Pain Treatment in Polish Emergency Medical Teams—Is the Pain Management Entitlement Being Used?—A Retrospective Study
Abstract
:1. Introduction
1.1. Pain Management Recommendations for Emergency Medical Teams and Emergency Departments in Poland
1.2. Rights of Paramedics and Emergency Nurses to Administer Analgesics
1.3. Aim
2. Methods
2.1. Study Design, Setting, and Ethical Considerations
2.2. Research Procedure
- Did the nature of the pain or injury suffered affect the type of pain treatment applied by the EMT?
- Did the type of medical rescue team (basic “P” or specialist “S”) affect the pain treatment applied?
- What kind of analgesics and routes of administration were most frequently used by the EMT?
2.3. Data Collection
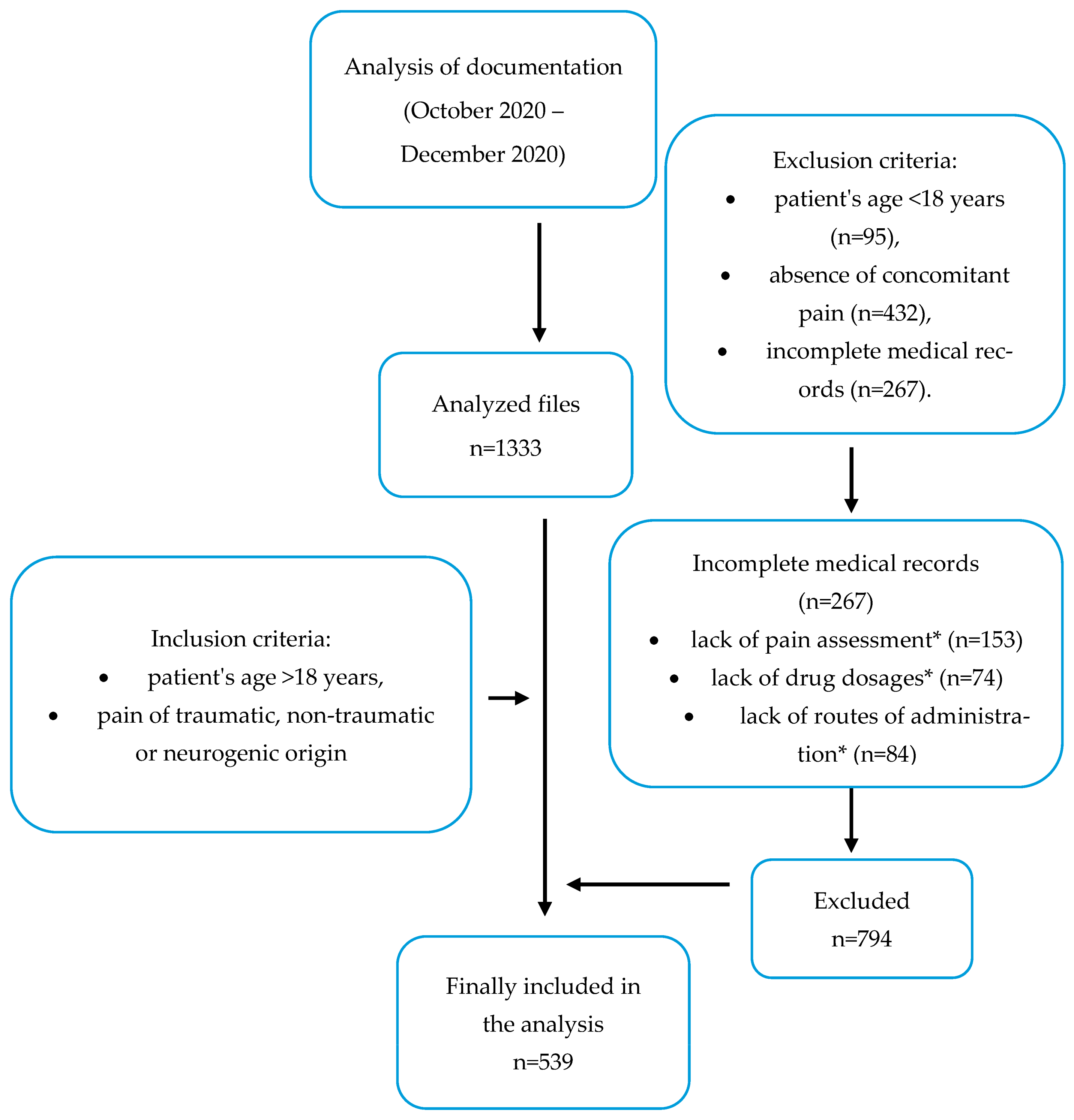
2.4. Inclusion and Exclusion Criteria of the Given Medical Records in the Analysis
- ▪
- patient’s age is over 18 years;
- ▪
- pain of traumatic, non-traumatic, or neurogenic origin.
- ▪
- patient’s age is under 18 years;
- ▪
- absence of concomitant pain;
- ▪
- incomplete medical records.
2.5. Statistics
3. Results
3.1. Characteristics of This Study Group
3.2. The Characteristics of Pain
3.3. The Analysis of Pain Treatment Implemented by the EMT
4. Discussion
5. Limitations
6. Conclusions
7. Implications for Practice
- ▪
- The vast majority of interventions were undertaken by a basic EMT consisting of paramedics and/or nurses. This indicates a significant need for pain management training and the creation of improved guidelines for these healthcare professionals.
- ▪
- A significant percentage of Emergency Medical Service interventions were undertaken in the case of pain localized in the chest. Pharmacotherapy for this specific type of pain requires experience and special training due to the specific etiology of the complaint. Moreover, the rare administration of aspirin in type ”P” emergency medical teams may indicate a need for the training of healthcare staff in this area.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Decosterd, I.; Hugli, O.; Tamchès, E.; Blanc, C.; Mouhsine, E.; Givel, J.G.; Yersin, B.; Buclin, T. Oligoanalgesia in the emergency department: Short-term beneficial effects of an education program on acute pain. Ann. Emerg. Med. 2007, 50, 462–471. [Google Scholar] [CrossRef] [PubMed]
- Wilder-Smith, O.H.G.; Möhrle, J.J.; Martin, N.C. Acute pain management after surgery or in the emergency room in Switzerland: A comparative survey of Swiss anaesthesiologists and surgeons. Eur. J. Pain 2002, 6, 189–201. [Google Scholar] [CrossRef] [PubMed]
- Wilson, J.E.; Pendleton, J.M. Oligoanalgesia in the emergency department. Am. J. Emerg. Med. 1989, 7, 620–623. [Google Scholar] [CrossRef] [PubMed]
- Friesgaard, K.D.; Paltved, C.; Nikolajsen, L. Acute pain in the emergency department: Effect of an educational intervention. Scand. J. Pain. 2017, 15, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Sampson, F.C.; O’Cathain, A.; Goodacre, S. How can pain management in the emergency department be improved? Findings from multiple case study analysis of pain management in three UK emergency departments. Emerg. Med. J. 2020, 37, 85–94. [Google Scholar] [CrossRef] [PubMed]
- IASP Announces Revised Definition of Pain. Available online: https://www.iasp-pain.org/publications/iasp-news/iasp-announces-revised-definition-of-pain/ (accessed on 15 November 2021).
- Stephan, F.P.; Nickel, C.N.; Martin, J.S.; Grether, D.; Delport-Lehnena, K.; Bingisser, R. Pain in the emergency department: Adherence to an implemented treatment protocol. Swiss Med. Wkly. 2010, 140, 334–341. [Google Scholar] [PubMed]
- Act of 8 September 2006 on the National Medical Rescue Service; Journal of Laws of 2006 No. 1410. Available online: https://isap.sejm.gov.pl/isap.nsf/DocDetails.xsp?id=WDU20061911410 (accessed on 25 November 2021).
- Krzyżanowski, K.; Ślęzak, D.; Basiński, A.; Żuratyński, P.; Buca, P. Uśmierzanie bólu po urazie na etapie przedszpitalnym—Wyniki wstępne. Ból 2017, 18, 37–43. [Google Scholar] [CrossRef]
- Dobre Praktyki Leczenia Bólu. Available online: https://www.gov.pl/web/zdrowie/dobre-praktyki-leczenia-bolu (accessed on 25 November 2021).
- The Regulation of the Minister of Health of 16 December 2019 on Medical Rescue Activities and Health Services Other than Medical Rescue Activities That May Be Provided by a Paramedic. Available online: http://isap.sejm.gov.pl/isap.nsf/DocDetails.xsp?id=WDU20190002478 (accessed on 25 November 2021).
- Regulation of the Minister of Health of 28 February 2017 on the Nature and Extent of Preventive, Diagnostic, Therapeutic, and Rehabilitation Services Independently Provided by a Nurse or a Midwife without the Physician’s Order. Available online: http://isap.sejm.gov.pl/isap.nsf/DocDetails.xsp?id=wdu20170000497 (accessed on 25 November 2021).
- International Pain Summit of the International Association for the Study of Pain. Declaration of Montréal: Declaration That Access to Pain Management Is a Fundamental Human Right. J. Pain Palliat. Care Pharmacother. 2011, 25, 29–31. [CrossRef] [PubMed]
- Van Woerden, G.; Van Den Brand, C.L.; Den Hartog, C.F.; Idenburg, F.J.; Grootendorst, D.C.; Van Der Linden, M.C. Increased analgesia administration in emergency medicine after implementation of revised guidelines. Int. J. Emerg. Med. 2016, 9, 4. [Google Scholar] [CrossRef] [PubMed]
- Albrecht, E.; Taffe, P.; Yersin, B.; Schoettker, P.; Decosterd, I.; Hugli, O. Undertreatment of acute pain (oligoanalgesia) and medical practice variation in prehospital analgesia of adult trauma patients: A 10 yr retrospective study. Br. J. Anaesth. 2013, 110, 96–106. [Google Scholar] [CrossRef] [PubMed]
- European Society for Emergency Medicine (EUSEM). Guidelines for the Management of Acute Pain in Emergency Situations. 2020. Available online: https://eusem.org/images/EUSEM_EPI_GUIDELINES_MARCH_2020.pdf (accessed on 25 April 2023).
- Pieretti, S.; Di Giannuario, A.; Di Giovannandrea, R.; Marzoli, F.; Piccaro, G.; Minosi, P.; Aloisi, A.M. Gender differences in pain and its relief. Ann. Ist. Super. Sanità 2016, 52, 184–189. [Google Scholar] [CrossRef] [PubMed]
- Yousefifard, M.; Askarian-Amiri, S.; Neishaboori, A.M.; Sadeghi, M.; Saberian, P.; Baratloo, A. Pre-hospital pain management; a systematic review of proposed guidelines. Arch. Acad. Emerg. Med. 2019, 7, e55. [Google Scholar] [CrossRef] [PubMed]
- Silka, P.A.; Roth, M.M.; Moreno, G.; Merrill, L.; Geiderman, J.M. Pain Scores Improve Analgesic Administration Patterns for Trauma Patients in the Emergency Department. Acad. Emerg. Med. 2004, 11, 264–270. [Google Scholar] [CrossRef] [PubMed]
- Zideman, D.A.; Singletary, E.M.; Borra, V.; Cassan, P.; Cimpoesu, C.D.; De Buck, E.; Djaerv, T.; Handley, A.J.; Klaassen, B.; Meyran, D.; et al. European Resuscitation Council Guidelines 2021: First aid. Resuscitation 2021, 161, 270–290. [Google Scholar] [CrossRef] [PubMed]
- Pistoia, F.; Sacco, S.; Sarà, M.; Carolei, A. The perception of pain and its management in disorders of consciousness topical collection on psychiatric management of pain. Curr. Pain Headache Rep. 2013, 17, 374. [Google Scholar] [CrossRef] [PubMed]
- Dijkstra, B.M.; Berben, S.A.A.; Van Dongen, R.T.M.; Schoonhoven, L. Review on pharmacological pain management in trauma patients in (pre-hospital) emergency medicine in the Netherlands. Eur. J. Pain 2014, 18, 3–19. [Google Scholar] [CrossRef] [PubMed]

| Paramedic/Emergency Nurse 1 | |
|---|---|
| Medication | Routes of Administration |
| Aspirin | tablets |
| Drotaverine | solution for injection |
| Fentanyl | solution for injection |
| Ibuprofen | tablets |
| Ketoprofen | tablets, solution for injection |
| Lidocaine | solution for injection, gel |
| Magnesium | solution for injection |
| Metamizole | solution for injection |
| Morphine | solution for injection |
| Papaverine | solution for injection |
| Paracetamol | tablets, solution for injection |
| Type of EMT | N | % | |
|---|---|---|---|
| Basic “P” | 453 | 84.04% | |
| Leader of the team 1 | Paramedic | 449 | 98.12% |
| Nurse | 4 | 0.88% | |
| Specialist “S” | 86 | 15.96% | |
| Leader of the team 2 | Paramedic | 8 | 9.30% |
| Doctor | 74 | 86.05% | |
| Nurse | 4 | 4.65% | |
| Leader of the team (”S” and ”P”) 3 | Paramedic | 457 | 84.78% |
| Doctor | 74 | 13.74% | |
| Nurse | 8 | 1.48% |
| N | % 1 | ||
|---|---|---|---|
| The nature of pain | acute | 323 | 59.92 |
| traumatic | 180 | 33.39 | |
| neuropathic | 26 | 4.82 | |
| chronic | 10 | 1.85 | |
| Non-traumatic pain 2 | abdominal pain | 94 | 17.43 |
| chest pain | 205 | 38.03 | |
| Traumatic pain | head trauma | 70 | 12.99 |
| chest trauma | 13 | 2.41 | |
| upper limb trauma | 20 | 3.71 | |
| lower limb trauma | 37 | 6.86 | |
| multiple injuries | 40 | 7.42 | |
| other 3 | 34 | 6.3 | |
| N | % 1 | |
|---|---|---|
| 0 | 56 | 10.39 |
| 1 | 24 | 4.45 |
| 2 | 70 | 12.99 |
| 3 | 82 | 15.21 |
| 4 | 74 | 13.72 |
| 5 | 65 | 12.05 |
| 6 | 39 | 7.23 |
| 7 | 43 | 7.98 |
| 8 | 28 | 5.2 |
| 9 | 13 | 2.41 |
| 10 | 14 | 2.59 |
| impossible to evaluate 2 | 31 | 5.75 |
| Implemented Treatment | Acute (n = 323) | Chronic (n = 10) | Neuropathic (n = 26) | Traumatic (n = 180) | Chi2 | df | p |
|---|---|---|---|---|---|---|---|
| acetylsalicylic acid | n = 33 | n = 0 | n = 0 | n = 1 | 20.85 | 3 | 0.000 |
| 10.22% | 0.00% | 0.00% | 0.56% | ||||
| fentanyl | n = 2 | n = 0 | n = 3 | n = 16 | 25.71 | 3 | 0.000 |
| 0.62% | 0.00% | 11.54% | 8.89% | ||||
| papaverine | n = 10 | n = 1 | n = 1 | n = 0 | 8.31 | 3 | 0.040 |
| 3.10% | 10.00% | 3.85% | 0.00% | ||||
| drotaverine | n = 36 | n = 0 | n = 1 | n = 0 | 23.63 | 3 | 0.000 |
| 11.15% | 0.00% | 3.85% | 0.00% |
| Implemented Treatment | Mild (n = 108) | Moderate (n = 234) | Severe (n = 34) | Chi2 | df | p |
|---|---|---|---|---|---|---|
| Paracetamol | n = 23 | n = 67 | n = 9 | 2.05 | 2 | 0.359 |
| 21.30% | 28.63% | 26.47% | ||||
| Metamizole | n = 4 | n = 45 | n = 7 | 15.01 | 2 | 0.001 |
| 3.70% | 19.23% | 20.59% | ||||
| Ketoprofen | n = 9 | n = 40 | n = 8 | 6.45 | 2 | 0.040 |
| 8.33% | 17.09% | 23.53% | ||||
| Morphine | n = 0 | n = 1 | n = 1 | 4.36 | 2 | 0.113 |
| 0.00% | 0.43% | 2.94% | ||||
| Fentanyl | n = 0 | n = 1 | n = 0 | 0.61 | 2 | 0.738 |
| 0.00% | 0.43% | 0.00% | ||||
| Drotaverine | n = 1 | n = 4 | n = 1 | 0.72 | 2 | 0.698 |
| 0.93% | 1.71% | 2.94% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pryba, B.; Mędrzycka-Dąbrowska, W.; Małecka-Dubiela, A. Pain Treatment in Polish Emergency Medical Teams—Is the Pain Management Entitlement Being Used?—A Retrospective Study. Safety 2023, 9, 74. https://doi.org/10.3390/safety9040074
Pryba B, Mędrzycka-Dąbrowska W, Małecka-Dubiela A. Pain Treatment in Polish Emergency Medical Teams—Is the Pain Management Entitlement Being Used?—A Retrospective Study. Safety. 2023; 9(4):74. https://doi.org/10.3390/safety9040074
Chicago/Turabian StylePryba, Bartosz, Wioletta Mędrzycka-Dąbrowska, and Anna Małecka-Dubiela. 2023. "Pain Treatment in Polish Emergency Medical Teams—Is the Pain Management Entitlement Being Used?—A Retrospective Study" Safety 9, no. 4: 74. https://doi.org/10.3390/safety9040074
APA StylePryba, B., Mędrzycka-Dąbrowska, W., & Małecka-Dubiela, A. (2023). Pain Treatment in Polish Emergency Medical Teams—Is the Pain Management Entitlement Being Used?—A Retrospective Study. Safety, 9(4), 74. https://doi.org/10.3390/safety9040074







