Alpha-Gal Syndrome: A Concise Review
Abstract
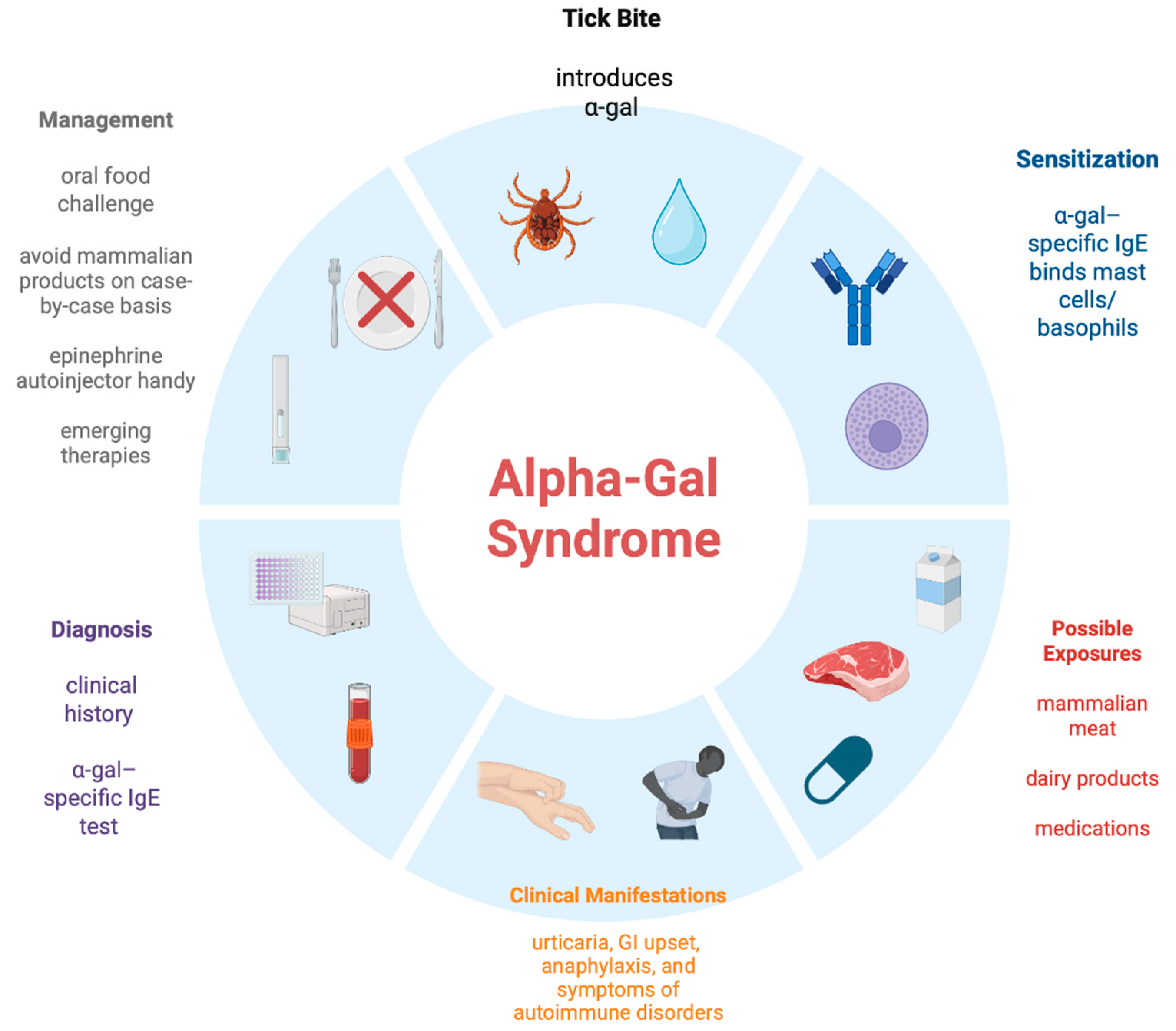
1. Introduction and Pathophysiology
2. Epidemiology
3. Clinical Features and Diagnosis
- Onset in adult life despite eating mammalian meat for several years before;
- Symptoms ranging from itching (pruritus), localized urticaria (hives), or frank angioedema and anaphylaxis;
- Predominantly gastrointestinal symptoms (loose bowel movements, abdominal cramping, nausea and vomiting) without any significant skin, pulmonary, or cardiovascular manifestations;
- Symptoms starting 3–8 (occasionally 2–10) h after ingestion of non-primate mammalian meat, less commonly dairy, or other mammalian-derived products like gelatin. Reactions do occur much faster with parenteral route;
- Serum alpha-gal IgE level > 0.1 IU/mL using standard testing available in the U.S. (via Viracor-Eurofins) or Europe (via Phadia ThermoFisher);
- Improvement in symptoms upon compliance with appropriate nutritional and other ways of avoiding exposure to mammalian products;
- Large local reactions to bites from ticks or other arthropods. Often, patients can hone-in on an ‘index’ bite, which is different from prior bites.
4. Overlap with Rheumatology
5. Management
6. Patients’ Challenges
7. Conclusions
Future Direction
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Chung, C.H.; Mirakhur, B.; Chan, E.; Le, Q.-T.; Berlin, J.; Morse, M.; Murphy, B.A.; Satinover, S.M.; Hosen, J.; Mauro, D.; et al. Cetuximab-induced anaphylaxis and IgE specific for galactose-α-1,3-galactose. N. Engl. J. Med. 2008, 358, 1109–1117. [Google Scholar] [CrossRef] [PubMed]
- Commins, S.P.; James, H.R.; Kelly, L.A.; Pochan, S.L.; Workman, L.J.; Perzanowski, M.S.; Kocan, K.M.; Fahy, J.V.; Nganga, L.W.; Ronmark, E.; et al. The relevance of tick bites to the production of IgE antibodies to α-gal. J. Allergy Clin. Immunol. 2011, 127, 1286–1293. [Google Scholar] [CrossRef]
- Hamsten, C.; Tran, T.A.T.; Starkhammar, M.; Brauner, A.; Commins, S.P.; Platts-Mills, T.A.E.; van Hage, M. Red meat allergy in Sweden: Association with tick sensitization and B-negative blood groups. J. Allergy Clin. Immunol. 2013, 132, 1431–1434. [Google Scholar] [CrossRef]
- Chinuki, Y.; Ishiwata, K.; Yamaji, K.; Takahashi, H.; Morita, E. Haemaphysalis longicornis tick bites are a possible cause of red meat allergy in Japan. Allergy 2016, 71, 421–425. [Google Scholar] [CrossRef]
- Kwak, M.; Somerville, C.; van Nunen, S. A novel Australian tick Ixodes australiensis inducing mammalian meat allergy after tick bite. Asia Pac. Allergy 2018, 8, e31. [Google Scholar] [CrossRef]
- Van Nunen, S.A.; O’Connor, K.S.; Clarke, L.R.; Boyle, R.X.; Fernando, S.L. An association between tick bite reactions and red meat allergy in humans. Med. J. Aust. 2009, 190, 510–511. [Google Scholar] [CrossRef]
- Iweala, O.I.; Choudhary, S.K.; Addison, C.T.; Commins, S.P. T and B lymphocyte transcriptional states differentiate between sensitized and unsensitized individuals in alpha-gal syndrome. Int. J. Mol. Sci. 2021, 22, 3185. [Google Scholar] [CrossRef]
- Crispell, G.; Commins, S.P.; Archer-Hartman, S.A.; Choudhary, S.; Dharmarajan, G.; Azadi, P.; Karim, S. Discovery of alpha-gal-containing antigens in North American tick species believed to induce red meat allergy. Front Immunol. 2019, 10, 1056. [Google Scholar] [CrossRef]
- Maldonado-Ruiz, L.P.; Reif, K.E.; Ghosh, A.; Foré, S.; Johnson, R.L.; Park, Y. High levels of alpha-gal with large variation in the salivary glands of lone star ticks fed on human blood. Sci. Rep. 2023, 13, 21409. [Google Scholar] [CrossRef] [PubMed]
- Thompson, J.M.; Carpenter, A.; Kersh, G.J.; Wachs, T.; Commins, S.P.; Salzer, J.S. Geographic distribution of suspected alpha-gal syndrome cases—United States, 2017–2022. Morb. Mortal. Wkly. Rep. 2023, 72, 815–820. [Google Scholar] [CrossRef] [PubMed]
- Springer, Y.P.; Jarnevich, C.S.; Barnett, D.T.; Monaghan, A.J.; Eisen, R.J. Modeling the present and future geographic distribution of the lone star tick, Amblyomma americanum, in the continental United States. Am. J. Trop. Med. Hyg. 2015, 93, 875–890. [Google Scholar] [CrossRef] [PubMed]
- Raghavan, R.K.; Peterson, A.T.; Cobos, M.E.; Ganta, R.; Foley, D. Current and future distribution of the lone star tick, Amblyomma americanum (Acari: Ixodidae), in North America. PLoS ONE 2019, 14, e0209082. [Google Scholar] [CrossRef] [PubMed]
- Carpenter, A.; Drexler, N.A.; McCormick, D.W.; Thompson, J.M.; Kersh, G.; Commins, S.P.; Salzer, J.S. Health Care Provider Knowledge Regarding Alpha-gal Syndrome—United States, March–May 2022. Morb. Mortal. Wkly. Rep. 2023, 72, 809–814. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Alpha-Gal Alliance Action Fund, a Nonprofit Advocacy Partner of Alpha-Gal Alliance. Available online: https://www.alphagalaction.org (accessed on 15 August 2025).
- Wilson, J.M.; Schuyler, A.J.; Workman, L.; Gupta, M.; James, H.R.; Posthumus, J.; McGowan, E.C.; Commins, S.P.; Platts-Mills, T.A.E. Investigation into the α-gal syndrome: Characteristics of 261 children and adults reporting red meat allergy. J. Allergy Clin. Immunol. Pract. 2019, 7, 2348–2354. [Google Scholar] [CrossRef]
- Busing, J.D.; Stone, C.A., Jr.; Nicholson, M.R. Clinical presentation of alpha-gal syndrome in pediatric gastroenterology and response to mammalian dietary elimination. Am. J. Gastroenterol. 2023, 118, 1293–1296. [Google Scholar] [CrossRef]
- Binder, A.M.; Cherry-Brown, D.; Biggerstaff, B.J.; Jones, E.S.; Amelio, C.L.; Beard, C.B.; Petersen, L.R.; Kersh, G.J.; Commins, S.P.; Armstrong, P.A. Clinical and laboratory features of patients diagnosed with alpha-gal syndrome-2010-2019. Allergy 2023, 78, 477–487. [Google Scholar] [CrossRef]
- McGill, S.K.; Commins, S.P.; Peery, A.F.; Galanko, J.; Keku, T.O.; Shaheen, N.J.; Anderson, C.; Sandler, R.S. Alpha-gal sensitization in a US screening population is not associated with a decreased meat intake or gastrointestinal symptoms. Am. J. Gastroenterol. 2023, 118, 1276–1281. [Google Scholar] [CrossRef]
- Nakagawa, Y.; Chinuki, Y.; Ogino, R.; Yamasaki, K.; Aiba, S.; Ugajin, T.; Yokozeki, H.; Kitamura, K.; Morita, E. Cohort study of subclinical sensitization against galactose-α-1,3-galactose in Japan: Prevalence and regional variations. J. Dermatol. 2022, 49, 1268–1277. [Google Scholar] [CrossRef]
- Kim, M.S.; Straesser, M.D.; Keshavarz, B.; Workman, L.; McGowan, E.C.; Platts-Mills, T.A.E.; Wilson, J.M. IgE to galactose-α-1,3-galactose wanes over time in patients who avoid tick bites. J. Allergy Clin. Immunol. Pract. 2020, 8, 364–367. [Google Scholar] [CrossRef]
- Commins, S.P. Diagnosis & management of alpha-gal syndrome: Lessons from 2,500 patients. Expert Rev. Clin. Immunol. 2020, 16, 667–677. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Levin, M.; Apostolovic, D.; Biedermann, T.; Commins, S.P.; Iweala, O.I.; Platts-Mills, T.A.E.; Savi, E.; van Hage, M.; Wilson, J.M. Galactose alpha-1,3-galactose phenotypes: Lessons from various patient populations. Ann. Allergy Asthma Immunol. 2019, 122, 598–602. [Google Scholar] [CrossRef] [PubMed]
- Mabelane, T.; Basera, W.; Botha, M.; Thomas, H.F.; Ramjith, J.; Levin, M.E. Predictive values of alpha-gal IgE levels and alpha-gal IgE: Total IgE ratio and oral food challenge-proven meat allergy in a population with a high prevalence of reported red meat allergy. Pediatr. Allergy Immunol. 2018, 29, 841–849. [Google Scholar] [CrossRef]
- Pollack, K.; Zlotoff, B.J.; Borish, L.C.; Commins, S.P.; Platts-Mills, T.A.E.; Wilson, J.M. Alpha-Gal Syndrome vs Chronic Urticaria. JAMA Dermatol. 2019, 155, 115–116. [Google Scholar] [CrossRef]
- Jones, S.; Bray, N.; Kaushik, P. Erythrodermic psoriasis and alpha-gal syndrome: A case report. J. Med. Clin. Res. Rev. 2025, 9, 1–3. [Google Scholar]
- Kaushik, P.; Suresh, S.; Alexander, C.S. Alpha-gal syndrome presenting as fibromyalgia in an American Indian population. J. Med. Clin. Res. Rev. 2024, 19, 329–330. [Google Scholar] [CrossRef]
- Brestoff, J.R.; Zaydman, M.A.; Scott, M.G.; Gronowski, A.M. Diagnosis of red meat allergy with antigen-specific IgE tests in serum. J. Allergy Clin. Immunol. 2017, 140, 608–610.e5. [Google Scholar] [CrossRef]
- Mehlich, J.; Fischer, J.; Hilger, C.; Swiontek, K.; Morisset, M.; Codreanu-Morel, F.; Schiener, M.; Blank, S.; Ollert, M.; Darsow, U.; et al. The basophil activation test differentiates between patients with alpha-gal syndrome and asymptomatic sensitization. J. Allergy Clin. Immunol. 2019, 143, 182–189. [Google Scholar] [CrossRef]
- Vaz-Rodrigues, R.; Mazuecos, L.; de la Fuente, J. Current and Future Strategies for the Diagnosis and Treatment of the Alpha-Gal Syndrome (AGS). J. Asthma Allergy 2022, 15, 957–970. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zychowski, D.L.; Alvarez, C.; Abernathy, H.; Giandomenico, D.; Choudhary, S.K.; Vorobiov, J.M.; Boyce, R.M.; Nelson, A.E.; Commins, S.P. Tick-Borne Disease Infections and Chronic Musculoskeletal Pain. JAMA Netw Open. 2024, 7, e2351418. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bosques, C.J.; Collins, B.E.; Meador, J.W., 3rd; Sarvaiya, H.; Murphy, J.L.; Dellorusso, G.; Bulik, D.A.; Hsu, I.H.; Washburn, N.; Sipsey, S.F.; et al. Chinese hamster ovary cells can produce galactose-alpha-1,3-galactose antigens on proteins. Nat. Biotechnol. 2010, 28, 1153–1156. [Google Scholar] [CrossRef]
- González Polanco, E.; Borowitz, S. Delayed Hypersensitivity Reaction to Infliximab Due to Mammalian Meat Allergy. JPGN Rep. 2023, 4, e322. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chitnavis, M.; Stein, D.J.; Commins, S.; Schuyler, A.J.; Behm, B. First-dose anaphylaxis to infliximab: A case of mammalian meat allergy. J. Allergy Clin. Immunol. Pract. 2017, 5, 1425–1426. [Google Scholar] [CrossRef]
- Leder, J.; Diederich, A.; Patel, B.; Bowie, M.; Renwick, C.M.; Mangunta, V. Perioperative Considerations in Alpha-Gal Syndrome: A Review. Cureus 2024, 16, e53208. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Commins, S.P. Invited Commentary: Alpha-Gal Allergy: Tip of the Iceberg to a Pivotal Immune Response. Curr. Allergy Asthma Rep. 2016, 16, 61. [Google Scholar] [CrossRef] [PubMed]
- Fischer, J.; Hebsaker, J.; Caponetto, P.; Platts-Mills, T.A.E.; Biedermann, T. Galactose-alpha-1,3-galactose sensitization is a prerequisite for pork-kidney allergy and cofactor-related mammalian meat anaphylaxis. J. Allergy Clin. Immunol. 2014, 134, 755–759.e1. [Google Scholar] [CrossRef]
- Commins, S.P.; James, H.R.; Stevens, W.; Pochan, S.L.; Land, M.H.; King, C.; Mozzicato, S.; Platts-Mills, T.A.E. Delayed clinical and ex vivo response to mammalian meat in patients with IgE to galactose-alpha-1,3-galactose. J. Allergy Clin. Immunol. 2014, 134, 108–115. [Google Scholar] [CrossRef]
- Kuravi, K.V.; Sorrells, L.T.; Nellis, J.R.; Rahman, F.; Walters, A.H.; Matheny, R.G.; Choudhary, S.K.; Ayares, D.L.; Commins, S.P.; Bianchi, J.R.; et al. Allergic response to medical products in patients with alpha-gal syndrome. J. Thorac. Cardiovasc. Surg. 2022, 164, e411–e424. [Google Scholar] [CrossRef]
- Hawkins, R.B.; Wilson, J.M.; Mehaffey, J.H.; Platts-Mills, T.A.E.; Ailawadi, G. Safety of intravenous heparin for cardiac surgery in patients with alpha-gal syndrome. Ann. Thorac. Surg. 2021, 111, 1991–1997. [Google Scholar] [CrossRef]
- Mozzicato, S.M.; Tripathi, A.; Posthumus, J.B.; Platts-Mills, T.A.E.; Commins, S.P. Porcine or bovine valve replacement in 3 patients with IgE antibodies to the mammalian oligosaccharide galactose-alpha-1,3-galactose. J. Allergy Clin. Immunol. Pract. 2014, 2, 637–638. [Google Scholar] [CrossRef] [PubMed]
- Mullins, R.J.; James, H.; Platts-Mills, T.A.E.; Commins, S.P. Relationship between red meat allergy and sensitization to gelatin and galactose-alpha-1,3-galactose. J. Allergy Clin. Immunol. 2012, 129, 1334–1342.e1. [Google Scholar] [CrossRef]
- Uyttebroek, A.; Sabato, V.; Bridts, C.H.; De Clerck, L.S.; Ebo, D.G. Anaphylaxis to succinylated gelatin in a patient with a meat allergy: Galactose-alpha(1, 3)-galactose (alpha-gal) as antigenic determinant. J. Clin. Anesth. 2014, 26, 574–576. [Google Scholar] [CrossRef]
- Stone, C.A., Jr.; Hemler, J.A.; Commins, S.P.; Schuyler, A.J.; Phillips, E.J.; Peebles, R.S., Jr.; Fahrenholz, J.M. Anaphylaxis after zoster vaccine: Implicating alpha-gal allergy as a possible mechanism. J. Allergy Clin. Immunol. 2017, 139, 1710–1713. [Google Scholar] [CrossRef]
- Stone, C.A., Jr.; Commins, S.P.; Choudhary, S.; Vethody, C.; Heavrin, J.L.; Wingerter, J.S.; Hemler, J.A.; Babe, K.; Phillips, E.J.; Norton, A.E. Anaphylaxis after vaccination in a pediatric patient: Further implicating alpha-gal allergy. J. Allergy Clin. Immunol. Pract. 2019, 7, 322–324.e2. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, R.B.; Frischtak, H.L.; Kron, I.L.; Ghanta, R.K. Premature Bioprosthetic Aortic Valve Degeneration Associated with Allergy to Galactose-Alpha-1,3-Galactose. J. Card. Surg. 2016, 31, 446–448. [Google Scholar] [CrossRef]
- Banner, W.; Edelen, K.; Epperson, L.C.; Moore, E. Hypersensitivity reactions due to North American pit viper antivenom administration and confirmed elevation of alpha-gal IgE. Toxicol. Commun. 2023, 8, 2314314. [Google Scholar] [CrossRef]
- Fischer, J.; Eberlein, B.; Hilger, C.; Eyer, F.; Eyerich, S.; Ollert, M.; Biedermann, T. Alpha-gal is a possible target of IgE-mediated reactivity to antivenom. Allergy 2017, 72, 764–771. [Google Scholar] [CrossRef]
- Navalpakam, A.; Thanaputkaiporn, N.; Poowuttikul, P. Management of anaphylaxis. Immunol. Allergy Clin. N. Am. 2022, 42, 65–76. [Google Scholar] [CrossRef]
- Bangale, T. Created in BioRender. 2025. Available online: https://BioRender.com/ (accessed on 15 August 2025).
- Lammerts van Bueren, J.J.; Rispens, T.; Verploegen, S.; van der Palen-Merkus, T.; Stapel, S.; Workman, L.J.; James, H.; van Berkel, P.H.; van de Winkel, J.G.; Platts-Mills, T.A.; et al. Anti-galactose-α-1,3-galactose IgE from allergic patients does not bind α-galactosylated glycans on intact therapeutic antibody Fc domains. Nat. Biotechnol. 2011, 29, 574–576. [Google Scholar] [CrossRef] [PubMed]
- Platts-Mills, T.A.E.; Li, R.C.; Keshavarz, B.; Smith, A.R.; Wilson, J.M. Diagnosis and Management of Patients with the α-Gal Syndrome. J. Allergy Clin. Immunol. Pract. 2020, 8, 15–23.e1. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaushik, P.; Bhatti, F.S.; Bangale, T.; Marak, C.P. Alpha-Gal Syndrome: A Concise Review. Allergies 2025, 5, 42. https://doi.org/10.3390/allergies5040042
Kaushik P, Bhatti FS, Bangale T, Marak CP. Alpha-Gal Syndrome: A Concise Review. Allergies. 2025; 5(4):42. https://doi.org/10.3390/allergies5040042
Chicago/Turabian StyleKaushik, Prashant, Faryal S. Bhatti, Tanmay Bangale, and Creticus P. Marak. 2025. "Alpha-Gal Syndrome: A Concise Review" Allergies 5, no. 4: 42. https://doi.org/10.3390/allergies5040042
APA StyleKaushik, P., Bhatti, F. S., Bangale, T., & Marak, C. P. (2025). Alpha-Gal Syndrome: A Concise Review. Allergies, 5(4), 42. https://doi.org/10.3390/allergies5040042





