Quantitative Analysis of the Clinical Reasons Influencing the Frequency of Pediatric Head CT Examinations: A Single-Center Observation Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Data Analysis
3. Results
3.1. Characterization of the Number of CT Examinations
3.2. Factors Governing the Number of Examinations
3.3. The Impact of the Number of Non-Head CT Examinations
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- ICRP. The 2007 Recommendations of the International Commission on Radiological Protection. ICRP Publication 103. Ann. ICRP 2007, 37, 1–332. [Google Scholar]
- Berrington de Gonzalez, A.; Darby, S. Risk of cancer from diagnostic X-rays: Estimates for the UK and 14 other countries. Lancet 2004, 363, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Brenner, D.J.; Hall, E.J. Computed Tomography—An Increasing Source of Radiation Exposure. N. Engl. J. Med. 2007, 357, 2277–2284. [Google Scholar] [CrossRef]
- Kadowaki, Y.; Hamada, N.; Kai, M.; Furukawa, K. Evaluation of the lifetime brain/central nervous system cancer risk associated with childhood head CT scanning in Japan. Int. J. Cancer 2020, 148, 2429–2439. [Google Scholar] [CrossRef] [PubMed]
- de Gonzalez, A.B.; Pasqual, E.; Veiga, L. Epidemiological studies of CT scans and cancer risk: The state of the science. Br. J. Radiol. 2021, 94, 20210471. [Google Scholar] [CrossRef] [PubMed]
- Pearce, M.S.; Salotti, J.A.; Little, M.P.; McHugh, K.; Lee, C.; Kim, K.P.; Howe, N.L.; Ronckers, C.M.; Rajaraman, P.; Craft, A.W.; et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: A retrospective cohort study. Lancet 2012, 380, 499–505. [Google Scholar] [CrossRef] [PubMed]
- Meulepas, J.M.; Ronckers, C.M.; Smets, A.M.J.B.; Nievelstein, R.A.J.; Gradowska, P.; Lee, C.; Jahnen, A.; Van Straten, M.; De Wit, M.-C.Y.; Zonnenberg, B.; et al. Radiation Exposure From Pediatric CT Scans and Subsequent Cancer Risk in the Netherlands. Gynecol. Oncol. 2018, 111, 256–263. [Google Scholar] [CrossRef] [PubMed]
- Boice, J. Radiation epidemiology and recent paediatric computed tomography studies. Ann. ICRP 2015, 44, 236–248. [Google Scholar] [CrossRef] [PubMed]
- Berrington De Gonzalez, A.; Salotti, J.A.; McHugh, K.; Little, M.P.; Harbron, R.W.; Lee, C.; Ntowe, E.; Braganza, M.Z.; Parker, L.; Rajaraman, P.; et al. Relationship between paediatric CT scans and subsequent risk of leukaemia and brain tumours: Assessment of the impact of underlying conditions. Br. J. Cancer 2016, 114, 388–394. [Google Scholar] [CrossRef]
- Meulepas, J.M.; Ronckers, C.M.; Merks, J.; Weijerman, M.E.; Lubin, J.H.; Hauptmann, M. Confounding of the association between radiation exposure from CT scans and risk of leukemia and brain tumors by cancer susceptibility syndromes. J. Radiol. Prot. 2016, 36, 953–974. [Google Scholar] [CrossRef]
- Meulepas, J.M.; Hauptmann, M.; Lubin, J.H.; Shuryak, I.; Brenner, D.J. Is there Unmeasured Indication Bias in Radiation-Related Cancer Risk Estimates from Studies of Computed Tomography? Radiat. Res. 2018, 189, 128–135. [Google Scholar] [CrossRef] [PubMed]
- Little, M.P.; Patel, A.; Lee, C.; Hauptmann, M.; de Gonzalez, A.B.; Albert, P. Impact of Reverse Causation on Estimates of Cancer Risk Associated With Radiation Exposure From Computerized Tomography: A Simulation Study Modeled on Brain Cancer. Am. J. Epidemiol. 2021, 191, 173–181. [Google Scholar] [CrossRef] [PubMed]
- Smoll, N.R.; Mathews, J.D.; Scurrah, K.J. CT scans in childhood predict subsequent brain cancer: Finite mixture modelling can help separate reverse causation scans from those that may be causal. Cancer Epidemiol. 2020, 67, 101732. [Google Scholar] [CrossRef] [PubMed]
- Mathews, J.D.; Forsythe, A.V.; Brady, Z.; Butler, M.W.; Goergen, S.K.; Byrnes, G.B.; Giles, G.G.; Wallace, A.B.; Anderson, P.R.; Guiver, T.A.; et al. Cancer risk in 680 000 people exposed to computed tomography scans in childhood or adolescence: Data linkage study of 11 million Australians. BMJ 2013, 346, f2360. [Google Scholar] [CrossRef]
- Hong, J.-Y.; Han, K.; Jung, J.-H.; Kim, J.S. Association of Exposure to Diagnostic Low-Dose Ionizing Radiation With Risk of Cancer Among Youths in South Korea. JAMA Netw. Open 2019, 2, e1910584. [Google Scholar] [CrossRef]
- Carozza, S.E.; Langlois, P.H.; Miller, E.A.; Canfield, M. Are children with birth defects at higher risk of childhood cancers? Am. J. Epidemiol. 2012, 175, 1217–1224. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2020. [Google Scholar]
- Yoshida, K.; Krille, L.; Dreger, S.; Hoenig, L.; Merzenich, H.; Yasui, K.; Kumagai, A.; Ohtsuru, A.; Uetani, M.; Mildenberger, P.; et al. Pediatric computed tomography practice in Japanese university hospitals from 2008–2010: Did it differ from German practice? J. Radiat. Res. 2017, 58, 135–141. [Google Scholar] [CrossRef]
- Yoshitake, T.; Ono, K.; Ishiguchi, T.; Maeda, T.; Kai, M. Clinical indications for the use of computed tomography in children who underwent frequent computed tomography: A near-13-year follow-up retrospective study at a single institution in Japan. Radiat. Environ. Biophys. 2020, 59, 407–414. [Google Scholar] [CrossRef]
- Journy, N.M.; McHugh, K.; Harbron, R.W.; Pearce, M.S.; De Gonzalez, A.B. Medical conditions associated with the use of CT in children and young adults, Great Britain, 1995–2008. Br. J. Radiol. 2016, 89, 20160532. [Google Scholar] [CrossRef]
- Sorantin, E.; Wegmann, H.; Zaupa, P.; Mentzel, H.J.; Riccabona, M. Computed tomographic scan in head trauma: What is the rational in children? Eur. J. Pediatr. Surg. 2013, 23, 444–453. [Google Scholar]
- Howe, J.; Fitzpatrick, C.M.; LaKam, D.R.; Gleisner, A.; Vane, D.W. Routine repeat brain computed tomography in all children with mild traumatic brain injury may result in unnecessary radiation exposure. J. Trauma Inj. Infect. Crit. Care 2014, 76, 292–296. [Google Scholar] [CrossRef] [PubMed]
- Dreger, S.; Krille, L.; Maier, W.; Pokora, R.; Blettner, M.; Zeeb, H. Regional Deprivation and Non-Cancer Related Computed Tomography Use in Pediatric Patients in Germany: Cross-Sectional Analysis of Cohort Data. PLoS ONE 2016, 11, e0153644. [Google Scholar] [CrossRef]
- Pearce, M.S.; Salotti, J.A.; McHugh, K.; Kim, K.P.; Craft, A.W.; Lubin, J.; Ron, E.; Parker, L. Socio-economic variation in CT scanning in Northern England, 1990-2002. BMC Health Serv. Res. 2012, 12, 24. [Google Scholar] [CrossRef] [PubMed]
- Hauptmann, M.; Byrnes, G.; Cardis, E.; Bernier, M.-O.; Blettner, M.; Dabin, J.; Engels, H.; Istad, T.S.; Johansen, C.; Kaijser, M.; et al. Brain cancer after radiation exposure from CT examinations of children and young adults: Results from the EPI-CT cohort study. Lancet Oncol. 2022, 24, 45–53. [Google Scholar] [CrossRef]
- Shibata, S.; Shibamoto, Y.; Maehara, M.; Hobo, A.; Hotta, N.; Ozawa, Y. Reasons for Undergoing CT During Childhood: Can CT-Exposed and CT-Naive Populations Be Compared? Dose Response 2020, 18, 1559325820907011. [Google Scholar] [CrossRef]
- Norwood, M.S.; Lupo, P.J.; Chow, E.J.; Scheurer, M.E.; Plon, S.E.; Danysh, H.E.; Spector, L.G.; Carozza, S.E.; Doody, D.R.; Mueller, B.A. Childhood cancer risk in those with chromosomal and non-chromosomal congenital anomalies in Washington State: 1984-2013. PLoS ONE 2017, 12, e0179006. [Google Scholar] [CrossRef] [PubMed]
- Kojimahara, N.; Yoshitake, T.; Ono, K.; Kai, M.; Bynes, G.; Schüz, J.; Cardis, E.; Kesminiene, A. Computed tomography of the head and the risk of brain tumours during childhood and adolescence: Results from a case–control study in Japan. J. Radiol. Prot. 2020, 40, 1010–1023. [Google Scholar] [CrossRef] [PubMed]


| Total | |||||
|---|---|---|---|---|---|
| No. of scans | 30,490 | ||||
| No. of patients | 4514 | ||||
| Head CT | |||||
| No. of scans | 19,498 | 63.9% | |||
| No. of patients | 3456 | 76.6% | |||
| Age when CT started | No. of patients | ||||
| Age < 1 | 1500 | 43.4% | |||
| 1 ≤ Age < 5 | 939 | 27.2% | |||
| 5 ≤ Age < 10 | 604 | 17.5% | |||
| 10 ≤ Age < 15 | 370 | 10.7% | |||
| 15 ≤ Age < 20 | 43 | 1.2% | |||
| Diseases | No. of patients | ICD-10 | |||
| Hydrocephalus | 421 | 12.2% | G910-G919, Q039, Q043, Q054 | ||
| Trauma | 331 | 9.6% | S00-T90, T8X not included | ||
| Brain tumors | 216 | 6.3% | C700-C793, D320-D432 | ||
| Other tumors | 574 | 16.6% | C000-C169 | ||
| Congenital anomalies | 677 | 19.6% | Q00-Q99 | ||
| Others | 939 | 27.2% | |||
| Unknown | 298 | 8.6% | |||
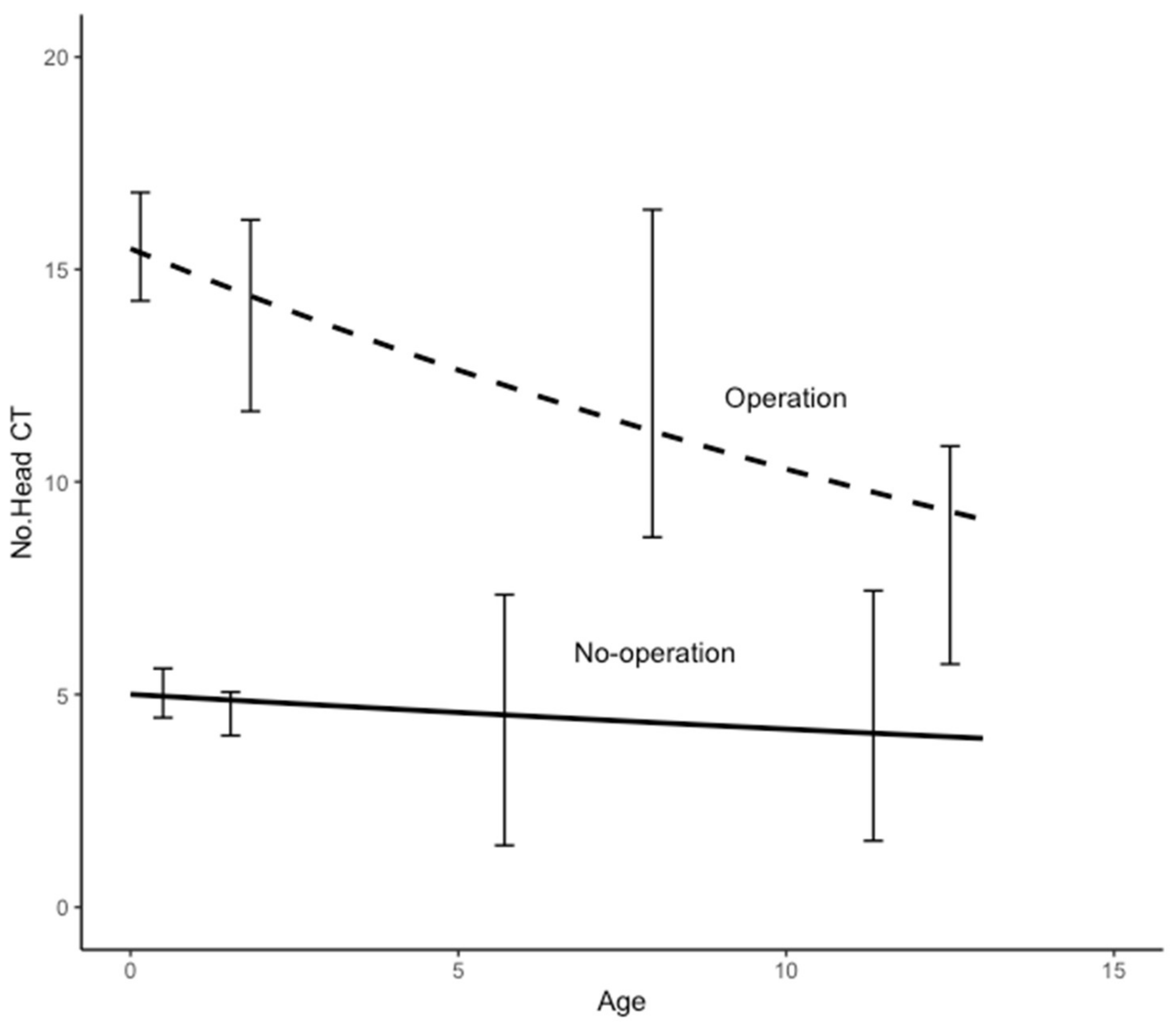
| (a) | ||||||||
| No. of Patients | Mean Age | Mean NCT | 95% CI Lower | 95% CI Upper | Mean Duration | 95% CI Lower | 95% CI Upper | |
| 421 | ||||||||
| with surgery | 333 | |||||||
| 0 ≤ Age < 1 | 215 | 0.28 | 15.5 | 14.3 | 16.8 | 5.2 | 3.9 | 7.5 |
| 1 ≤ Age < 5 | 71 | 2.18 | 13.9 | 11.7 | 16.2 | 5.9 | 4.9 | 6.8 |
| 5 ≤ Age < 10 | 29 | 7.67 | 12.6 | 8.7 | 16.4 | 7.3 | 5.7 | 8.9 |
| 10 ≤ Age < 20 | 18 | 12.7 | 8.3 | 5.7 | 10.8 | 5.7 | 3.9 | 7.5 |
| without surgery | 88 | |||||||
| 0 ≤ Age < 1 | 59 | 0.46 | 5.0 | 4.5 | 5.6 | 2.3 | 1.6 | 3.1 |
| 1 ≤ Age < 5 | 22 | 1.92 | 4.5 | 4.0 | 5.1 | 2.1 | 0.9 | 3.3 |
| 5 ≤ Age < 10 | 5 | 6.3 | 4.4 | 1.5 | 7.3 | 1.7 | −1.3 | 4.7 |
| 10 ≤ Age < 20 | 2 | 11.3 | 4.5 | 1.6 | 7.4 | 1.3 | −1.0 | 3.7 |
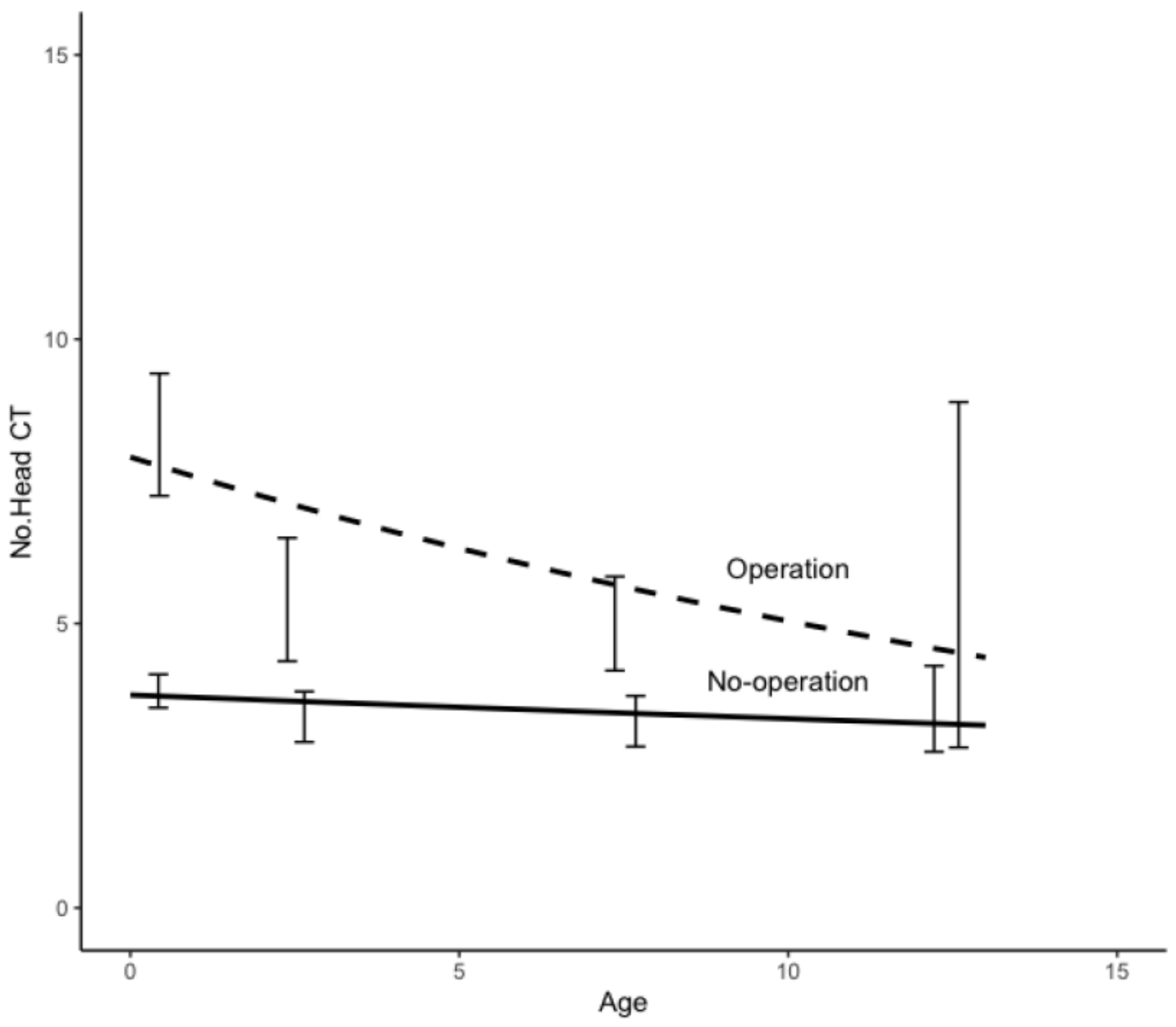
| (b) | ||||||||
| No. of Patients | Mean Age | Mean NCT | 95% CI Lower | 95% CI Upper | Mean Duration | 95% CI Lower | 95% CI Upper | |
| 331 | ||||||||
| with surgery | 92 | |||||||
| 0 ≤ Age < 1 | 56 | 0.4 | 8.3 | 7.2 | 9.4 | 2.4 | 1.8 | 3.1 |
| 1 ≤ Age < 5 | 19 | 2.4 | 5.4 | 4.3 | 6.5 | 3.7 | 2.0 | 5.5 |
| 5 ≤ Age < 10 | 10 | 7.4 | 5.0 | 4.2 | 5.8 | 1.3 | 0.2 | 2.4 |
| 10 ≤ Age < 20 | 7 | 12.6 | 5.9 | 2.8 | 8.9 | 1.9 | 0.4 | 3.4 |
| without surgery | 239 | |||||||
| 0 ≤ Age < 1 | 117 | 0.4 | 3.8 | 3.5 | 4.1 | 0.9 | 0.5 | 1.3 |
| 1 ≤ Age < 5 | 50 | 2.6 | 3.4 | 2.9 | 3.8 | 0.7 | 0.2 | 1.2 |
| 5 ≤ Age < 10 | 46 | 7.7 | 3.3 | 2.8 | 3.7 | 1.2 | 0.5 | 1.8 |
| 10 ≤ Age < 20 | 26 | 12.2 | 3.5 | 2.7 | 4.3 | 0.7 | 0.3 | 1.1 |
| (c) | ||||||||
| No. of Patients | Mean Age | Mean NCT | 95% CI Lower | 95% CI Upper | Mean Duration | 95% CI Lower | 95% CI Upper | |
| 216 | ||||||||
| with surgery | 193 | |||||||
| 0 ≤ Age < 1 | 25 | 0.4 | 11.4 | 8.3 | 14.4 | 1.4 | 0.6 | 2.1 |
| 1 ≤ Age < 5 | 60 | 2.9 | 8.2 | 6.8 | 9.6 | 2.1 | 1.5 | 2.8 |
| 5 ≤ Age < 10 | 59 | 7.4 | 6.9 | 5.9 | 7.9 | 1.4 | 0.8 | 2.0 |
| 10 ≤ Age < 20 | 49 | 12.3 | 6.7 | 5.5 | 7.9 | 2.0 | 1.2 | 2.7 |
| without surgery | 23 | |||||||
| 0 ≤ Age < 1 | 4 | 0.3 | 2.5 | 0.8 | 4.2 | 3.0 | 1.1 | 4.8 |
| 1 ≤ Age < 5 | 5 | 2.9 | 3.0 | 0.9 | 5.1 | 6.4 | 1.6 | 11.2 |
| 5 ≤ Age < 10 | 11 | 6.4 | 5.6 | 2.9 | 8.4 | 2.0 | 0.2 | 3.7 |
| 10 ≤ Age < 20 | 3 | 11.0 | 4.0 | 2.0 | 6.0 | 0.9 | −0.2 | 2.0 |
| (d) | ||||||||
| No. of Patients | Mean Age | Mean NCT | 95% CI Lower | 95% CI Upper | Mean Duration | 95% CI Lower | 95% CI Upper | |
| 677 | ||||||||
| with surgery | 472 | |||||||
| 0 ≤ Age < 1 | 281 | 0.30 | 7.6 | 6.7 | 8.5 | 4.1 | 3.7 | 4.5 |
| 1 ≤ Age < 5 | 118 | 2.40 | 6.2 | 5.5 | 7.0 | 4.7 | 4.1 | 5.4 |
| 5 ≤ Age < 10 | 49 | 7.24 | 5.3 | 3.4 | 7.3 | 4.2 | 3.1 | 5.2 |
| 10 ≤ Age < 20 | 24 | 13.05 | 6.8 | 4.5 | 9.1 | 4.6 | 2.9 | 6.3 |
| without surgery | 205 | |||||||
| 0 ≤ Age < 1 | 129 | 0.32 | 2.2 | 1.9 | 2.4 | 2.7 | 2.2 | 3.1 |
| 1 ≤ Age < 5 | 33 | 2.28 | 1.9 | 1.4 | 2.4 | 4.1 | 3.0 | 5.2 |
| 5 ≤ Age < 10 | 24 | 7.05 | 2.5 | 1.7 | 3.4 | 5.4 | 4.0 | 6.8 |
| 10 ≤ Age < 20 | 19 | 12.74 | 3.1 | 1.7 | 4.5 | 7.3 | 5.2 | 9.3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoshitake, T.; Miyazaki, O.; Kitamura, M.; Ono, K.; Kai, M. Quantitative Analysis of the Clinical Reasons Influencing the Frequency of Pediatric Head CT Examinations: A Single-Center Observation Study. Tomography 2023, 9, 829-839. https://doi.org/10.3390/tomography9020067
Yoshitake T, Miyazaki O, Kitamura M, Ono K, Kai M. Quantitative Analysis of the Clinical Reasons Influencing the Frequency of Pediatric Head CT Examinations: A Single-Center Observation Study. Tomography. 2023; 9(2):829-839. https://doi.org/10.3390/tomography9020067
Chicago/Turabian StyleYoshitake, Takayasu, Osamu Miyazaki, Masayuki Kitamura, Koji Ono, and Michiaki Kai. 2023. "Quantitative Analysis of the Clinical Reasons Influencing the Frequency of Pediatric Head CT Examinations: A Single-Center Observation Study" Tomography 9, no. 2: 829-839. https://doi.org/10.3390/tomography9020067
APA StyleYoshitake, T., Miyazaki, O., Kitamura, M., Ono, K., & Kai, M. (2023). Quantitative Analysis of the Clinical Reasons Influencing the Frequency of Pediatric Head CT Examinations: A Single-Center Observation Study. Tomography, 9(2), 829-839. https://doi.org/10.3390/tomography9020067






