Highlights
- Premedication should be administered before the electroconvulsive therapy.
- Premedication may prevent hemodynamic responses that may occur as a response to this therapy. It also prevents the occurrence of side effects.
Highlights
- Premedication should be administered before the electroconvulsive therapy
- Premedication may prevent hemodynamic responses that may occur as a response to this therapy. It also prevents the occurrence of side effects.
Abstract
Objective: The aim of this study was to examine the effects of anesthetic agents used as premedication in patients undergoing electroconvulsive therapy (ECT) for diagnoses of bipolar disorder or major depression in terms of convulsion, recovery period, and hemodynamic parameters. Materials and Method: This retrospective study was carried out by screening the anesthesia forms of patients in a psychiatry clinic in Turkey. Results: Researchers reviewed 104 patient files, of which 39 fit the inclusion criteria. 26 patients were given premedication; 13 patients were not given premedication. The study found a significant difference between the group to which dexmedetomidine was given and the non-premedication group in terms of mean arterial blood pressure and heart rate. A significant difference was also found between the group to which midazolam was given and the non-premedication group in terms of peripheral oxygen saturation. Conclusion: Premedication before ECT may be used to reduce the side effects after ECT without affecting convulsions and the recovery period.
Introduction
Intravenous anesthetic agents such as short-acting midazolam and propofol are widely used to provide anesthesia in ECT applications [1]. Ideal hypnotic medications used in ECT as anesthetics should have short half-lives, should not affect the onset/attack period and the quality, and should not disturb the hemodynamic balance. However, these anesthetic medications used for induction shorten the convulsion period and lengthen the recovery period, and also cause changes in hemodynamic parameters [2,3].
Constituting sufficient convulsion for an effective ECT enables the occurrence of the desired therapeutic effect. The motor attack period should continue for approximately 20-30 seconds to achieve a successful clinical result. If the attack period is shorter than 15 seconds or longer than 120 seconds, the ECT will be ineffective. One of the factors affecting this result is the anesthetic medication used. These medications may shorten the attack period by increasing the attack threshold based on the medication dose [2,3].
Although there have been no notifications about side effect occurrence in patients to whom ECT has been applied when dexmedetomidine and midazolam have been given, the number of studies examining these two sedative medications is low. A study by Mızrak et al. [4] indicated that low-dose dexmedetomidine given as premedication may be a beneficial alternative to midazolam. Several studies have reported that dexmedetomidine increases the attack period, while others have reported no effect on the attack period [5,6]. Various studies have shown that midazolam, which is an anticonvulsive agent in the benzodiazepine group and which decreases the hemodynamic response, prominently increases the attack period when used in ECT induction. However, studies that demonstrate an effect of midazolam applied in low doses as premedication on the attack period have been lacking [3,7].
This study assessed the effects of anesthetic agents used as premedication for patients undergoing ECT for diagnoses of bipolar disorder or major depression in terms of convulsion, recovery period, and hemodynamic parameters.
Materials and Methods
This study was carried out at the psychiatry service of a training and research hospital by reviewing the files of patients to whom ECT was applied within a six-month period after the necessary approvals from the local ethical committee (Decision No: 2725, Meeting Date: June 6, 2012) and from the institution were obtained. The researchers reviewed the follow-up forms of 18-65-year-old patients who were categorized as physical status 1 and 2 by the American Society of Anesthesiologists (ASA), who were diagnosed with bipolar disorder or major depression, and who underwent three sessions of ECT. Patients with ischemic heart disease, arrhythmia, hypertension, or epilepsy, or who were pregnant, used beta blockers, or were allergic to any medications, were not included in the study.
The population considered for the study consisted of 104 patients to whom ECT was given within a six-month period. Of these, 39 fit the inclusion criteria and thus were included. 26 patients had been given either dexmedetomidine (n = 13) or midazolam (n = 13), and no premedication occurred in another 13. In terms of premedication, 0.025 mg/kg IV midazolam or 0.5 μg/kg IV dexmedetomidine were administered by infusion. For the general anesthesia, a 4 mg/kg dose of thiopental and a 1 mg/kg dose of succinylcholine were administered intravenously to all patients regardless of whether dexmedetomidine, midazolam, or no premedication had been previously administered.
Researchers used a sub-structured questionnaire in which features related to descriptive characteristics, ECT side effects, and hemodynamic parameters of participants were recorded.
- ○
- Questionnaire related to the descriptive characteristics of participants: This questionnaire included questions about the age, sex, height, weight, and the diagnosis of participants.
- ○
- Questionnaire related to ECT side effects and hemodynamic parameters: Data for this questionnaire were obtained from patient files and were related to (1) the current amount given (in joules), (2) the mean arterial blood pressure (MAP), (3) heart rate (HR) and peripheral oxygen saturation (SpO2) values, (4) the recovery period, (4) the convulsion period, and (5) the side effects that occurred.
Data were analyzed using the Statistical Package for Social Sciences (SPSS Inc., Chicago, IL., USA) 15.0 program. The mean ± standard deviation and frequency analysis were used for descriptive statistics. The Kruskal-Wallis test was used for inter-group comparisons of continuous variables. Bonferroni corrections for Mann-Whitney U tests were used for advanced binary comparisons. Significant p values were set at < 0.05.
Results
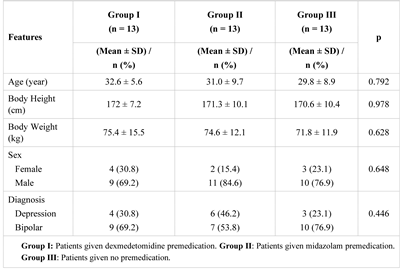
Table 1 presents the descriptive characteristics of the participants.

Table 1.
Comparison of the descriptive characteristics of the participants
The study found that dexmedetomidine was used in 13 patients in Group I, and midazolam was used in 13 patients in Group II as premedication, and no premedication was used in 13 patients in Group III.
No statistically significant difference between the groups were found in terms of age, height, weight, sex, or disease diagnosis.
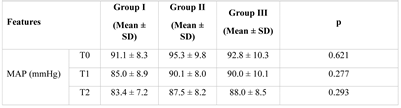
Table 2 presents group comparisons of hemodynamic parameters, convulsion, and recovery periods. A statistically significant difference was found between the 5th, 10th, and 15th minute after ECT in terms of MAP; between the 5th and 10th minute after ECT in terms of HR; and at the 10th minute after the premedication was given in terms of SpO2 value. Further analysis found that the difference between MAP and HR occurs across Groups I and III (p < 0.017), and the difference in SpO2 occurs across Groups II and III (p = 0.008). No statistically significant difference was found between groups in terms of recovery and convulsion periods (p > 0.05).

Table 2.
Comparison of patients in terms of hemodynamic parameters, convulsion, and recovery period
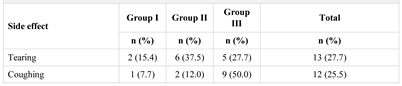
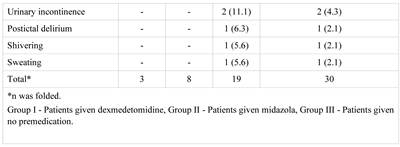
Table 3 shows the side effects noticed in the patients. The patients in Groups I, II, and III showed two, three, and five side effects, respectively. The most frequent side effects were tearing in Groups I and II and coughing in Group III.

Table 3.
Side effects noticed in patients
Discussions
This study found a statistically significant difference between the dexmedetomidine group and the no premedication group in terms of MAP and HR. The incidence of side effects in patients given no premedication was higher than that in patients given premedication.
Dexmedetomidine is an α2-adrenergic agonist which can be used with other intravenous anesthetic medications in various surgical fields. The use of dexmedetomidine in ECT may decrease hemodynamic responses [8,9,10]. Previous studies have shown that MAP and HR decreased in patients to whom ECT was administered [5,11,12]. The results of the present study show similar results.
Anesthetic agents used in ECT are desirable as they decrease the recovery period [13]. The effect of dexmedetomidine and midazolam on the recovery period is controversial in the research literature. Some studies have found that dexmedetomidine and midazolam increase the recovery period [14]; however, other studies have found that they have no effect on the recovery period [4,11]. The present study found no significant difference in terms of the recovery period between patients to whom dexmedetomidine and midazolam were administered as premedication and patients to whom no premedication was administered.
Although the therapeutic action of ECT is not fully understood, the attack period is one of the more significant indicators related to the efficacy of the therapy [15]. The recommended convulsion period is 25 seconds for effective ECT. Recent studies have reported that the healing efficiency of convulsions that continue for less than 15 seconds is decreased [5]. A study by Mızrak et al. [4] found that the convulsion periods in patients to whom dexmedetomidine was administered were longer than those of patients who were administered either midazolam or no premedication. A study by Loimer et al. [16] reported that midazolam shortened the attack period. According to the above-mentioned study by Mızrak et al. [4], dexmedetomidine may increase the attack period by allowing better convulsion activity than midazolam. The results of this study found that the attack periods in dexmedetomidine patients were longer than in midazolam patients. However, this difference was not statistically significant. This non-significant difference may have resulted from the use of barbiturates, which are known to decrease the attack activity when used as the induction agents in ECT.
A statistically significant difference was found between midazolam patients and non-premedication in terms of SpO2 value at the 10th minute after the premedication. This effect may have resulted from midazolam suppressing the respiration center by decreasing oxygen consumption and cerebral circulation, based on the medication dose [17]. Although side effects such as coughing, headache, postictal delirium, bradycardia, or hypertension due either to ECT or to the anesthetic agents used were observed in patients in a previous study, most of the patients had good prognoses and recovered on their own [18]. Decreasing possible side effects that may occur in patients, and waking patients up in a comfortable way, are the aims of premedication administered before ECT [19]. Mızrak et al. [4] reported that 4 patients developed coughing, and 5 developed headaches among dexmedetomidine patients. 2 patients developed coughing and 6 developed headaches among midazolam patients [4]. In the present study, only coughing and tearing occurred as side effects in premedication patients. In contrast, coughing, tearing, urinary incontinence, sweating, shivering, and postictal delirium occurred as side effects in patients given no premedication.
Conclusions
Midazolam or dexmedetomidine administered as premedication before ECT may prevent acute hemodynamic responses that may occur as a response to this therapy. Therefore, premedication administration may be beneficial in reducing the side effects that occur after ECT without affecting either the convulsion or the recovery periods.
Conflict of interest disclosure
There are no known conflicts of interest in the publication of this article. The manuscript was read and approved by all authors.
Compliance with ethical standards
Any aspect of the work covered in this manuscript has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript.
References
- Algül, A.; Şen, H.; Ateş, M.A.; Yen, T.; Durmaz, O.; Özkan, S.; Başoğlu, C.; Semiz, Ü.B.; Ebrinç, S.; Dağlı, G.; Çetin, M. Propofol versus propofol-remifentanil combination anaesthesia in electroconvulsive therapy: Effects on seizure duration and hemodynamics. Bulletin of Clinical Psychopharmacology. 2009, 19, 24–28. [Google Scholar]
- Folk, J.W.; Kellner, C.H.; Beale, M.D.; Conroy, J.M.; Duc, T.A. Anesthesia for electroconvulsive therapy: a review. J ECT. 2000, 16, 157–170. [Google Scholar] [CrossRef] [PubMed]
- Ding, Z.; White, P.F. Anesthesia for electroconvulsive therapy. Anesth Analg. 2002, 94, 1351–1364. [Google Scholar] [CrossRef] [PubMed]
- Mizrak, A.; Koruk, S.; Ganidagli, S.; Bulut, M.; Oner, U. Premedication with dexmedetomidine and midazolam attenuates agitation after electroconvulsive therapy. J Anaesth. 2009, 23, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Begeç, Z.; Köroğlu, A.; Gedik, E.; Yücel, A.; Toprak, H.I.; Karlıdağ, R.; Ersoy, M.Ö. Retrospective evaluation of our anesthetic applications for electroconvulsive therapy. Turk J Anaesthesiol Reanim 2008, 36, 238–243. [Google Scholar]
- Aydogan, M.S.; Yücel, A.; Begec, Z.; Colak, Y.Z.; Durmus, M. The hemodynamic effects of dexmedetomidine and esmolol in electroconvulsive therapy: a retrospective comparison. J ECT. 2013, 29, 308–311. [Google Scholar] [CrossRef] [PubMed]
- Shah, P.J.; Dubey, K.P.; Watti, C.; Lalwani, J. Effectiveness of thiopentone, propofol and midazolam as an ideal intravenous anaesthetic agent for modified electroconvulsive therapy: A comparative study. Indian J Anaesth. 2010, 54, 296–301. [Google Scholar] [CrossRef] [PubMed]
- Le Bot, A.; Michelet, D.; Hilly, J.; Maesani, M.; Dilly, M.P.; Brasher, C.; Mantz, J.; Dahmani, S. Efficacy of intraoperative dexmedetomidine compared with placebo for surgery in adults: a meta-analysis of published studies. Minerva Anestesiol. 2015, 81, 1105–1117. [Google Scholar] [PubMed]
- Arain, S.R.; Ebert, T.J. The efficacy, side effects, and recovery characteristics of dexmedetomidine versus propofol when used for intraoperative sedation. Anesth Analg. 2002, 95, 461–466, table of contents. [Google Scholar] [CrossRef] [PubMed]
- Ozkose, Z.; Demir, F.S.; Pampal, K.; Yardim, S. Hemodynamic and anesthetic advantages of dexmedetomidine, an alpha 2-agonist, for surgery in prone position. Tohoku J Exp Med. 2006, 210, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Begec, Z.; Toprak, H.I.; Demirbilek, S.; Erdil, F.; Onal, D.; Ersoy, M.O. Deksmedetomidine blunts acute hyperdynamic to responses Electroconvulsive therapy without altering seizure duration. Acta Anaesthesiol Scand. 2008, 52, 302–306. [Google Scholar] [CrossRef] [PubMed]
- Fu, W.; Stool, L.A.; White, P.F.; Husain, M.M. Is oral clonidine effective in modifying the acute hemodynamic response during electroconvulsive therapy? Anesth Analg. 1998, 86, 1127–1130. [Google Scholar] [PubMed]
- Surve, R.; Bansal, S.; Sriganesh, K.; Subbakrishna, D.K.; Thirthalli, J.; Umamaheswara Rao, G.S. Incidence and risk factors for oxygen desaturation during recovery from modified electroconvulsive therapy: a prospective observational study. J Anaesthesiol Clin Pharmacol. 2015, 31, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Moshiri, E.; Modir, H.; Bagheri, N.; Mohammadbeigi, A.; Jamilian, H.; Eshrati, B. Premedication effect of dexmedetomidine and alfentanil on seizure time, recovery duration, and hemodynamic responses in electroconvulsive therapy. Ann Card Anaesth. 2016, 19, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Fink, M. What is an adequate treatment in convulsive therapy? Acta Psychiatr Scand. 1991, 84, 424–427. [Google Scholar] [CrossRef] [PubMed]
- Loimer, N.; Hofmann, P.; Chaudhry, H.R. Midazolam shortens seizure duration following electroconvulsive therapy. J Psychiatr Res. 1992, 26, 97–101. [Google Scholar] [CrossRef] [PubMed]
- Wong, H.Y.; Fragen, R.J.; Dunn, K. Dose-finding study of intramuscular midazolam preanesthetic medication in the elderly. Anesthesiology. 1991, 74, 675–679. [Google Scholar] [CrossRef] [PubMed]
- Lisanby, S.H.; Morales, O.; Payne, N.; Kwon, E.; Fitzsimons, L.; Luber, B.; Nobler, M.S.; Sackeim, H.A. New developments in electroconvulsive therapy and magnetic seizure therapy. CNS Spectr. 2003, 8, 529–536. [Google Scholar] [CrossRef]
- Collins Vincent, J. Principles of anesthesiology: general and regional anesthesia. Lea & Febiger, Philadelphia, 3th ed.; 1993. [Google Scholar]
© 2019 by the author. 2019 Volkan Ozen, Mehmet Emin Orhan