Insights into Women’s Occupational Health and Safety: A Decade in Review of Primary Data Studies
Abstract
1. Introduction
- Research Question 1. How much attention did research studies draw to women’s health and safety in workplaces between 2010 and 2021?
- Research Question 2. In which occupations within specific sectors have research studies primarily concentrated on the female population, examining women’s OHS in those occupations?
- Research Question 3. Based on previous research studies, what are the primary OHS challenges or issues that women face in the occupations identified from Research Question 2?
2. Materials and Methods
2.1. Search Strategy
2.2. Selection of Studies
- Only English-language articles were included. Therefore, articles in languages other than English were excluded.
- Only articles with full-text availability were included.
- Review articles, editorials, letters to the editor, articles presented at seminars and conferences, reports and books were excluded.
- Only articles that used primary data, with all or part of their participants from the female population, were included.
- Studies that included both women and men in their research but presented results in a generalized manner were excluded from the study because the focus of this review is on women’s OHS. Therefore, studies that did not present results focused on women were excluded. It is worth noting that this review does not intend to compare the OHS challenges faced by men and women. Instead, its focus is specifically on women.
- Studies that were unrelated to the human population (e.g., animal population) were excluded.
2.3. Quality Assessment of Articles
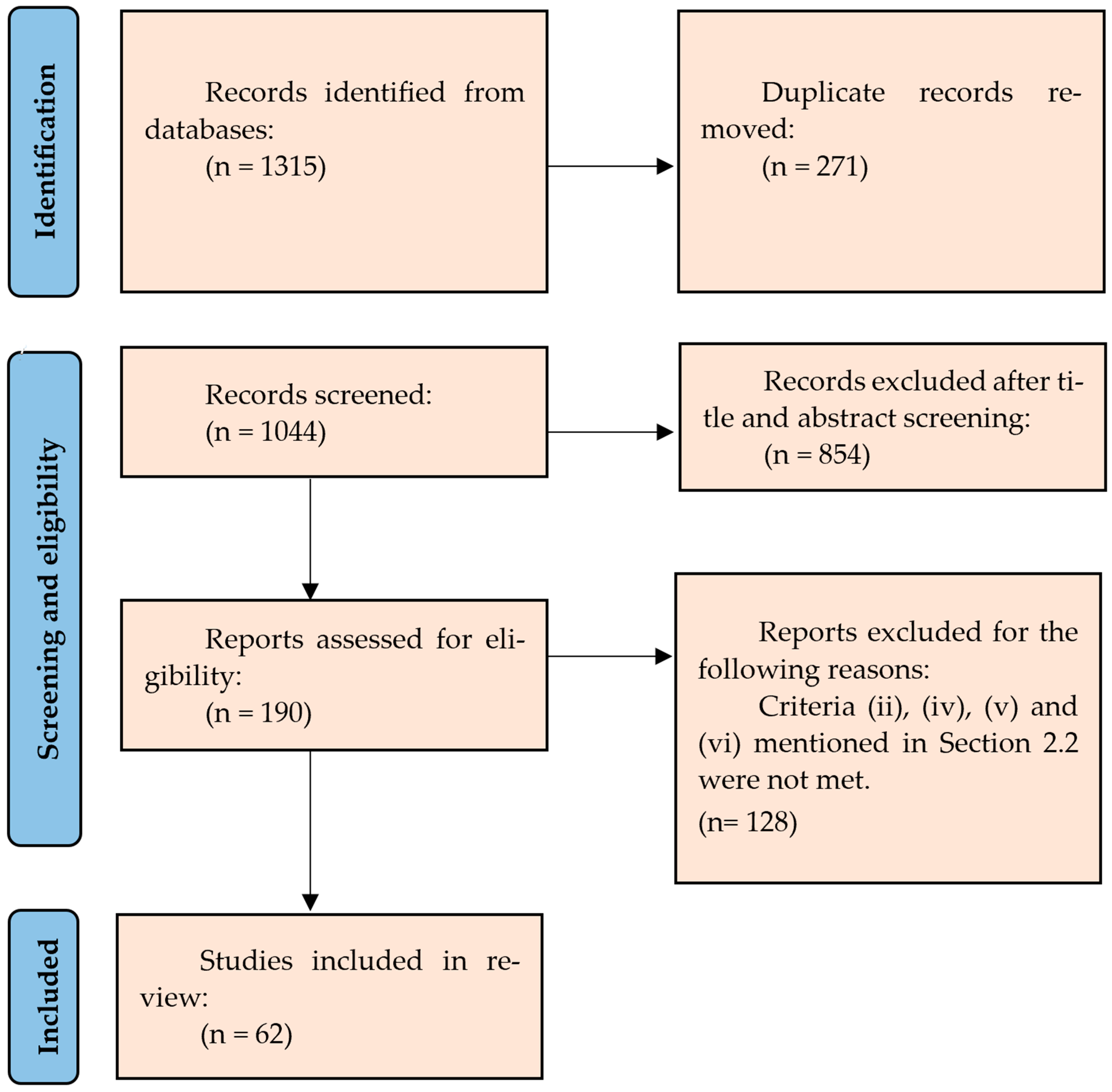
2.4. Screening Process
3. Results
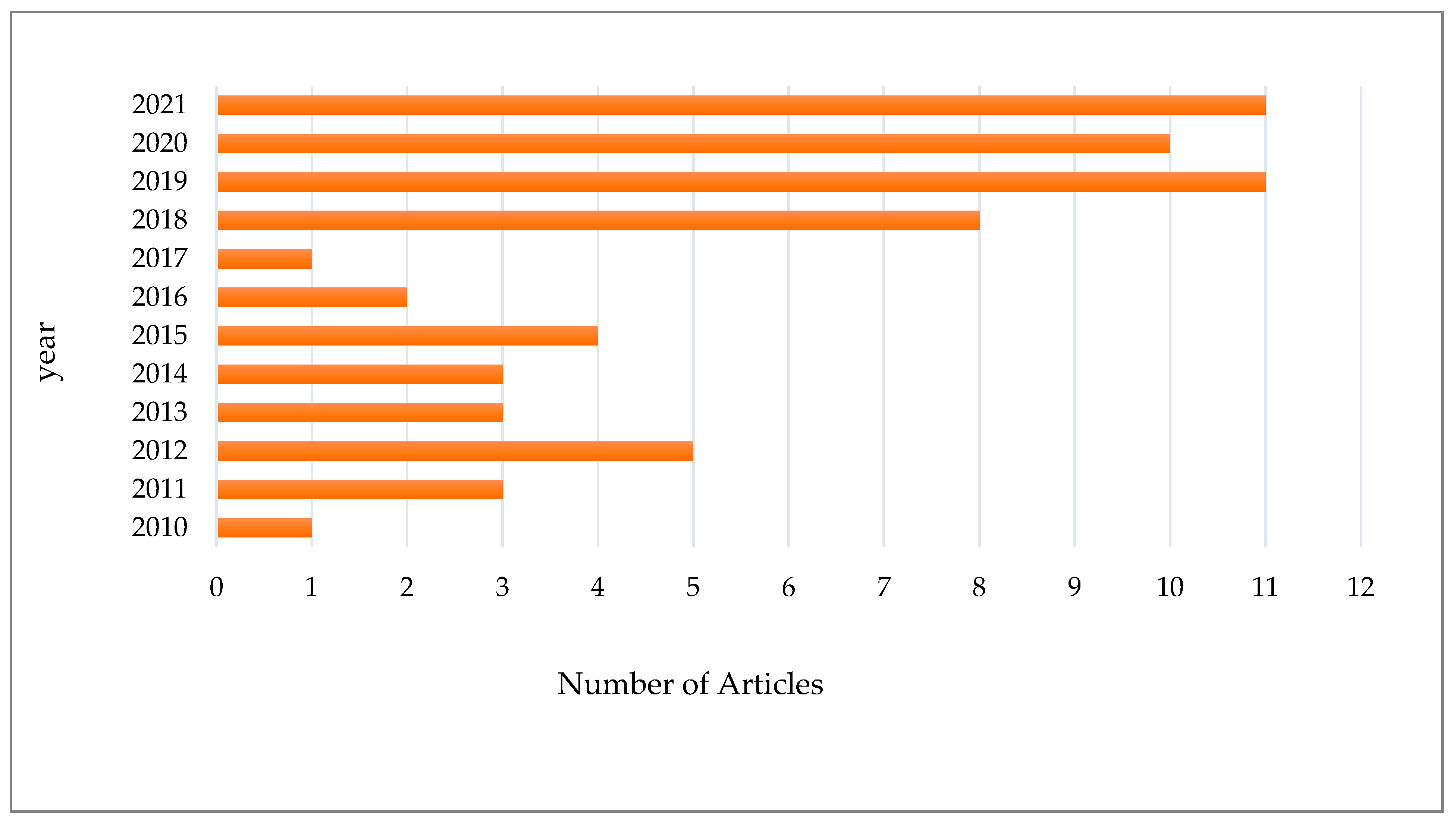
3.1. Preliminary Results Based on the Literature
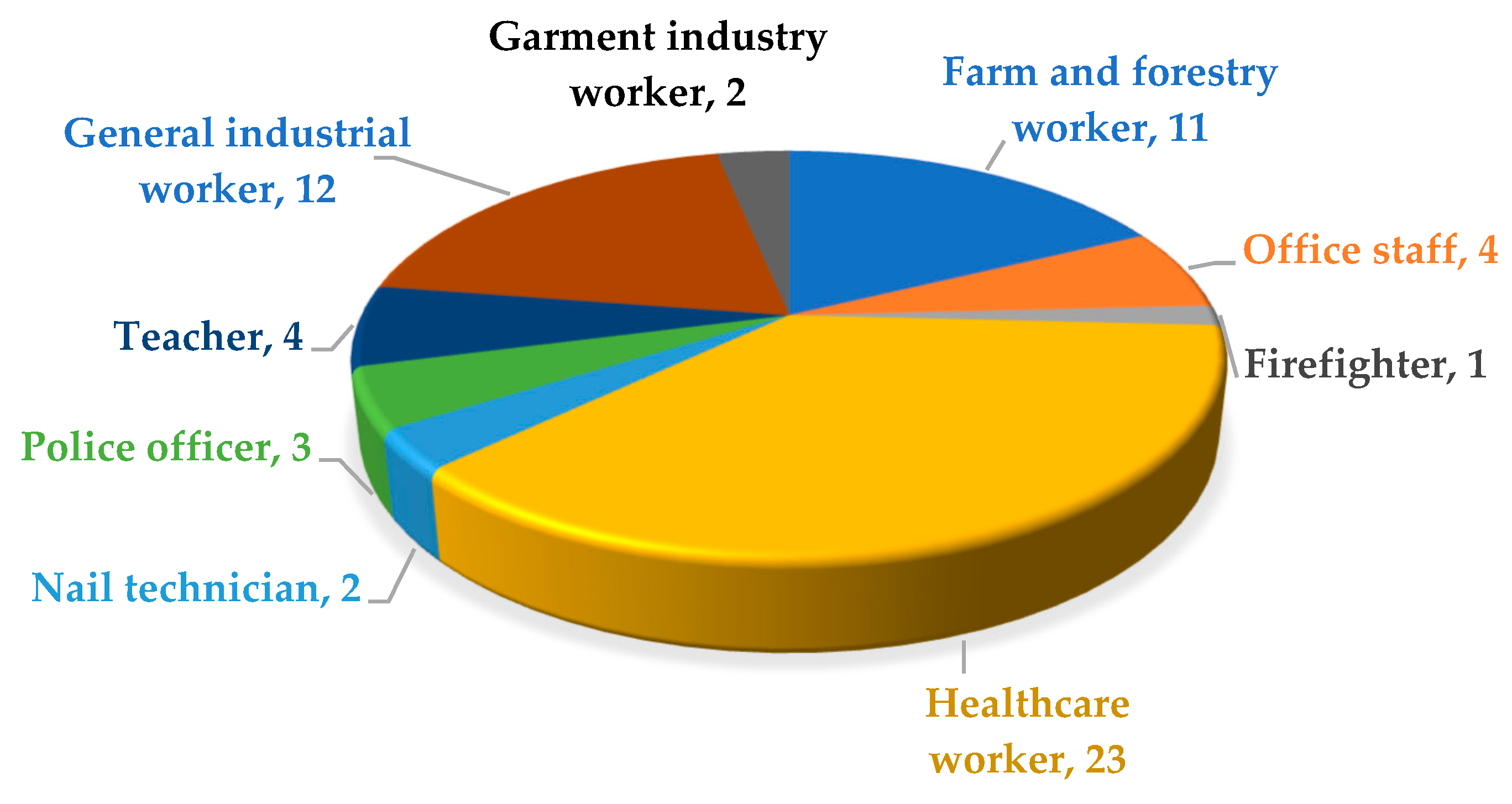
3.2. Results Related to Occupations in Specific Sectors as Found in the Literature
4. Discussion
4.1. OHS Challenges or Issues for Women in Specific Occupations Based on the Literature
4.1.1. OHS Challenges or Issues Faced by Female HCWs
- Female HCWs are at high risk of job stress and job burnout, both of which can lead to less effective nursing care and psychological problems (11 studies);
- Three studies conducted between 2010 and 2021 considered workplace violence as a factor affecting the health level of female HCWs. Overall, the results showed that female HCWs were exposed to varying degrees of verbal, organizational, sexual, and physical violence;
- Another factor affecting HCWs health is fatigue due to high workload, long hours of work, and stress. Among the studies conducted in the field of fatigue, two were found in this case;
- Sleep is an essential factor that plays an important role in health. Sleep, as a physiological mechanism of the body, can restore lost power and eliminate fatigue caused by activity. Sleep disturbances can lead to physical and mental problems and a decrease in performance. One case study related to the sleep health of women working in the healthcare sector showed the results of sleep disturbances in working women;
- Two studies investigated the use of PPE related to reduced employee health levels;
- HCWs are at risk of ischemic heart disease (one study).
4.1.2. OHS Challenges or Issues Faced by Female Farm and Forestry Workers
4.1.3. OHS Challenges or Issues Faced by Female Office Staff
4.1.4. OHS Challenges or Issues Faced by Female Firefighters
4.1.5. OHS Challenges or Issues Faced by Female Police Officers
4.1.6. OHS Challenges or Issues Faced by Female Teachers
4.1.7. OHS Challenges or Issues Faced by Female Nail Technicians
4.1.8. OHS Challenges or Issues Faced by Female Workers in the Clothing Industry
4.1.9. OHS Challenges or Issues Faced by Female General Industrial Workers
4.2. Strengths Impact, and Future Research Avenues
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Elsan, M. Citizenship Rights from the View Point of Iranian Law and Global Citizenship. Hum Rts. 2008, 3, 2. [Google Scholar]
- Hakimzade Khoei, P.; Rajabzadeh, A.; Sotode, S. Promoting the human rights status of women by emphasizing the Iranian legal system. Mod. Jurisprud. Law 2021, 2, 63–89. [Google Scholar]
- Flaspöler, E.; Hauke, A.; Koppisch, D.; Reinert, D.; Koukoulaki, T.; Vilkevicius, G.; Žemės, L.; Águila Martínez-Casariego, M.; Baquero Martínez, M.; González Lozar, L. New Risks and Trends in the Safety and Health of Women at Work. 2013. Available online: https://irep.ntu.ac.uk/id/eprint/31145/1/PubSub8694_Hassard.pdf (accessed on 14 August 2022).
- Ahmadi, B.; Tabibi, J.; Mahmoodi, M. Designing a model of administration structure for Iranian women’s health development. Soc. Welf. Q. 2006, 5, 9–38. [Google Scholar]
- World Health Organization. Health and Human Rights; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- World Health Organization. World Report on Knowledge for Better Health: Strengthening Health Systems; World Health Organization: Geneva, Switzerland, 2004. [Google Scholar]
- Kasle, S.; Wilhelm, M.S.; Reed, K.L. Optimal health and well-being for women: Definitions and strategies derived from focus groups of women. Women’s Health Issues 2002, 12, 178–190. [Google Scholar] [CrossRef] [PubMed]
- National Center for Health Statistics (US); National Center for Health Services Research. Health, United States; US Department of Health, Education, and Welfare, Public Health Service: Hyattsville, MD, USA, 2011.
- Somani, T. Importance of educating girls for the overall development of society: A global perspective. J. Educ. Res. Pract. 2017, 7, 10. [Google Scholar] [CrossRef]
- Davidson, P.M.; McGrath, S.J.; Meleis, A.I.; Stern, P.; DiGiacomo, M.; Dharmendra, T.; Correa-de-Araujo, R.; Campbell, J.C.; Hochleitner, M.; Messias, D.K.; et al. The health of women and girls determines the health and well-being of our modern world: A white paper from the International Council on Women’s Health Issues. Health Care Women Int. 2011, 32, 870–886. [Google Scholar] [CrossRef] [PubMed]
- Ahmadi, B.; Babashahy, S. Women health management: Policies, research, and services. Soc. Welf. Q. 2013, 12, 29–59. [Google Scholar]
- Abdullah, H.; Azam, M.; Zakariya, S.K. The impact of environmental quality on public health expenditure in Malaysia. Asia Pac. J. Adv. Bus. Soc. Stud. 2016, 2, 365–379. [Google Scholar]
- Oppenheimer, V.K. Women’s rising employment and the future of the family in industrial societies. Popul. Dev. Rev. 1994, 20, 293–342. [Google Scholar] [CrossRef]
- Jurczyk, K.; Jentsch, B.; Sailer, J.; Schier, M. Female-breadwinner families in Germany: New gender roles? J. Fam. Issues 2019, 40, 1731–1754. [Google Scholar] [CrossRef]
- Levy, B.S. Occupational and Environmental Health: Recognizing and Preventing Disease and Injury; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2006. [Google Scholar]
- Basu, A. Globalization of the local/localization of the global: Mapping transnational women’s movements. Meridians 2000, 1, 68–84. [Google Scholar] [CrossRef]
- London, L.; De Grosbois, S.; Wesseling, C.; Kisting, S.; Rother, H.A.; Mergler, D. Pesticide usage and health consequences for women in developing countries: Out of sight out of mind? Int. J. Occup. Environ. Health 2002, 8, 46–59. [Google Scholar] [CrossRef] [PubMed]
- Memon, Q.U.A.; Wagan, S.A.; Chunyu, D.; Shuangxi, X.; Jingdong, L.; Damalas, C.A. Health problems from pesticide exposure and personal protective measures among women cotton workers in southern Pakistan. Sci. Total Environ. 2019, 685, 659–666. [Google Scholar] [CrossRef] [PubMed]
- Garcia, A.M. Pesticide exposure and women’s health. Am. J. Ind. Med. 2003, 44, 584–594. [Google Scholar] [CrossRef]
- Sathish, V.; Prakash, Y. Sex differences in pulmonary anatomy and physiology: Implications for health and disease. Sex Differ. Physiol. 2016, 10, 89–103. [Google Scholar] [CrossRef]
- Tur, E. Physiology of the skin—Differences between women and men. Clin. Dermatol. 1997, 15, 5–16. [Google Scholar] [CrossRef] [PubMed]
- Legato, M.J.; Leghe, J.K. Gender and the heart: Sex-specific differences in the normal myocardial anatomy and physiology. Princ. Gend.-Specif. Med. 2010, 151–161. [Google Scholar] [CrossRef]
- Miller, A.E.J.; MacDougall, J.; Tarnopolsky, M.; Sale, D. Gender differences in strength and muscle fiber characteristics. Eur. J. Appl. Physiol. Occup. Physiol. 1993, 66, 254–262. [Google Scholar] [CrossRef]
- Nindl, B.C.; Jones, B.H.; Van Arsdale, S.J.; Kelly, K.; Kraemer, W.J. Operational physical performance and fitness in military women: Physiological, musculoskeletal injury, and optimized physical training considerations for successfully integrating women into combat-centric military occupations. Mil. Med. 2016, 181 (Suppl. S1), 50–62. [Google Scholar] [CrossRef] [PubMed]
- Lipscomb, H.J.; Dement, J.M.; Epling, C.A.; Gaynes, B.N.; McDonald, M.A.; Schoenfisch, A.L. Depressive symptoms among working women in rural North Carolina: A comparison of women in poultry processing and other low-wage jobs. Int. J. Law Psychiatry 2007, 30, 284–298. [Google Scholar] [CrossRef]
- Gallagher, C.M.; Chen, J.J.; Kovach, J.S. The relationship between body iron stores and blood and urine cadmium concentrations in US never-smoking, non-pregnant women aged 20–49 years. Environ. Res. 2011, 111, 702–707. [Google Scholar] [CrossRef] [PubMed]
- Soldin, O.P.; Mattison, D.R. Sex differences in pharmacokinetics and pharmacodynamics. Clin. Pharmacokinet. 2009, 48, 143–157. [Google Scholar] [CrossRef] [PubMed]
- Neugarten, J.; Golestaneh, L. Gender and the prevalence and progression of renal disease. Adv. Chronic Kidney Dis. 2013, 20, 390–395. [Google Scholar] [CrossRef] [PubMed]
- Earnest, G.S.; Flesch, J.P.; Hagedorn, R.T.; Hayden, C.S.; Watkins, D.S. Control of Exposure to Perchloroethylene in Commercial Drycleaning (Ventilation). 1997. Available online: https://stacks.cdc.gov/view/cdc/13416 (accessed on 19 August 2022).
- Wilson, R.T.; Donahue, M.; Gridley, G.; Adami, J.; Ghormli, L.E.; Dosemeci, M. Shared occupational risks for transitional cell cancer of the bladder and renal pelvis among men and women in Sweden. Am. J. Ind. Med. 2008, 51, 83–99. [Google Scholar] [CrossRef] [PubMed]
- Gardner, K.M.; Ou Shu, X.; Jin, F.; Dai, Q.; Ruan, Z.; Thompson, S.J.; Hussey, J.R.; Gao, Y.T.; Zheng, W. Occupations and breast cancer risk among Chinese women in urban Shanghai. Am. J. Ind. Med. 2002, 42, 296–308. [Google Scholar] [CrossRef] [PubMed]
- Langseth, H.; Andersen, A. Cancer incidence among women in the Norwegian pulp and paper industry. Am. J. Ind. Med. 1999, 36, 108–113. [Google Scholar] [CrossRef]
- Bulbulyan, M.A.; Ilychova, S.A.; Zahm, S.H.; Astashevsky, S.V.; Zaridze, D.G. Cancer mortality among women in the Russian printing industry. Am. J. Ind. Med. 1999, 36, 166–171. [Google Scholar] [CrossRef]
- Kaewdok, T.; Sirisawasd, S.; Taptagaporn, S. Agricultural risk factors related musculoskeletal disorders among older farmers in Pathum Thani Province, Thailand. J. Agromedicine 2021, 26, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Watkins, E.R.; Walker, A.; Mol, E.; Jahnke, S.; Richardson, A.J. Women firefighters’ health and well-being: An international survey. Women’s Health Issues 2019, 29, 424–431. [Google Scholar] [CrossRef]
- Van Dyck, L.; Baecke, M.; Grosjean, M.; Isaie, H.; Gregoire, Y.; Barbieux, C.; Tock, R.; Verbrugghe, M. Screening of work-related musculoskeletal upper limb disorders using the SALTSA protocol: A work-site study in Belgium. Workplace Health Saf. 2021, 69, 548–555. [Google Scholar] [CrossRef]
- Bryman, A. Social Research Methods; Oxford University Press: Oxford, UK, 2016. [Google Scholar]
- Creswell, J.W.; Creswell, J.D. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches; Sage Publications: Thousand Oaks, CA, USA, 2017. [Google Scholar]
- Hempel, S.; Xenakis, L.; Danz, M. Systematic Reviews for Occupational Safety and Health Questions: Resources for Evidence Synthesis. 2016. Available online: https://www.rand.org/content/dam/rand/pubs/research_reports/RR1400/RR1463/RAND_RR1463.pdf (accessed on 20 November 2022).
- The Joanna Briggs Institute. JBI Critical Appraisal Checklist for Qualitative Research 2017. Available online: https://jbi.global/sites/default/files/2019-05/JBI_Critical_Appraisal-Checklist_for_Qualitative_Research2017_0.pdf (accessed on 5 May 2023).
- Ramirez-Moreno, J.M.; Ceberino, D.; Plata, A.G.; Rebollo, B.; Sedas, P.M.; Hariramani, R.; Roa, A.M.; Constantino, A.B. Mask-associated ‘de novo’headache in healthcare workers during the COVID-19 pandemic. Occup. Environ. Med. 2021, 78, 548–554. [Google Scholar] [CrossRef] [PubMed]
- Abderhalden-Zellweger, A.; Probst, I.; Mercier, M.-P.P.; Danuser, B.; Krief, P. Protecting pregnancy at work: Normative safety measures and employees’ safety strategies in reconciling work and pregnancy. Saf. Sci. 2021, 142, 105387. [Google Scholar] [CrossRef]
- Paul, A.; Sultana, N.N.; Nazir, N.; Das, B.K.; Jabed, M.; Nath, T.K. Self-reported health problems of tobacco farmers in south-eastern Bangladesh. J. Public Health 2021, 29, 595–604. [Google Scholar] [CrossRef]
- Ahn, J.; Lee, S.H.; Park, M.Y.; Oh, S.H.; Lee, W. The Association Between Long Working Hours and Infertility. Saf. Health Work 2021, 12, 517–521. [Google Scholar] [CrossRef] [PubMed]
- Fattori, A.; Cantù, F.; Comotti, A.; Tombola, V.; Colombo, E.; Nava, C.; Bordini, L.; Riboldi, L.; Bonzini, M.; Brambilla, P. Hospital workers mental health during the COVID-19 pandemic: Methods of data collection and characteristics of study sample in a university hospital in Milan (Italy). BMC Med. Res. Methodol. 2021, 21, 163. [Google Scholar] [CrossRef] [PubMed]
- Faghihi, M.; Farshad, A.; Abhari, M.B.; Azadi, N.; Mansourian, M. The components of workplace violence against nurses from the perspective of women working in a hospital in Tehran: A qualitative study. BMC Women’s Health 2021, 21, 209. [Google Scholar] [CrossRef] [PubMed]
- Stelnicki, A.M.; Jamshidi, L.; Ricciardelli, R.; Carleton, R.N. Exposures to potentially psychologically traumatic events among nurses in Canada. Can. J. Nurs. Res. 2021, 53, 277–291. [Google Scholar] [CrossRef] [PubMed]
- Aiswarya, A.; Bhagya, D. Effect of COVID-19 lockdown on the lifestyle and dietary diversity of women handloom workers. Clin. Epidemiol. Glob. Health 2021, 12, 100856. [Google Scholar] [CrossRef]
- Uymaz, P.; Ozpinar, S. Exposure to occupational accidents and near miss events of the healthcare workers in a university hospital. ASEAN J. Psychiatry 2021, 22, 1. [Google Scholar]
- Dang, J.V.; Rosemberg, M.-A.S.; Le, A.B. Perceived work exposures and expressed intervention needs among Michigan nail salon workers. Int. Arch. Occup. Environ. Health 2021, 94, 2001–2013. [Google Scholar] [CrossRef]
- Poursadeqiyan, M.; Arefi, M.F.; Khaleghi, S.; Moghaddam, A.S.; Mazloumi, E.; Raei, M.; Hami, M.; Khammar, A. Investigation of the relationship between the safety climate and occupational fatigue among the nurses of educational hospitals in Zabol. J. Educ. Health Promot. 2020, 9, 238. [Google Scholar] [PubMed]
- Hong, C.Y.; Lee, C.G.; Kim, D.H.; Cho, Y.S.; Kim, K.Y.; Ryu, S.Y.; Song, H.S. Work-related risk factors of knee meniscal tears in Korean farmers: A cross-sectional study. Saf. Health Work 2020, 11, 485–490. [Google Scholar] [CrossRef] [PubMed]
- Bani-Issa, W.; Radwan, H.; Al Marzooq, F.; Al Awar, S.; Al-Shujairi, A.M.; Khasawneh, W.; Albluwi, N. Salivary cortisol, subjective stress and quality of sleep among female healthcare professionals. J. Multidiscip. Healthc. 2020, 13, 125. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Zhang, M.; Li, R.; Chen, N.; Huang, Y.; Lv, Y.; Wang, Y. Risk assessment of workplace violence towards health workers in a Chinese hospital: A cross-sectional study. BMJ Open 2020, 10, e042800. [Google Scholar] [CrossRef] [PubMed]
- Harthi, M.; Olayan, M.; Abugad, H.; Wahab, M.A. Workplace violence among health-care workers in emergency departments of public hospitals in Dammam, Saudi Arabia. East. Mediterr. Health J. 2020, 26, 1473–1481. [Google Scholar] [CrossRef] [PubMed]
- Carleton, R.N.; Ricciardelli, R.; Taillieu, T.; Mitchell, M.M.; Andres, E.; Afifi, T.O. Provincial correctional service workers: The prevalence of mental disorders. Int. J. Environ. Res. Public Health 2020, 17, 2203. [Google Scholar] [CrossRef] [PubMed]
- Chun, H.-r.; Cho, I.; Choi, Y.; Cho, S.-i. Effects of emotional labor factors and working environment on the risk of depression in pink-collar workers. Int. J. Environ. Res. Public Health 2020, 17, 5208. [Google Scholar] [CrossRef] [PubMed]
- Vilella, S.B.; Zarceño, E.L.; Serrano Rosa, M.A. Mood, Physical, and Mental Load in Spanish Teachers of Urban School: The role of intensive or split shift. Educ. Urban Soc. 2020, 52, 759–773. [Google Scholar] [CrossRef]
- Boström, M.; Björklund, C.; Bergström, G.; Nybergh, L.; Schäfer Elinder, L.; Stigmar, K.; Wåhlin, C.; Jensen, I.; Kwak, L. Health and work environment among female and male Swedish elementary school teachers—A cross-sectional study. Int. J. Environ. Res. Public Health 2020, 17, 227. [Google Scholar] [CrossRef]
- Lagrosen, Y.; Lagrosen, S. Gender, quality and health–a study of Swedish secondary school teachers. Int. J. Workplace Health Manag. 2020, 13, 223–238. [Google Scholar] [CrossRef]
- Lee, S.; Lee, K.; Lee, S.-J. Hearing impairment among Korean farmers, based on a 3-year audiometry examination. Ann. Agric. Environ. Med. 2019, 26, 148–153. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.C.; Hartley, T.A.; Sarkisian, K.; Fekedulegn, D.; Mnatsakanova, A.; Owens, S.; Gu, J.K.; Tinney-Zara, C.; Violanti, J.M.; Andrew, M.E. Influence of work characteristics on the association between police stress and sleep quality. Saf. Health Work 2019, 10, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Villar, R.; Serra, L.; Serra, C.; Benavides, F.G. Working conditions and absence from work during pregnancy in a cohort of healthcare workers. Occup. Environ. Med. 2019, 76, 236–242. [Google Scholar] [CrossRef] [PubMed]
- Rocha, L.J.; Cortes, M.d.C.J.W.; Dias, E.C.; de Meira Fernandes, F.; Gontijo, E.D. Burnout and job satisfaction among emergency and intensive care providers in a public hospital. Rev. Bras. Med. Trab. 2019, 17, 300. [Google Scholar] [CrossRef] [PubMed]
- Gander, P.; O’Keeffe, K.; Santos-Fernandez, E.; Huntington, A.; Walker, L.; Willis, J. Fatigue and nurses’ work patterns: An online questionnaire survey. Int. J. Nurs. Stud. 2019, 98, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Gu, B.; Tan, Q.; Zhao, S. The association between occupational stress and psychosomatic wellbeing among Chinese nurses: A cross-sectional survey. Medicine 2019, 98, e15836. [Google Scholar] [CrossRef] [PubMed]
- Seo, J.Y.; Chao, Y.-Y.; Strauss, S.M. Work-related symptoms, safety concerns, and health service utilization among Korean and Chinese nail salon workers in the greater New York City Area. Asia Pac. J. Public Health 2019, 31, 199–209. [Google Scholar] [CrossRef] [PubMed]
- Akhter, S.; Rutherford, S.; Chu, C. Sufferings in silence: Violence against female workers in the ready-made garment industry in Bangladesh: A qualitative exploration. Women’s Health 2019, 15, 1745506519891302. [Google Scholar] [CrossRef] [PubMed]
- Ahn, J.; Kim, N.-S.; Lee, B.-K.; Park, J.; Kim, Y. Relationship of occupational category with risk of physical and mental health problems. Saf. Health Work 2019, 10, 504–511. [Google Scholar] [CrossRef]
- Kongtip, P.; Nankongnab, N.; Mahaboonpeeti, R.; Bootsikeaw, S.; Batsungnoen, K.; Hanchenlaksh, C.; Tipayamongkholgul, M.; Woskie, S. Differences among Thai agricultural workers’ health, working conditions, and pesticide use by farm type. Ann. Work Expo. Health 2018, 62, 167–181. [Google Scholar] [CrossRef]
- Park, J.; Kim, Y.; Han, B. Work sectors with high risk for work-related musculoskeletal disorders in Korean men and women. Saf. Health Work 2018, 9, 75–78. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, A.d.; Silva, M.T.; Galvão, T.F.; Lopes, L.C. The relationship between job satisfaction, burnout syndrome and depressive symptoms: An analysis of professionals in a teaching hospital in Brazil. Medicine 2018, 97, e13364. [Google Scholar] [CrossRef] [PubMed]
- Stuetzle, K.V.; Pavlin, B.; Smith, N.A.; Weston, K.M. Survey of occupational fatigue in anaesthetists in Australia and New Zealand. Anaesth. Intensive Care 2018, 46, 414–423. [Google Scholar] [CrossRef] [PubMed]
- Azimi, H.; Majd Teimouri, Z.; Mousavi, S.; Kazem Nezhad Leyli, E.; Jafaraghaee, F. Individual protection adopted by ICU nurses against radiation and its related factors. J. Holist. Nurs. Midwifery 2018, 28, 18–25. [Google Scholar]
- Starc, J. Stress factors among nurses at the primary and secondary level of public sector health care: The case of Slovenia. Open Access Maced. J. Med. Sci. 2018, 6, 416. [Google Scholar] [CrossRef] [PubMed]
- Tei-Tominaga, M.; Nakanishi, M. The influence of supportive and ethical work environments on work-related accidents, injuries, and serious psychological distress among hospital nurses. Int. J. Environ. Res. Public Health 2018, 15, 240. [Google Scholar] [CrossRef]
- Cherry, N.; Arrandale, V.; Beach, J.; Galarneau, J.-M.F.; Mannette, A.; Rodgers, L. Health and work in women and men in the welding and electrical trades: How do they differ? Ann. Work Expo. Health 2018, 62, 393–403. [Google Scholar] [CrossRef]
- Sunindijo, R.Y.; Kamardeen, I. Work stress is a threat to gender diversity in the construction industry. J. Constr. Eng. Manag. 2017, 143, 04017073. [Google Scholar] [CrossRef]
- Kim, H.; Räsänen, K.; Chae, H.; Kim, K.; Kim, K.; Lee, K. Farm work–related injuries and risk factors in South Korean agriculture. J. Agromed. 2016, 21, 345–352. [Google Scholar] [CrossRef]
- Chen, C.H.; Wang, J.; Yang, C.S.; Fan, J.Y. Nurse practitioner job content and stress effects on anxiety and depressive symptoms, and self-perceived health status. J. Nurs. Manag. 2016, 24, 695–704. [Google Scholar] [CrossRef]
- Honda, A.; Abe, Y.; Date, Y.; Honda, S. The impact of multiple roles on psychological distress among Japanese workers. Saf. Health Work 2015, 6, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Castro, M.; Carvalhais, J.; Teles, J. Irregular working hours and fatigue of cabin crew. Work 2015, 51, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Botha, D.; Cronjé, F. Occupational health and safety considerations for women employed in core mining positions. SA J. Hum. Resour. Manag. 2015, 13, 1–12. [Google Scholar] [CrossRef]
- Allesøe, K.; Holtermann, A.; Aadahl, M.; Thomsen, J.F.; Hundrup, Y.A.; Søgaard, K. High occupational physical activity and risk of ischaemic heart disease in women: The interplay with physical activity during leisure time. Eur. J. Prev. Cardiol. 2015, 22, 1601–1608. [Google Scholar] [CrossRef] [PubMed]
- Alexopoulos, E.C.; Palatsidi, V.; Tigani, X.; Darviri, C. Exploring stress levels, job satisfaction, and quality of life in a sample of police officers in Greece. Saf. Health Work 2014, 5, 210–215. [Google Scholar] [CrossRef] [PubMed]
- Turk, M.; Davas, A.; Tanik, F.A.; Montgomery, A.J. Organizational stressors, work–family interface and the role of gender in the hospital: E xperiences from T urkey. Br. J. Health Psychol. 2014, 19, 442–458. [Google Scholar] [CrossRef]
- Honda, A.; Date, Y.; Abe, Y.; Aoyagi, K.; Honda, S. Work-related stress, caregiver role, and depressive symptoms among Japanese workers. Saf. Health Work 2014, 5, 7–12. [Google Scholar] [CrossRef]
- Tatsuse, T.; Sekine, M. Job dissatisfaction as a contributor to stress-related mental health problems among Japanese civil servants. Ind. Health 2013, 51, 307–318. [Google Scholar] [CrossRef]
- Artazcoz, L.; Cortès, I.; Escribà-Agüir, V.; Bartoll, X.; Basart, H.; Borrell, C. Long working hours and health status among employees in Europe: Between-country differences. Scand. J. Work Environ. Health 2013, 39, 369–378. [Google Scholar] [CrossRef]
- Berecki-Gisolf, J.; Tawatsupa, B.; McClure, R.; Seubsman, S.-A.; Sleigh, A. Determinants of workplace injury among Thai Cohort Study participants. BMJ Open 2013, 3, e003079. [Google Scholar] [CrossRef]
- Kheiraoui, F.; Gualano, M.R.; Mannocci, A.; Boccia, A.; La Torre, G. Quality of life among healthcare workers: A multicentre cross-sectional study in Italy. Public Health 2012, 126, 624–629. [Google Scholar] [CrossRef] [PubMed]
- Van Houtte, E.; Claeys, S.; Wuyts, F.; Van Lierde, K. Voice disorders in teachers: Occupational risk factors and psycho-emotional factors. Logop. Phoniatr. Vocol. 2012, 37, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Lederer, V.; Rivard, M.; Mechakra-Tahiri, S.D. Gender differences in personal and work-related determinants of return-to-work following long-term disability: A 5-year cohort study. J. Occup. Rehabil. 2012, 22, 522–531. [Google Scholar] [CrossRef] [PubMed]
- Herrero, S.G.; Saldaña, M.Á.M.; Rodriguez, J.G.; Ritzel, D.O. Influence of task demands on occupational stress: Gender differences. J. Saf. Res. 2012, 43, 365–374. [Google Scholar] [CrossRef] [PubMed]
- Wirtz, A.; Lombardi, D.A.; Willetts, J.L.; Folkard, S.; Christiani, D.C. Gender differences in the effect of weekly working hours on occupational injury risk in the United States working population. Scand. J. Work Environ. Health 2012, 38, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Blanco-Muñoz, J.; Lacasaña, M. Practices in pesticide handling and the use of personal protective equipment in Mexican agricultural workers. J. Agromed. 2011, 16, 117–126. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Zhao, W.; Jing, R.; Wheeler, K.; Smith, G.A.; Stallones, L.; Xiang, H. Work-related pesticide poisoning among farmers in two villages of Southern China: A cross-sectional survey. BMC Public Health 2011, 11, 429. [Google Scholar] [CrossRef]
- Özden, S.; Nayir, I.; Göl, C.; Ediş, S.; Yilmaz, H. Health problems and conditions of the forestry workers in Turkey. Afr. J. Agric. Res. 2011, 6, 5884–5890. [Google Scholar]
- Naidoo, S.; London, L.; Rother, H.-A.; Burdorf, A.; Naidoo, R.; Kromhout, H. Pesticide safety training and practices in women working in small-scale agriculture in South Africa. Occup. Environ. Med. 2010, 67, 823–828. [Google Scholar] [CrossRef]
- World Health Organization. Multilevel Course on the Safe Use of Pesticides and on the Diagnosis and Treatment of Pesticide Poisoning; World Health Organization: Geneva, Switzerland, 1994. [Google Scholar]
- Abdollahpour, I. Quality of life and effective factors on it among governmental staff in Boukan city. Stud. Med. Sci. 2011, 22, 40–47. [Google Scholar]
- Rezaei, E.; Moghadam, Z.B.; Saraylu, K. Quality of life in pregnant women with sleep disorder. J. Fam. Reprod. Health 2013, 7, 87. [Google Scholar]
- Pien, G.W.; Schwab, R.J. Sleep disorders during pregnancy. Sleep 2004, 27, 1405–1417. [Google Scholar] [CrossRef] [PubMed]
- Bolghanabadi, S.; Mousavi Kordmiri, S.; Mahmodi, A.; Mehdiabadi, S. The effect of mental workload on stress and Quality of Work Life firefighters. J. Sabzevar Univ. Med. Sci. 2019, 26, 547–553. [Google Scholar]
- Konopko, M.; Jarosz, W.; Bienkowski, P.; Sienkiewicz-Jarosz, H. Work-related factors and depressive symptoms in firefighters-preliminary data. In MATEC Web of Conferences; EDP Sciences: Les Ulis, France, 2018; p. 00065. [Google Scholar]
- Quach, T.; Nguyen, K.-D.; Doan-Billings, P.-A.; Okahara, L.; Fan, C.; Reynolds, P. A preliminary survey of Vietnamese nail salon workers in Alameda County, California. J. Community Health 2008, 33, 336–343. [Google Scholar] [CrossRef] [PubMed]
- Ulrich, C.M.; Taylor, C.; Soeken, K.; O’Donnell, P.; Farrar, A.; Danis, M.; Grady, C. Everyday ethics: Ethical issues and stress in nursing practice. J. Adv. Nurs. 2010, 66, 2510–2519. [Google Scholar] [CrossRef] [PubMed]
- Haahr, A.; Norlyk, A.; Martinsen, B.; Dreyer, P. Nurses experiences of ethical dilemmas: A review. Nurs. Ethics 2020, 27, 258–272. [Google Scholar] [CrossRef] [PubMed]
- Roy, B.; Kumar, A.; Kumar, A.; Gowda, K.R. Ethical conflicts among the leading medical and healthcare leaders. Asia Pac. J. Health Manag. 2022, 17, 165–172. [Google Scholar] [CrossRef]
- Zakaria, A.M.; Sleem, W.F.; Seada, A.M. Effectiveness of ethical issues teaching program on knowledge, ethical behavior and ethical stress among nurses. J. Nurs. Educ. Pract. 2016, 6, 125–134. [Google Scholar] [CrossRef]
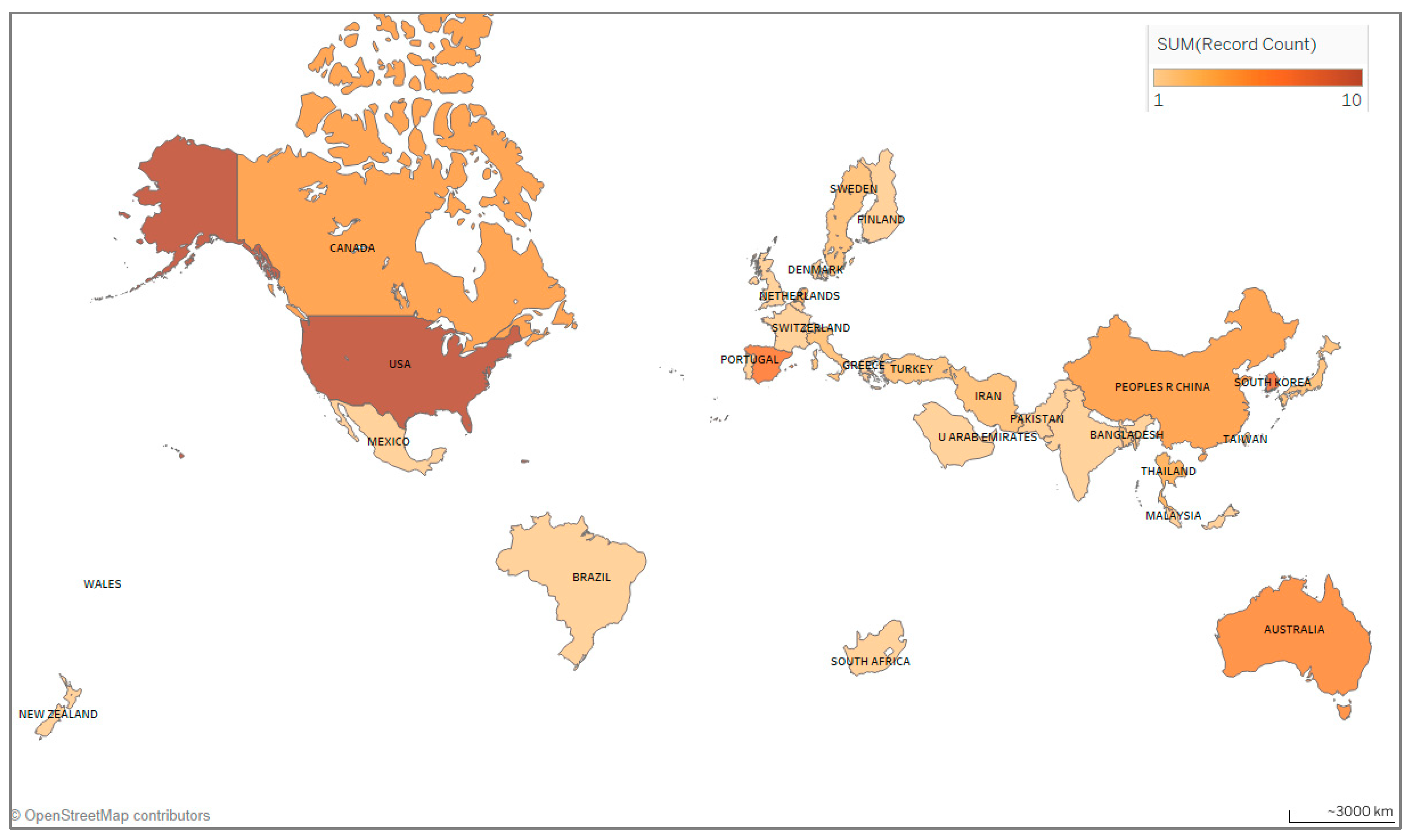

| Country | Documents | Citations | Average Number of Citations per Document | Total Link Strength * |
|---|---|---|---|---|
| USA | 10 | 290 | 29 | 6 |
| South Korea | 7 | 64 | 9.1 | 0 |
| Spain | 6 | 168 | 28 | 1 |
| Australia | 5 | 129 | 25.8 | 4 |
| Canada | 4 | 95 | 23.7 | 1 |
| China | 4 | 184 | 46 | 1 |
| Netherlands | 3 | 66 | 22 | 3 |
| Thailand | 3 | 52 | 17.3 | 2 |
| Bangladesh | 2 | 10 | 5 | 2 |
| Iran | 2 | 28 | 14 | 0 |
| Journals | Documents | Citations | Impact Factor | Total Link Strength * |
|---|---|---|---|---|
| Safety and Health at Work | 5 | 59 | 3.5 | 10 |
| International Journal of Environmental Research and Public Health | 4 | 84 | - | 28 |
| Journal of Agromedicine | 3 | 68 | 2.4 | 5 |
| Occupational and Environmental Medicine | 3 | 86 | 4.9 | 5 |
| Annals of Work Exposures and Health | 2 | 49 | 2.6 | 4 |
| BMJ Open | 2 | 18 | 2.9 | 5 |
| Medicine | 2 | 76 | 1.6 | 9 |
| Scandinavian Journal of Work Environment & Health | 2 | 62 | 6.3 | 8 |
| African Journal of Agricultural Research | 1 | 13 | - | 0 |
| Anesthesia and Intensive Care | 1 | 9 | - | 3 |
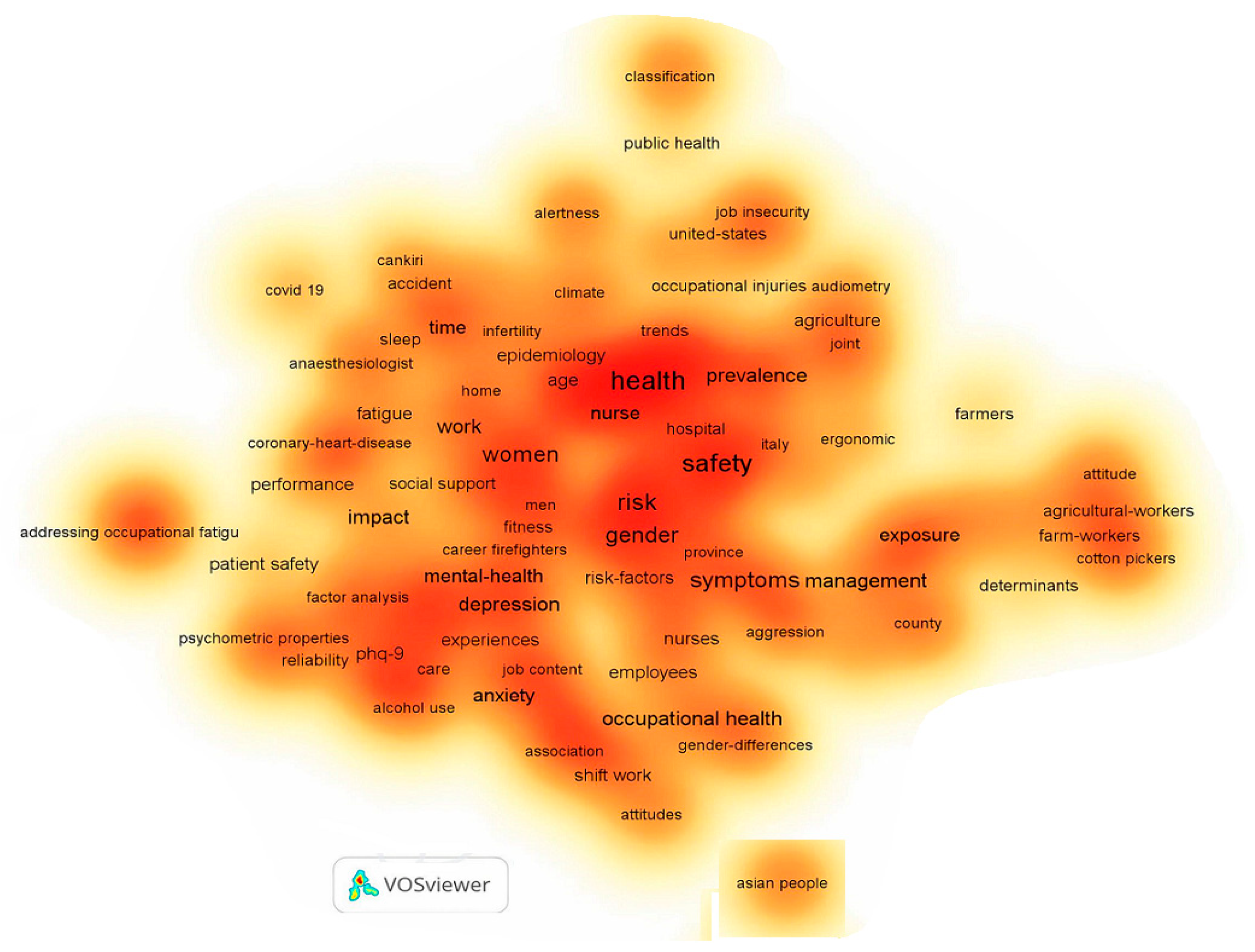
| Keyword | Occurrence | Total Link Strength * |
|---|---|---|
| Health | 14 | 31 |
| Safety | 13 | 30 |
| Stress | 11 | 26 |
| Gender | 11 | 17 |
| Women | 8 | 20 |
| Symptoms | 8 | 16 |
| Burnout | 8 | 15 |
| Management | 6 | 15 |
| Prevalence | 6 | 12 |
| Depression | 6 | 12 |
| Row | Author | Year | Occupation | Type of Study | Target of the Study | Number of Women Investigated |
|---|---|---|---|---|---|---|
| 1 | Teeraphun Kaewdok [34] | 2021 | Farm and forestry workers | Cross-Sectional | Risk identification of MSDs among farmers | 284 |
| 2 | Ramirez-Moreno [41] | 2021 | Healthcare workers | Cross-Sectional | Possible effects of the mask on new headaches during the COVID-19 pandemic | 244 |
| 3 | Alessia Abderhalden-Zellweger [42] | 2021 | Office staff | Qualitative | Maternity support at work, work-match strategies, and pregnancy | 202 |
| 4 | Alak Paul [43] | 2021 | Farm and forestry workers | NIP * | Tobacco’s effect on farm workers’ health | 48 |
| 5 | J Ahn [44] | 2021 | General industrial workers | Cross-Sectional | Study on the effect of long working hours with infertility | 5909 |
| 6 | Fattori A [45] | 2021 | Healthcare workers | Observational | Systematic study of mental health in health workers | 353 |
| 7 | M Faghihi [46] | 2021 | Healthcare workers | Qualitative | Explaining the components of workplace violence against nurses from the perspective of working women in hospital | 21 |
| 8 | AM Stelnicki [47] | 2021 | Healthcare workers | NIP | Prevalence of mental disorders among nurses | 4067 |
| 9 | A Aiswarya [48] | 2021 | Garment industry workers | Cross-Sectional | Identification of occupational health problems, assessment of nutrition specifications and anthropometric changes, comparison of sleeping hours of working women, and evaluation of job stress levels before and during COVID-19 quarantine in female weavers | 100 |
| 10 | Uymaz Pelin [49] | 2021 | Healthcare workers | Descriptive | Frequency of exposure to occupational accidents | 83 |
| 11 | Jenny V. Dang [50] | 2021 | Nail technicians | Qualitative | Assessing and promoting nail technicians’ health | 23 |
| 12 | Poursadeqiyan Mohsen [51] | 2020 | Healthcare workers | Cross-Sectional | Determining the relationship between safety climate and nurses’ job fatigue | 82 |
| 13 | Chae Young Hong [52] | 2020 | Farm and forestry workers | Cross-Sectional | Relationship between meniscus tear and occupational risk factors in the agricultural profession | 248 |
| 14 | Bani-Issa Wegdan [53] | 2020 | Healthcare workers | Cross-Sectional | Stress assessment among healthcare workers (HCWs) using cortisol level measurements, mental stress, and sleep quality | 335 |
| 15 | Liu Yujie [54] | 2020 | Healthcare workers | Cross-Sectional | Evaluation of risk factors related to violence in the workplace | 847 |
| 16 | Harthi Moussa [55] | 2020 | Healthcare workers | Cross-Sectional | Estimating prevalence and potential factors associated with workplace violence | 215 |
| 17 | RN Carleton [56] | 2020 | Police officers | Cross-Sectional | Review of mental disorders | 451 |
| 18 | H Chun [57] | 2020 | General industrial workers | Cross-Sectional | Investigating the critical factors of mental problems and the occurrence of depression | 5173 |
| 19 | SB Vilella [58] | 2020 | Teachers | Descriptive | Job satisfaction levels, fatigue, and burnout in teachers | 102 |
| 20 | M Boström [59] | 2020 | Teachers | Cross-Sectional | Describing how teachers experience health in the workplace, the social and safety climate, and socio-psychological health at work | 387 |
| 21 | Y Lagrosen [60] | 2020 | Teachers | NIP | Review of gender differences in the field of quality management experience and workplace health | 183 |
| 22 | Sujin Lee [61] | 2019 | Farm and forestry workers | NIP | Evaluation of hearing disorders in farmers | 1121 |
| 23 | Memon Qurat Ul Ain [18] | 2019 | Farm and forestry workers | NIP | Study of the problem related to the health of harvest workers in the face of pesticides and the necessity of using PPE | 260 |
| 24 | Watkins Emily R [35] | 2019 | Firefighters | NIP | Identification of female fire fighters’ health problems | 840 |
| 25 | Claudia C.Ma [62] | 2019 | Police officers | NIP | Analysis of the relationship between stress, sleep quality, and incidence of occupational accidents | 100 |
| 26 | Villar Rocio [63] | 2019 | Healthcare workers | Cohort | Investigating the relationship between workplace risk factors during pregnancy and absence from work | 428 |
| 27 | Rocha Luiz Junior [64] | 2019 | Healthcare workers | Cross-Sectional | Identifying factors related to the prevalence of burnout and job satisfaction among emergency personnel and special care staff | 33 |
| 28 | Gander Philippa [65] | 2019 | Healthcare workers | NIP | Investigating the increase in risk and fatigue of nurses | 2813 |
| 29 | Gu Bo [66] | 2019 | Healthcare workers | Cross-Sectional | The relationship between job stress and cognitive symptoms of nurses | 2795 |
| 30 | Jin Young Seo [67] | 2019 | Nail technicians | Cross-Sectional | Determining the similarities and differences in health effects, safety concerns, and the use of health services among immigrant women | 148 |
| 31 | Akhter Sadika [68] | 2019 | Garment industry workers | NIP | Study of violence and social norms in garment workers | 56 |
| 32 | J Ahn [69] | 2019 | General industrial workers | Cross-Sectional | Assessment of physical and mental health problems of workers | 11,023 |
| 33 | Pornpimol Kongtip [70] | 2018 | Farm and forestry workers | Cross-Sectional | Comparison of population statistics, working conditions, health of individuals, and the health behaviors in different agricultural workers | 255 |
| 34 | Park Jungsun [71] | 2018 | Office staff | NIP | Identification of work-related MSDs | 2248 |
| 35 | Oliveira AM de [72] | 2018 | Healthcare workers | Cross-Sectional | Investigating the relationship between individual and occupational aspects of hospital staff with job satisfaction, burnout, and depressive symptoms | 213 |
| 36 | Karien Stuetzle [73] | 2018 | Healthcare workers | NIP | Determining sources and effects of job fatigue | 115 |
| 37 | Azimi Hanifeh [74] | 2018 | Healthcare workers | Cross-Sectional | Determining the status of intensive care unit (ICU) nurses’ protection against radiation | 91 |
| 38 | Starc Jasmina [75] | 2018 | Healthcare workers | Descriptive | Determining the leading causes of stress and investigating the symptoms of stress among health care professionals at the primary and secondary level of health care | 318 |
| 39 | Tei-Tominaga Maki [76] | 2018 | Healthcare workers | Cross-Sectional | Studying the influence of supportive environments on occupational accidents, injury, and mental disorders | 822 |
| 40 | N Cherry [77] | 2018 | General industrial workers | Cohort | Difference between work type and health level in welding and electrical professionals | 447 |
| 41 | Sunindijo Riza Yosia [78] | 2017 | General industrial workers | NIP | Examining stress and factors influencing the conditions of stress in construction workers | 110 |
| 42 | Hyocher Kim [79] | 2016 | Farm and forestry workers | NIP | Identifying related agricultural job injuries and assessing the relationship between injury and possible risk factors | 7658 |
| 43 | Chen Chin-Huang [80] | 2016 | Healthcare workers | Cross-Sectional | Study on the effect of job satisfaction and stress on anxiety, depression symptoms, and perceived health status | 159 |
| 44 | A Honda [81] | 2015 | General industrial workers | NIP | Study on the impact of factors affecting the psychological issues of workers | 366 |
| 45 | Castro Marta [82] | 2015 | General industrial workers | NIP | Investigating the factors affecting the fatigue of airplane cabin crew | 39 |
| 46 | D Botha [83] | 2015 | General industrial workers | Descriptive | Investigating the health, safety, and hygiene of women working in mines | 290 |
| 47 | Allesøe Karen [84] | 2015 | Healthcare workers | Cohort | Physical activity in the workplace and ischemic heart disease | 12,093 |
| 48 | Evangelos C. Alexopoulo [85] | 2014 | Police officers | Cross-Sectional | Stress perception, job satisfaction, and the relationship between the two | 45 |
| 49 | Turk Meral [86] | 2014 | Healthcare workers | NIP | Relationship between organizational culture, burnout, and the quality of care in hospital | 36 |
| 50 | A Honda [87] | 2014 | Healthcare workers | NIP | Investigation of stress and mental health of elderly caregivers | 367 |
| 51 | Takashi TATSUSE [88] | 2013 | Office staff | NIP | Studying the relationship between job satisfaction and health problems related to stress | 570 |
| 52 | Artazcoz Lucía [89] | 2013 | Office staff | NIP | Studying the relationship between long working hours and family responsibilities | 6295 |
| 53 | J Berecki-Gisolf [90] | 2013 | General industrial workers | Cohort | Exploring factors determining workplace injury among workers | 28,428 |
| 54 | Kheiraoui F [91] | 2012 | Healthcare workers | Cross-Sectional | Assessing HCWs’ quality of life | 185 |
| 55 | E Van Houtte [92] | 2012 | Teachers | NIP | Assessment of risk factors and identification of new risk factors in teachers | 670 |
| 56 | Lederer Valérie [93] | 2012 | General industrial workers | Cohort | Assessing the impact of individual and psychological factors related to work and the effective physical and organizational factors after long-term disability | 169 |
| 57 | SG Herrero [94] | 2012 | General industrial workers | NIP | Analysis of gender differences in perceived stress | 5137 |
| 58 | A Wirtz [95] | 2012 | General industrial workers | Cross-Sectional | Investigating gender differences in the impact of long weekly working hours on occupational risk and injury | 48,099 |
| 59 | Julia Blanco-Muñoz [96] | 2011 | Farm and forestry workers | Case-Control | Description of the risk perceptions and methods related to the use of PPE | 35 |
| 60 | Xujun Zhang [97] | 2011 | Farm and forestry workers | Cross-Sectional | The study of prevalence and risk factors of acute poisoning with work-related pesticides among farmers | 351 |
| 61 | Sezgin Ouml Zden [98] | 2011 | Farm and forestry workers | NIP | Identification of the working conditions and attitudes of seasonal forestry workers regarding accidents and work safety | 47 |
| 62 | Saloshni Naidoo [99] | 2010 | Farm and forestry workers | Cross-Sectional | Investigation of training and safety practices when mixing and spraying pesticides, and levels of acetylcholinesterase among farmers | 803 |
| Specific Occupations | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| HCWs | Farm and Forestry Workers | Office Staff | Teachers | Firefighters | Police Officers | Nail Technicians | Workers in the Clothing Industry | General Industrial Workers | ||
| OHS challenges or issues | Auditory and respiratory disorders | ✓ | ✓ | |||||||
| Allergies and skin problems | ✓ | ✓ | ✓ | |||||||
| Conjunctivitis | ✓ | |||||||||
| Cuts | ✓ | |||||||||
| Depression and Anxiety | ✓ | ✓ | ✓ | |||||||
| Digestive problems | ✓ | |||||||||
| Educational interventions | ✓ | |||||||||
| Fatigue | ✓ | ✓ | ✓ | ✓ | ||||||
| Gender-specific factors (e.g., menstrual health) | ✓ | |||||||||
| High workload | ✓ | |||||||||
| Toxic chemicals and Inhalation of fumes | ✓ | |||||||||
| Ischemic heart disease | ✓ | |||||||||
| Job satisfaction | ✓ | ✓ | ||||||||
| Job stress and job burnout | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
| Lack of sports facilities | ✓ | |||||||||
| Long working hours | ✓ | ✓ | ✓ | |||||||
| MSDs and pain | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Poisoning with pesticides | ✓ | |||||||||
| Poor working conditions | ✓ | ✓ | ||||||||
| Pregnancy considerations | ✓ | |||||||||
| Rehabilitation challenges | ✓ | |||||||||
| Slip, trips, and falls | ✓ | |||||||||
| Sleep | ✓ | ✓ | ✓ | ✓ | ||||||
| Strength and conditioning support | ✓ | |||||||||
| Ability to meet job needs | ✓ | |||||||||
| Use of PPE | ✓ | ✓ | ||||||||
| Voice disorder | ✓ | |||||||||
| Workplace violence | ✓ | ✓ | ✓ | |||||||
| Issues or Challenges | Author | A Summary of Studies |
|---|---|---|
| Job stress and job burnout | Rocha et al. [64] |
|
| Turk et al. [86] |
| |
| Starc [75] |
| |
| Fattori et al. [45] |
| |
| Oliveira et al. [72] |
| |
| Chen et al. [80] |
| |
| Tominaga [76] |
| |
| Honda et al. [87] |
| |
| Stelnicki et al. [47] |
| |
| Gu et al. [66] |
| |
| Bani-Issa et al. [53] |
| |
| Workplace violence | Liu et al. [54] |
|
| Harthi et al. [55] |
| |
| Faghihi et al. [46] |
| |
| Fatigue | Poursadeqiyan et al. [51] |
|
| Stuetzle et al. [73] |
| |
| Sleep | Gander et al. [65] |
|
| The use of PPE | Ramirez-Moreno et al. [41] |
|
| Azimi et al. [74] |
| |
| Ischemic heart disease | Allesøe et al. [84] |
|
| Issues or Challenges | Author | A Summary of Studies |
|---|---|---|
| Poisoning with pesticides | Blanco et al. [96] |
|
| Naidoo et al. [99] |
| |
| Zhang et al. [97] |
| |
| Kongtip et al. [70] |
| |
| MSDs | Kaewdok et al. [34] |
|
| Hong [52] |
| |
| Sezgin et al. [98] |
| |
| Auditory and respiratory disorders | Lee et al. [61] |
|
| Sezgin et al. [98] |
| |
| Others (e.g., slips, trips, and falls, PPE and cut) | Kongtip et al. [70] |
|
| Sezgin et al. [98] |
| |
| Memon et al. [18] |
| |
| Kim et al. [79] |
| |
| Paul et al. [43] |
|
| Issues or Challenges | Author | A Summary of Studies |
|---|---|---|
| Stress, fatigue, and sleep | Tatsuse and Sekine [88] |
|
| Pregnancy considerations | Abderhalden-Zellweger et al. [42] |
|
| Long working hours | Artazcoz et al. [89] |
|
| MSDs | Park et al. [71] |
|
| Issues or Challenges | Author | A Summary of Studies |
|---|---|---|
| Fatigue and job satisfaction | Vilella et al. [58] |
|
| Boström et al. [59] |
| |
| Workplace violence | Lagrosen et al. [60] |
|
| Voice disorder | Van Houtte et al. [92] |
|
| Industries/Units | Author | A Summary of Studies |
|---|---|---|
| Mining | Botha and Cronjé [83] |
|
| Construction | Sunindijo and Kamardeen [78] |
|
| Air transportation | Castro et al. [82] |
|
| Welding and electrical units | Cherry et al. [77] |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bolghanabadi, S.; Haghighi, A.; Jahangiri, M. Insights into Women’s Occupational Health and Safety: A Decade in Review of Primary Data Studies. Safety 2024, 10, 47. https://doi.org/10.3390/safety10020047
Bolghanabadi S, Haghighi A, Jahangiri M. Insights into Women’s Occupational Health and Safety: A Decade in Review of Primary Data Studies. Safety. 2024; 10(2):47. https://doi.org/10.3390/safety10020047
Chicago/Turabian StyleBolghanabadi, Somayeh, Aida Haghighi, and Mehdi Jahangiri. 2024. "Insights into Women’s Occupational Health and Safety: A Decade in Review of Primary Data Studies" Safety 10, no. 2: 47. https://doi.org/10.3390/safety10020047
APA StyleBolghanabadi, S., Haghighi, A., & Jahangiri, M. (2024). Insights into Women’s Occupational Health and Safety: A Decade in Review of Primary Data Studies. Safety, 10(2), 47. https://doi.org/10.3390/safety10020047






