LARS-like Symptoms in the General Population May Suggest the Significance of Postoperative Functional Problems and Emotional Implications of Rectal Surgery
Highlights
- LARS-like symptoms (with important psycho-emotional impact on the affected persons) may also be present in normal healthy population.
- Clinicians should thus estimate to what extent the observed LARS-like symptoms affect the individual before and after treatment.
Highlights
- LARS-like symptoms (with important psycho-emotional impact on the affected persons) may also be present in normal healthy population.
- Clinicians should thus estimate to what extent the observed LARS-like symptoms affect the individual before and after treatment.
Abstract
Introduction
Materials and Methods
The LARS score and sociodemographic variables
Statistical analysis
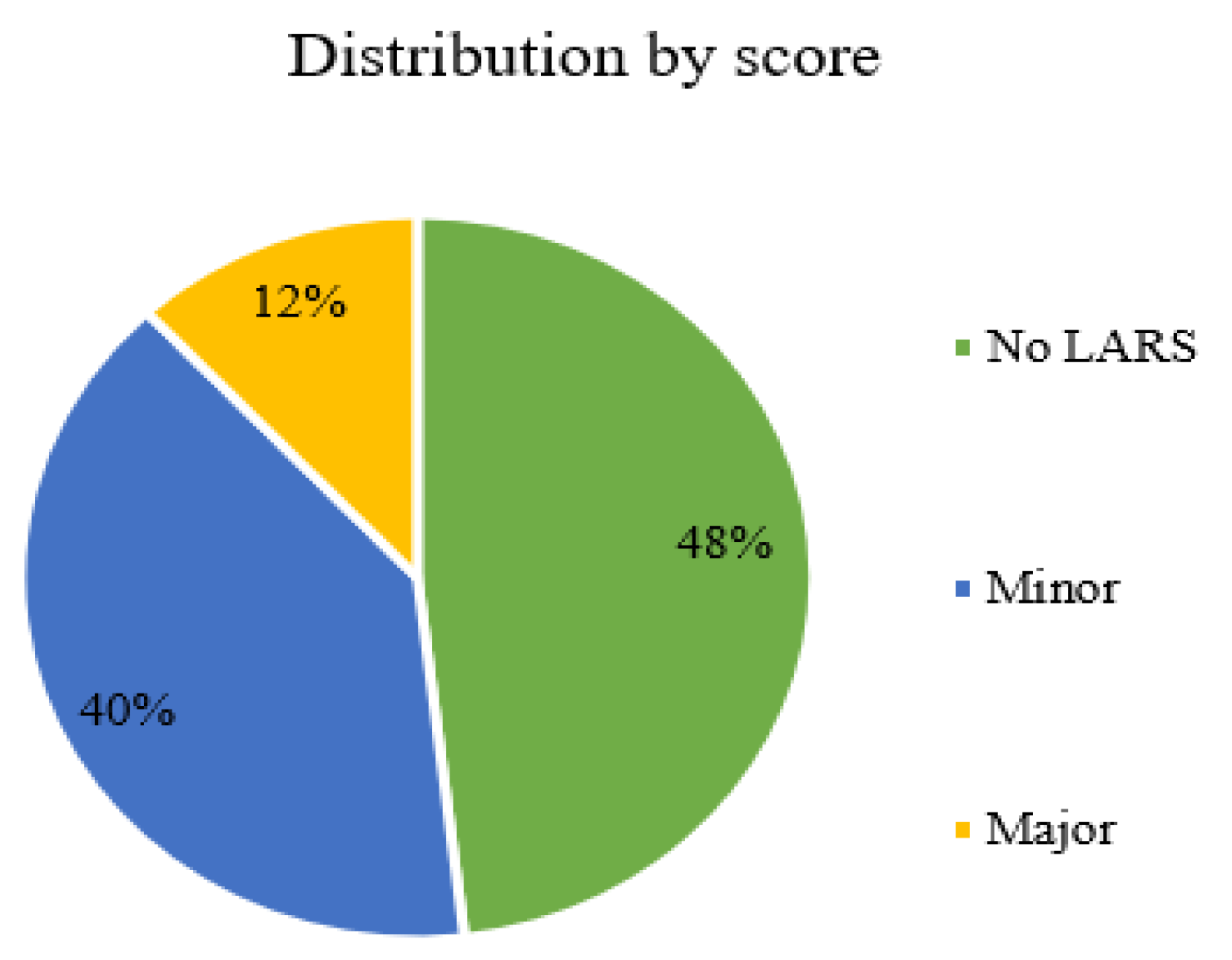
Results
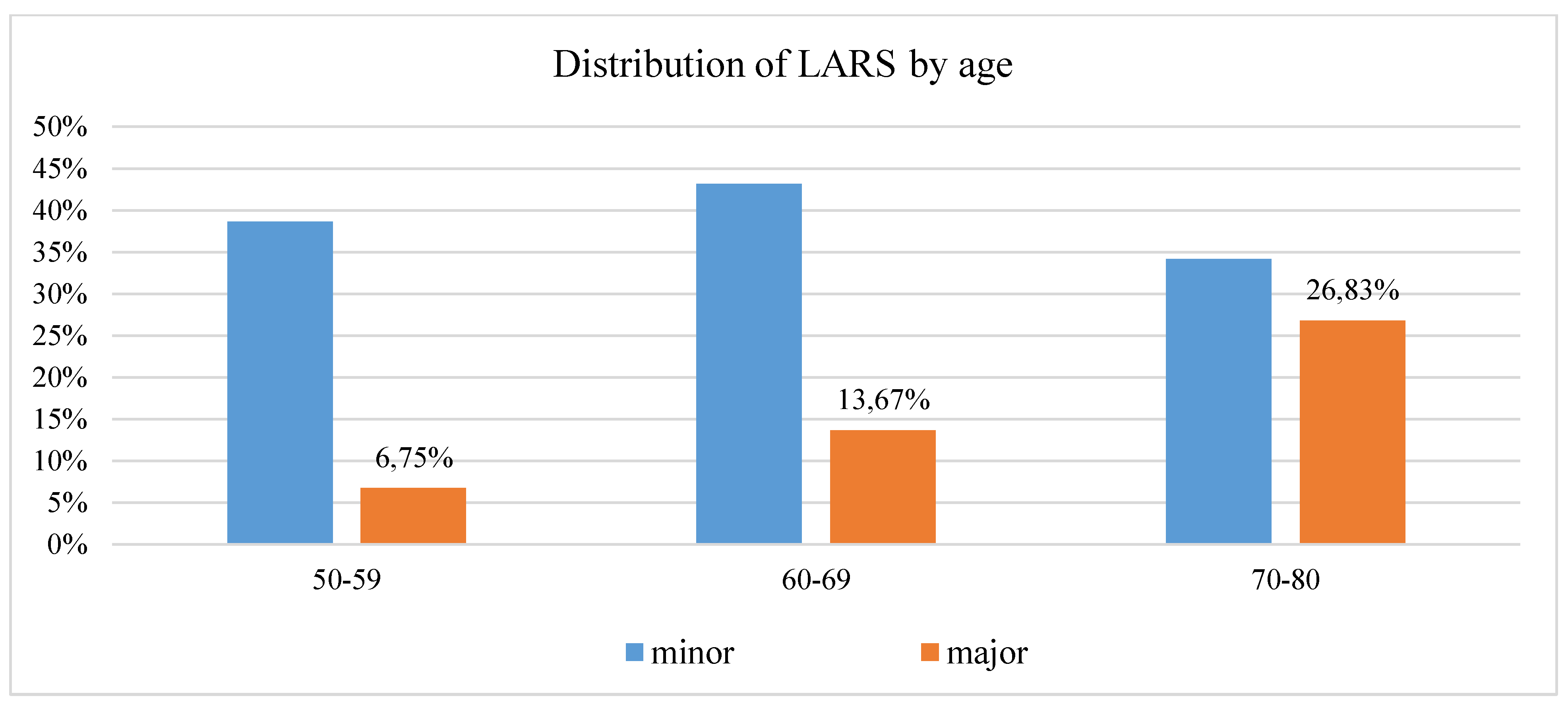
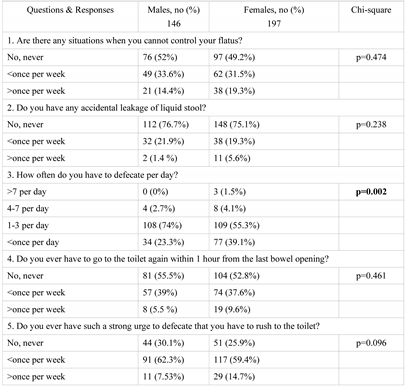
Characteristics of the responders and responses
Correlations of associated symptoms
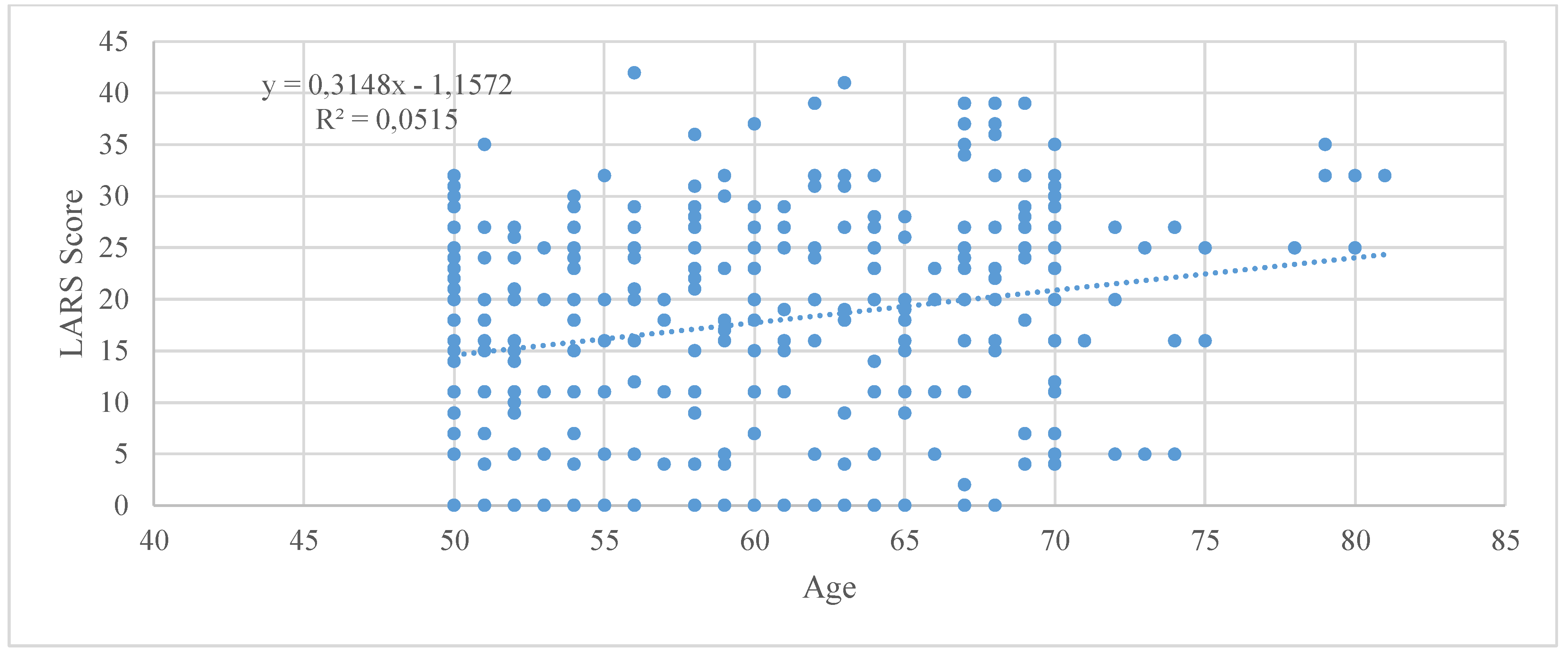
Factors associated with a higher LARS Score
Discussions
Social backgrounds and cultural influences
Conclusions
Conflict of interest disclosure
Compliance with ethical standards
References
- Bryant, C.; Lunniss, P.; Knowles, C.; Thaha, M.; Chan, C. Anterior resection syndrome. Lancet Oncol. 2012, 13, 403–408. [Google Scholar] [CrossRef] [PubMed]
- Lunniss, P.J.; Gladman, M.A.; Benninga, M.A.; Rao, S.S. Pathophysiology of evacuation disorders. Neurogastroenterol Motil. 2009, 21 (suppl 2), 31–40. [Google Scholar] [CrossRef] [PubMed]
- Pachler, J.; Wille-Jorgensen, P. Quality of life after rectal resection for cancer, with or without permanent colostomy. Cochrane Database Syst Rev. 2005, 2, CD004323. [Google Scholar]
- Pares, D.; Vial, M.; Bohle, B. Prevalence of faecal incontinence and analysis of its impact on quality of life and mental health. Colorectal Dis. 2011, 13, 899–905. [Google Scholar] [CrossRef] [PubMed]
- Irvine, E.J.; Ferrazzi, S.; Pare, P.; Thompson, W.G.; Rance, L. Health-related quality of life in functional GI disorders: focus on constipation and resource utilization. Am J Gastroenterol. 2002, 97, 1986–93. [Google Scholar] [CrossRef] [PubMed]
- Emmertsen, K.J.; Laurberg, S. Low anterior resection syndrome score: development and validation of a symptom-based scoring system for bowel dysfunction after low anterior resection for rectal cancer. Annals of surgery. 2012, 255, 922–928. [Google Scholar] [CrossRef] [PubMed]
- Sarcher, T.; Dupont, B.; Alves, A.; Menahem, B. Anterior resection syndrome: What should we tell practitioners and patients in 2018? Journal of Visceral Surgery. 2018, 155, 383–391. [Google Scholar] [CrossRef] [PubMed]
- Hou, X.T.; Pang, D.; Lu, Q.; Yang, P.; Jin, S.L.; Zhou, Y.J.; Tian, S.H. Validation of the Chinese version of the low anterior resection syndrome score for measuring bowel dysfunction after sphincter-preserving surgery among rectal cancer patients. European Journal of Oncology Nursing. 2015, 19, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Juul, T.; Elfeki, H.; Christensen, P.; Laurberg, S.; Emmertsen, K.J.; Bager, P. Normative Data for the Low Anterior Resection Syndrome Score (LARS Score). Ann Surg. 2018. [CrossRef] [PubMed]
- Battersby, N.J.; Bouliotis, G.; Emmertsen, K.J. Development and external validation of a nomogram and online tool to predict bowel dysfunction following restorative rectal cancer resection: the POLARS score. Gut. 2018, 67, 688–696. [Google Scholar] [CrossRef] [PubMed]
- Croese, A.D.; Lonie, J.; Trollope, A.F.; Vangaveti, V.N.; Ho, Y.H. A meta-analysis of the prevalence of Low Anterior Resection Syndrome and systematic review of risk factors. International Journal of Surgery. 2018, 56, 234–241. [Google Scholar] [CrossRef] [PubMed]
- Croese, A.D.; Zubair, O.N.; Lonie, J.; Trollope, A.F.; Vangaveti, V.N.; Mushaya, C.; Ho, Y.H. Prevalence of low anterior resection syndrome at a regional Australian centre. ANZ J Surg. 2018, 88, 813–817. [Google Scholar] [CrossRef] [PubMed]
- Bock, D.; Angenete, E.; Gonzales, E. Assessing health, quality of life and urogenital function in a sample of the Swedish general population: a cross-sectional study. BMJ Open. 2018, 8, e021974. [Google Scholar] [CrossRef] [PubMed]
- Bregendahl S, Emmertsen KJ, Lous J; et al. Bowel dysfunction after low anterior resection with and without neoadjuvant therapy for rectal cancer: a population-based cross-sectional study. Colorectal Dis. 2013, 15, 1130–1139. [Google Scholar] [CrossRef] [PubMed]
- Ribas, Y.; Aguilar, F.; Jovell-Fernández, E.; Cayetano, L.; Navarro-Luna, A.; Muñoz-Duyos, A. Clinical application of the LARS score: results from a pilot study. Int J Colorectal Dis. 2017, 32, 409–418. [Google Scholar] [CrossRef] [PubMed]
- Juul, T.; Ahlberg, M.; Biondo, S.; Emmertsen, K.J.; Espin, E.; Jimenez, L.M.; Matzel, K.; Palmer, G.; Sauermann, A.; Trenti, L.; Zhang, W.; Laurberg, S.; Christensen, P. International Validation of the Low Anterior Resection Syndrome Score. Annals of Surgery. 2014, 259, 728–734. [Google Scholar] [CrossRef] [PubMed]
- Bong, J.W.; Lim, S.B.; Lee, J.L.; Kim, C.W.; Yoon, Y.S.; Park, I.J.; Yu, C.S.; Kim, J.C. Comparison of Anthropometric Parameters after Ultralow Anterior Resection and Abdominoperineal Resection in Very Low-Lying Rectal Cancers. Gastroenterology research and practice. 2018, 9274618. [Google Scholar] [CrossRef] [PubMed]
- Tan, S.H.; Liao, Y.M.; Lee, K.C.; Ko, Y.L.; Lin, P.C. Exploring bowel dysfunction of patients following colorectal surgery: A cohort study. J Clin Nurs. 2019, 28, 1577–1584. [Google Scholar] [CrossRef] [PubMed]

 |
 |
© 2019 by the authors. 2019 Tudor-Cristian Frunza, Sorinel Lunca, Iustina Baciu, Iulia Axinia, Cezar Valentin Mocanu, Andreea Crudu, Narcis Bujor, Lucia Flavia Livenschi, Claudiu Alexandru Nicolaiev, Andreea Hulubencu, Anca Diaconu, Emilia Valasciu, Ioana Jalobceastai, Malina Tibirna, Mihail Gabriel Dimofte.
Share and Cite
Frunza, T.-C.; Lunca, S.; Baciu, I.; Axinia, I.; Mocanu, C.V.; Crudu, A.; Bujor, N.; Livenschi, L.F.; Nicolaiev, C.A.; Hulubencu, A.; et al. LARS-like Symptoms in the General Population May Suggest the Significance of Postoperative Functional Problems and Emotional Implications of Rectal Surgery. J. Mind Med. Sci. 2019, 6, 278-285. https://doi.org/10.22543/7674.62.P278285
Frunza T-C, Lunca S, Baciu I, Axinia I, Mocanu CV, Crudu A, Bujor N, Livenschi LF, Nicolaiev CA, Hulubencu A, et al. LARS-like Symptoms in the General Population May Suggest the Significance of Postoperative Functional Problems and Emotional Implications of Rectal Surgery. Journal of Mind and Medical Sciences. 2019; 6(2):278-285. https://doi.org/10.22543/7674.62.P278285
Chicago/Turabian StyleFrunza, Tudor-Cristian, Sorinel Lunca, Iustina Baciu, Iulia Axinia, Cezar Valentin Mocanu, Andreea Crudu, Narcis Bujor, Lucia Flavia Livenschi, Claudiu Alexandru Nicolaiev, Andreea Hulubencu, and et al. 2019. "LARS-like Symptoms in the General Population May Suggest the Significance of Postoperative Functional Problems and Emotional Implications of Rectal Surgery" Journal of Mind and Medical Sciences 6, no. 2: 278-285. https://doi.org/10.22543/7674.62.P278285
APA StyleFrunza, T.-C., Lunca, S., Baciu, I., Axinia, I., Mocanu, C. V., Crudu, A., Bujor, N., Livenschi, L. F., Nicolaiev, C. A., Hulubencu, A., Diaconu, A., Valasciu, E., Jalobceastai, I., Tibirna, M., & Dimofte, M. G. (2019). LARS-like Symptoms in the General Population May Suggest the Significance of Postoperative Functional Problems and Emotional Implications of Rectal Surgery. Journal of Mind and Medical Sciences, 6(2), 278-285. https://doi.org/10.22543/7674.62.P278285



