019 (COVID-2019) in China: a review. Pathog Dis. 2020, 78, ftaa026. [Google Scholar] [CrossRef]
- Yao, X.H.; Li, T.Y.; He, Z.C.; Ping, Y.F.; Liu, H.W.; Yu, S.C.; Mou, H.M.; Wang, L.H.; Zhang, H.R.; Fu, W.J.; Luo, T.; Liu, F.; Guo, Q.N.; Chen, C.; Xiao, H.L.; Guo, H.T.; Lin, S.; Xiang, D.F.; Shi, Y.; Pan, G.Q.; Li, Q.R.; Huang, X.; Cui, Y.; Liu, X.Z.; Tang, W.; Pan, P.F.; Huang, X.Q.; Ding, Y.Q.; Bian, X.W. [A pathological report of three COVID-19 cases by minimal invasive autopsies]. Zhonghua Bing Li Xue Za Zhi. 2020, 49, 411–417. [Google Scholar] [CrossRef]
- Barton, L.M.; Duval, E.J.; Stroberg, E.; Ghosh, S.; Mukhopadhyay, S. COVID-19 Autopsies, Oklahoma, USA. Am J Clin Pathol. 2020, 153, 725–733. [Google Scholar] [CrossRef]

Share and Cite
Faur, M.; Moisin, A.; Mohor, C.; Sabau, D. A Rare Complication in a COVID-19 Positive Patient with Sigmoid Colon Cancer-Hemoperitoneum Due to Gallbladder Necrosis Following Micro-Thrombosis. J. Mind Med. Sci. 2021, 8, 317-323. https://doi.org/10.22543/7674.82.P317323
Faur M, Moisin A, Mohor C, Sabau D. A Rare Complication in a COVID-19 Positive Patient with Sigmoid Colon Cancer-Hemoperitoneum Due to Gallbladder Necrosis Following Micro-Thrombosis. Journal of Mind and Medical Sciences. 2021; 8(2):317-323. https://doi.org/10.22543/7674.82.P317323
Chicago/Turabian StyleFaur, Mihai, Andrei Moisin, Calin Mohor, and Dan Sabau. 2021. "A Rare Complication in a COVID-19 Positive Patient with Sigmoid Colon Cancer-Hemoperitoneum Due to Gallbladder Necrosis Following Micro-Thrombosis" Journal of Mind and Medical Sciences 8, no. 2: 317-323. https://doi.org/10.22543/7674.82.P317323
APA StyleFaur, M., Moisin, A., Mohor, C., & Sabau, D. (2021). A Rare Complication in a COVID-19 Positive Patient with Sigmoid Colon Cancer-Hemoperitoneum Due to Gallbladder Necrosis Following Micro-Thrombosis. Journal of Mind and Medical Sciences, 8(2), 317-323. https://doi.org/10.22543/7674.82.P317323


