From FRAM Guidelines to Reality: Incorporating Stakeholder Variability in Work-as-Done in Healthcare
Abstract
1. Introduction
2. Materials and Methods
2.1. Components of FRAM Visualisations
2.2. Design
2.3. Ethical Approval
2.4. Participants
2.5. Data Collection
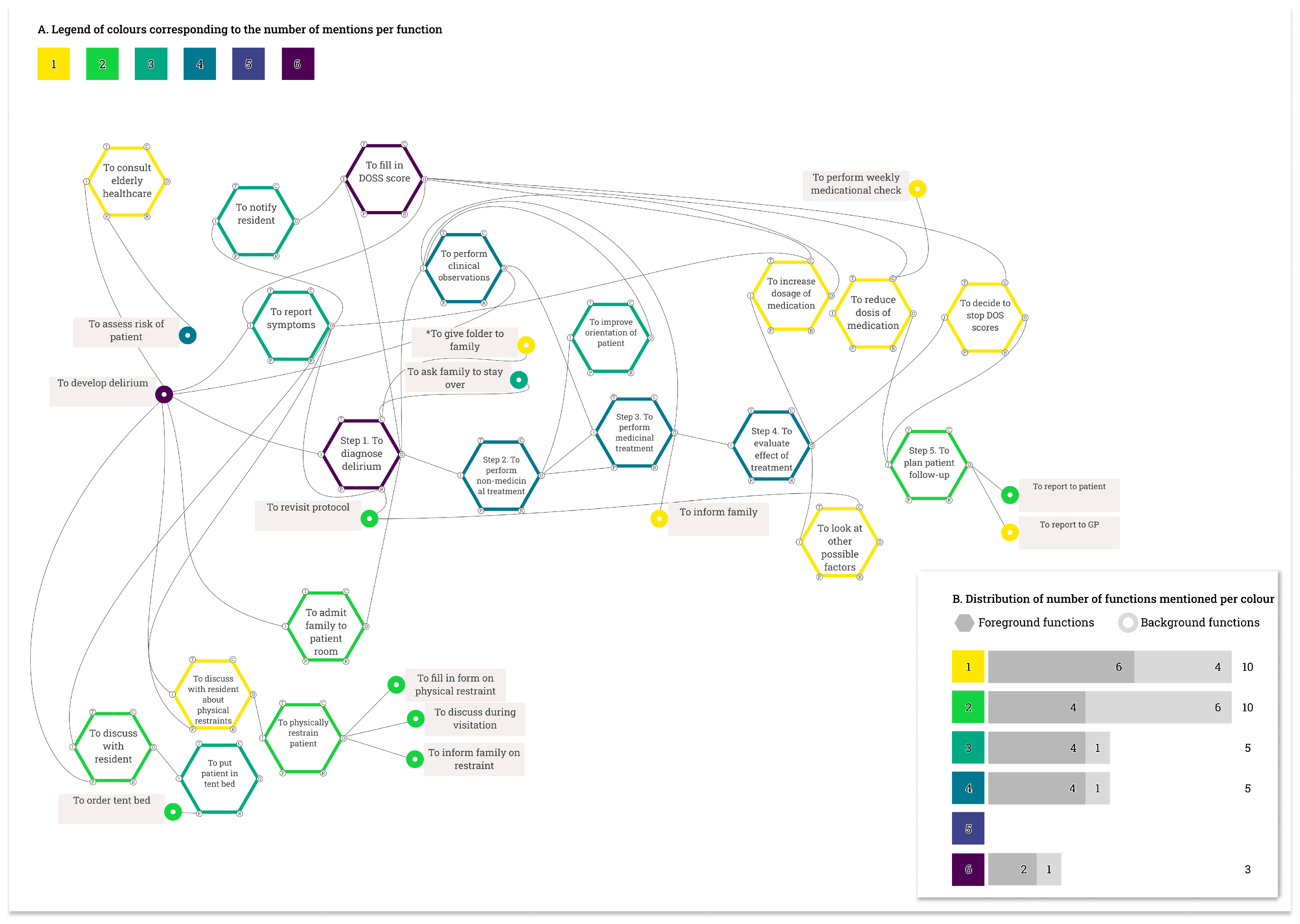
2.5.1. Case Study 1: Delirium Management
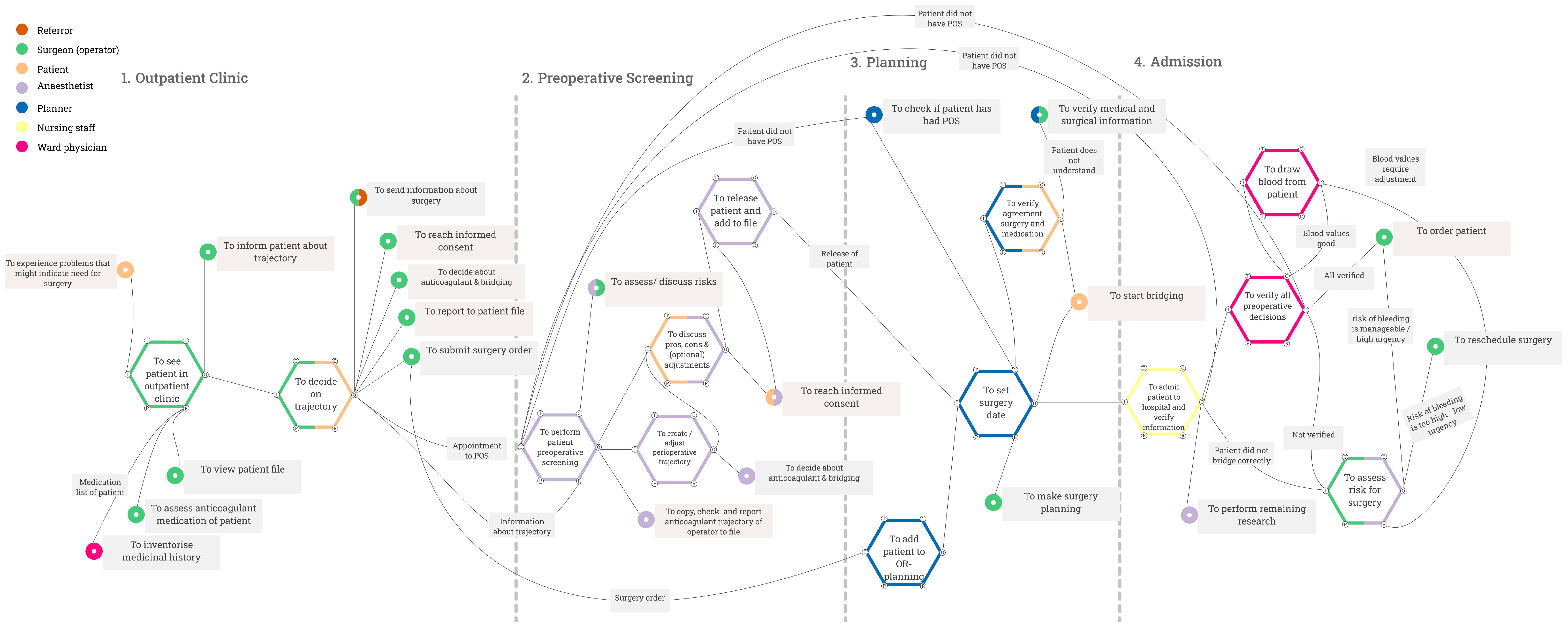
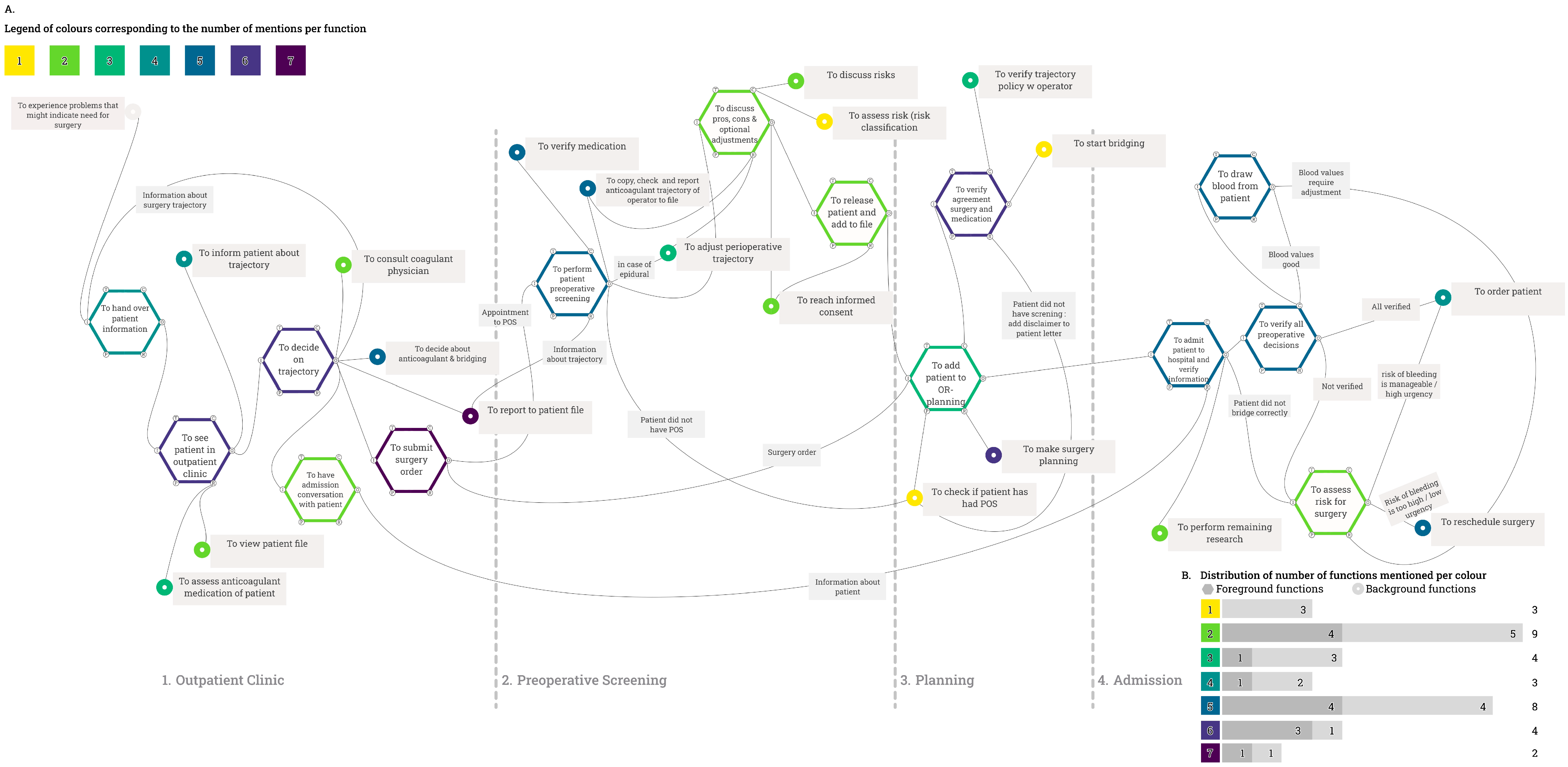
2.5.2. Case Study 2: Anticoagulant Medication in the Peri-Operative Process
2.6. FRAM Visualisations
2.7. Outcome Measures
2.8. Analyses
3. Results
3.1. Case Study 1: Delirium Management
3.1.1. Between-Stakeholder Variability in Work-as-Done
3.1.2. Impact on Differences Between Work-as-Imagined and Work-as-Done
3.2. Case Study 2: Anticoagulants in the Perioperative Process
3.2.1. Between-Stakeholder Variability in Work-as-Done
3.2.2. Impact on Differences Between Work-as-Imagined and Work-as-Done
4. Discussion
4.1. Strengths and Limitations
4.2. Practical Implications and Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| FRAM | Functional Resonance Analysis Method |
| H1 | Hospital 1 |
| H2 | Hospital 2 |
Appendix A
Appendix A.1. Interview Formats per Case Study
Appendix A.1.1. Case Study 1: Delirium Diagnosis and Management
| General Questions | |
| 1. | What are the steps from the moment that it is suspected that a patient has a delirium? |
| 2. | How is a patient diagnosed with delirium? |
| 3. | If something changes about the treatment plan of a patient, on the basis of what (kind of) information are such decisions made? |
| 4. | Do you use the protocol of delirium? If yes, how do you use it? |
| 5. | To what extent is what is done in practice in line with how the protocol of delirium is written? Why is this (not) done? |
| 6. | If you deviate from a protocol, do you report this? Why (not)? |
| 7. | Are you educated periodically about delirium and its protocol? |
| Added questions | |
| 1. | Can you please tell me about the preventive measures that you take if a patient has an (increased) risk to develop delirium? |
| 2. | Could you please tell me about non-medicinal interventions that are performed on patients who show signs of delirium or are diagnosed with delirium? |
| 3. | Could you please tell me about medicinal interventions that are performed on patients who show signs of delirium or are diagnosed with delirium? |
| 4. | When are freedom-restricting measures used on patients who show signs of delirium or are diagnosed with delirium? |
| 5. | How do you indicate whether the patient shows more/fewer symptoms? |
| 6. | When do you mention any specifics about the patient to the doctor? (only asked nursing staff) |
| 7. | Can you please tell me about the aftercare of a patient? |
| 8. | From what moment do you initiate the aftercare of a patient? |
| 9. | How do you receive the information that a patient shows signs of delirium? (only asked doctors) |
Appendix A.1.2. Case Study 2: Perioperative Anticoagulants
- Phase 1. Introduction
- Phase 2. The steps
- Step 1. The inpatient clinic of the surgeon.
- Step 2. Preoperative screening
- Step 3. Planning
- Step 4. Admission of the patient
- What is being communicated between professionals?
- Distinction between responsibility and execution
- Where is information documented or saved?
- Phase 3. Summary and conclusion
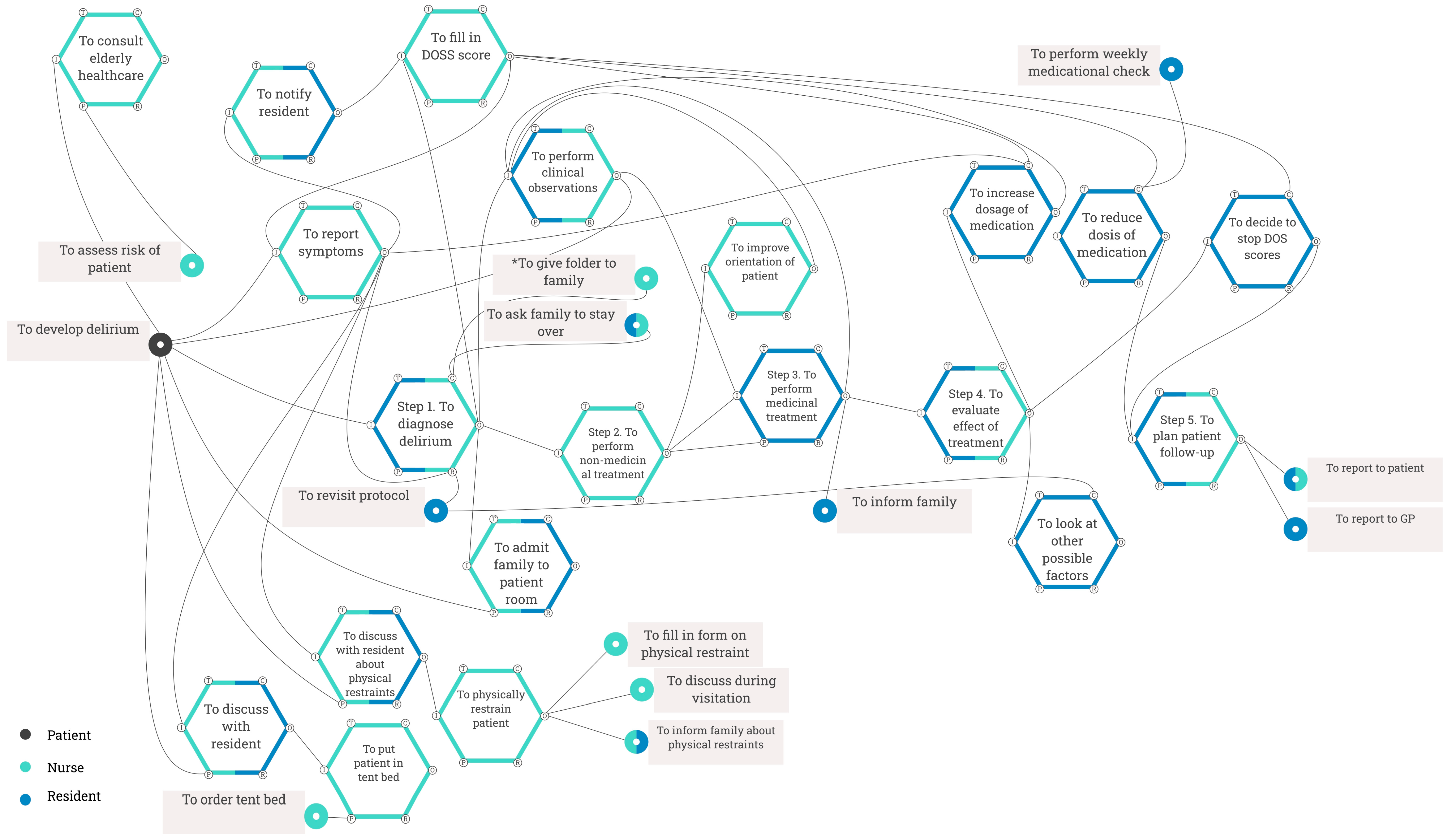
Appendix B. FRAM Visualisations of Case Study 1
Appendix B.1. Work-as-Imagined
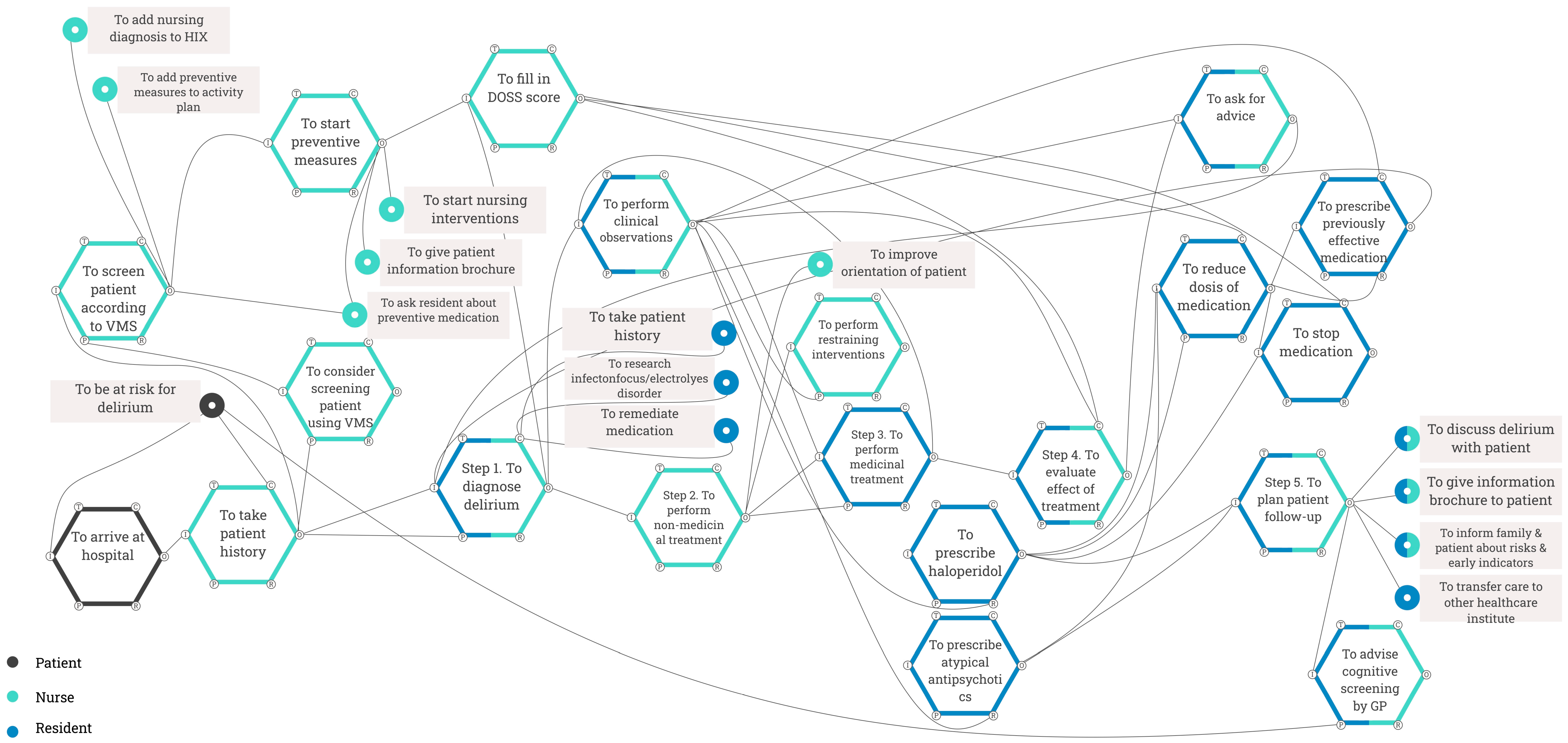
Appendix B.2. Work-as-Done
Appendix C. FRAM Visualisations of Case Study 2
Appendix C.1. Work-as-Imagined Hospital 1
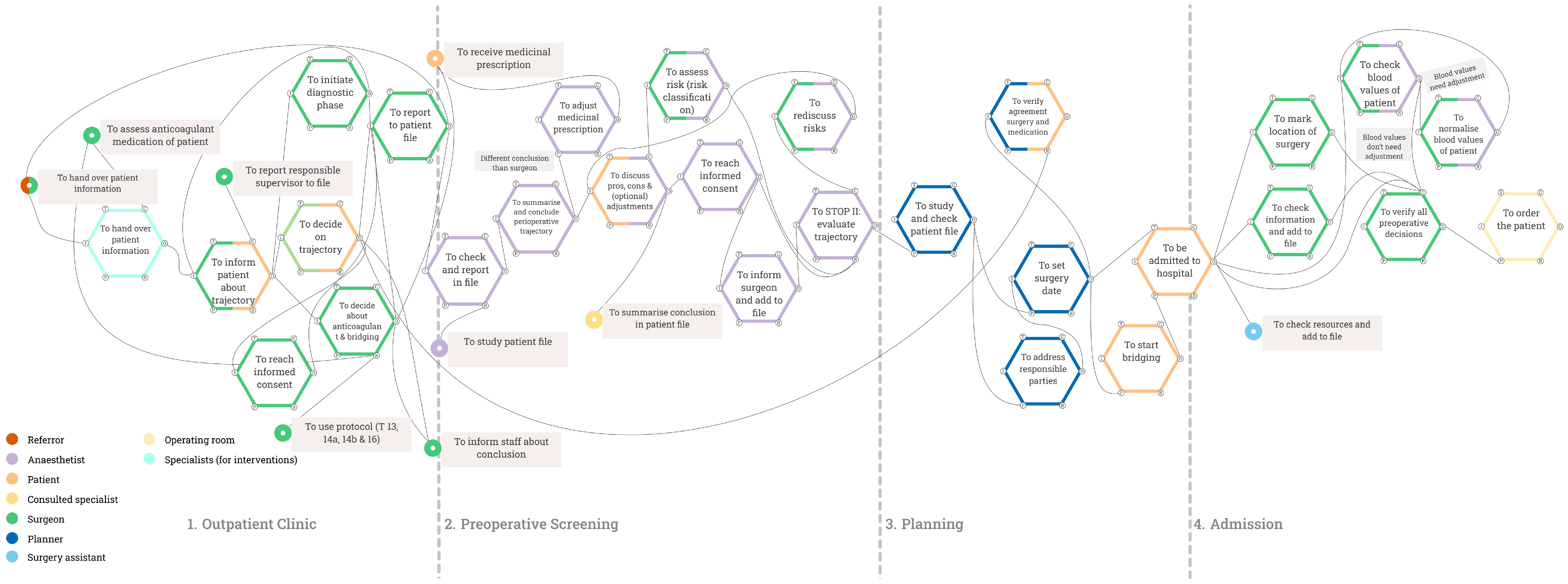
Appendix C.2. Work-as-Done Hospital 1
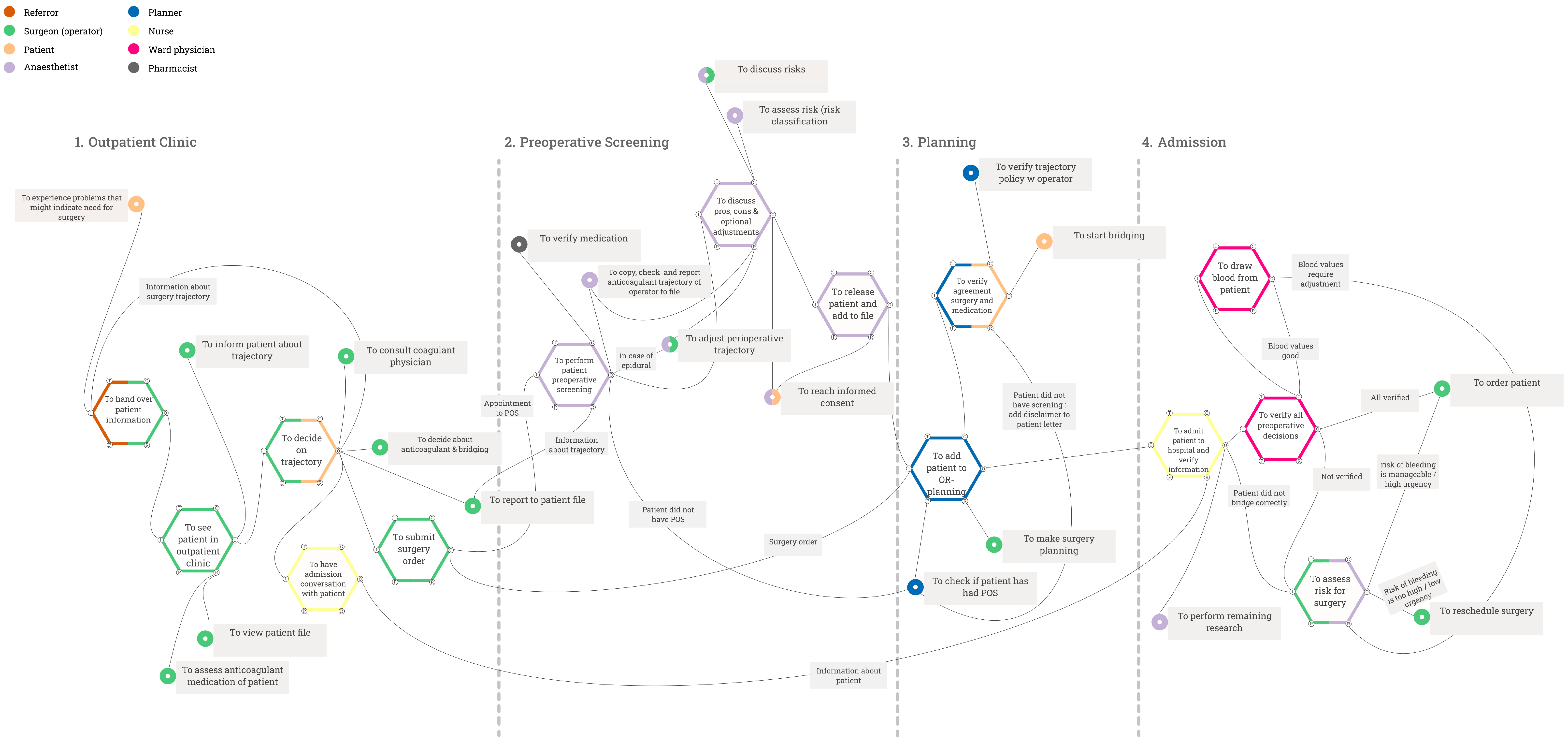
Appendix C.3. Work-as-Imagined Hospital 2

Appendix C.4. Work-as-Done Hospital 2
References
- Patriarca, R.; Di Gravio, G.; Woltjer, R.; Costantino, F.; Praetorius, G.; Ferreira, P.; Hollnagel, E. Framing the FRAM: A literature review on the functional resonance analysis method. Saf. Sci. 2020, 129, 104827. [Google Scholar] [CrossRef]
- Rad, M.A.; Lefsrud, L.M.; Hendry, M.T. Application of systems thinking accident analysis methods: A review for railways. Saf. Sci. 2023, 160, 106066. [Google Scholar] [CrossRef]
- Reiser, C.; Villani, E.; Junior, M.M.C. The Functional Resonance Analysis Method (FRAM) on Aviation: A Systematic Review. In Proceedings of the 33rd European Safety and Reliability Conference (ESREL 2023), Southampton, UK, 3–8 September 2023; pp. 304–311. [Google Scholar] [CrossRef]
- Tian, W.; Caponecchia, C. Using the Functional Resonance Analysis Method (FRAM) in Aviation Safety: A Systematic Review. J. Adv. Transp. 2020, 2020, 8898903. [Google Scholar] [CrossRef]
- Hollnagel, E. FRAM: The Functional Resonance Analysis Method; CRC Press: Boca Raton, FL, USA, 2012. [Google Scholar] [CrossRef]
- Damen, N.L.; de Vos, M.S.; Moesker, M.J.; Braithwaite, J.; de van Wijngaarden, R.A.F.L.; Kaplan, J.; Hamming, J.F.; Clay-Williams, R. Preoperative Anticoagulation Management in Everyday Clinical Practice: An International Comparative Analysis of Work-as-Done Using the Functional Resonance Analysis Method. J. Patient Saf. 2021, 17, 157–165. [Google Scholar] [CrossRef]
- Schreurs, R.H.P.; Joore, M.A.; Ten Cate, H.; Ten Cate-Hoek, A.J. Using the Functional Resonance Analysis Method to explore how elastic compression therapy is organised and could be improved from a multistakeholder perspective. BMJ Open 2021, 11, e048331. [Google Scholar] [CrossRef]
- Tresfon, J.; Langeveld, K.; Brunsveld-Reinders, A.H.; Hamming, J. Coming to Grips—How Nurses Deal With Restlessness, Confusion, and Physical Restraints on a Neurological/Neurosurgical Ward. Glob. Qual. Nurs. Res. 2023, 10, 23333936221148816. [Google Scholar] [CrossRef]
- Hedqvist, A.T.; Praetorius, G.; Ekstedt, M. Exploring interdependencies, vulnerabilities, gaps and bridges in care transitions of patients with complex care needs using the Functional Resonance Analysis Method. BMC Health Serv. Res. 2023, 23, 851. [Google Scholar] [CrossRef]
- Fargnoli, M.; Murgianu, L.; Tronci, M. The Functional Resonance Analysis Method (FRAM) Application in the Healthcare Sector: Lessons Learned from Two Case Studies on Medical Device Management. Appl. Sci. 2024, 14, 9495. [Google Scholar] [CrossRef]
- Op’t Hoog, S.A.J.J.; van Mersbergen-De Bruin, M.P.J.; Damen, N.L.M.; Chaboyer, W.; Weggelaar-Jansen, A.M.; Eskes, A.M.; Vloet, L.C.M.; Vermeulen, H. Learning by Visualize a Nurse-Led CCOS Using the Functional Resonance Analysis Method. J. Patient Saf. 2024, 21, 15–23. [Google Scholar] [CrossRef]
- van Stralen, S.A.; van Eikenhorst, L.; Vonk, A.S.; Schutijser, B.C.F.M.; Wagner, C. Evaluating deviations and considerations in daily practice when double-checking high-risk medication administration: A qualitative study using the FRAM. Heliyon 2024, 10, e25637. [Google Scholar] [CrossRef]
- Meulman, M.D.; Merten, H.; Van Munster, B.; Wagner, C. Comparing Guidelines to Daily Practice When Screening Older Patients for the Risk of Functional Decline in Hospitals: Outcomes of a Functional Resonance Analysis Method (FRAM) Study. J. Patient Saf. 2024, 20, 461–473. [Google Scholar] [CrossRef] [PubMed]
- McGill, A.; Smith, D.; McCloskey, R.; Morris, P.; Goudreau, A.; Veitch, B. The Functional Resonance Analysis Method as a health care research methodology: A scoping review. JBI Evid. Synth. 2022, 20, 1074–1097. [Google Scholar] [CrossRef] [PubMed]
- Salehi, V.; Veitch, B.; Smith, D. Modeling complex socio-technical systems using the FRAM: A literature review. Hum. Factors Ergon. Manuf. 2021, 31, 118–142. [Google Scholar] [CrossRef]
- McGill, A.; McCloskey, R.; Smith, D.; Veitch, B. Establishing Trustworthiness in Health Care Process Modelling: A Practical Guide to Quality Enhancement in Studies Using the Functional Resonance Analysis Method. Int. J. Qual. Methods 2023, 22, 16094069231183616. [Google Scholar] [CrossRef]
- Tresfon, J.; Brunsveld-Reinders, A.H.; Van Valkenburg, D.; Langeveld, K.; Hamming, J. Aligning work-as-imagined and work-as-done using FRAM on a hospital ward: A roadmap. BMJ Open Qual. 2022, 11, e001992. [Google Scholar] [CrossRef]
- Edgar, L.; Jones, M.D., Jr.; Harsy, B.; Passiment, M. Better Decision-Making: Shared Mental Models and the Clinical Competency Committee. J. Grad. Med. Educ. 2021, 13, 51–58. [Google Scholar] [CrossRef]
- Verhagen, M.J.; De Vos, M.S.; Van Schaik, J. Surgical team dynamics in a reflective team meeting to improve quality of care: Qualitative analysis of a shared. Br. J. Surg. 2023, 110, 1271–1275. [Google Scholar] [CrossRef]
- Inouye, S.K.; Westendorp, R.G.J.; Saczynski, J.S. Delirium in elderly people. Lancet 2014, 383, 911–922. [Google Scholar] [CrossRef]
- Dreijer, A.R.; Diepstraten, J.; Bukkems, V.E.; Mol, P.G.M.; Leebeek, F.W.G.; Kruip, M.J.H.A.; van den Bemt, P.M. Anticoagulant medication errors in hospitals and primary care: A cross-sectional study. Int. J. Qual. Health Care 2019, 31, 346–352. [Google Scholar] [CrossRef]
- The FRAM Model Visualiser. 2012. Available online: https://functionalresonance.com/the-fram-model-visualiser/ (accessed on 14 March 2025).
- Figma Version 124.4.7. 2016. Available online: https://www.figma.com/ (accessed on 14 March 2025).
- Mohammed, S.; Ferzandi, L.; Hamilton, K. Metaphor No More: A 15-Year Review of the Team Mental Model Construct. J. Manag. 2010, 36, 876–910. [Google Scholar] [CrossRef]
- Evans-Lacko, S.; Jarrett, M.; McCrone, P.; Thornicroft, G. Facilitators and barriers to implementing clinical care pathways. BMC Health Serv. Res. 2010, 10, 182. [Google Scholar] [CrossRef] [PubMed]
- Hudson, C.C.; Gauvin, S.; Tabanfar, R.; Poffenroth, A.M.; Lee, J.S.; O’Riordan, A.L. Promotion of role clarification in the Health Care Team Challenge. J. Interprofessional Care 2017, 31, 401–403. [Google Scholar] [CrossRef] [PubMed]

| Case Study 1 | Case Study 2 | |||
|---|---|---|---|---|
| Roles | Participants | Roles | Participants | |
| H1 | H2 | |||
| Nurse | 3 | Surgeon | 2 | 2 |
| Physician | 2 | Anaesthetist | 2 | 2 |
| Manager | 1 | Planner | 1 | 1 |
| Nurse | 1 | 1 | ||
| Recovery nurse | 1 | 1 | ||
| Ward physician | 1 | 1 | ||
| Total | 6 | 8 | 8 | |
| Work-as-Done | Work-as-Imagined | |||
|---|---|---|---|---|
| Function | Role | Function | Role | Match |
| To consult elderly healthcare | Nurse | - | - | - |
| To discuss with resident about physical restraints | Resident/ Nurse | - | - | - |
| To give folder to family | Nurse | To give patient information brochure | Nurse | Partial * |
| To inform family | Resident | - | - | - |
| To look at other possible factors | Resident | - | - | - |
| To reduce dose of medication | Resident | To reduce dose of medication | Resident | Yes |
| To perform weekly medicinal check | Resident | - | - | - |
| To increase dosage of medication | Resident | - | - | - |
| To decide to stop DOS scores | Resident | - | - | - |
| To report to GP | Resident | To transfer care to other healthcare institute | Resident | Partial |
| Hospital | Work-as-Done | Work-as-Imagined | |||
|---|---|---|---|---|---|
| Function | Role | Function | Role | Match | |
| Hospital 1 | To assess risk (risk classification) | Anaesthetist | To assess risk (risk classification) | Anaesthetist/ Surgeon | Partial |
| To check if patient had POS | Planner | - | - | - | |
| To start bridging | Patient | To start bridging | Patient | Yes | |
| Hospital 2 | To reach informed consent | Surgeon/Patient | - | - | - |
| To discuss pros, cons, and optional adjustments | Anaesthetist/Patient | To discuss pros, cons, and optional adjustments | Anaesthetist/ Patient | Yes | |
| To decide about anticoagulant and bridging | Anaesthetist | - | - | - |
| Scenario | Advantages | Disadvantages |
|---|---|---|
| Include all identified functions | Representation of all information | Might include perspectives that are not representative of most stakeholders |
| Include functions shared by multiple stakeholders and those that relate to their own work | Assumptions about the roles of other stakeholders are excluded Maintenance of detailed role-specific steps | Limits the opportunity to discuss role-based assumptions and shared learning |
| Exclude functions mentioned by only one stakeholder, regardless of role | Systematic approach Ensures functions are represented by multiple stakeholders | Relevant bottlenecks, workarounds, or functions important for safety could be missed |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Luijcks, N.M.; Marang-van de Mheen, P.J.; van der Laan, M.J.; Groeneweg, J. From FRAM Guidelines to Reality: Incorporating Stakeholder Variability in Work-as-Done in Healthcare. Safety 2025, 11, 66. https://doi.org/10.3390/safety11030066
Luijcks NM, Marang-van de Mheen PJ, van der Laan MJ, Groeneweg J. From FRAM Guidelines to Reality: Incorporating Stakeholder Variability in Work-as-Done in Healthcare. Safety. 2025; 11(3):66. https://doi.org/10.3390/safety11030066
Chicago/Turabian StyleLuijcks, Nienke M., Perla J. Marang-van de Mheen, Maarten J. van der Laan, and Jop Groeneweg. 2025. "From FRAM Guidelines to Reality: Incorporating Stakeholder Variability in Work-as-Done in Healthcare" Safety 11, no. 3: 66. https://doi.org/10.3390/safety11030066
APA StyleLuijcks, N. M., Marang-van de Mheen, P. J., van der Laan, M. J., & Groeneweg, J. (2025). From FRAM Guidelines to Reality: Incorporating Stakeholder Variability in Work-as-Done in Healthcare. Safety, 11(3), 66. https://doi.org/10.3390/safety11030066






