High-Resolution 3D versus Standard-Resolution 2D T2-Weighted Turbo Spin Echo MRI for the Assessment of Lumbar Nerve Root Compromise
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Subjects
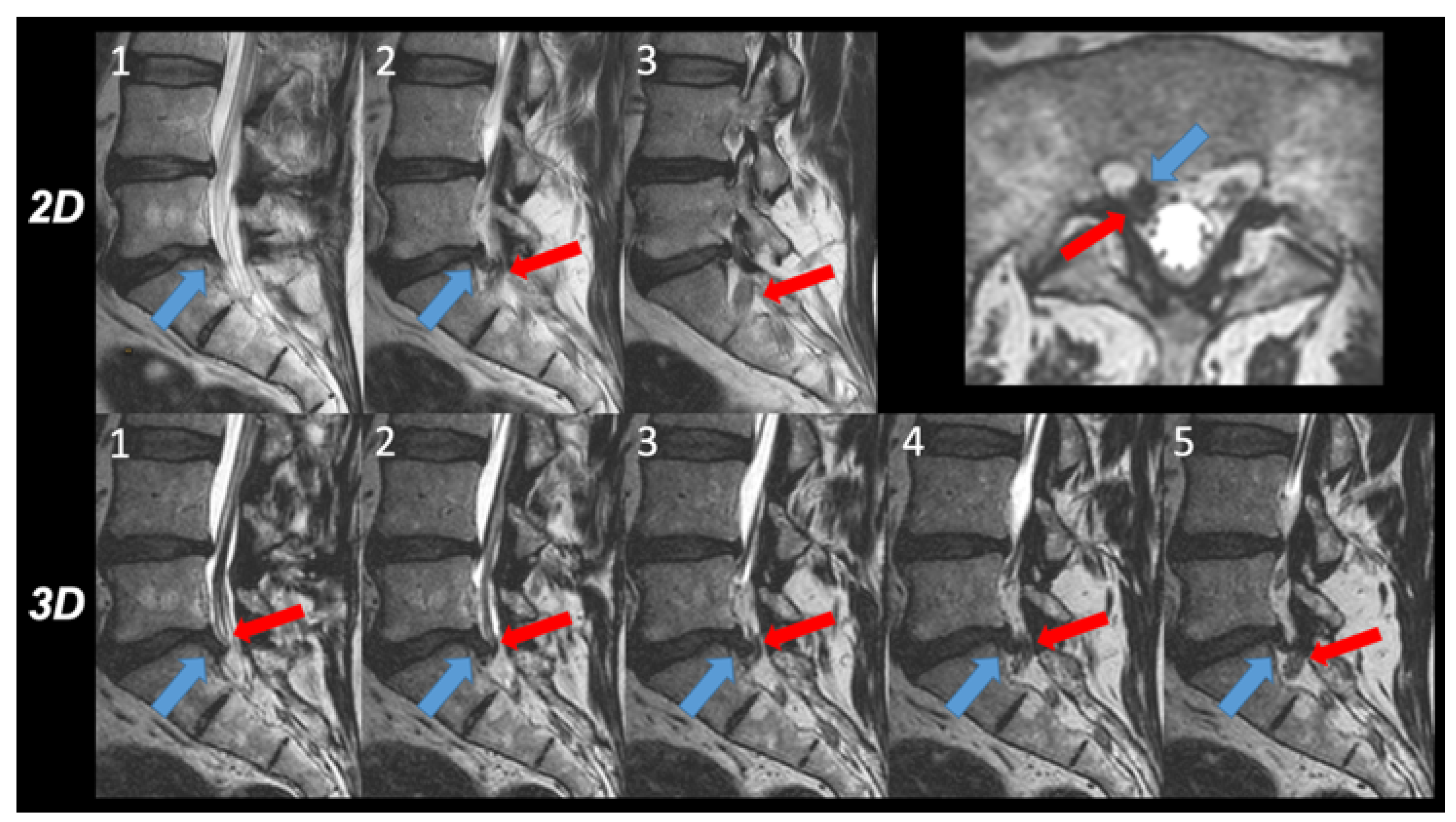
2.2. MRI Protocol
- (a)
- 2D T2w TSE sequence: acquisition sagittal, repetition time (TR) 3000 ms, echo time (TE) 100 ms, flip angle 90°, echo train length 20, number of echoes 1, FOV 160 × 270 × 65 mm, slice thickness 4 mm, acquired voxel size 0.75 × 0.95 × 4.0 mm3, reconstructed voxel size: 0.63 × 0.63 × 4.0 mm3, number of signal averages (NSA) 2.0. Acquisition time 03 min 02 s.
- (b)
- 3D T2w TSE sequence: acquisition sagittal, DRIVE pulse yes, TR 1300 ms, TE 95 ms, flip angle 90°, echo train length 50, number of echoes 1, field of view (FOV) 200 × 300 × 90 mm3, acquired voxel size 0.8 × 0.8 × 1.0 mm3, reconstructed voxel size 0.4 × 0.4 × 0.5 mm3, number of slices 180, acceleration: Compressed SENSE factor 7.0, NSA 1.0, acquisition time 04 min 46 s. This sequence was accelerated with the compressed SENSE acceleration technique that uses a variable density Poisson disk-sampling scheme followed by iterative reconstruction. A more detailed description of this acceleration technique can be found elsewhere [10,13]. The sequence was generally acquired in the sagittal plane of the section parallel to the spinal column. In patients with scoliosis, however, a secondary curved sagittal reconstruction parallel to the scoliotic lumbar vertebrae was obtained. Curved transverse reconstructions were computed parallel to the individual disc levels.
2.3. Image Evaluation
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fardon, D.F.; Williams, A.L.; Dohring, E.J.; Murtagh, F.R.; Rothman, S.L.G.; Sze, G.K. Lumbar disc nomenclature: Version 2.0: Recommendations of the combined task forces of the North American Spine Society, the American Society of Spine Radiology and the American Society of Neuroradiology. Spine J. 2014, 14, 2525–2545. [Google Scholar] [CrossRef] [Green Version]
- Wildermuth, S.; Zanetti, M.; Duewell, S.; Schmid, M.R.; Romanowski, B.; Benini, A.; Böni, T.; Hodler, J. Lumbar spine: Quantitative and qualitative assessment of positional (upright flexion and extension) MR imaging and myelography. Radiology 1998, 207, 391–398. [Google Scholar] [CrossRef]
- Stephens, M.M.; Evans, J.H.; O’Brien, J.P. Lumbar intervertebral foramens. An in vitro study of their shape in relation to intervertebral disc pathology. Spine 1991, 16, 525–529. [Google Scholar] [CrossRef]
- Kunogi, J.-I.; Hasue, M. Diagnosis and Operative Treatment of Intraforaminal and Extraforaminal Nerve Root Compression. Spine 1991, 16, 1312–1320. [Google Scholar] [CrossRef]
- Lee, S.; Lee, J.W.; Yeom, J.S.; Kim, K.-J.; Kim, H.-J.; Chung, S.K.; Kang, H.S. A Practical MRI Grading System for Lumbar Foraminal Stenosis. Am. J. Roentgenol. 2010, 194, 1095–1098. [Google Scholar] [CrossRef] [Green Version]
- Park, H.-J.; Kim, S.; Lee, S.-Y.; Park, N.-H.; Rho, M.-H.; Hong, H.-P.; Kwag, H.-J.; Kook, S.-H.; Choi, S.-H. Clinical Correlation of a New MR Imaging Method for Assessing Lumbar Foraminal Stenosis. Am. J. Neuroradiol. 2012, 33, 818–822. [Google Scholar] [CrossRef] [Green Version]
- Sartoretti, E.; Wyss, M.; Alfieri, A.; Binkert, C.A.; Erne, C.; Sartoretti-Schefer, S.; Sartoretti, T. Introduction and reproducibility of an updated practical grading system for lumbar foraminal stenosis based on high-resolution MR imaging. Sci. Rep. 2021, 11, 12000. [Google Scholar] [CrossRef]
- Pfirrmann, C.W.A.; Dora, C.; Schmid, M.R.; Zanetti, M.; Hodler, J.; Boos, N. MR Image–based Grading of Lumbar Nerve Root Compromise due to Disk Herniation: Reliability Study with Surgical Correlation. Radiology 2004, 230, 583–588. [Google Scholar] [CrossRef]
- Bratke, G.; Rau, R.; Weiss, K.; Kabbasch, C.; Sircar, K.; Morelli, J.N.; Persigehl, T.; Maintz, D.; Giese, D.; Haneder, S. Accelerated MRI of the Lumbar Spine Using Compressed Sensing: Quality and Efficiency. J. Magn. Reson. Imaging 2019, 49, e164–e175. [Google Scholar] [CrossRef]
- Sartoretti, T.; Sartoretti, E.; Wyss, M.; Schwenk, Á.; van Smoorenburg, L.; Eichenberger, B.; Najafi, A.; Binkert, C.; Becker, A.S.; Sartoretti-Schefer, S. Compressed SENSE accelerated 3D T1w black blood turbo spin echo versus 2D T1w turbo spin echo sequence in pituitary magnetic resonance imaging. Eur. J. Radiol. 2019, 120, 108667. [Google Scholar] [CrossRef]
- Sartoretti, E.; Sartoretti, T.; Binkert, C.; Najafi, A.; Schwenk, Á.; Hinnen, M.; Van Smoorenburg, L.; Eichenberger, B.; Sartoretti-Schefer, S. Reduction of procedure times in routine clinical practice with Compressed SENSE magnetic resonance imaging technique. PLoS ONE 2019, 14, e0214887. [Google Scholar] [CrossRef]
- Lustig, M.; Donoho, D.; Pauly, J.M. Sparse MRI: The application of compressed sensing for rapid MR imaging. Magn. Reson. Med. 2007, 58, 1182–1195. [Google Scholar] [CrossRef]
- Vranic, J.; Cross, N.; Wang, Y.; Hippe, D.; De Weerdt, E.; Mossa-Basha, M. Compressed Sensing–Sensitivity Encoding (CS-SENSE) Accelerated Brain Imaging: Reduced Scan Time without Reduced Image Quality. Am. J. Neuroradiol. 2019, 40, 92–98. [Google Scholar] [CrossRef] [Green Version]
- Wu, A.; March, L.; Zheng, X.; Huang, J.; Wang, X.; Zhao, J.; Blyth, F.M.; Smith, E.; Buchbinder, R.; Hoy, D. Global low back pain prevalence and years lived with disability from 1990 to 2017: Estimates from the Global Burden of Disease Study 2017. Ann. Transl. Med. 2020, 8, 299. [Google Scholar] [CrossRef]
- Orita, S.; Inage, K.; Eguchi, Y.; Kubota, G.; Aoki, Y.; Nakamura, J.; Matsuura, Y.; Furuya, T.; Koda, M.; Ohtori, S. Lumbar foraminal stenosis, the hidden stenosis including at L5/S1. Eur. J. Orthop. Surg. Traumatol. 2016, 26, 685–693. [Google Scholar] [CrossRef]
- Jenis, L.G.; An, H.S. Spine Update. Lumbar foraminal stenosis. Spine 2000, 25, 389–394. [Google Scholar] [CrossRef]
- Lee, S.; Jee, W.-H.; Jung, J.-Y.; Lee, S.-Y.; Ryu, K.-S.; Ha, K.-Y. MRI of the lumbar spine: Comparison of 3D isotropic turbo spin-echo SPACE sequence versus conventional 2D sequences at 3.0 T. Acta Radiol. 2015, 56, 174–181. [Google Scholar] [CrossRef]
- Sung, J.; Jee, W.-H.; Jung, J.-Y.; Jang, J.; Kim, J.-S.; Kim, Y.-H.; Ha, K.-Y. Diagnosis of Nerve Root Compromise of the Lumbar Spine: Evaluation of the Performance of Three-dimensional Isotropic T2-weighted Turbo Spin-Echo SPACE Sequence at 3T. Korean J. Radiol. 2017, 18, 249–259. [Google Scholar] [CrossRef] [Green Version]
- Kong, C.; Li, X.-Y.; Sun, S.-Y.; Sun, X.-Y.; Zhang, M.; Sun, Z.; Wang, Y.; Lu, J.; Lu, S.-B. The value of contrast-enhanced three-dimensional isotropic T2-weighted turbo spin-echo SPACE sequence in the diagnosis of patients with lumbosacral nerve root compression. Eur. Spine J. 2021, 30, 855–864. [Google Scholar] [CrossRef]
- Sayah, A.; Jay, A.K.; Toaff, J.S.; Makariou, E.V.; Berkowitz, F. Effectiveness of a Rapid Lumbar Spine MRI Protocol Using 3D T2-Weighted SPACE Imaging Versus a Standard Protocol for Evaluation of Degenerative Changes of the Lumbar Spine. Am. J. Roentgenol. 2016, 207, 614–620. [Google Scholar] [CrossRef]
- Hossein, J.; Fariborz, F.; Mehrnaz, R.; Babak, R. Evaluation of diagnostic value and T2-weighted three-dimensional isotropic turbo spin-echo (3D-SPACE) image quality in comparison with T2-weighted two-dimensional turbo spin-echo (2D-TSE) sequences in lumbar spine MR imaging. Eur. J. Radiol. Open 2019, 6, 36–41. [Google Scholar] [CrossRef] [Green Version]
- Eichinger, P.; Hock, A.; Schön, S.; Preibisch, C.; Kirschke, J.S.; Mühlau, M.; Zimmer, C.; Wiestler, B. Acceleration of Double Inversion Recovery Sequences in Multiple Sclerosis with Compressed Sensing. Investig. Radiol. 2019, 54, 319–324. [Google Scholar] [CrossRef]
- Mugler, J.P. Optimized three-dimensional fast-spin-echo MRI. J. Magn. Reson. Imaging 2014, 39, 745–767. [Google Scholar] [CrossRef]
- Csutak, C.; Ștefan, P.-A.; Lenghel, L.; Moroșanu, C.; Lupean, R.-A.; Șimonca, L.; Mihu, C.; Lebovici, A. Differentiating High-Grade Gliomas from Brain Metastases at Magnetic Resonance: The Role of Texture Analysis of the Peritumoral Zone. Brain Sci. 2020, 10, 638. [Google Scholar] [CrossRef]
- Lambin, P.; Leijenaar, R.T.H.; Deist, T.M.; Peerlings, J.; de Jong, E.E.C.; van Timmeren, J.; Sanduleanu, S.; Larue, R.T.H.M.; Even, A.J.G.; Jochems, A.; et al. Radiomics: The bridge between medical imaging and personalized medicine. Nat. Rev. Clin. Oncol. 2017, 14, 749–762. [Google Scholar] [CrossRef]
- Kim, D.; Jensen, L.J.; Elgeti, T.; Steffen, I.G.; Hamm, B.; Nagel, S.N. Radiomics for Everyone: A New Tool Simplifies Creating Parametric Maps for the Visualization and Quantification of Radiomics Features. Tomography 2021, 7, 477–487. [Google Scholar] [CrossRef]
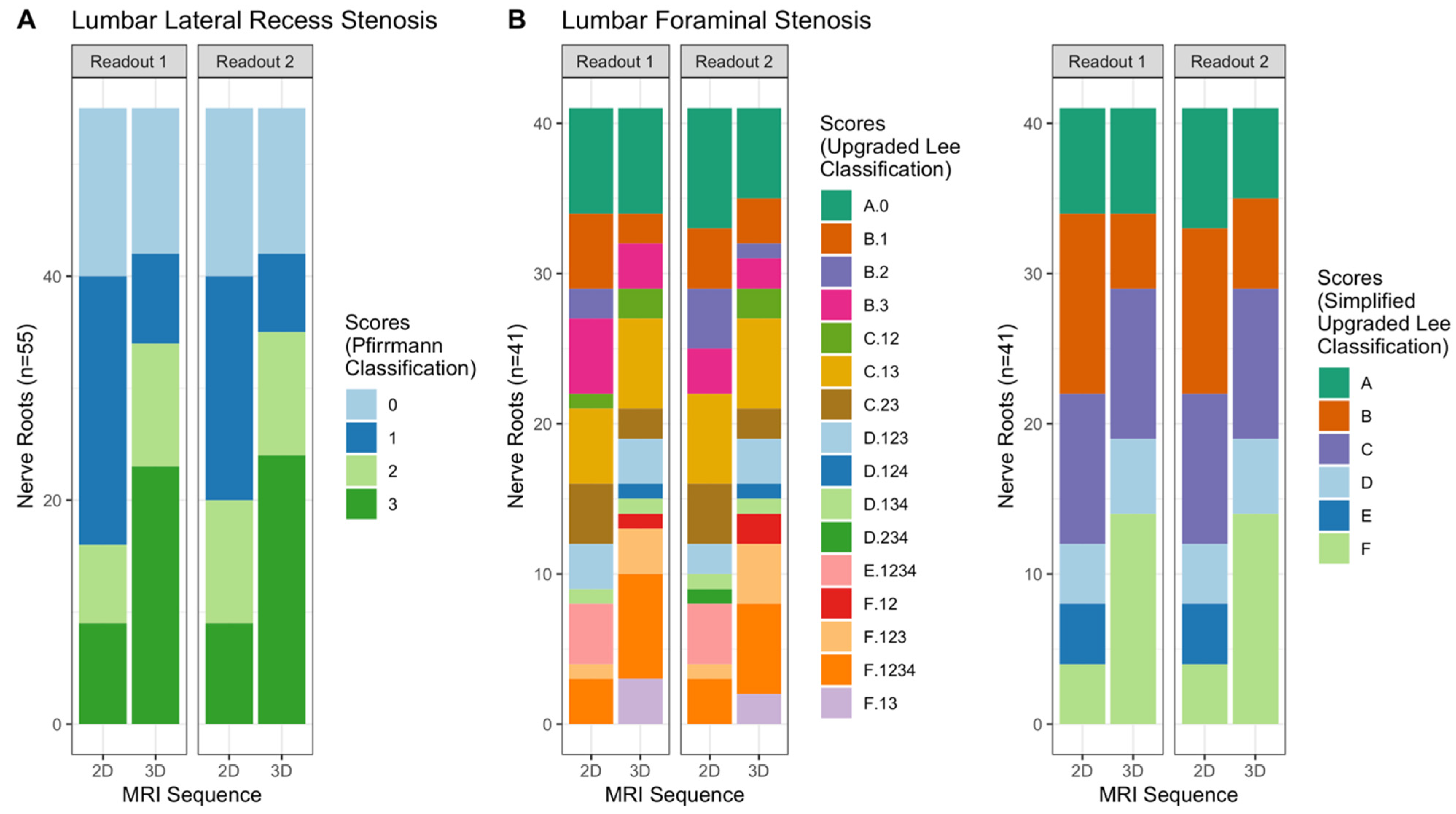

| Readout 1 | Readout 2 | |||
|---|---|---|---|---|
| 2D T2w TSE | 3D T2w TSE | 2D T2w TSE | 3D T2w TSE | |
| Lumbar Lateral Recess Stenosis (n = 55) | Grade 0: 15 (27.3%) | Grade 0: 13 (23.6%) | Grade 0: 15 (27.3%) | Grade 0: 13 (23.6%) |
| Grade 1: 24 (43.6%) | Grade 1: 8 (14.5%) | Grade 1: 20 (36.4%) | Grade 1: 7 (12.7%) | |
| Grade 2: 7 (12.7%) | Grade 2: 11 (20%) | Grade 2: 11 (20%) | Grade 2: 11 (20%) | |
| Grade 3: 9 (16.4%) | Grade 3: 23 (41.8%) | Grade 3: 9 (16.4%) | Grade 3: 24 (43.6%) | |
| Lumbar Foraminal Stenosis (n = 41) | Grade A: 7 (17.1%) | Grade A: 7 (17.1%) | Grade A: 8 (19.5%) | Grade A: 6 (14.6%) |
| Grade B: 12 (29.3%) | Grade B: 5 (12.2%) | Grade B: 11 (26.8%) | Grade B: 6 (14.6%) | |
| Grade C: 10 (24.4%) | Grade C: 10 (24.4%) | Grade C: 10 (24.4%) | Grade C: 10 (24.4%) | |
| Grade D: 4 (9.8%) | Grade D: 5 (12.2%) | Grade D: 4 (9.8%) | Grade D: 5 (12.2%) | |
| Grade E: 4 (9.8%) | Grade E: 0 (0%) | Grade E: 4 (9.8%) | Grade E: 0 (0%) | |
| Grade F: 4 (9.8%) | Grade F: 14 (34.1%) | Grade F: 4 (9.8%) | Grade F: 14 (34.1%) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sartoretti, E.; Sartoretti, T.; Schwenk, Á.; Alfieri, A.; Czell, D.; Wyss, M.; Wildi, L.; Binkert, C.A.; Sartoretti-Schefer, S. High-Resolution 3D versus Standard-Resolution 2D T2-Weighted Turbo Spin Echo MRI for the Assessment of Lumbar Nerve Root Compromise. Tomography 2022, 8, 257-266. https://doi.org/10.3390/tomography8010020
Sartoretti E, Sartoretti T, Schwenk Á, Alfieri A, Czell D, Wyss M, Wildi L, Binkert CA, Sartoretti-Schefer S. High-Resolution 3D versus Standard-Resolution 2D T2-Weighted Turbo Spin Echo MRI for the Assessment of Lumbar Nerve Root Compromise. Tomography. 2022; 8(1):257-266. https://doi.org/10.3390/tomography8010020
Chicago/Turabian StyleSartoretti, Elisabeth, Thomas Sartoretti, Árpád Schwenk, Alex Alfieri, David Czell, Michael Wyss, Lukas Wildi, Christoph A. Binkert, and Sabine Sartoretti-Schefer. 2022. "High-Resolution 3D versus Standard-Resolution 2D T2-Weighted Turbo Spin Echo MRI for the Assessment of Lumbar Nerve Root Compromise" Tomography 8, no. 1: 257-266. https://doi.org/10.3390/tomography8010020
APA StyleSartoretti, E., Sartoretti, T., Schwenk, Á., Alfieri, A., Czell, D., Wyss, M., Wildi, L., Binkert, C. A., & Sartoretti-Schefer, S. (2022). High-Resolution 3D versus Standard-Resolution 2D T2-Weighted Turbo Spin Echo MRI for the Assessment of Lumbar Nerve Root Compromise. Tomography, 8(1), 257-266. https://doi.org/10.3390/tomography8010020






