Long-Term Effectiveness and Sustainability of Integrating Peer-Assisted Ultrasound Courses into Medical School—A Prospective Study
Abstract
1. Introduction
1.1. Background
1.2. Research Problem and Question
2. Materials and Methods
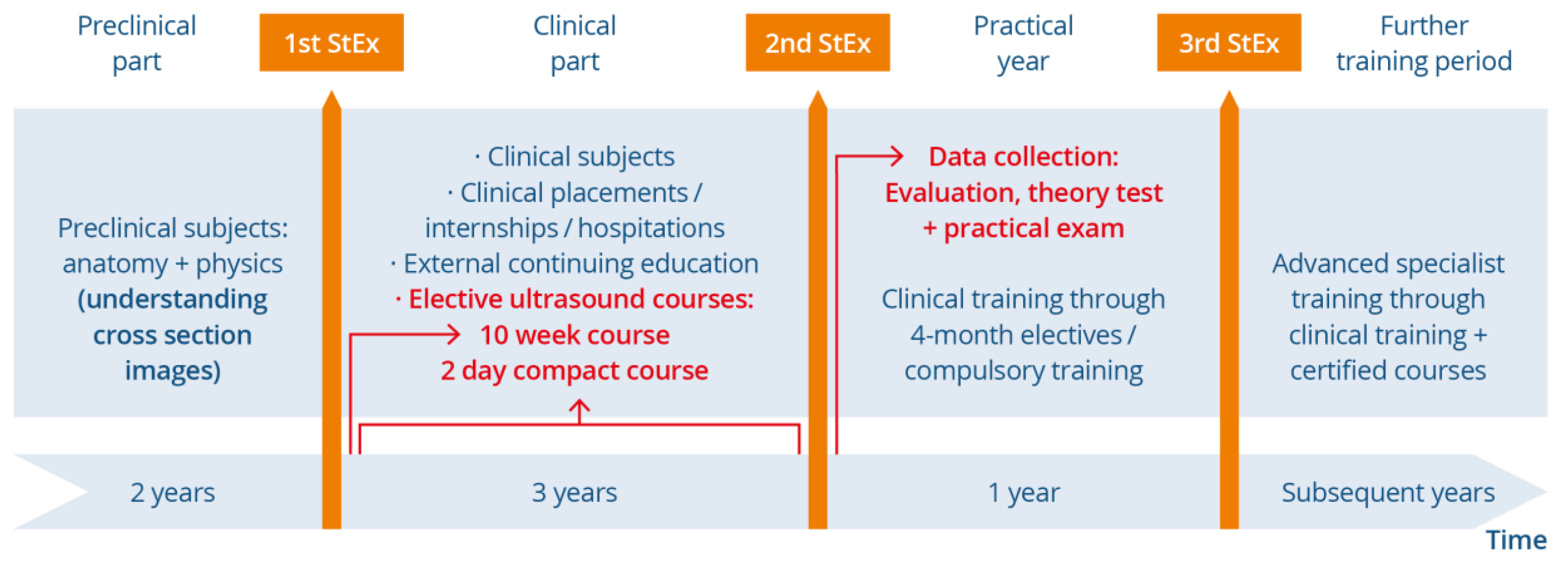
2.1. Study Design, (Recruitment of) Participants and Study Procedure
2.2. Measuring Instruments
2.2.1. Evaluation
2.2.2. Written Test
2.2.3. Practical Examination
2.3. Statistical Analysis
3. Results
3.1. Results of Evaluations
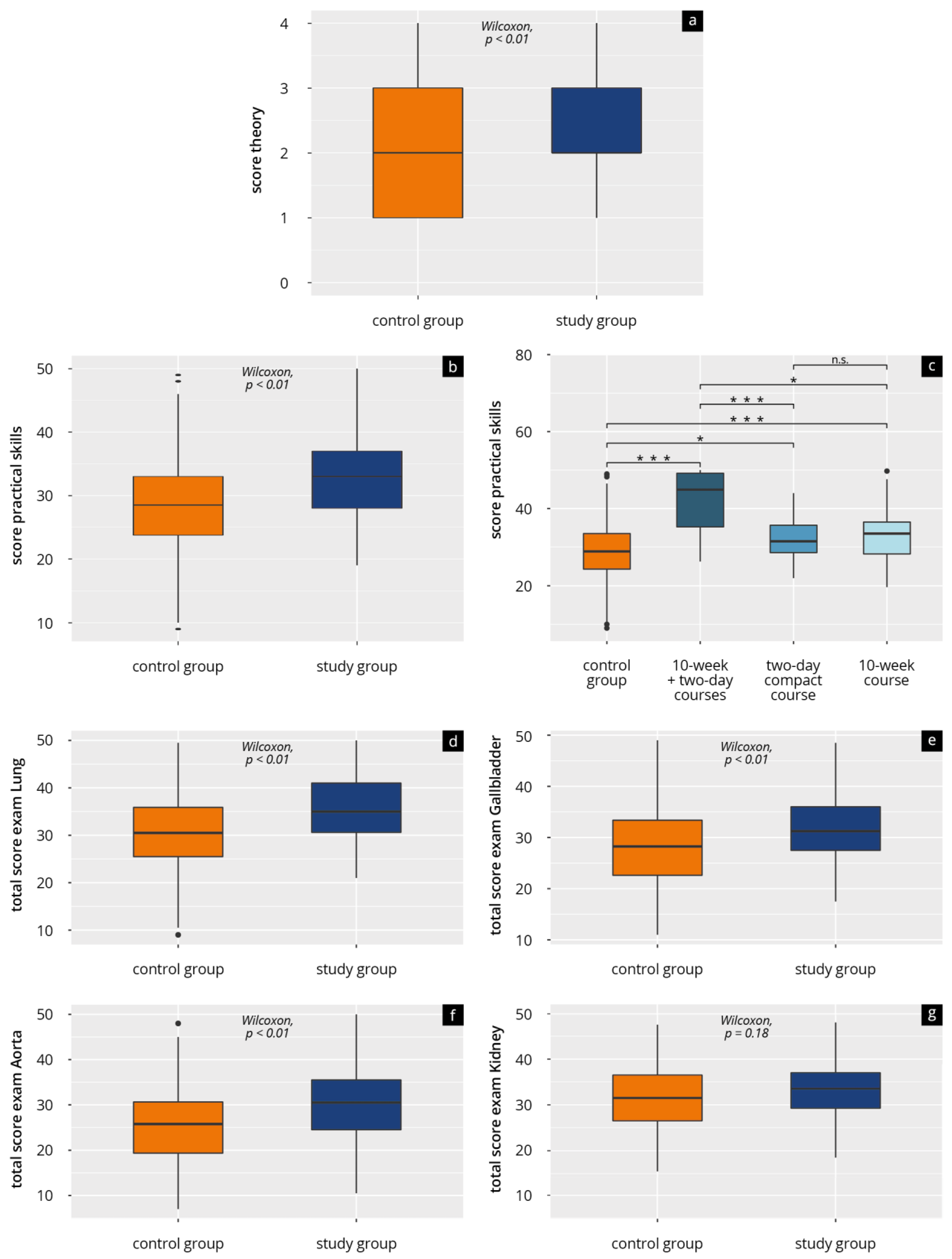
3.2. Results of Theory Tests and Practical Examinations
4. Discussion
4.1. Discussion of Subjective Assessment of Competency
4.2. Discussion of Objective Measurement of Competency and Influencing Factors
4.3. Discussion of the Attitude to Ultrasound Teaching within Medical Studies
4.4. Future Prospects for Curriculum Design
4.5. Limitations
4.6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dietrich, C.F.; Bolondi, L.; Duck, F.; Evans, D.H.; Ewertsen, C.; Fraser, A.G.; Gilja, O.H.; Jenssen, C.; Merz, E.; Nolsoe, C.; et al. History of Ultrasound in Medicine from its birth to date (2022), on occasion of the 50 Years Anniversary of EFSUMB. A publication of the European Federation of Societies for Ultrasound In Medicine and Biology (EFSUMB), designed to record the historical development of medical ultrasound. Med. Ultrason. 2022, 24, 434–450. [Google Scholar] [CrossRef]
- Custers, E. Long-term retention of basic science knowledge: A review study. Adv. Health Sci. Educ. Theory Pract. 2010, 15, 109–128. [Google Scholar] [CrossRef] [PubMed]
- Tarique, U.; Tang, B.; Singh, M.; Kulasegaram, K.M.; Ailon, J. Ultrasound Curricula in Undergraduate Medical Education: A Scoping Review. J. Ultrasound Med. 2018, 37, 69–82. [Google Scholar] [CrossRef] [PubMed]
- Wolf, R.; Geuthel, N.; Gnatzy, F.; Rotzoll, D. Undergraduate ultrasound education at German-speaking medical faculties: A survey. GMS J. Med. Educ. 2019, 36, Doc34. [Google Scholar] [CrossRef]
- Prosch, H.; Radzina, M.; Dietrich, C.F.; Nielsen, M.B.; Baumann, S.; Ewertsen, C.; Jenssen, C.; Kabaalioğlu, A.; Kosiak, W.; Kratzer, W.; et al. Ultrasound Curricula of Student Education in Europe: Summary of the Experience. Ultrasound Int. Open 2020, 6, E25–E33. [Google Scholar] [CrossRef]
- Bahner, D.P.; Goldman, E.; Way, D.; Royall, N.A.; Liu, Y.T. The State of Ultrasound Education in U.S. Medical Schools: Results of a National Survey. Acad. Med. 2014, 89, 1681–1686. [Google Scholar] [CrossRef]
- Kameda, T.; Taniguchi, N.; Konno, K.; Koibuchi, H.; Omoto, K.; Itoh, K. Ultrasonography in undergraduate medical education: A comprehensive review and the education program implemented at Jichi Medical University. J. Med. Ultrason. (2001) 2022, 49, 217–230. [Google Scholar] [CrossRef] [PubMed]
- Recker, F.; Barth, G.; Lo, H.; Haverkamp, N.; Nürnberg, D.; Kravchenko, D.; Raupach, T.; Schäfer, V.S. Students’ Perspectives on Curricular Ultrasound Education at German Medical Schools. Front. Med. 2021, 8, 2290. [Google Scholar] [CrossRef]
- So, S.; Patel, R.M.; Orebaugh, S.L. Ultrasound imaging in medical student education: Impact on learning anatomy and physical diagnosis. Anat. Sci. Educ. 2017, 10, 176–189. [Google Scholar] [CrossRef]
- Glass, C.; Sarwal, A.; Zavitz, J.; Nitsche, J.; Joyner, J.; Johnson, L.L.; Garcia-Vargas, J.; O’Brien, M.C. Scoping review of implementing a longitudinal curriculum in undergraduate medical education: The wake forest experience. Ultrasound J. 2021, 13, 23. [Google Scholar] [CrossRef]
- Hoffmann, B.; Blaivas, M.; Abramowicz, J.; Bachmann, M.; Badea, R.; Braden, B.; Cantisani, V.; Chammas, M.C.; Cui, X.W.; Dong, Y.; et al. Medical Student Ultrasound Education, a WFUMB Position Paper, Part II. A consensus statement of ultrasound societies. Med. Ultrason. 2020, 22, 220–229. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, C.F.; Hoffmann, B.; Abramowicz, J.; Badea, R.; Braden, B.; Cantisani, V.; Chammas, M.C.; Cui, X.W.; Dong, Y.; Gilja, O.H.; et al. Medical Student Ultrasound Education: A WFUMB Position Paper, Part I. Ultrasound Med. Biol. 2019, 45, 271–281. [Google Scholar] [CrossRef]
- Cantisani, V.; Dietrich, C.; Badea, R.; Dudea, S.; Prosch, H.; Cerezo, E.; Nuernberg, D.; Serra, A.; Sidhu, P.; Radzina, M.; et al. EFSUMB Statement on Medical Student Education in Ultrasound [long version]. Ultrasound Int. Open 2016, 02, E2–E7. [Google Scholar] [CrossRef]
- Hoppmann, R.A.; Mladenovic, J.; Melniker, L.; Badea, R.; Blaivas, M.; Montorfano, M.; Abuhamad, A.; Noble, V.; Hussain, A.; Prosen, G.; et al. International consensus conference recommendations on ultrasound education for undergraduate medical students. Ultrasound J. 2022, 14, 31. [Google Scholar] [CrossRef]
- Hoppmann, R.A.; Rao, V.V.; Bell, F.; Poston, M.B.; Howe, D.B.; Riffle, S.; Harris, S.; Riley, R.; McMahon, C.; Wilson, L.B.; et al. The evolution of an integrated ultrasound curriculum (iUSC) for medical students: 9-year experience. Crit. Ultrasound J. 2015, 7, 18. [Google Scholar] [CrossRef] [PubMed]
- Heinzow, H.S.; Friederichs, H.; Lenz, P.; Schmedt, A.; Becker, J.C.; Hengst, K.; Marschall, B.; Domagk, D. Teaching ultrasound in a curricular course according to certified EFSUMB standards during undergraduate medical education: A prospective study. BMC Med. Educ. 2013, 13, 84. [Google Scholar] [CrossRef] [PubMed]
- Celebi, N.; Griewatz, J.; Malek, N.P.; Krieg, S.; Kuehnl, T.; Muller, R.; Pauluschke-Frohlich, J.; Debove, I.; Riessen, R.; Zipfel, S.; et al. Development and implementation of a comprehensive ultrasound curriculum for undergraduate medical students—A feasibility study. BMC Med. Educ. 2019, 19, 170. [Google Scholar] [CrossRef]
- Krause, C.; Krause, R.; Krause, R.; Gomez, N.; Jafry, Z.; Dinh, V.A. Effectiveness of a 1-Hour Extended Focused Assessment With Sonography in Trauma Session in the Medical Student Surgery Clerkship. J. Surg. Educ. 2017, 74, 968–974. [Google Scholar] [CrossRef]
- Ang, J.; Doyle, B.; Allen, P.; Cheek, C. Teaching bedside ultrasound to medical students. Clin. Teach. 2018, 15, 331–335. [Google Scholar] [CrossRef]
- Arger, P.H.; Schultz, S.M.; Sehgal, C.M.; Cary, T.W.; Aronchick, J. Teaching medical students diagnostic sonography. J. Ultrasound Med. 2005, 24, 1365–1369. [Google Scholar] [CrossRef]
- Wong, I.; Jayatilleke, T.; Kendall, R.; Atkinson, P. Feasibility of a Focused Ultrasound Training Programme for Medical Undergraduate Students. Clin. Teach. 2011, 8, 3–7. [Google Scholar] [CrossRef]
- Mullen, A.; Kim, B.; Puglisi, J.; Mason, N.L. An economical strategy for early medical education in ultrasound. BMC Med. Educ. 2018, 18, 169. [Google Scholar] [CrossRef]
- Shapiro, R.S.; Ko, P.K.; Jacobson, S. A pilot project to study the use of ultrasonography for teaching physical examination to medical students. Comput. Biol. Med. 2002, 32, 403–409. [Google Scholar] [CrossRef]
- Rempell, J.S.; Saldana, F.; DiSalvo, D.; Kumar, N.; Stone, M.B.; Chan, W.; Luz, J.; Noble, V.E.; Liteplo, A.; Kimberly, H.; et al. Pilot Point-of-Care Ultrasound Curriculum at Harvard Medical School: Early Experience. West. J. Emerg. Med. 2016, 17, 734–740. [Google Scholar] [CrossRef]
- Teichgräber, U.; Ingwersen, M.; Ehlers, C.; Mentzel, H.J.; Redies, C.; Stallmach, A.; Behringer, W.; Guntinas-Lichius, O. Integration of ultrasonography training into undergraduate medical education: Catch up with professional needs. Insights Imaging 2022, 13, 150. [Google Scholar] [CrossRef]
- Höhne, E.; Recker, F.; Dietrich, C.F.; Schäfer, V.S. Assessment Methods in Medical Ultrasound Education. Front. Med. (Lausanne) 2022, 9, 871957. [Google Scholar] [CrossRef] [PubMed]
- Nourkami-Tutdibi, N.; Tutdibi, E.; Schmidt, S.; Zemlin, M.; Abdul-Khaliq, H.; Hofer, M. Long-Term Knowledge Retention after Peer-Assisted Abdominal Ultrasound Teaching: Is PAL a Successful Model for Achieving Knowledge Retention? Ultraschall Med. 2020, 41, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Dinh, V.A.; Dukes, W.S.; Prigge, J.; Avila, M. Ultrasound Integration in Undergraduate Medical Education: Comparison of Ultrasound Proficiency Between Trained and Untrained Medical Students. J. Ultrasound Med. 2015, 34, 1819–1824. [Google Scholar] [CrossRef] [PubMed]
- Prats, M.I.; Royall, N.A.; Panchal, A.R.; Way, D.P.; Bahner, D.P. Outcomes of an Advanced Ultrasound Elective: Preparing Medical Students for Residency and Practice. J. Ultrasound Med. 2016, 35, 975–982. [Google Scholar] [CrossRef] [PubMed]
- Kelm, D.J.; Ratelle, J.T.; Azeem, N.; Bonnes, S.L.; Halvorsen, A.J.; Oxentenko, A.S.; Bhagra, A. Longitudinal Ultrasound Curriculum Improves Long-Term Retention Among Internal Medicine Residents. J. Grad. Med. Educ. 2015, 7, 454–457. [Google Scholar] [CrossRef]
- Boivin, Z.; Carpenter, S.; Lee, G.; Chimileski, B.; Harrison, J.; Choudhary, D.; Herbst, M. Evaluation of a Required Vertical Point-of-Care Ultrasound Curriculum for Undergraduate Medical Students. Cureus 2022, 14, e30002. [Google Scholar] [CrossRef] [PubMed]
- Steinmetz, P.; Oleskevich, S.; Lewis, J. Acquisition and Long-term Retention of Bedside Ultrasound Skills in First-Year Medical Students. J. Ultrasound Med. 2016, 35, 1967–1975. [Google Scholar] [CrossRef] [PubMed]
- Town, J.A.; Bergl, P.A.; Narang, A.; McConville, J.F. Internal Medicine Residents’ Retention of Knowledge and Skills in Bedside Ultrasound. J. Grad. Med. Educ. 2016, 8, 553–557. [Google Scholar] [CrossRef] [PubMed]
- Weimer, J.M. Die Etablierung und der Vergleich Verschiedener Ultraschallkursformate an der Universitätsmedizin Mainz. Ph.D. Thesis, Johannes Gutenberg-Universität Mainz, Mainz, Germany, 2021. [Google Scholar]
- DEGUM e. V. Kurskonzept Innere Medizin. Available online: https://www.degum.de/en/sektionen/innere-medizin/kurse.html (accessed on 25 May 2023).
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef] [PubMed]
- Hofer, M.; Kamper, L.; Sadlo, M.; Sievers, K.; Heussen, N. Evaluation of an OSCE assessment tool for abdominal ultrasound courses. Ultraschall Med. 2011, 32, 184–190. [Google Scholar] [CrossRef]
- Jünger, J. Ärztliche Kommunikation—Praxisbuch zum Masterplan Medizinstudium 2020, 1st ed.; Schattauer Verlag: Stuttgart, Germany, 2018; p. S. 645 f. [Google Scholar]
- Weimer, J.; Rolef, P.; Müller, L.; Bellhäuser, H.; Göbel, S.; Buggenhagen, H.; Weimer, A.; Waezsada, E.; Kirchhoff, F.; Weinmann-Menke, J. FoCUS cardiac ultrasound training for undergraduates based on current national guidelines: A prospective, controlled, single-center study on transferability. BMC Med. Educ. 2023, 23, 80. [Google Scholar] [CrossRef]
- Oteri, V.; Occhipinti, F.; Gribaudo, G.; Marastoni, F.; Chisari, E. Integration of ultrasound in medical School: Effects on Physical Examination Skills of Undergraduates. Med. Sci. Educ. 2020, 30, 417–427. [Google Scholar] [CrossRef]
- Dinh, V.A.; Lakoff, D.; Hess, J.; Bahner, D.P.; Hoppmann, R.; Blaivas, M.; Pellerito, J.S.; Abuhamad, A.; Khandelwal, S. Medical Student Core Clinical Ultrasound Milestones: A Consensus Among Directors in the United States. J. Ultrasound Med. 2016, 35, 421–434. [Google Scholar] [CrossRef]
- MFT Medizinischer Fakultätentag der Bundesrepublik Deutschland e.V. Nationaler Kompetenzbasierter Lernzielkatalog Medizin Version 2.0. Available online: http://www.nklm.de/ (accessed on 18 April 2022).
- Vallée, A.; Blacher, J.; Cariou, A.; Sorbets, E. Blended Learning Compared to Traditional Learning in Medical Education: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2020, 22, e16504. [Google Scholar] [CrossRef]
- Darras, K.E.; Spouge, R.J.; de Bruin, A.B.H.; Sedlic, A.; Hague, C.; Forster, B.B. Undergraduate Radiology Education During the COVID-19 Pandemic: A Review of Teaching and Learning Strategies [Formula: See text]. Can. Assoc. Radiol. J. 2021, 72, 194–200. [Google Scholar] [CrossRef]
- Blank, V.; Strobel, D.; Karlas, T. Digital Training Formats in Ultrasound Diagnostics for physicians: What options are available and how can they be successfully integrated into current DEGUM certified course concepts? Ultraschall Med. 2022, 43, 428–434. [Google Scholar] [CrossRef] [PubMed]
- Yuan, X. Evidence of the Spacing Effect and Influences on Perceptions of Learning and Science Curricula. Cureus 2022, 14, e21201. [Google Scholar] [CrossRef]
- Theobald, M.; Bellhäuser, H.; Imhof, M. Identifying individual differences using log-file analysis: Distributed learning as mediator between conscientiousness and exam grades. Learn. Individ. Differ. 2018, 65, 112–122. [Google Scholar] [CrossRef]
- Wijnen-Meijer, M.; van den Broek, S.; Koens, F.; Ten Cate, O. Vertical integration in medical education: The broader perspective. BMC Med. Educ. 2020, 20, 509. [Google Scholar] [CrossRef]
- Dickerson, J.; Paul, K.; Vila, P.; Whiticar, R. The role for peer-assisted ultrasound teaching in medical school. Clin. Teach. 2017, 14, 170–174. [Google Scholar] [CrossRef]
- Weimer, J.M.; Rink, M.; Müller, L.; Dirks, K.; Ille, C.; Bozzato, A.; Sproll, C.; Weimer, A.M.; Neubert, C.; Buggenhagen, H.; et al. Development and Integration of DOPS as Formative Tests in Head and Neck Ultrasound Education: Proof of Concept Study for Exploration of Perceptions. Diagnostics 2023, 13, 661. [Google Scholar] [CrossRef] [PubMed]
- Yang, B.W.; Razo, J.; Persky, A.M. Using Testing as a Learning Tool. Am. J. Pharm. Educ. 2019, 83, 7324. [Google Scholar] [CrossRef] [PubMed]
- Chernikova, O.; Heitzmann, N.; Stadler, M.; Holzberger, D.; Seidel, T.; Fischer, F. Simulation-Based Learning in Higher Education: A Meta-Analysis. Rev. Educ. Res. 2020, 90, 499–541. [Google Scholar] [CrossRef]
| Variables | Control Group (n = 161) | Study Group (n = 141) | p Value |
|---|---|---|---|
| Attended weekend course, n (%) | 0 (0.0) | 39 (27.6) | |
| Attended weekly course, n (%) | 0 (0.0) | 90 (63.8) | |
| Attended weekend course + weekly course, n (%) | 0 (0.0) | 12 (8.6) | |
| Age, mean (SD) | 28.4 (3.6) | 27.5 (3.1) | 0.05 |
| Gender | n (%) | n (%) | 0.30 |
| female | 83 (51.6) | 82 (58.2) | |
| male | 77 (47.8) | 59 (41.8) | |
| no information | 1 (0.6) | 0 (0.0) | |
| Training prior to study | n (%) | n (%) | 0.64 |
| yes | 88 (54.7) | 81 (57.5) | |
| no | 73 (45.3) | 60 (42.5) | |
| Previous medical experience | n (%) | n (%) | 0.99 |
| yes | 92 (57.1) | 81 (57.5) | |
| no | 69 (42.9) | 60 (42.5) | |
| Contact points with ultrasound in clinical placement | n (%) | n (%) | 0.60 |
| no | 18 (11.2) | 19 (13.5) | |
| yes | 142 (88.2) | 121 (85.8) | |
| no information | 1 (0.6) | 1 (0.7) | |
| Internal medicine (hospital) | 80 (49.7) | 63 (44.7) | |
| GP | 93 (57.8) | 95 (67.4) | |
| Radiology | 5 (3.1) | 10 (7.1) | |
| Gynaecology | 19 (11.8) | 13 (9.2) | |
| Urology | 21 (13.0) | 4 (2.8) | |
| Paediatrics | 0 (0.0) | 0 (0.0) | |
| Anaesthesiology | 0 (0.0) | 0 (0.0) | |
| Surgery | 0 (0.0) | 0 (0.0) | |
| Number of patients independently examined | n (%) | n (%) | 0.66 |
| 0–50 | 132 (82.0) | 114 (80.9) | |
| 50–100 | 10 (6.2) | 12 (8.5) | |
| 100–150 | 1 (0.6) | 2 (1.4) | |
| 150–200 | 0 (0.0) | 0 (0.0) | |
| >200 | 1 (0.6) | 2 (1.4) | |
| No information | 17 (10.6) | 11 (7.8) | |
| Other ultrasound experience | n (%) | n (%) | 0.32 |
| no | 134 (83.2) | 122 (86.5) | |
| yes | 25 (15.5) | 16 (11.4) | |
| no information | 2 (1.2) | 3 (2.1) |
| Variables | Control Group (n = 161) | Study Group (n = 141) | p Value |
|---|---|---|---|
| Mean (SD) | Mean (SD) | ||
| Expectations and need (1 = fully agree; 7 = do not agree at all) | |||
| Diagnostic competency during studies | 1.38 (0.91) | 1.38 (1.04) | 0.59 |
| Diagnostic competency within compulsory teaching | 1.45 (0.98) | 1.41 (0.90) | 0.91 |
| Integration of digital teaching media into ultrasound education | 2.04 (1.35) | 1.81 (1.09) | 0.10 |
| Further development of digital teaching media | 1.88 (1.22) | 1.70 (1.03) | 0.16 |
| Current subjective assessment of competency (1 = very low, 7 = very high) | |||
| Theoretical ultrasound knowledge | 2.88 (1.22) | 3.39 (1.36) | <0.01 |
| Practical ultrasound knowledge | 2.70 (1.27) | 3.36 (1.31) | <0.01 |
| Topographical anatomical knowledge | 3.69 (1.28) | 4.11 (1.35) | 0.01 |
| Spatial perception/orientation in the image | 3.61 (1.36) | 4.16 (1.4) | <0.01 |
| Handling of an ultrasound machine | 3.57 (1.24) | 4.38 (1.39) | <0.01 |
| Optimal adjustment of the image | 2.79 (1.34) | 3.51 (1.36) | <0.01 |
| Retrievable knowledge from that time | % (SD) | ||
| Two-day compact course (n = 39) | 0 | 48.2 (21.5) | |
| 10-week course (n =90) | 0 | 42.9 (17.7) | |
| Both courses (n= 12) | 0 | 72.05 (22.6) | |
| Control Group | Study Group | p Value | |
|---|---|---|---|
| Mean (SD) | Mean (SD) | ||
| Overall test and examination results | |||
| Pathology diagnoses (theory test) (max. 4 AP) | 2.43 (1.18) | 2.8 (1.08) | <0.01 |
| Practical exam average (max. 50 AP) | 28.6 (7.75) | 33.2 (6.6) | <0.01 |
| Test results per practical exam | |||
| Exam—lung (n) | 72 | 54 | |
| Total (max. 50 P) | 30.6 (8.30) | 35.3 (7.33) | <0.01 |
| Opening the dialogue (max. 4 P) | 3.32 (0.87) | 3.20 (0.77) | 0.14 |
| Handling the transducer (max. 8 P) | 4.72 (1.75) | 5.5 (1.56) | <0.01 |
| Patient guidance (max. 6 P) | 2.83 (2.13) | 4.25 (1.86) | <0.01 |
| Examination procedure (max. 13 P) | 8.26 (3.0) | 9.93 (2.12) | <0.01 |
| Overall performance (max. 8 P) | 4.57 (1.73) | 5.35 (1.62) | 0.01 |
| Communication (max. 4 P) | 2.60 (1.21) | 2.55 (1.00) | 0.77 |
| Theory questions (max. 7 P) | 4.32 (1.10) | 4.55 (1.22) | 0.39 |
| Exam—gallbladder (n) | 71 | 50 | |
| Total (max. 50 P) | 28.5 (7.89) | 32.1 (6.65) | <0.01 |
| Opening the dialogue (max. 4 P) | 3.41 (0.74) | 3.10 (0.73) | <0.01 |
| Handling the transducer (max. 8) | 4.78 (1.74) | 5.17 (1.36) | 0.27 |
| Patient guidance (max. 6 P) | 2.89 (2.19) | 4.05 (1.90) | <0.01 |
| Examination procedure (max. 16 P) | 8.68 (3.04) | 10.40 (2.90) | <0.01 |
| Overall performance (max. 8 P) | 4.02 (1.68) | 4.79 (1.39) | <0.01 |
| Communication (max. 4 P) | 2.41 (0.97) | 2.42 (0.87) | 0.93 |
| Theory questions (max. 4 P) | 2.14 (0.94) | 2.19 (0.72) | 0.55 |
| Exam—aorta (n) | 60 | 41 | |
| Total (max. 50 P) | 25.5 (8.20) | 30.70 (8.33) | <0.01 |
| Opening the dialogue (max. 4 P) | 3.27 (0.82) | 2.96 (0.75) | 0.02 |
| Handling the transducer (max. 8 P) | 5.12 (1.76) | 5.95 (1.33) | 0.02 |
| Patient guidance (max. 6 P) | 2.03 (2.13) | 3.05 (2.13) | 0.02 |
| Examination procedure (max. 13 P) | 6.72 (3.09) | 8.60 (2.65) | <0.01 |
| Overall performance (max. 8 P) | 3.98 (1.52) | 4.98 (1.61) | <0.01 |
| Communication (max. 4 P) | 2.24 (0.98) | 2.40 (0.92) | 0.52 |
| Theory questions (max. 7 P) | 2.15 (1.42) | 2.68 (2.00) | 0.35 |
| Exam—kidney (n) | 61 | 61 | |
| Total (max. 50 P) | 32.0 (7.62) | 33.6 (5.92) | 0.18 |
| Opening the dialogue (max 4 P) | 3.19 (0.84) | 3.14 (0.69) | 0.34 |
| Handling the transducer (max. 8 P) | 5.43 (1.67) | 5.80 (1.42) | 0.24 |
| Patient guidance (max. 6 P) | 3.16 (2.20) | 3.57 (2.02) | 0.30 |
| Examination procedure (max. 14 P) | 9.45 (2.56) | 9.98 (2.46) | 0.30 |
| Overall performance (max. 8 P) | 5.11 (1.62) | 5.32 (1.38) | 0.37 |
| Communication (max. 4 P) | 2.48 (0.92) | 2.54 (0.85) | 0.77 |
| Theory question (max. 6 P) | 3.20 (0.87) | 3.26 (0.87) | 0.79 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Weimer, J.M.; Widmer, N.; Strelow, K.-U.; Hopf, P.; Buggenhagen, H.; Dirks, K.; Künzel, J.; Börner, N.; Weimer, A.M.; Lorenz, L.A.; et al. Long-Term Effectiveness and Sustainability of Integrating Peer-Assisted Ultrasound Courses into Medical School—A Prospective Study. Tomography 2023, 9, 1315-1328. https://doi.org/10.3390/tomography9040104
Weimer JM, Widmer N, Strelow K-U, Hopf P, Buggenhagen H, Dirks K, Künzel J, Börner N, Weimer AM, Lorenz LA, et al. Long-Term Effectiveness and Sustainability of Integrating Peer-Assisted Ultrasound Courses into Medical School—A Prospective Study. Tomography. 2023; 9(4):1315-1328. https://doi.org/10.3390/tomography9040104
Chicago/Turabian StyleWeimer, Johannes Matthias, Nina Widmer, Kai-Uwe Strelow, Paula Hopf, Holger Buggenhagen, Klaus Dirks, Julian Künzel, Norbert Börner, Andreas Michael Weimer, Liv Annebritt Lorenz, and et al. 2023. "Long-Term Effectiveness and Sustainability of Integrating Peer-Assisted Ultrasound Courses into Medical School—A Prospective Study" Tomography 9, no. 4: 1315-1328. https://doi.org/10.3390/tomography9040104
APA StyleWeimer, J. M., Widmer, N., Strelow, K.-U., Hopf, P., Buggenhagen, H., Dirks, K., Künzel, J., Börner, N., Weimer, A. M., Lorenz, L. A., Rink, M., Bellhäuser, H., Schiestl, L. J., Kloeckner, R., Müller, L., & Weinmann-Menke, J. (2023). Long-Term Effectiveness and Sustainability of Integrating Peer-Assisted Ultrasound Courses into Medical School—A Prospective Study. Tomography, 9(4), 1315-1328. https://doi.org/10.3390/tomography9040104







