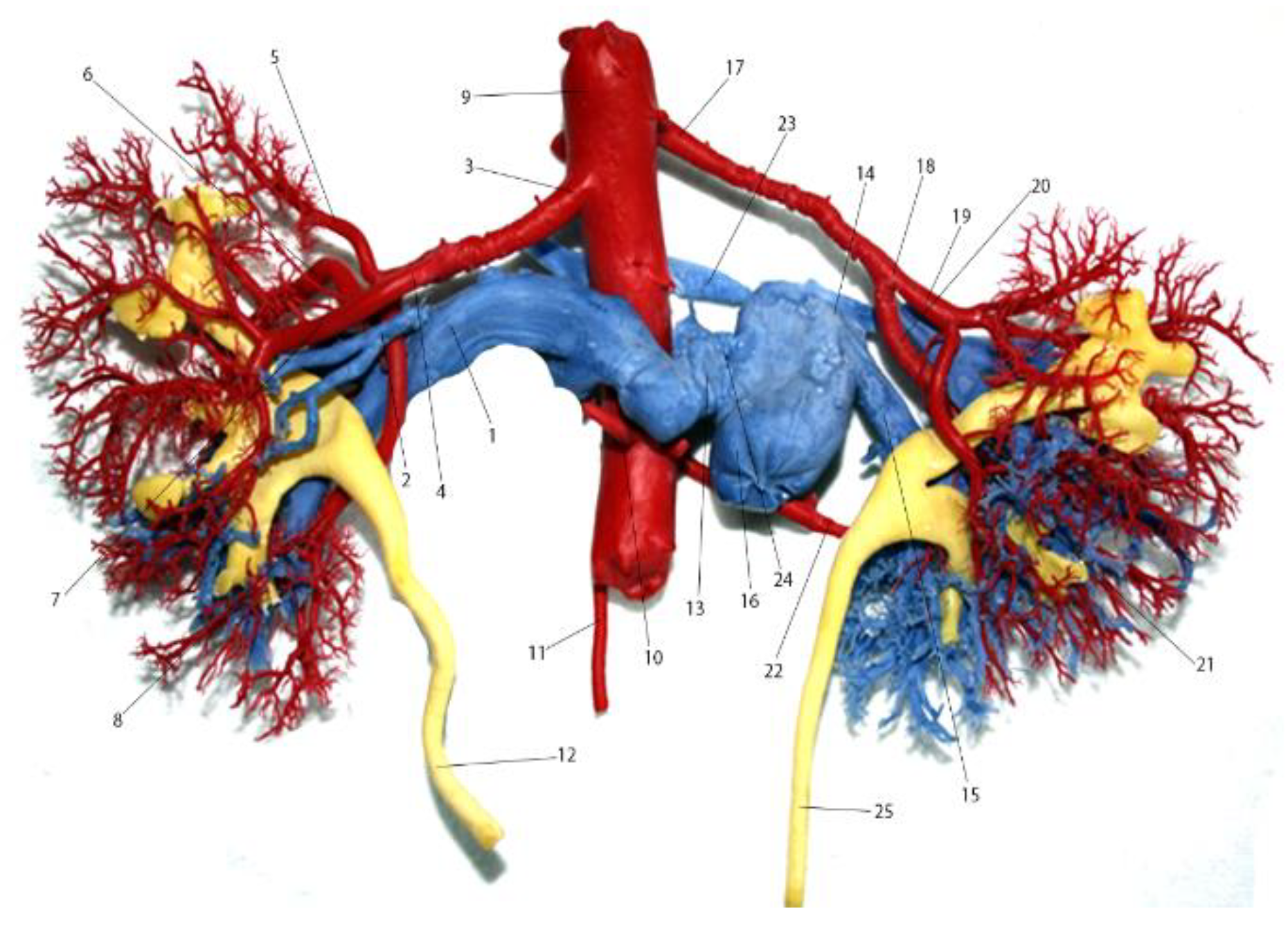
Periaortic Venous Necklace and Renal Right Double Arteries; Case Report
Abstract
Introduction
Case Presentation
Discussions
Highlights
- ✓
- The presence of the periaortic venous ring, depending on its size, can evolve asymptomatically if widened, being accidentally discovered at an angiographic examination or after death, at the necropsy examination.
- ✓
- When tightened, it can compress the aorta, which can cause adrenal aortic aneurysm, presenting the characteristic symptomatology.
Conclusions
Conflicts of Interest disclosure
Compliance with ethical standards
References
- Standring, S. Gray’s Anatomy. The Anatomical Basis of Clinical Practice. Ed. Elsevier, Churchill Livinngstone. Edinburgh. London. New York, 2015. ISBN 9780702068515.
- Ayaz, S.; Ayaz, Ü.Y. Detection of retroaortic left renal vein and circumaortic left renal vein by PET/CT images to avoid misdiagnosis and support possible surgical procedures. Hell J Nucl Med. 2016, 19, 135–9. [Google Scholar] [CrossRef] [PubMed]
- Karkos, C.D.; Bruce, I.A.; Thomson, G.J.; Lambert, M.E. Retroaortic left renal vein and its implications in abdominal aortic surgery. Ann Vasc Surg. 2001, 15, 703–8. [Google Scholar] [CrossRef] [PubMed]
- Ghandour, A.; Partovi, S.; Karuppasamy, K.; Rajiah, P. Congenital anomalies of the IVC-embryological perspective and clinical relevance. Cardiovasc Diagn Ther. 2016, 6, 482–492. [Google Scholar] [CrossRef] [PubMed]
- Trigaux, J.P.; Vandroogenbroek, S.; De Wispelaere, J.F.; Lacrosse, M.; Jamart, J. Congenital anomalies of the inferior vena cava and left renal vein: evaluation with spiral CT. J Vasc Interv Radiol. 1998, 9, 339–45. [Google Scholar] [CrossRef] [PubMed]
- Chircor, L.; Surdu, L. Morphogenesis of the inferior cav system. In: Human Embryology. Ed. Ex Ponto. Constanţa, 2014; 416–417ISBN 978-606-598-355-7. [Google Scholar]
- Chen, R.Y.; Chang, H. Renal dysplasia. Arch Pathol Lab Med. 2015, 139, 547–51. [Google Scholar] [CrossRef] [PubMed]
- Date, Y.; Takano, T.; Fujii, T.; Terasaki, T.; Sakaguchi, M. Double D Technique: An Innovative Modified Bifurcated Stent Graft Deployment Strategy for an Isolated Common Iliac Artery Aneurysm With a Challenging Renal Artery Anatomy. Vasc Endovascular Surg. 2019, 53, 613–616. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, K.; Miyajima, A.; Fukumoto, K.; Komatsuda, A.; Niwa, N.; Hattori, S.; Takeda, T.; Kikuchi, E.; Asanuma, H.; Oya, M. Factors influencing the operating time for single-port laparoscopic radical nephrectomy: focus on the anatomy and distribution of the renal artery and vein. Jpn J Clin Oncol. 2017, 47, 976–980. [Google Scholar] [CrossRef] [PubMed]
- Bordei, P.; Sapte, E.; Iliescu, D. Double renal arteries originating from the aorta. Surg Radiol Anat. 2004, 26, 474–9. [Google Scholar] [CrossRef] [PubMed]
- Mir, N.S.; Ul Hassan, A.; Rangrez, R.; Hamid, S.; Sabia, Tabish, S. A.; Iqbal, Suhaila, Masarat, Rasool, Z. Bilateral Duplication of Renal Vessels: Anatomical, Medical and Surgical perspective. Int J Health Sci (Qassim). 2008, 2, 179–85. [Google Scholar] [PubMed]
- Yokuş, A.; Toprak, N.; Gündüz, A.M.; Akdeniz, H.; Akdemir, Z.; Dündar, İ.; Arslan, H. Anterior Cerebral Artery and Anterior Communicating Artery Variations: Assessment with Magnetic Resonance Angiography. World Neurosurg. 2021, 155, e203–e209. [Google Scholar] [CrossRef] [PubMed]
- Regmi, P.R.; Amatya, I.; Kayastha, P.; Paudel, S.; Suwal, S.; Ghimire, R.K. Normal Anatomy and Variants of Renal Vasculature with Multidetector Computed Tomography in a Tertiary Care Hospital: A Descriptive Cross-sectional Study. JNMA J Nepal Med Assoc. 2020, 58, 911–914. [Google Scholar] [CrossRef] [PubMed]
- Resende, F.C.; Avelar, G.F. The sexual segment of the kidney of a tropical rattlesnake, Crotalus durissus (Reptilia, Squamata, Viperidae), and its relationship to seasonal testicular and androgen cycles. J Morphol. 2021, 282, 1402–1414. [Google Scholar] [CrossRef] [PubMed]
- Cordier, G.; Nguyen-Huu, B.M.H.S. Segmenttion Arterielle du rein [Arterial segmentation of the kidney]. Presse Med. 1964, 72, 2433–2438. [Google Scholar]
- Spinu Arsenie, D.; Bratu, O.G.; Marcu, D.R.; Stanciu, A.E.; Gherghiceanu, F.; Ionita-Radu, F.; Bungau, S.; Stanescu, A.M.A.; Mischianu, D. Underactive bladder - an underestimated entity. J Mind Med Sci. 2020, 7, 23–28. [Google Scholar] [CrossRef]
- Jun, K.W.; Cho, J.; Kim, M.H.; Hwang, J.K.; Park, S.C.; Moon, I.S.; Kim, J.I. Changes in hemostatic factors after kidney transplantation: A retrospective cohort study. Medicine (Baltimore). 2021, 100, e27179. [Google Scholar] [CrossRef] [PubMed]
- Singh, G.; Jolly, N. Peripheral Vascular Disease Involving Transplant Renal Artery. J Invasive Cardiol. 2021, 7, 257–260. [Google Scholar] [CrossRef]
- Onisâi, M.C.; Iordan, I.; Gaman, M.; Bumbea, H.; Vlădăreanu, A.M. Unexpected hope for a multiple myeloma patient. J Mind Med Sci. 2020, 7, 257–260. [Google Scholar] [CrossRef]
- Elian, V.; Cioca, G.; Pantea, A.S.; et al. Metabolic syndrome and chronic kidney disease: pathogenic, clinical, and therapeutic correlations. 1st International Conference on Interdisciplinary Management of Diabetes Mellitus and its Complications (INTERDIAB). Interdisciplinary approaches in diabetic chronic kidney disease. 2015, pp. 48–52.
- Ardeleanu, V.; Georgescu, C.; Frîncu, L.D.; Frâncu, L.L.; Vesa, D. Angiogenesis as Prospective Molecular Biology Technique for Cancer Study. Romanian Biotehnological Letters. 2014, 19, 9637–9648. [Google Scholar]
- Motofei, I.G.; Rowland, D.L.; Georgescu, S.R.; Tampa, M.; Paunica, S.; Constantin, V.D.; Balalau, C.; Manea, M.; Baleanu, B.C.; Sinescu, I. Post-Finasteride Adverse Effects in Male Androgenic Alopecia: A Case Report of Vitiligo. Skin Pharmacol Physiol. 2017, 30, 42–45. [Google Scholar] [CrossRef] [PubMed]
- Ardeleanu, V.; Francu, L.; Georgescu, C. Neoangiogenesis. Assessment in Esophageal Adenocarcinomas. Indian J Surg. 2015, 77 (Suppl 3), 971–976. [Google Scholar] [CrossRef] [PubMed][Green Version]

Share and Cite
Bordei, P.; Rusali, C.A.; Ionescu, C.; Serban, D.; Ardeleanu, V. Periaortic Venous Necklace and Renal Right Double Arteries; Case Report. J. Mind Med. Sci. 2021, 8, 312-316. https://doi.org/10.22543/7674.82.P312316
Bordei P, Rusali CA, Ionescu C, Serban D, Ardeleanu V. Periaortic Venous Necklace and Renal Right Double Arteries; Case Report. Journal of Mind and Medical Sciences. 2021; 8(2):312-316. https://doi.org/10.22543/7674.82.P312316
Chicago/Turabian StyleBordei, Petru, Constantin Andrei Rusali, Constantin Ionescu, Dragos Serban, and Valeriu Ardeleanu. 2021. "Periaortic Venous Necklace and Renal Right Double Arteries; Case Report" Journal of Mind and Medical Sciences 8, no. 2: 312-316. https://doi.org/10.22543/7674.82.P312316
APA StyleBordei, P., Rusali, C. A., Ionescu, C., Serban, D., & Ardeleanu, V. (2021). Periaortic Venous Necklace and Renal Right Double Arteries; Case Report. Journal of Mind and Medical Sciences, 8(2), 312-316. https://doi.org/10.22543/7674.82.P312316


