Abstract
Unverified beta-lactam allergies are a substantial public health problem, as the majority of patients labeled as beta-lactam allergic do not have clinically significant allergies that may hinder the use beta-lactam therapy when indicated. Outdated or inaccurate beta-lactam or penicillin allergies can result in serious consequences, including suboptimal antibiotic therapy, increased risk of adverse effects, and use of broader spectrum antibiotics than indicated, which may contribute to antimicrobial resistance. The purpose of this review is to provide an overview of beta-lactam allergy and highlight the role of pharmacists in managing beta-lactam allergies. Studies have shown that pharmacists can play a vital role in allergy assessment, penicillin skin testing, beta-lactam desensitization, evaluation of beta-lactam cross-reactivity and recommending appropriate antibiotic therapy in patients with beta-lactam allergies.
1. Introduction
Beta-lactam antibiotics are considered a first-line therapy in many bacterial infections and include agents such as penicillins, cephalosporins and carbapenems. However, beta-lactam antibiotics are a common cause of adverse drug reactions and are associated with high rates of antibiotic allergy [1].
Unverified beta-lactam allergies are a substantial public health problem, as the majority of patients labeled as penicillin allergic do not have clinically significant IgE-mediated allergies that may hinder the use of beta-lactam therapy when indicated [2]. The vast majority of patients have a subjective and inaccurate understanding of beta-lactam allergy. Approximately 10% of patients report an allergy to penicillin; however, up to 90% of these patients do not have a true allergy [3]. A true allergy, better known as an IgE-mediated or type I reaction, typically occurs immediately or within 1 h of medication administration, and can consist of hives, angioedema, wheezing, shortness of breath, and anaphylaxis [4]. Even in patients with true beta-lactam allergies, the IgE antibodies decrease over time. In patients who have previously tested positive for beta-lactam allergy, there is an expected 10% decrease per year of a subsequent positive reaction. Therefore, with the avoidance of beta-lactams, 80% to 100% of patients will ultimately test negative for beta-lactam allergy 10 years after the initial positive test [3].
Outdated or inaccurate beta-lactam allergies can result in serious consequences, such as suboptimal antibiotic therapy, increased risk for adverse effects, and use of broader spectrum antibiotics than needed, which may contribute to antimicrobial resistance [5]. Pharmacists can play a vital role in evaluating the patient and identifying a true allergy, assisting in de-labeling inaccurate allergies, performing a standard of care skin test, deciding when desensitization is an appropriate option, and considering cross-reactivity for optimal antibiotic treatment.
2. Purpose and Methods
The purpose of this review is to provide an overview of the beta-lactam allergy and highlight the role of the pharmacist in managing beta-lactam allergies. A literature search was conducted via PubMed using the following search terms “pharmacist, beta-lactam, penicillin, allergy, impact, management” from February to March 2021. Relevant English language studies were included in this review.
3. Discussion
3.1. Beta-Lactam Allergy Overview
3.1.1. Pathophysiology
Beta-lactam allergies are hypersensitivity reactions that are the consequence of an adaptive immune response. Of the four reaction types described in Table 1, penicillin allergies most often present as type I or type IV hypersensitivity reactions [3]. Type I hypersensitivity reactions are triggered by the interaction of an allergen with allergen-specific IgE bound to mast cells, basophils, and eosinophils. This interaction causes the cells to degranulate and release a potent mixture of histamine and inflammatory mediators [6]. In response to histamine and other inflammatory mediators, there is an increase in vascular permeability and a widespread constriction of smooth muscle, which can ultimately lead to anaphylactic shock [6]. Type I reactions are immediate in nature and may result in symptoms such as urticaria, flushing, dyspnea, bronchospasm, angioedema, hypotension, tachycardia, altered mental status or gastrointestinal upset [3].

Table 1.
Classification of hypersensitivity reactions [3,5,6,7].
Because all penicillin antibiotics share a similar beta-lactam core ring structure, one must consider the potential for cross-allergenicity between different agents in the beta-lactam class. When a beta-lactam is administered, the common core ring structure is metabolized into major and minor antigenic determinants. The major determinant is penicilloyl, and the minor determinants include penicillin, penicilloate, and penilloate [3]. In patients with beta-lactam allergy, the minor antigenic determinants generate IgE-specific responses associated with type I allergy. The major antigenic determinant is more commonly associated with less severe urticarial reactions [3]. In addition to a core ring structure, beta-lactams have various side chains, which can also result in type I allergic reactions [3]. Type I reactions to beta-lactam antibiotics are individualized and have effects of varying severity.
Less frequently, beta-lactam allergies may present as other types of hypersensitivity reactions. Type II hypersensitivities are less severe, but can be caused by an IgG response to small molecules like penicillin that become covalently bound to the outside surface of cells. The chemical reaction modifies the structures of human cell surface components, which become perceived as foreign antigens by the immune system. B cells are stimulated to make IgG antibodies against the new epitopes. On binding to their specific cell-surface antigens, the antibodies cause the modified human cells to become subject to complement activation and phagocytosis, resulting in inflammation and damaged tissue [6].
Type III hypersensitivities involve small, soluble, immune complexes of antigen and specific IgG, forming deposits in the walls of small blood vessels or the alveoli of the lungs. At these sites, the immune complexes activate complement and an inflammatory response that damages the tissue and impairs its function. Typically, type III hypersensitivities are not associated with beta-lactam exposure [5].
Type IV hypersensitivities are caused by CD4 T-cells responding to the epitopes of foreign proteins or to peptides derived from chemically modified human proteins [6]. The result is typically cutaneous reactions such as a maculopapular rash or urticarial eruption. Although rare, severe reactions, such as Stevens–Johnson syndrome (SJS), toxic epidermal necrolysis (TEN) or drug rash with eosinophilia and systemic symptoms (DRESS) may occur as a result of a type IV hypersensitivity. Type IV hypersensitivities are delayed in nature, occurring several days to weeks after the last administered dose, and have been associated with beta-lactam allergy [7].
3.1.2. Risk Factors
Although data are currently limited in regard to the risk factors for a beta-lactam allergy, there is speculation about a correlation between the clinical and genetic risk factors of self-reported penicillin allergy. A recent case-control study identified factors such as having a family history of penicillin allergy or an IL-4 gene single nucleotide polymorphism as possible risk factors of penicillin allergy. [8] Another recent study found that HLA-DRB1*10:01 predisposed patients to an immediate hypersensitivity reaction [9]. Furthermore, other studies suggest a greater risk of penicillin allergy in females and a greater risk of beta-lactam allergy in those with a history of a prior adverse reaction to penicillin [10,11].
3.1.3. Cross-Allergenicity
As noted earlier, all beta-lactam antibiotics share a similar chemical core ring structure. This core ring consists of a beta-lactam ring attached to a five- or six-membered ring. In addition to this core structure, beta-lactams have side chains (R1 and R2) that vary between the specific agents [12]. Because of the common core ring structure among beta-lactam antibiotics and the potential similarities in side-chains, there is a risk for cross-allergenicity among the different beta-lactam classes. Knowledge and understanding of the risk of beta-lactam cross-allergenicity plays an important role in selecting the appropriate antibiotic therapy for a patient with a beta lactam allergy. The rates of cross-allergenicity between penicillin and other beta-lactams can be found in Table 2.

Table 2.
Beta-lactam cross-reactivity [12,14,15,16,17,18].
The early studies of penicillin cross-allergenicity with cephalosporin antibiotics cite rates as high as 10%. However, these rates are considered artificially high and are attributed to the contamination of early generation cephalosporins by penicillin because of the early manufacturing processes used to create the cephalosporin ring structure [13]. The actual rate of cross-allergenicity between penicillin and cephalosporins is likely <2% [12,13]. Similarities in the R1 side chains of cephalosporins have been shown to be the most important predictor of cross-allergenicity as compared to a common beta-lactam ring [14,15]. Certain cephalosporins and penicillins have identical side chains, such as cephalexin, cefaclor, and ampicillin, and cefadroxil, cefprozil and amoxicillin. In general, most patients reporting an allergy to beta-lactams can safely receive cephalosporin therapy. However, agents with identical side chains should be avoided in patients with a true IgE-mediated beta-lactam allergy [15].
Carbapenems, another group of beta-lactam antibiotics, are generally well tolerated and have a low risk of causing allergic reactions. Studies evaluating the cross-allergenicity between penicillins and carbapenems demonstrate rates of cross-allergenicity of 0%–0.3% in patients with a true IgE-mediated penicillin allergy [16,17]. Typically, carbapenems are considered safe for administration in patients with a reported penicillin allergy [18].
Aztreonam is a monobactam antibiotic that differs structurally from beta-lactams because of its monocyclic core ring structure. Because of this major difference, the risk of cross-allergenicity with the beta-lactam class is considered negligible [15]. However, it is important to note that aztreonam and ceftazidime, a third generation cephalosporin, share an identical side chain. Patients with a true ceftazidime allergy may also have an aztreonam allergy, therefore aztreonam should be avoided in these patients [15].
4. Approach to Management
4.1. Initial Allergy Assessment
The initial management of patients with a history of beta-lactam allergy requires a detailed allergy assessment, given that many patients are inappropriately labeled as beta-lactam allergic. Oftentimes, known adverse effects of a beta-lactam are mislabeled and documented as a beta-lactam allergy. Approximately 90% of patients labeled as allergic can be de-labeled through a detailed allergy assessment or allergy testing [19,20]. The appropriate assessment of beta-lactam allergy includes the evaluation of factors such as the specific agent causing the reaction, the type, severity, and timing of the reaction, and previous tolerability of other beta-lactam agents. The de-labeling of penicillin allergy, based on historical evaluation alone, has been demonstrated to be safe and effective in patients reporting a mild, non-immune-mediated adverse drug reaction, or where subsequent tolerance to the implicated penicillin has been identified through their medical or pharmacy records [19]. Figure 1 includes a list of questions that may be appropriate to ask patients who report a beta-lactam allergy.
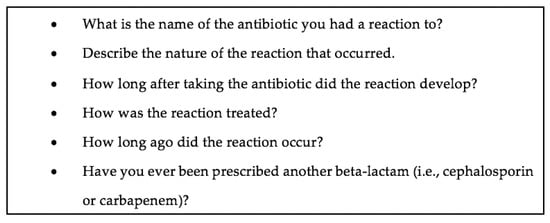
Figure 1.
Sample allergy assessment questions.
Additionally, a direct oral challenge may be an effective option in de-labeling patients with low-risk penicillin allergies and has been used in both the inpatient and outpatient setting. Direct oral challenges offer a means to de-labeling penicillin allergies in patients who are low risk or have an inaccurate allergy label without having to pursue traditional allergy testing. Appropriate risk stratification is needed to ensure the safety of a direct oral challenge; however, no standard criteria to determine low-risk allergy patients has been established. Factors such as reaction type, onset of allergy symptoms, and severity have been utilized to determine risk. Validated allergy phenotyping tools may be used to identify low-risk allergy patients and help to facilitate de-labeling when appropriate [21].
4.2. Penicillin Skin Testing
In patients with ambiguous allergy histories, or those reporting allergies that are severe in nature, additional steps should be taken to determine the nature of their allergy and whether a beta-lactam can safely be administered. Penicillin skin testing (PST) is a safe and effective means of evaluating a penicillin allergy in these patients. It is used to detect the presence of penicillin-specific IgE and predicts the likelihood of a type I allergic reaction to penicillin [22]. PST is indicated in patients with documented or suspected type I clinical penicillin hypersensitivity. Patients with a history of desquamating type IV hypersensitivity reactions, such as SJS, TEN, or DRESS or other non-IgE-related hypersensitivity, are not candidates for PST [21]. Implementing PST requires the consideration of several logistical factors such as the development of policies and protocols, specialized training for staff, storage and preparation of PST components, and determining whether PST should be offered in the inpatient versus outpatient setting [23].
PST involves epicutaneous skin testing, followed by intradermal testing, and is conducted using degradation products of penicillin, known as major and minor determinants. PST offers a negative predictive value of 97–99% [24] and a positive predictive value of approximately 50% [25].
In patients who have a negative PST, a test dose of the beta-lactam to which the patient reported allergy should be administered in order to confirm the absence of an allergy. The patient should then be observed for 1–2 h after the test dose to confirm no immediate reaction occurs. If no reaction occurs after the observation period, the patient can receive the beta-lactam and should have their allergy information updated accordingly.
4.3. Beta-lactam Desensitization
In patients with a positive PST, beta-lactam therapy may still be administered after desensitization is performed. Avoiding beta-lactam therapy in these patients can lead to the use of suboptimal therapy, as beta-lactams have been demonstrated as superior agents in the management of infections such as methicillin-susceptible Staphylococcus aureus (MSSA), severe Pseudomonas aeruginosa, and syphilis [23].
Desensitization may be indicated in patients with a true beta-lactam allergy or in those where the results of the penicillin skin testing is indeterminate, but still require beta-lactam therapy [7]. The process should be performed by a specialist and involves administering incremental increases in beta-lactam doses over time to allow patients to tolerate beta-lactam therapy on a temporary basis. Desensitization is often conducted in a hospital setting or intensive care unit, as patients will require frequent monitoring throughout the procedure. Numerous beta-lactam desensitization protocols exist and often take several hours to days to complete [26].
As seen in Table 3, initial management of patients with reported beta-lactam allergies should be decided based on allergy assessment and the suspected reaction. For individuals with low risk of allergy, a direct oral challenge may be considered. For individuals with signs and symptoms of an IgE mediated allergy (type I), PST should be performed. If PST is negative, a beta-lactam challenge dose may be administered. If PST is positive, beta-lactam desensitization may be considered. In patients with signs and symptoms of non-IgE mediated allergy (types II-IV) PST, challenge doses, and desensitization are contraindicated [27].

Table 3.
Initial approach to managing patients with penicillin allergy [21,27].
5. Role of the Pharmacist
5.1. Allergy Assessment
As medication experts, pharmacists are uniquely poised to conduct beta-lactam allergy assessments to assist with de-labeling when appropriate. Several studies have demonstrated the benefit of having pharmacists involved in beta-lactam allergy interviews.
One pilot study utilized a pharmacy resident and infectious diseases clinical pharmacist to clarify a beta-lactam allergy, and, where appropriate, recommended a change to the patients’ antibiotic regimen. In total, 32 patients with a documented beta-lactam allergy were interviewed, and 24 were identified as candidates for beta-lactam therapy. The intervention by the pharmacy resulted in over 65% of the patients being changed from a non-penicillin antibiotic to a cephalosporin, carbapenem, or penicillin. Although small, this study demonstrates the efficacy of a pharmacist-driven beta-lactam allergy assessment [28]. In a larger retrospective study, including 418 patients, Holmes and colleagues evaluated the impact of a pharmacy-driven assessment on the prescribing frequency of penicillin or cephalosporin antibiotics in patients with a reported beta-lactam allergy. Pharmacy staff were notified, through an alert system, of any patient with a documented penicillin allergy receiving a non-penicillin antibiotic. Upon notification, the pharmacy staff performed an allergy assessment, which included a review of previous beta-lactam tolerance, and clarification of the reaction type, severity, and timing of the allergy. The pharmacist allergy assessment resulted in increased frequency of beta-lactam prescribing in patients with previously reported beta-lactam allergy, by 12.9%, and a decrease in the days of therapy of non-penicillin antibiotic use, by 123 days of therapy per 1000 patient days, again showing the benefit of pharmacist involvement in penicillin allergy assessment [29].
Additionally, a study by Campbell and colleagues evaluated a pharmacist-led penicillin allergy assessment at a community hospital in 380 patients. The assessment included a chart review, patient interview, follow-up antibiotic discussion with the provider, and updating the allergy documentation when appropriate. The pharmacist-led assessment resulted in improved use of guideline preferred antibiotics by 13% and reduced fluoroquinolone use by 11%. [30] Furthermore, the pharmacist-driven allergy assessment has also been associated with cost savings for patients with beta-lactam allergy, with one study estimating cost savings of $21,000 over a 3-month period [31].
5.2. Penicillin Skin Testing
Pharmacists also play a role in the diagnosis of beta-lactam allergy by participating in PST. When the initial allergy assessment does not provide clear information on whether a patient has a true penicillin allergy, PST can be used as a simple means of diagnosing penicillin allergy. When pharmacists are involved in PST, the state board of the pharmacy should first be consulted to determine whether PST completed by a pharmacist falls within a pharmacist’s scope of practice, as scopes vary between states. If PST is not allowable under the state board of pharmacy, the pharmacist may still serve as part of a collaborative team conducting PST [23].
A recent study investigated a pharmacist-driven PST service for adults at a community hospital. Twenty-two patients with documented type I allergies, who were prescribed alternative antibiotics, were identified and underwent PST by trained pharmacists. All of the skin tests were negative, with no type I reactions occurring to the test itself or to the beta-lactam antibiotic administered thereafter. Additionally, 68.2% of the patients were successfully transitioned to a beta-lactam after skin testing, leading to a decreased use of vancomycin and fluoroquinolones. The authors concluded that pharmacist-driven PST can be successfully implemented and is another means for pharmacists to expand antimicrobial stewardship practices [32].
Another study describes pharmacist-managed and pharmacist-administered PST incorporation into an antimicrobial stewardship program at a community hospital. Patients who were at least 18 years old, and reported a history of a type I or unknown type of allergic reaction to penicillin, occurring more than 5 years prior, were considered for inclusion. In total, PST was initiated in 90 patients, with 94% completing PST. Nearly 85% of the patients who completed PST were transitioned to a preferred beta-lactam, allowing alternative antibiotics to be avoided for a median of 11 days per patient. This study demonstrates that pharmacist-managed/-administered PST improved the utilization of preferred antibiotics and the avoidance of alternative therapy [33].
Additionally, Griffith and colleagues conducted a retrospective cohort study evaluating the impact of an inpatient pharmacist- and pharmacy trainee-administered penicillin allergy assessment and PST service on allergy reconciliation and antibiotic use. There was a total of 161 evaluations conducted, 74% allergy assessments and 26% PST. The reconciled allergies improved from 11% to 75% post-evaluation, and no PSTs were positive. Following PST, antibiotic therapy was optimized in 58% of the patients, the vancomycin use decreased from 44% to 17%, and the use of penicillins increased from 0% to 39% [34].
Other studies assessing the role of pharmacists in beta-lactam allergy evaluation and PST also demonstrated similar findings, with increased use of beta-lactams after intervention, decreased use of broader spectrum antibiotics, and no severe adverse drug reactions noted [35,36,37,38].
5.3. Desensitization
Another area where pharmacists provide valued insight is identifying and managing patients who are candidates for beta-lactam desensitization.
Chen and colleagues evaluated the successfulness and the safety of antibiotic desensitization protocols developed by their pharmacy department. Each protocol provided specific instructions regarding reconstitution, administration, time to target dose, reaction, management, storage, and stability. Desensitizations were conducted in an intensive care unit through a multidisciplinary team approach that included a clinical pharmacotherapy specialist. The study reviewed 61 desensitizations, 89% of which were completed without the development of any adverse reactions. The 10% of cases where adverse reactions occurred were managed during desensitization and were able to successfully complete the process. The results suggest that pharmacy-developed antibiotic desensitization protocols are successful and safe [39].
5.4. Cross-Allergenicity/Antibiotic Selection
Additionally, pharmacists serve as crucial resources when it comes to educating and advising clinicians about the determinants and likelihood of cross-reactivity between penicillin-related compounds. Pharmacists, being well versed in medicinal chemistry, can make adjustments and interventions using this knowledge base. As a result, patients with a history of non-IgE-mediated, non-severe beta-lactam allergies are often able to safely receive beta-lactams that are structurally dissimilar [14]. By taking into consideration these cross-allergenicity rates, pharmacists can directly influence clinicians to determine when patients with reported beta-lactam allergies remain appropriate candidates to receive beta-lactam therapy [14].
In a quasi-experimental pre-post study at Aurora BayCare Medical Center, educational efforts and modified workflow were implemented for the purpose of improving allergy histories and documentation, and increasing the use of beta-lactams, when appropriate, among patients with a reported beta-lactam allergy. Pharmacists were educated on allergy mechanisms, beta-lactam cross-reactivity rates and use of the developed reference tools. Prescribers, hospitalists, and intensivists were educated on the efficacy, safety, and economic implications of the consistent avoidance of beta-lactams in patients with reported beta-lactam allergies, and current estimates of cross-reactivity rates between the beta-lactam classes. It was concluded that multidisciplinary education combined with pharmacy-led efforts to confront the challenge of beta-lactam allergies among hospitalized patients may improve allergy documentation and selection in patients with a reported beta-lactam allergy. Although the intervention was not associated with an overall reduction in non-beta-lactam use, it did increase the number of patients who were transitioned from non-beta-lactam to beta-lactam therapy. The authors suggest that the overall reduction in non-beta-lactam use was likely not observed due to the time requirement in ascertaining a sufficient allergy history and allowing for a corresponding intervention to occur, and suggest that more distinct interventions may be required to impact empiric prescribing practices [14].
6. Conclusions
Understanding the beta-lactam allergy is critical to managing patients with infectious diseases. Mislabeled beta-lactam allergies continue to pose a risk to patient care, as patients with a documented allergy are often prescribed suboptimal antibiotic agents to avoid beta-lactam therapy. If a patient reports a beta-lactam allergy, several steps should be taken confirm the allergy. All patients reporting a beta-lactam allergy should undergo a detailed allergy assessment, followed by PST if necessary. In patients with confirmed type I allergies, beta-lactam desensitization may be considered as a means of safely administering beta-lactam therapy on a temporary basis.
As medication experts, pharmacists are particularly skilled in managing and offering insight into beta-lactam allergies. Their value has been established in areas including the initial allergy assessment, penicillin skin testing, antibiotic desensitization, and evaluating the risk of cross-reactivity to assist with appropriate antibiotic selection.
Author Contributions
Conceptualization, N.B. and Y.L.; writing—original draft preparation, N.B., Y.L., D.W.; writing—review and editing, N.B., Y.L., D.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- McClimon, B.; Park, M. Beta-Lactam Antibiotic Allergy. Infectious Disease and Antimicrobial Agents. Available online: http://www.antimicrobe.org/e35.asp (accessed on 8 June 2021).
- Macy, E. Penicillin and Beta-Lactam Allergy: Epidemiology and Diagnosis. Curr. Allergy Asthma Rep. 2014, 14, 1–7. [Google Scholar] [CrossRef]
- Patterson, R.A.; Stankewicz, H.A. Penicillin Allergy. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2020. Available online: https://www.ncbi.nlm.nih.gov/books/NBK459320/ (accessed on 2 January 2021).
- Centers for Disease Control and Prevention [Internet]. Is It Really a Penicillin Allergy. Available online: https://www.cdc.gov/antibiotic-use/community/pdfs/penicillin-factsheet.pdf (accessed on 2 April 2021).
- Jones, B.M.; Jozefczyk, C.; Maguire, C.; Milliken, S.; Weisz, E.E.; Bland, C.M. Beta-lactam Allergy Review: Implications for Antimicrobial Stewardship Programs. Curr. Treat. Options Infect. Dis. 2019, 11, 103–114. [Google Scholar] [CrossRef]
- Parham, P. The Immune System, 4th ed.; Garland Science, Taylor & Francis Group, LLC: New York, NY, USA, 2021. [Google Scholar]
- Shenoy, E.S.; Macy, E.; Rowe, T.; Blumenthal, K.G. Evaluation and Management of Penicillin Allergy. JAMA 2019, 321, 188–199. [Google Scholar] [CrossRef] [PubMed]
- Apter, A.J.; Schelleman, H.; Walker, A.; Addya, K.; Rebbeck, T. Clinical and genetic risk factors of self-reported penicillin allergy. J Allergy Clin Immunol. 2008, 122, 152–158. [Google Scholar] [CrossRef] [PubMed]
- Nicoletti, P.; Carr, D.F.; Barrett, S.; McEvoy, L.; Friedmann, P.S.; Shear, N.H.; Nelson, M.R.; Chiriac, A.M.; Blanca-López, N.; Cornejo-García, J.A.; et al. Beta-lactam-induced immediate hypersensitivity reactions: A genome-wide association study of a deeply phenotyped cohort. J. Allergy Clin. Immunol. 2021, 147, 1830–1837.e15. [Google Scholar] [CrossRef] [PubMed]
- Park, M.A.; Matesic, D.; Markus, P.J.; Li, J.T.-C. Female sex as a risk factor for penicillin allergy. Ann. Allergy Asthma Immunol. 2007, 99, 54–58. [Google Scholar] [CrossRef]
- Kelkar, P.S.; Li, J.T. Cephalosporin allergy. N. Engl. J. Med. 2001, 345, 804–809. [Google Scholar] [CrossRef]
- Zagursky, R.J.; Pichichero, M.E. Cross-reactivity in β-Lactam Allergy. J. Allergy Clin. Immunol. Pract. 2018, 6, 72–81.e1. [Google Scholar] [CrossRef]
- Gueant, J.L.; Gueant-Rodriguez, R.M.; Viola, M.; Valluzzi, R.L.; Romano, A. IgE mediated hypersensitivity to cephalosporins. Curr. Pharm. Des. 2006, 12, 3335–3345. [Google Scholar] [CrossRef]
- Krey, S.C.; Waise, J.; Skrupky, L.P. Confronting the Challenge of Beta-Lactam Allergies: A Quasi-Experimental Study Assessing Impact of Pharmacy-Led Interventions. J. Pharm. Pr. 2017, 32, 139–146. [Google Scholar] [CrossRef]
- Chaudhry, S.B.; Veve, M.P.; Wagner, J.L. Cephalosporins: A Focus on Side Chains and β-Lactam Cross-Reactivity. Pharmacy 2019, 7, 103. [Google Scholar] [CrossRef]
- Kula, B.; Djordjevic, G.; Robinson, J.L. A systematic review: Can one prescribe carbapenems to patients with IgE-mediated allergy to penicillins or cephalosporins? Clin. Infect. Dis. 2014, 59, 1113–1122. [Google Scholar] [CrossRef]
- Gaeta, F.; Valluzzi, R.L.; Alonzi, C.; Maggioletti, M.; Caruso, C.; Romano, A. Tolerability of aztreonam and carbapenems in patients with IgE-mediated hypersensitivity to penicillins. J. Allergy Clin. Immunol. 2015, 135, 972–976. [Google Scholar] [CrossRef]
- Lee, Y.; Bradley, N. Overview and Insights into Carbapenem Allergy. Pharmacy 2019, 7, 110. [Google Scholar] [CrossRef]
- Chua, K.Y.L.; Vogrin, S.; Bury, S.; Douglas, A.; E Holmes, N.; Tan, N.; Brusco, N.K.; Hall, R.; Lambros, B.; Lean, J.; et al. The Penicillin Allergy Delabeling Program: A Multicenter Whole-of-Hospital Health Services Intervention and Comparative Effectiveness Study. Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef] [PubMed]
- Trubiano, J.; Phillips, E. Antimicrobial stewardship’s new weapon? A review of antibiotic allergy and pathways to “de-labeling”. Curr. Opin. Infect. Dis. 2013, 26, 526–537. [Google Scholar] [PubMed]
- Rose, M.T.; Salvin, M.; Trubiano, J. The democratization of de-labeling: A review of direct oral challenge in adults with low-risk penicillin allergy. Expert Rev Anti Infect Ther. 2020, 18, 1143–1153. [Google Scholar] [CrossRef] [PubMed]
- Yates, A.B. Management of Patients with a History of Allergy to Beta-Lactam Antibiotics. Am. J. Med. 2008, 121, 572–576. [Google Scholar] [CrossRef]
- Bland, C.M.; Bookstaver, P.B.; Griffith, N.C.; Heil, E.L.; Jones, B.M.; Justo, J.A.; Staicu, M.L.; Torney, N.P.; Wall, G.C. A practical guide for pharmacists to successfully implement penicillin allergy skin testing. Am. J. Health Pharm. 2019, 76, 136–147. [Google Scholar] [CrossRef]
- Rimawi, R.H.; Cook, P.P.; Gooch, M.; Kabchi, B.; Ashraf, M.S.; Rimawi, B.H.; Gebregziabher, M.; Siraj, D.S. The impact of penicillin skin testing on clinical practice and antimicrobial stewardship. J. Hosp. Med. 2013, 8, 341–345. [Google Scholar] [CrossRef]
- Sogn, D.D.; Evans, R.; Shepherd, G.M.; Casale, T.B.; Condemi, J.; Greenberger, P.A.; Kohler, P.F.; Saxon, A.; Summers, R.J.; VanArsdel, P.P.; et al. Results of the National Institute of Allergy and Infectious Diseases Collaborative Clinical Trial to Test the Predictive Value of Skin Testing with Major and Minor Penicillin Derivatives in Hospitalized Adults. Arch. Intern. Med. 1992, 152, 1025–1032. [Google Scholar] [CrossRef]
- Chastain, D.B.; Hutzley, V.J.; Parekh, J.; Alegro, J.V.G. Antimicrobial Desensitization: A Review of Published Protocols. Pharmacy 2019, 7, 112. [Google Scholar] [CrossRef]
- Gonzalez-Estrada, A.; Radojicic, C. Penicillin allergy: A practical guide for clinicians. Clevel. Clin. J. Med. 2015, 82, 295–300. [Google Scholar] [CrossRef]
- Sigona, N.S.; Steele, J.M.; Miller, C.D. Impact of a pharmacist-driven beta-lactam allergy interview on inpatient antimicrobial therapy: A pilot project. J. Am. Pharm. Assoc. 2016, 56, 665–669. [Google Scholar] [CrossRef]
- Holmes, A.K.; Bennett, N.T.; Berry, T.P. Pharmacy driven assessment of appropriate antibiotic selection in patients with reported beta-lactam allergy. J. Am. Coll. Clin. Pharm. 2019, 2, 509–514. [Google Scholar] [CrossRef]
- Campbell, S.; Hauler, G.; Immler, E.L.; Seiti, S.; Dandache, P.; Srinivas, P. Pharmacist-led Penicillin Allergy Assessment in the Emergency Department Reduced Empiric Fluoroquinolone Use. Clin. Infect. Dis. 2020, 71. [Google Scholar] [CrossRef] [PubMed]
- Chamoun, C.; Bendyk, O.; Gapalani, R.; Montes, A.; Wolfel, T. Improving Penicillin Allergy Documentation and Its Effect on Antibiotic Prescribing at a Community Hospital. Abstract # 4-105. 2019 ASHP Midyear Clinical Meeting. Available online: https://midyear.ashp.org/-/media/midyear-conference/docs/2019/2019-MCM-Professional-Poster-Abstracts (accessed on 8 June 2021).
- Englert, E.; Weeks, A. Pharmacist-driven penicillin skin testing service for adults prescribed nonpreferred antibiotics in a community hospital. Am. J. Health Pharm. 2019, 76, 2060–2069. [Google Scholar] [CrossRef] [PubMed]
- Torney, N.P.; Tiberg, M.D. Description of a pharmacist-managed/administered penicillin allergy skin testing service at a community hospital. Am. J. Health Pharm. 2021. [Google Scholar] [CrossRef]
- Griffith, N.C.; Justo, J.A.; Winders, H.R.; Al-Hasan, M.N.; Mediwala, K.N.; Bookstaver, P.B. Regulatory Approval, Implementation, and Brief Assessment of a Pharmacist- and Pharmacy Trainee-Administered Penicillin Allergy Assessment and Skin Testing Program. J. Am. Coll. Clin. Pharm. 2020, 3, 1269–1279. [Google Scholar] [CrossRef]
- Chen, J.R.; Tarver, S.A.; Alvarez, K.S.; Tran, T.; Khan, D.A. A proactive approach to penicillin allergy testing in hospitalized patients. J. Allergy Clin. Immunol. Pract. 2017, 5, 686–693. [Google Scholar] [CrossRef]
- Gugkaeva, Z.; Crago, J.S.; Yasnogorodsky, M. Next step in antibiotic stewardship: Pharmacist-provided penicillin allergy testing. J. Clin. Pharm. Ther. 2017, 42, 509–512. [Google Scholar] [CrossRef] [PubMed]
- Wall, G.C.; Peters, L.; Leaders, C.B.; Willie, J.A. Pharmacist-managed service providing pencillin allergy skin tests. Am. J. Health Syst. Pharm. 2004, 61, 1271–1375. [Google Scholar] [CrossRef]
- Leis, J.A.; Palmay, L.; Ho, G.; Raybardhan, S.; Gill, S.; Kan, T.; Campbell, J.; Kiss, A.; McCready, J.B.; Das, P.; et al. Point of care B-lactam allergy skin testing by antimicrobial stewardship programs. A pragmatic multicenter prospective evalutation. Clin. Infect. Dis. 2017, 65, 1059–1065. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.J.C.; Fong, K.; Altshuler, D.; Dubrovskaya, Y.; Louie, E.; Amoroso, N.; Goldenberg, R.; Papadopoulos, J. Evaluation of Pharmacy-Developed Antibiotic Desensitization Protocols. Ann. Pharmacother. 2018, 53, 229–251. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).