The Effect of Argon Plasma Surface Treatment on Poly(lactic-co-glycolic acid)/Collagen-Based Biomaterials for Bone Tissue Engineering
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Sample Preparation
2.2.1. Solvent Casting
2.2.2. Three-Dimensional Bioplotting
2.3. Argon Plasma Surface Modification
2.4. Thermogravimetric Analysis
2.5. Differential Scanning Calorimetry
2.6. Contact Angle and Surface Energy Measurements
2.7. Bicinchoninic Acid Assay
2.8. Scanning Electron Microscopy
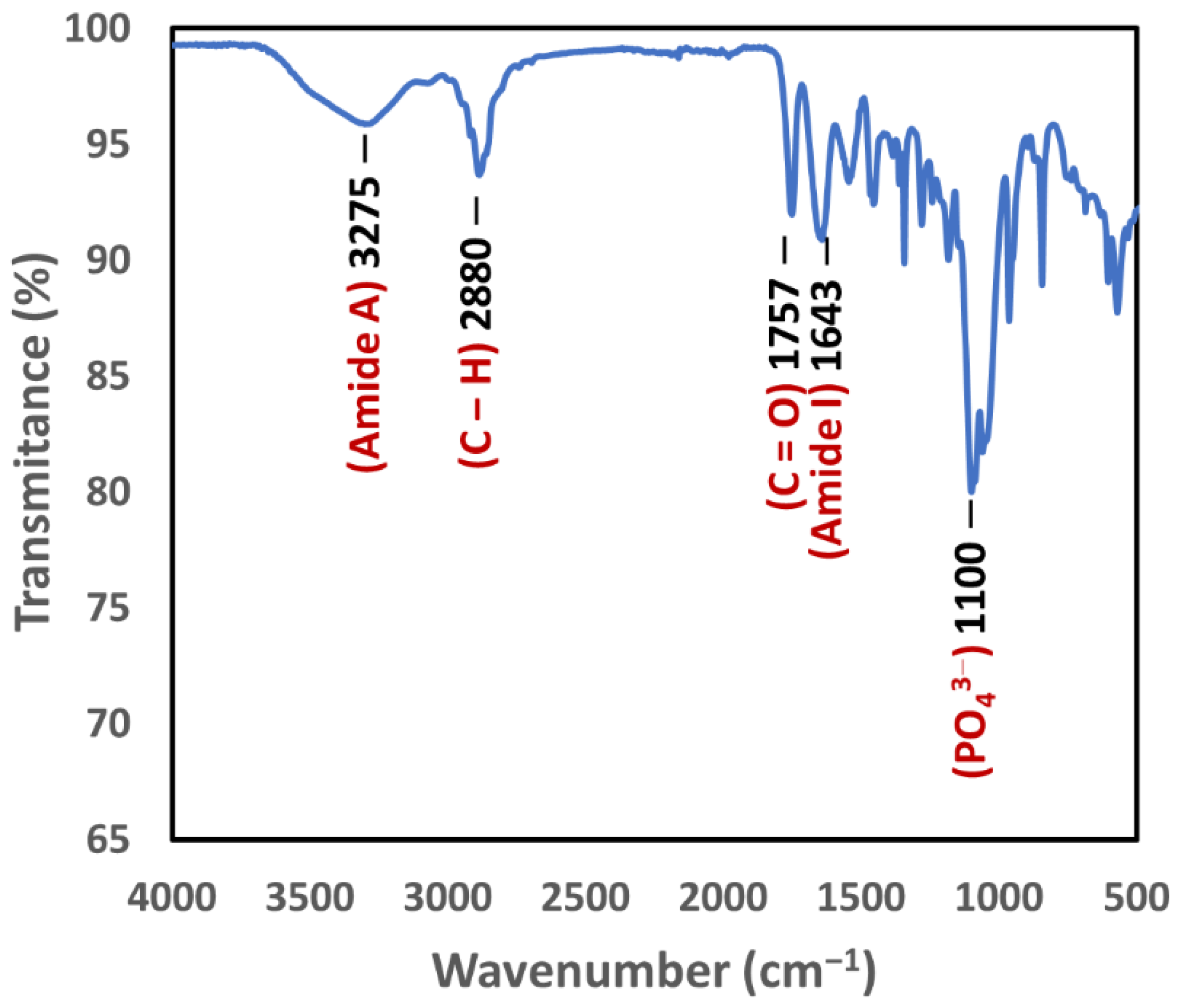
2.9. Fourier-Transform Infrared Spectroscopy
2.10. Statistical Analysis
3. Results
3.1. Prepared Films and Scaffolds
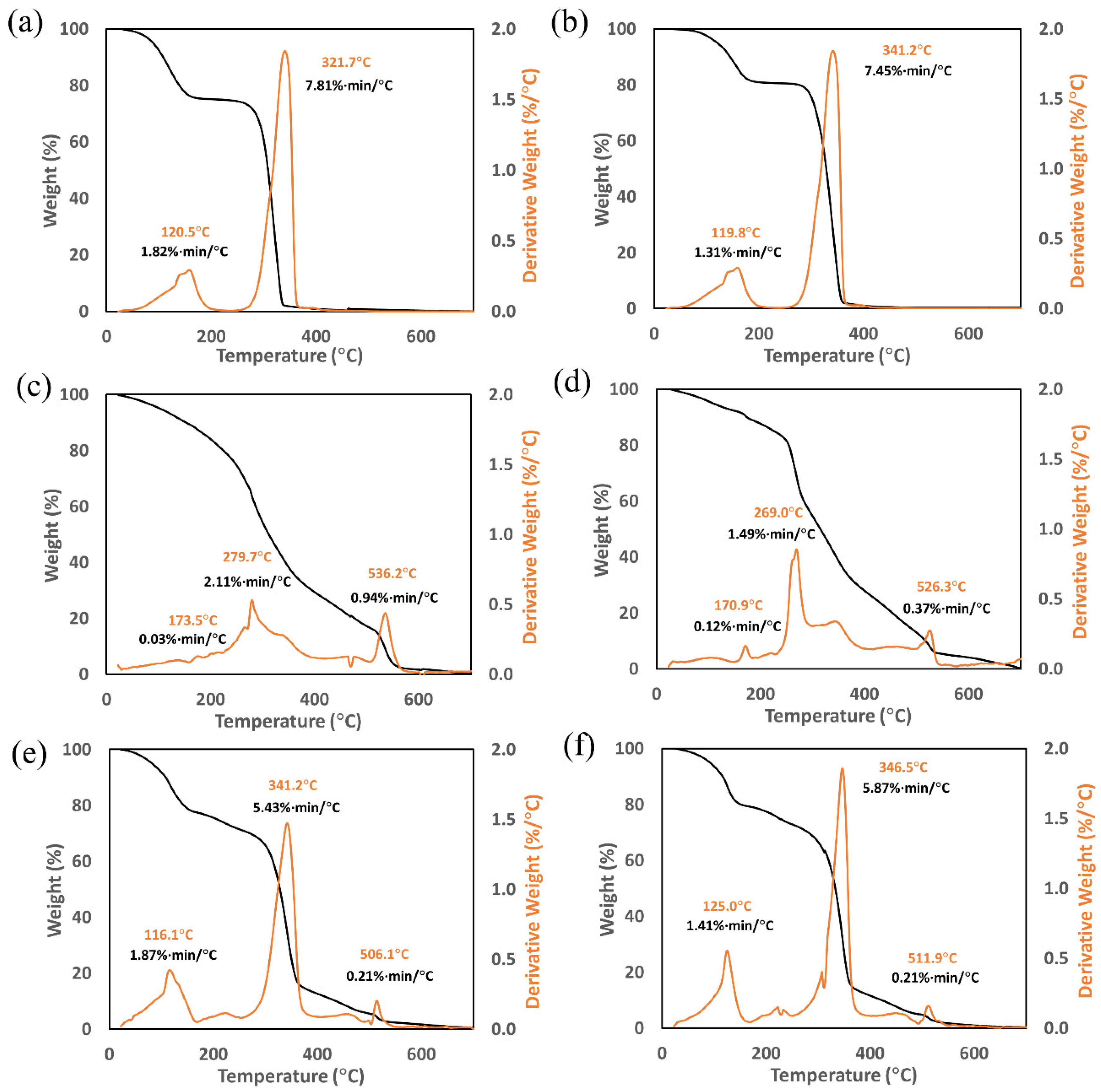
3.2. Thermogravimetric Analysis
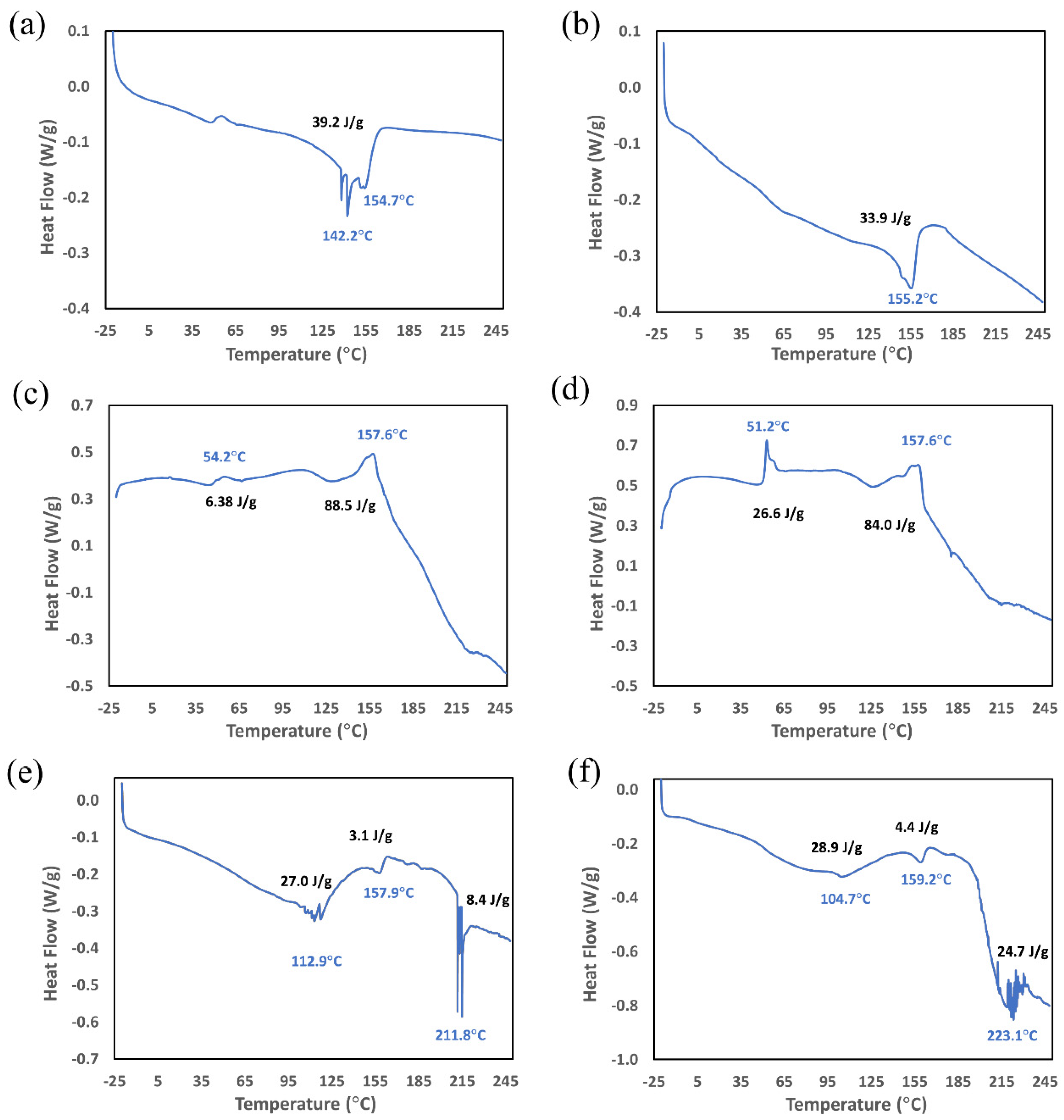
3.3. Differential Scanning Calorimetry
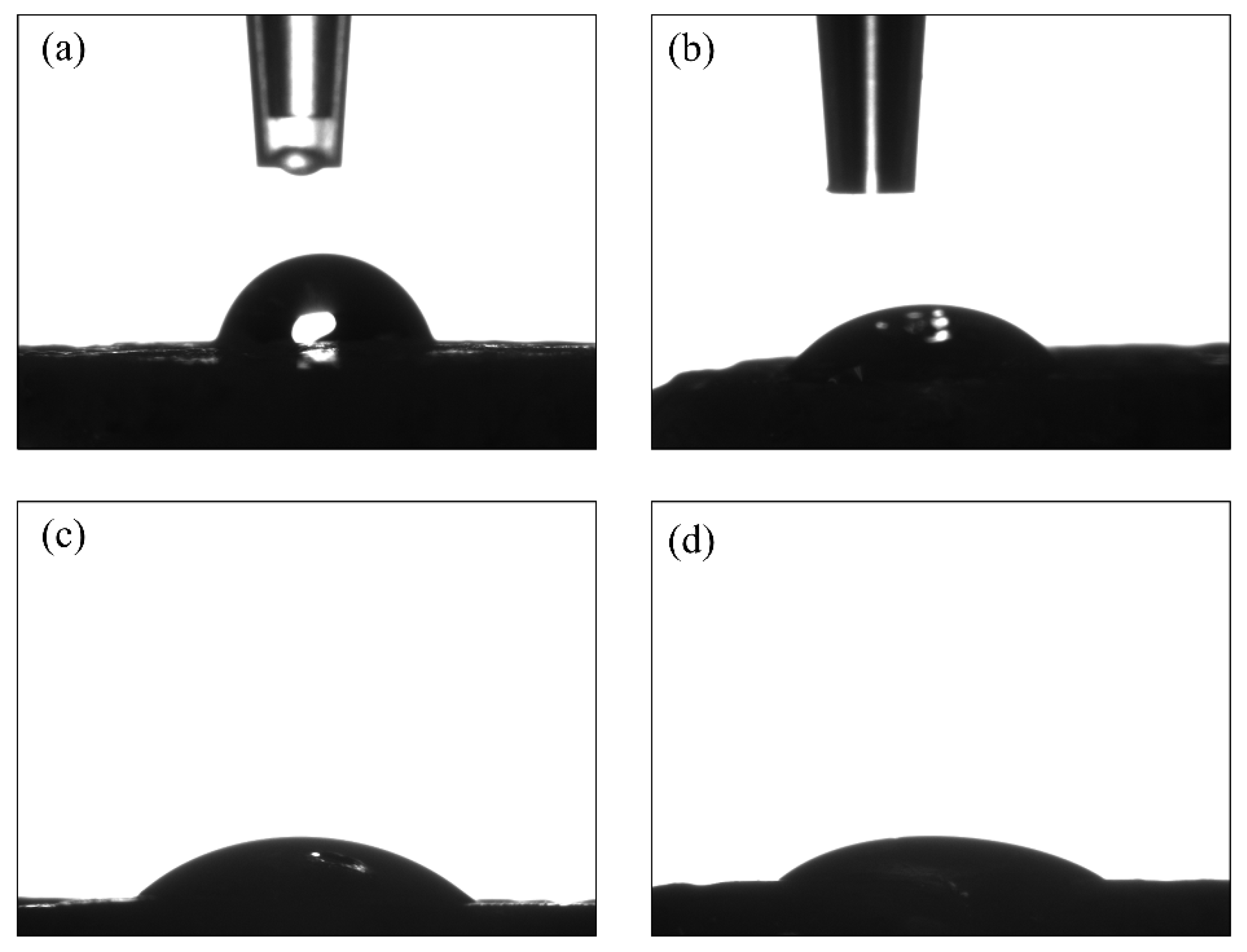
3.4. Contact Angle Measurements
3.5. Critical Surface Tension (Surface Energy)
3.6. Fourier-Transform Infrared Spectroscopy
3.7. Bicinchoninic Acid Assay
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Amini, A.R.; Laurencin, C.T.; Nukavarapu, S.P. Bone tissue engineering: Recent advances and challenges. Crit. Rev. Biomed. Eng. 2012, 40, 363–408. [Google Scholar] [CrossRef] [PubMed]
- Ho-Shui-Ling, A.; Bolander, J.; Rustom, L.E.; Johnson, A.W.; Luyten, F.P.; Picart, C. Bone regeneration strategies: Engineered scaffolds, bioactive molecules and stem cells current stage and future perspectives. Biomaterials 2018, 180, 143–162. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, R.; García, A.J. Biomaterial strategies for engineering implants for enhanced osseointegration and bone repair. Adv. Drug Deliv. Rev. 2015, 94, 53–62. [Google Scholar] [CrossRef]
- Antmen, E.; Vrana, N.E.; Hasirci, V. The role of biomaterials and scaffolds in immune responses in regenerative medicine: Macrophage phenotype modulation by biomaterial properties and scaffold architectures. Biomater. Sci. 2021, 9, 8090–8110. [Google Scholar] [CrossRef] [PubMed]
- Song, J.E.; Lee, D.H.; Choi, J.H.; Lee, S.W.; Khang, G.; Yoon, S.-J. Biomimetic sponge using duck’s feet derived collagen and hydroxyapatite to promote bone regeneration. J. Biomater. Sci. Polym. Ed. 2022, 33, 769–782. [Google Scholar] [CrossRef]
- Binlateh, T.; Thammanichanon, P.; Rittipakorn, P.; Thinsathid, N.; Jitprasertwong, P. Collagen-Based Biomaterials in Periodontal Regeneration: Current Applications and Future Perspectives of Plant-Based Collagen. Biomimetics 2022, 7, 34. [Google Scholar] [CrossRef]
- Campana, V.; Milano, G.; Pagano, E.; Barba, M.; Cicione, C.; Salonna, G.; Lattanzi, W.; Logroscino, G. Bone substitutes in orthopaedic surgery: From basic science to clinical practice. J. Mater. Sci. Mater. Med. 2014, 25, 2445–2461. [Google Scholar] [CrossRef]
- Lee, J.C.; Pereira, C.T.; Ren, X.; Huang, W.; Bischoff, D.; Weisgerber, D.W.; Yamaguchi, D.T.; Harley, B.A.; Miller, T.A. Optimizing Collagen Scaffolds for Bone Engineering: Effects of Cross-linking and Mineral Content on Structural Contraction and Osteogenesis. J. Craniofac. Surg. 2015, 26, 1992–1996. [Google Scholar] [CrossRef]
- Seong, Y.-J.; Song, E.-H.; Park, C.; Lee, H.; Kang, I.-G.; Kim, H.-E.; Jeong, S.-H. Porous calcium phosphate-collagen composite microspheres for effective growth factor delivery and bone tissue regeneration. Mater. Sci. Eng. C Mater. Biol. Appl. 2020, 109, 110480. [Google Scholar] [CrossRef]
- Jin, S.; Xia, X.; Huang, J.; Yuan, C.; Zuo, Y.; Li, Y.; Li, J. Recent advances in PLGA-based biomaterials for bone tissue regeneration. Acta Biomater. 2021, 127, 56–79. [Google Scholar] [CrossRef]
- Yang, J.; Bei, J.; Wang, S. Enhanced cell affinity of poly (D,L-lactide) by combining plasma treatment with collagen anchorage. Biomaterials 2002, 23, 2607–2614. [Google Scholar] [CrossRef]
- Wan, Y.; Qu, X.; Lu, J.; Zhu, C.; Wan, L.; Yang, J.; Bei, J.; Wang, S. Characterization of surface property of poly(lactide-co-glycolide) after oxygen plasma treatment. Biomaterials 2004, 25, 4777–4783. [Google Scholar] [CrossRef]
- Jelil, R.A. A review of low-temperature plasma treatment of textile materials. J. Mater. Sci. 2015, 50, 5913–5943. [Google Scholar] [CrossRef]
- Slepička, P.; Trostová, S.; Slepičková Kasálková, N.; Kolská, Z.; Sajdl, P.; Švorčík, V. Surface Modification of Biopolymers by Argon Plasma and Thermal Treatment. Plasma Process. Polym. 2012, 9, 197–206. [Google Scholar] [CrossRef]
- Griffin, M.; Palgrave, R.; Baldovino-Medrano, V.G.; Butler, P.E.; Kalaskar, D.M. Argon plasma improves the tissue integration and angiogenesis of subcutaneous implants by modifying surface chemistry and topography. Int. J. Nanomed. 2018, 13, 6123–6141. [Google Scholar] [CrossRef]
- Mozaffari, A.; Parvinzadeh Gashti, M.; Mirjalili, M.; Parsania, M. Argon and Argon-Oxygen Plasma Surface Modification of Gelatin Nanofibers for Tissue Engineering Applications. Membranes 2021, 11, 31. [Google Scholar] [CrossRef]
- Cao, Y.; Croll, T.I.; Cooper-White, J.J.; O’ Connor, A.J.; Stevens, G.W. Production and Surface Modification of Polylactide-Based Polymeric Scaffolds for Soft-Tissue Engineering. In Biopolymer Methods in Tissue Engineering; Hollander, A.P., Hatton, P.V., Eds.; Humana Press: Totowa, NJ, USA, 2004; pp. 87–111. ISBN 978-1-59259-428-3. [Google Scholar]
- Kabza, K.G.; Gestwicki, J.E.; McGrath, J.L. Contact Angle Goniometry as a Tool for Surface Tension Measurements of Solids, Using Zisman Plot Method. A Physical Chemistry Experiment. J. Chem. Educ. 2000, 77, 63. [Google Scholar] [CrossRef]
- Zdziennicka, A.; Szymczyk, K.; Krawczyk, J.; Jańczuk, B. Some remarks on the solid surface tension determination from contact angle measurements. Appl. Surf. Sci. 2017, 405, 88–101. [Google Scholar] [CrossRef]
- Uth, N.; Mueller, J.; Smucker, B.; Yousefi, A.-M. Validation of scaffold design optimization in bone tissue engineering: Finite element modeling versus designed experiments. Biofabrication 2017, 9, 015023. [Google Scholar] [CrossRef]
- Chen, G.; Ushida, T.; Tateishi, T. Poly(DL-lactic-co-glycolic acid) sponge hybridized with collagen microsponges and deposited apatite particulates. J. Biomed. Mater. Res. 2001, 57, 8–14. [Google Scholar] [CrossRef]
- Liu, X.; Ma, P.X. Polymeric scaffolds for bone tissue engineering. Ann. Biomed. Eng. 2004, 32, 477–486. [Google Scholar] [CrossRef] [PubMed]
- Hatakeyama, W.; Taira, M.; Sawada, T.; Hoshi, M.; Hachinohe, Y.; Sato, H.; Takafuji, K.; Kihara, H.; Takemoto, S.; Kondo, H. Bone Regeneration of Critical-Size Calvarial Defects in Rats Using Highly Pressed Nano-Apatite/Collagen Composites. Materials 2022, 15, 3376. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-S.; Sun Park, M.; Jeon, O.; Yong Choi, C.; Kim, B.-S. Poly(lactide-co-glycolide)/hydroxyapatite composite scaffolds for bone tissue engineering. Biomaterials 2006, 27, 1399–1409. [Google Scholar] [CrossRef] [PubMed]
- Baino, F.; Yamaguchi, S. The Use of Simulated Body Fluid (SBF) for Assessing Materials Bioactivity in the Context of Tissue Engineering: Review and Challenges. Biomimetics 2020, 5, 57. [Google Scholar] [CrossRef]
- Shaikh, M.S.; Zafar, M.S.; Alnazzawi, A. Comparing Nanohydroxyapatite Graft and Other Bone Grafts in the Repair of Periodontal Infrabony Lesions: A Systematic Review and Meta-Analysis. Int. J. Mol. Sci. 2021, 22, 2021. [Google Scholar] [CrossRef]
- Schnettler, R.; Stahl, J.P.; Alt, V.; Pavlidis, T.; Dingeldein, E.; Wenisch, S. Calcium Phosphate-Based Bone Substitutes. Eur. J. Trauma 2004, 30, 219–229. [Google Scholar] [CrossRef]
- Rekik, S.B.; Gassara, S.; Bouaziz, J.; Deratani, A.; Baklouti, S. Enhancing hydrophilicity and permeation flux of chitosan/kaolin composite membranes by using polyethylene glycol as porogen. Appl. Clay Sci. 2019, 168, 312–323. [Google Scholar] [CrossRef]
- El-Ayoubi, R.; Eliopoulos, N.; Diraddo, R.; Galipeau, J.; Yousefi, A.-M. Design and fabrication of 3D porous scaffolds to facilitate cell-based gene therapy. Tissue Eng. Part A 2008, 14, 1037–1048. [Google Scholar] [CrossRef]
- Coutu, D.L.; Cuerquis, J.; El Ayoubi, R.; Forner, K.-A.; Roy, R.; François, M.; Griffith, M.; Lillicrap, D.; Yousefi, A.M.; Blostein, M.D.; et al. Hierarchical scaffold design for mesenchymal stem cell-based gene therapy of hemophilia B. Biomaterials 2011, 32, 295–305. [Google Scholar] [CrossRef]
- Smith, P.K.; Krohn, R.I.; Hermanson, G.T.; Mallia, A.K.; Gartner, F.H.; Provenzano, M.D.; Fujimoto, E.K.; Goeke, N.M.; Olson, B.J.; Klenk, D.C. Measurement of protein using bicinchoninic acid. Anal. Biochem. 1985, 150, 76–85. [Google Scholar] [CrossRef]
- Dolci, L.S.; Liguori, A.; Panzavolta, S.; Miserocchi, A.; Passerini, N.; Gherardi, M.; Colombo, V.; Bigi, A.; Albertini, B. Non-equilibrium atmospheric pressure plasma as innovative method to crosslink and enhance mucoadhesion of econazole-loaded gelatin films for buccal drug delivery. Colloids Surf. B Biointerfaces 2018, 163, 73–82. [Google Scholar] [CrossRef]
- Holy, C.E.; Cheng, C.; Davies, J.E.; Shoichet, M.S. Optimizing the sterilization of PLGA scaffolds for use in tissue engineering. Biomaterials 2001, 22, 25–31. [Google Scholar] [CrossRef]
- Walker, J.M. The Bicinchoninic Acid (BCA) Assay for Protein Quantitation BT—The Protein Protocols Handbook; Walker, J.M., Ed.; Humana Press: Totowa, NJ, USA, 2009; pp. 11–15. ISBN 978-1-59745-198-7. [Google Scholar]
- Huang, T.; Long, M.; Huo, B. Competitive Binding to Cuprous Ions of Protein and BCA in the Bicinchoninic Acid Protein Assay. Open Biomed. Eng. J. 2010, 4, 271–278. [Google Scholar] [CrossRef]
- Gulley-Stahl, H.J.; Haas, J.A.; Schmidt, K.A.; Evan, A.P.; Sommer, A.J. Attenuated total internal reflection Fourier transform infrared spectroscopy: A quantitative approach for kidney stone analysis. Appl. Spectrosc. 2009, 63, 759–766. [Google Scholar] [CrossRef]
- Gauza-Włodarczyk, M.; Kubisz, L.; Mielcarek, S.; Włodarczyk, D. Comparison of thermal properties of fish collagen and bovine collagen in the temperature range 298–670 K. Mater. Sci. Eng. C 2017, 80, 468–471. [Google Scholar] [CrossRef]
- Lu, B.; Lv, X.; Le, Y. Chitosan-Modified PLGA Nanoparticles for Control-Released Drug Delivery. Polymers 2019, 11, 304. [Google Scholar] [CrossRef]
- de Campos Vidal, B.; Mello, M.L.S. Collagen type I amide I band infrared spectroscopy. Micron 2011, 42, 283–289. [Google Scholar] [CrossRef]
- Shaltout, A.A.; Allam, M.A.; Moharram, M.A. FTIR spectroscopic, thermal and XRD characterization of hydroxyapatite from new natural sources. Spectrochim. Acta Part A Mol. Biomol. Spectrosc. 2011, 83, 56–60. [Google Scholar] [CrossRef]
- García, J.L.; Asadinezhad, A.; Pacherník, J.; Lehocký, M.; Junkar, I.; Humpolícek, P.; Sáha, P.; Valásek, P. Cell proliferation of HaCaT keratinocytes on collagen films modified by argon plasma treatment. Molecules 2010, 15, 2845–2856. [Google Scholar] [CrossRef]
- Donate, R.; Alemán-Domínguez, M.E.; Monzón, M. On the Effectiveness of Oxygen Plasma and Alkali Surface Treatments to Modify the Properties of Polylactic Acid Scaffolds. Polymers 2021, 13, 1643. [Google Scholar] [CrossRef]
- Ferreira, B.M.P.; Pinheiro, L.M.P.; Nascente, P.A.P.; Ferreira, M.J.; Duek, E.A.R. Plasma surface treatments of poly(l-lactic acid) (PLLA) and poly(hydroxybutyrate-co-hydroxyvalerate) (PHBV). Mater. Sci. Eng. C 2009, 29, 806–813. [Google Scholar] [CrossRef]
- Cheng, Q.; Lee, B.L.-P.; Komvopoulos, K.; Yan, Z.; Li, S. Plasma surface chemical treatment of electrospun poly(L-lactide) microfibrous scaffolds for enhanced cell adhesion, growth, and infiltration. Tissue Eng. Part A 2013, 19, 1188–1198. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, S.; Hagiwara, K.; Hasebe, T.; Hotta, A. Surface modification of polymers by plasma treatments for the enhancement of biocompatibility and controlled drug release. Surf. Coat. Technol. 2013, 233, 99–107. [Google Scholar] [CrossRef]
- Khorasani, M.T.; Mirzadeh, H.; Irani, S. Plasma surface modification of poly (l-lactic acid) and poly (lactic-co-glycolic acid) films for improvement of nerve cells adhesion. Radiat. Phys. Chem. 2008, 77, 280–287. [Google Scholar] [CrossRef]
- Richbourg, N.R.; Peppas, N.A.; Sikavitsas, V.I. Tuning the biomimetic behavior of scaffolds for regenerative medicine through surface modifications. J. Tissue Eng. Regen. Med. 2019, 13, 1275–1293. [Google Scholar] [CrossRef]
- Law, J.X.; Liau, L.L.; Saim, A.; Yang, Y.; Idrus, R. Electrospun Collagen Nanofibers and Their Applications in Skin Tissue Engineering. Tissue Eng. Regen. Med. 2017, 14, 699–718. [Google Scholar] [CrossRef]
- Griffin, M.F.; Ibrahim, A.; Seifalian, A.M.; Butler, P.E.M.; Kalaskar, D.M.; Ferretti, P. Argon plasma modification promotes adipose derived stem cells osteogenic and chondrogenic differentiation on nanocomposite polyurethane scaffolds; implications for skeletal tissue engineering. Mater. Sci. Eng. C 2019, 105, 110085. [Google Scholar] [CrossRef]
- Krok-Borkowicz, M.; Reczyńska, K.; Rumian, Ł.; Menaszek, E.; Orzelski, M.; Malisz, P.; Silmanowicz, P.; Dobrzyński, P.; Pamuła, E. Surface-Modified Poly(l-lactide-co-glycolide) Scaffolds for the Treatment of Osteochondral Critical Size Defects-In Vivo Studies on Rabbits. Int. J. Mol. Sci. 2020, 21, 7541. [Google Scholar] [CrossRef]
- MacDonald, D.E.; Deo, N.; Markovic, B.; Stranick, M.; Somasundaran, P. Adsorption and dissolution behavior of human plasma fibronectin on thermally and chemically modified titanium dioxide particles. Biomaterials 2002, 23, 1269–1279. [Google Scholar] [CrossRef]
- Canullo, L.; Genova, T.; Tallarico, M.; Gautier, G.; Mussano, F.; Botticelli, D. Plasma of Argon Affects the Earliest Biological Response of Different Implant Surfaces: An In Vitro Comparative Study. J. Dent. Res. 2016, 95, 566–573. [Google Scholar] [CrossRef]
- Carossa, M.; Cavagnetto, D.; Mancini, F.; Mosca Balma, A.; Mussano, F. Plasma of Argon Treatment of the Implant Surface, Systematic Review of In Vitro Studies. Biomolecules 2022, 12, 1219. [Google Scholar] [CrossRef]
- Asadian, M.; Dhaenens, M.; Onyshchenko, I.; De Waele, S.; Declercq, H.; Cools, P.; Devreese, B.; Deforce, D.; Morent, R.; De Geyter, N. Plasma Functionalization of Polycaprolactone Nanofibers Changes Protein Interactions with Cells, Resulting in Increased Cell Viability. ACS Appl. Mater. Interfaces 2018, 10, 41962–41977. [Google Scholar] [CrossRef]
- Dave, K.; Mahmud, Z.; Gomes, V.G. Superhydrophilic 3D-printed scaffolds using conjugated bioresorbable nanocomposites for enhanced bone regeneration. Chem. Eng. J. 2022, 445, 136639. [Google Scholar] [CrossRef]
- Ayyoob, M.; Kim, Y.J. Effect of Chemical Composition Variant and Oxygen Plasma Treatments on the Wettability of PLGA Thin Films, Synthesized by Direct Copolycondensation. Polymers 2018, 10, 1132. [Google Scholar] [CrossRef]
- Silva, M.F.; Hechenleitner, A.A.W.; Irache, J.M.; Oliveira, A.J.A.D.; Pineda, E.A.G. Study of thermal degradation of PLGA, PLGA nanospheres and PLGA/maghemite superparamagnetic nanospheres. Mater. Res. 2015, 18, 1400–1406. [Google Scholar] [CrossRef]
- Fouad, H.; Elsarnagawy, T.; Almajhdi, F.N.; Khalil, K.A. Preparation and in vitro thermo-mechanical characterization of electrospun PLGA nanofibers for soft and hard tissue replacement. Int. J. Electrochem. Sci 2013, 8, 2293–2304. [Google Scholar]
- Bozec, L.; Odlyha, M. Thermal denaturation studies of collagen by microthermal analysis and atomic force microscopy. Biophys. J. 2011, 101, 228–236. [Google Scholar] [CrossRef]
- Saadatkhah, N.; Carillo Garcia, A.; Ackermann, S.; Leclerc, P.; Latifi, M.; Samih, S.; Patience, G.S.; Chaouki, J. Experimental methods in chemical engineering: Thermogravimetric analysis—TGA. Can. J. Chem. Eng. 2020, 98, 34–43. [Google Scholar] [CrossRef]
- Ayhan, F.; Ayhan, H.; Piskin, E. Sterilization of Sutures by Low Temperature Argon Plasma. J. Bioact. Compat. Polym. 1998, 13, 65–72. [Google Scholar] [CrossRef]
- Samouillan, V.; Merbahi, N.; Yousfi, M.; Gardou, J.-P.; Delaunay, F.; Dandurand, J.; Lacabanne, C. Effect of Low-Temperature Plasma Jet on Thermal Stability and Physical Structure of Type I Collagen. IEEE Trans. Plasma Sci. 2012, 40, 1688–1695. [Google Scholar] [CrossRef][Green Version]
- Schön, A.; Clarkson, B.R.; Jaime, M.; Freire, E. Temperature stability of proteins: Analysis of irreversible denaturation using isothermal calorimetry. Proteins 2017, 85, 2009–2016. [Google Scholar] [CrossRef] [PubMed]
- Fitzsimons, S.M.; Mulvihill, D.M.; Morris, E.R. Denaturation and aggregation processes in thermal gelation of whey proteins resolved by differential scanning calorimetry. Food Hydrocoll. 2007, 21, 638–644. [Google Scholar] [CrossRef]
- Kissinger, H.E. Reaction kinetics in differential thermal analysis. Anal. Chem. 1957, 29, 1702–1706. [Google Scholar] [CrossRef]
- Salomé Machado, A.A.; Martins, V.C.A.; Plepis, A.M.G. Thermal and Rheological Behavior of Collagen. Chitosan blends. J. Therm. Anal. Calorim. 2002, 67, 491–498. [Google Scholar] [CrossRef]
- Shi, L.-S.; Wang, L.-Y.; Wang, Y.-N. The investigation of argon plasma surface modification to polyethylene: Quantitative ATR-FTIR spectroscopic analysis. Eur. Polym. J. 2006, 42, 1625–1633. [Google Scholar] [CrossRef]

| Sample # | Sample Name | Argon Plasma | PLGA Mass (g) | Collagen Mass (g) | HFP Volume (mL) |
|---|---|---|---|---|---|
| 1 | Untreated PLGA | No | 0.30 | 0 | 0.51 |
| 2 | Plasma-treated PLGA | Yes | 0.30 | 0 | 0.51 |
| 3 | Untreated collagen | No | 0 | 0.20 | 1.50 |
| 4 | Plasma-treated collagen | Yes | 0 | 0.20 | 1.50 |
| 5 | Untreated PLGA–collagen | No | 0.20 | 0.20 | 1.84 |
| 6 | Plasma-treated PLGA–collagen | Yes | 0.20 | 0.20 | 1.84 |
| Sample # | Sample Name | Tpeak (°C) | ΔH (J/g) |
|---|---|---|---|
| 1 | Untreated PLGA | 154.7 | 39.2 |
| 2 | Plasma-treated PLGA | 155.2 | 33.9 |
| 3 | Untreated collagen | - | - |
| 4 | Plasma-treated collagen | - | - |
| 5 | Untreated PLGA–collagen | 112.9 157.9 211.8 | 27.0 - 8.40 |
| 6 | Plasma-treated PLGA–collagen | 104.7 159.2 223.1 | 28.9 - 24.7 |
| Sample # | Liquid | Measurement 1 (°) | Measurement 2 (°) | Measurement 3 (°) | θ (°) |
|---|---|---|---|---|---|
| Untreated PLGA | Water | 73.7 | 76.8 | 59.6 | 70.0 ± 7.5 |
| Diiodomethane | 55.1 | 58.1 | 47.0 | 53.4 ± 4.7 | |
| Plasma-treated PLGA | Water | 42.8 | 42.0 | 41.6 | 42.1 ± 0.5 |
| Diiodomethane | 31.1 | 33.0 | 33.3 | 32.5 ± 0.9 |
| Sample # | Sample Name | Measurement 1 γ (mN/m) | Measurement 2 γ (mN/m) | Measurement 3 γ (mN/m) | Mean ± SD γ (mN/m) |
|---|---|---|---|---|---|
| 1 | Untreated PLGA | 18.2 | 16.0 | 11.0 | 15.1 ± 3.0 |
| 2 | Plasma-treated PLGA | 25.0 | 13.7 | 9.7 | 16.1 ± 6.5 |
| Sample # | Sample Name | Measurement 1 (μg/μL) | Measurement 2 (μg/μL) | Measurement 3 (μg/μL) | Mean ± SD (μg/μL) |
|---|---|---|---|---|---|
| 1 | Untreated scaffold | 0.516 | 0.723 | 0.725 | 0.655 ± 0.10 |
| 2 | Plasma-treated scaffold | 0.237 | 0.207 | 0.420 | 0.288 ± 0.09 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vu, P.T.; Conroy, J.P.; Yousefi, A.M. The Effect of Argon Plasma Surface Treatment on Poly(lactic-co-glycolic acid)/Collagen-Based Biomaterials for Bone Tissue Engineering. Biomimetics 2022, 7, 218. https://doi.org/10.3390/biomimetics7040218
Vu PT, Conroy JP, Yousefi AM. The Effect of Argon Plasma Surface Treatment on Poly(lactic-co-glycolic acid)/Collagen-Based Biomaterials for Bone Tissue Engineering. Biomimetics. 2022; 7(4):218. https://doi.org/10.3390/biomimetics7040218
Chicago/Turabian StyleVu, Phat T., Jackson P. Conroy, and Amy M. Yousefi. 2022. "The Effect of Argon Plasma Surface Treatment on Poly(lactic-co-glycolic acid)/Collagen-Based Biomaterials for Bone Tissue Engineering" Biomimetics 7, no. 4: 218. https://doi.org/10.3390/biomimetics7040218
APA StyleVu, P. T., Conroy, J. P., & Yousefi, A. M. (2022). The Effect of Argon Plasma Surface Treatment on Poly(lactic-co-glycolic acid)/Collagen-Based Biomaterials for Bone Tissue Engineering. Biomimetics, 7(4), 218. https://doi.org/10.3390/biomimetics7040218