Inertial Motion Capturing in Ergonomic Workplace Analysis: Assessing the Correlation between RULA, Upper-Body Posture Deviations and Musculoskeletal Discomfort
Abstract
1. Introduction
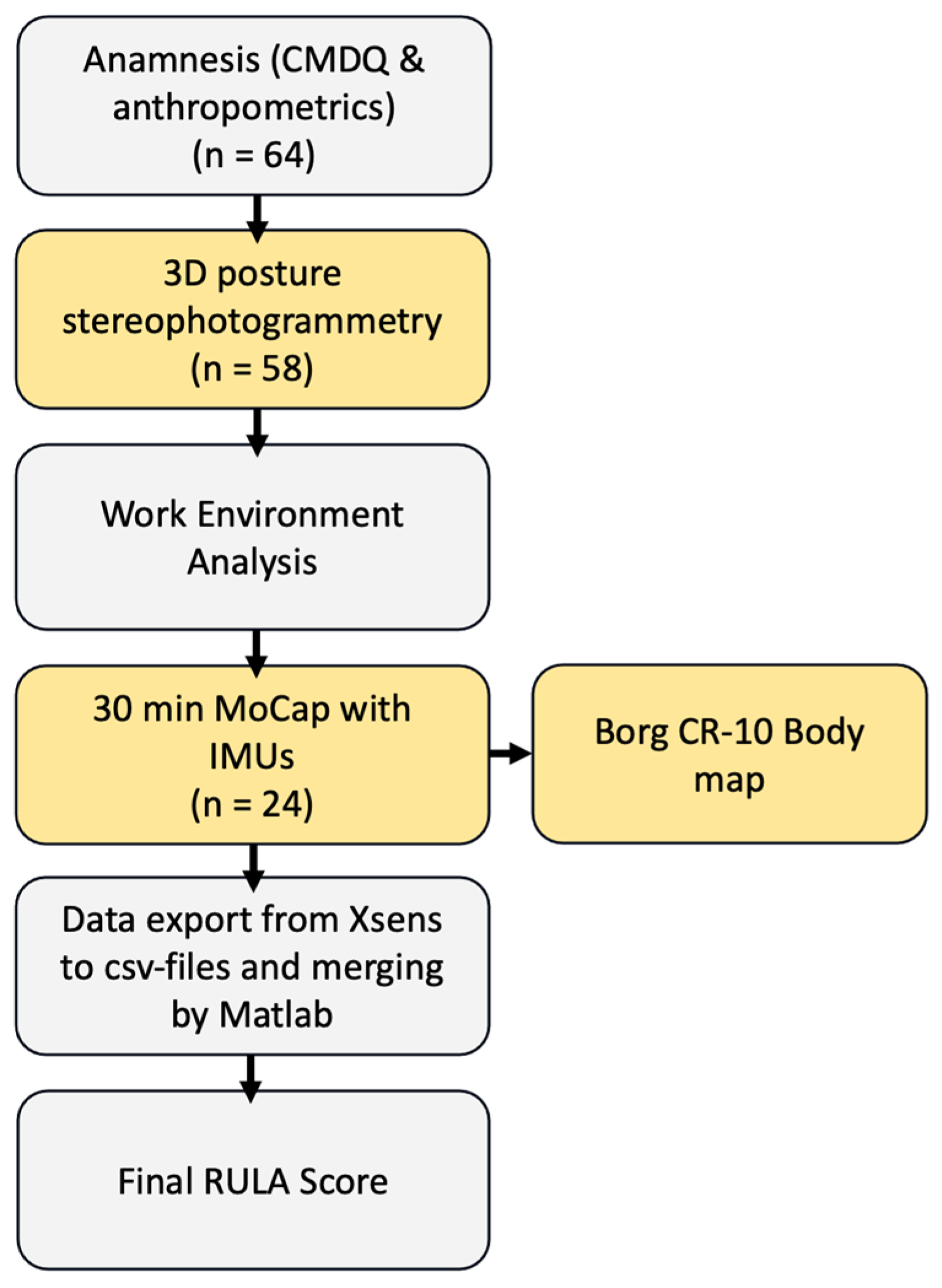
2. Materials and Methods
2.1. Subjects and Experimental Design
- Over 18 years old;
- Permanent, full-time employment contract at the company;
- Minimum of one year of professional job experience in the current professional segment.
- Acute restriction of physical activity (=medical prohibition to engage in work-related physical activity due to a medical condition or a current injury);
- Surgical treatment of the musculoskeletal system in the last 12 months [34].
2.1.1. Work Description
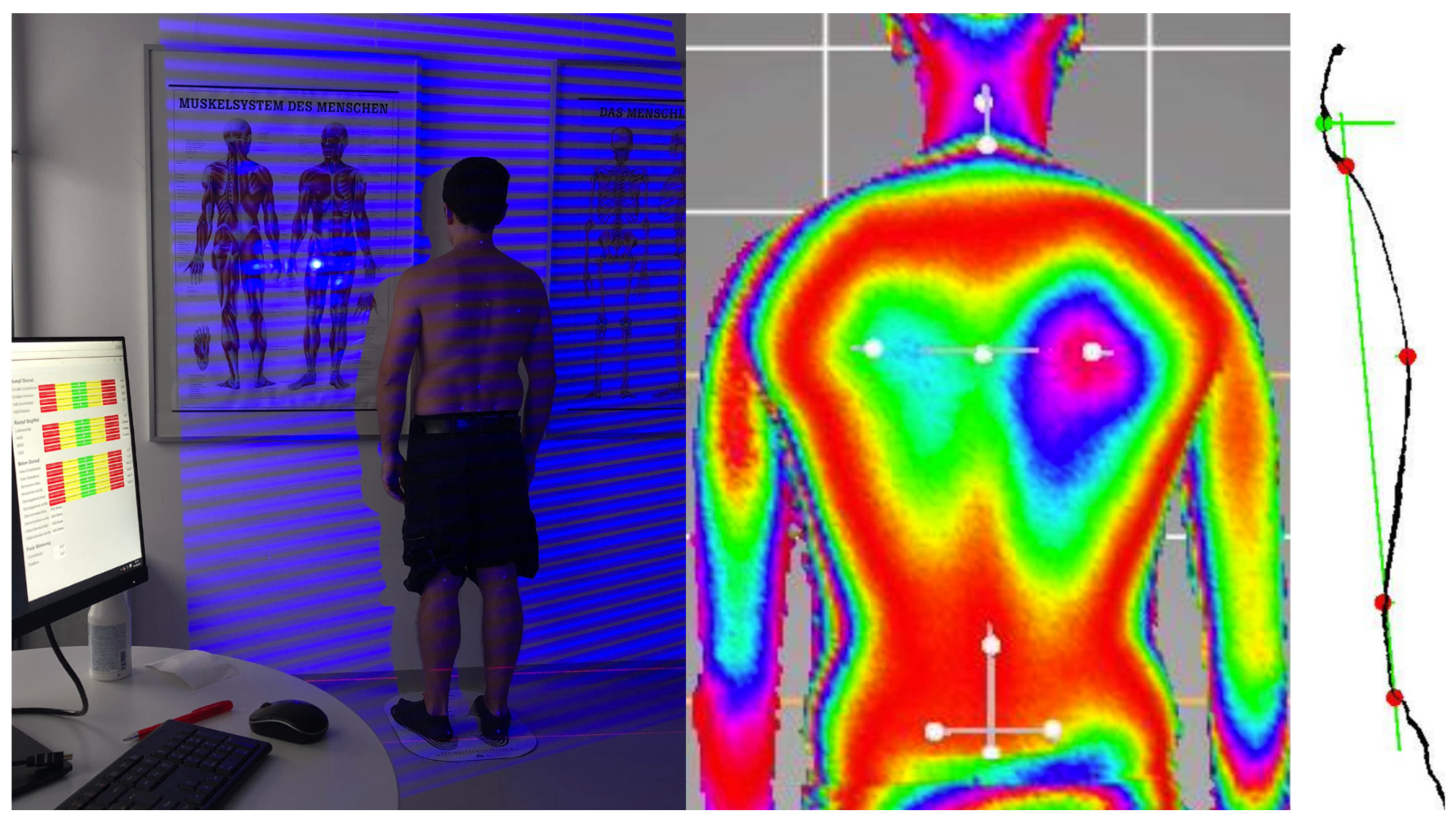
2.1.2. Assessing Musculoskeletal Discomfort and 3D Upper-Body Posture
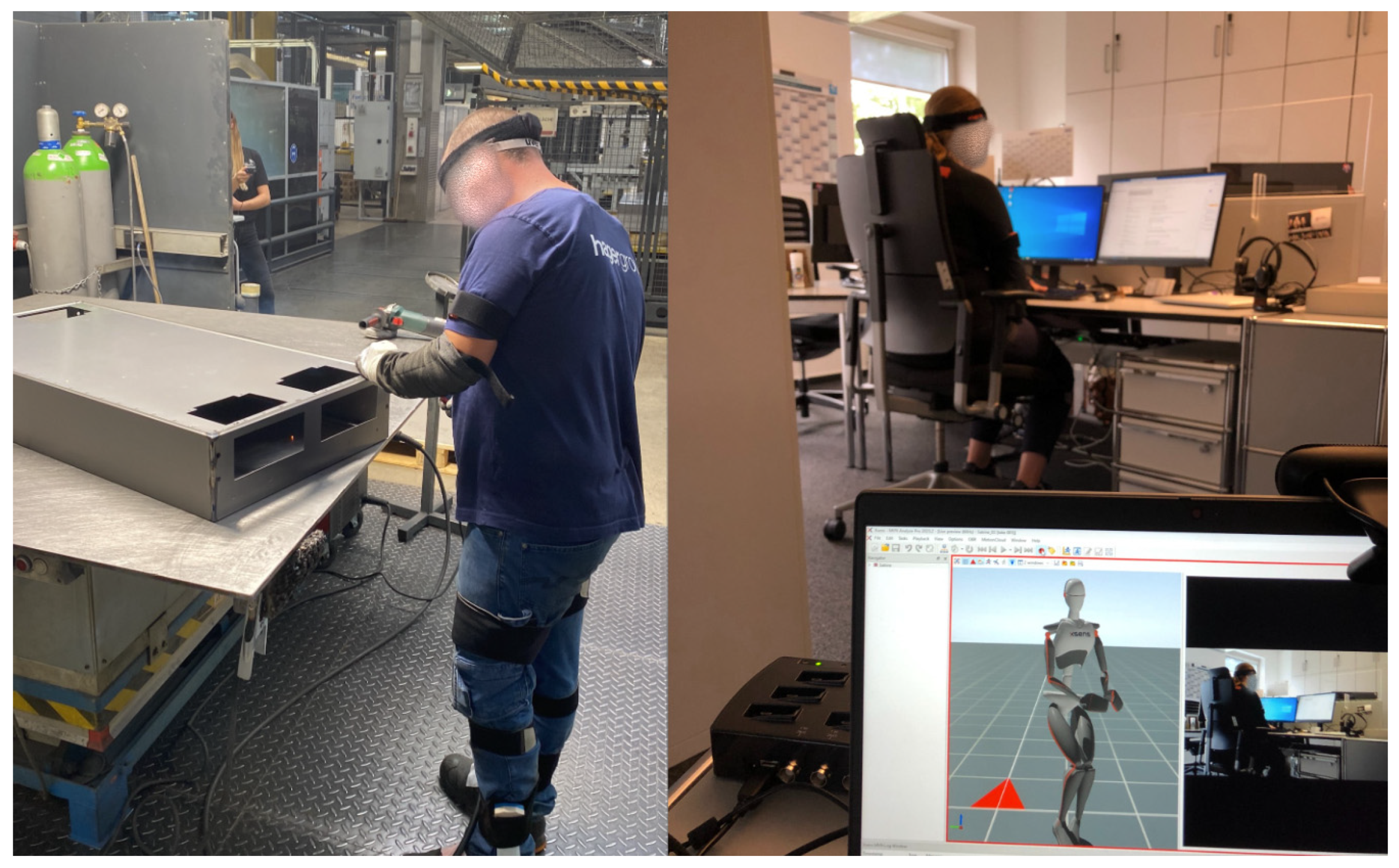
2.1.3. Kinematic Data Collection during the Work Process
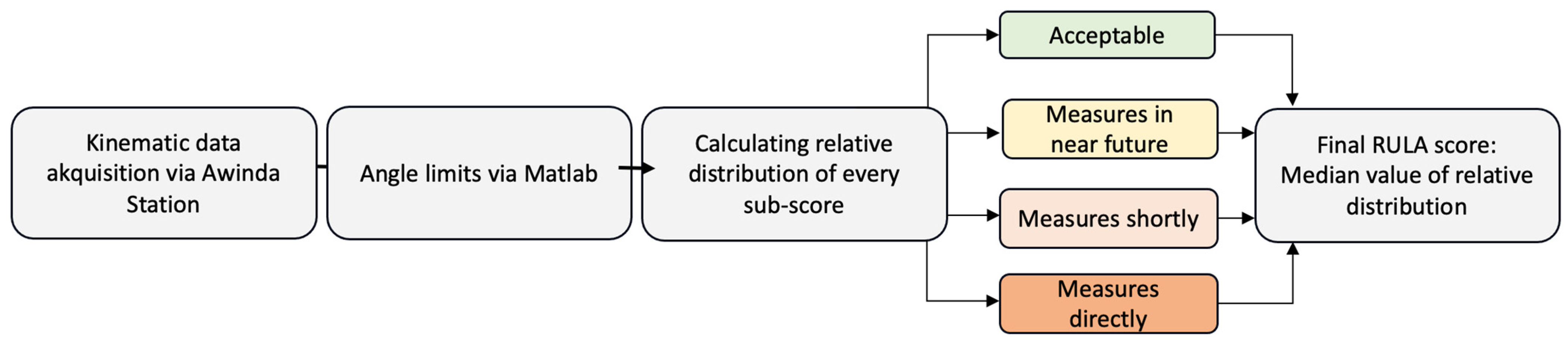
2.1.4. Observational Method RULA
- A: Upper- and lower-arms and wrists + muscle activity (none = 0; repetition or static posture > 1 min = 1) and forces (<2 kg = 0; 2–10 kg temporary = 1, 2–10 kg static or repetitive = 2; >10 kg repetitive or sudden = 3),
- B: Neck, trunk, legs + muscle activity (see above) and forces (see above).
- Office employees who exclusively worked sitting and personnel managers who worked half-sitting and half-standing/walking = 1.
- Industrial employees who worked almost exclusively from standing = 1–1.5; industrial employees who had to work with additional loads = 1.5–2.
2.2. Data Processing and Analysis
- (1) Physical exertion and musculoskeletal discomfort
- (2 + 3) Upper-body posture, RULA, and musculoskeletal discomfort
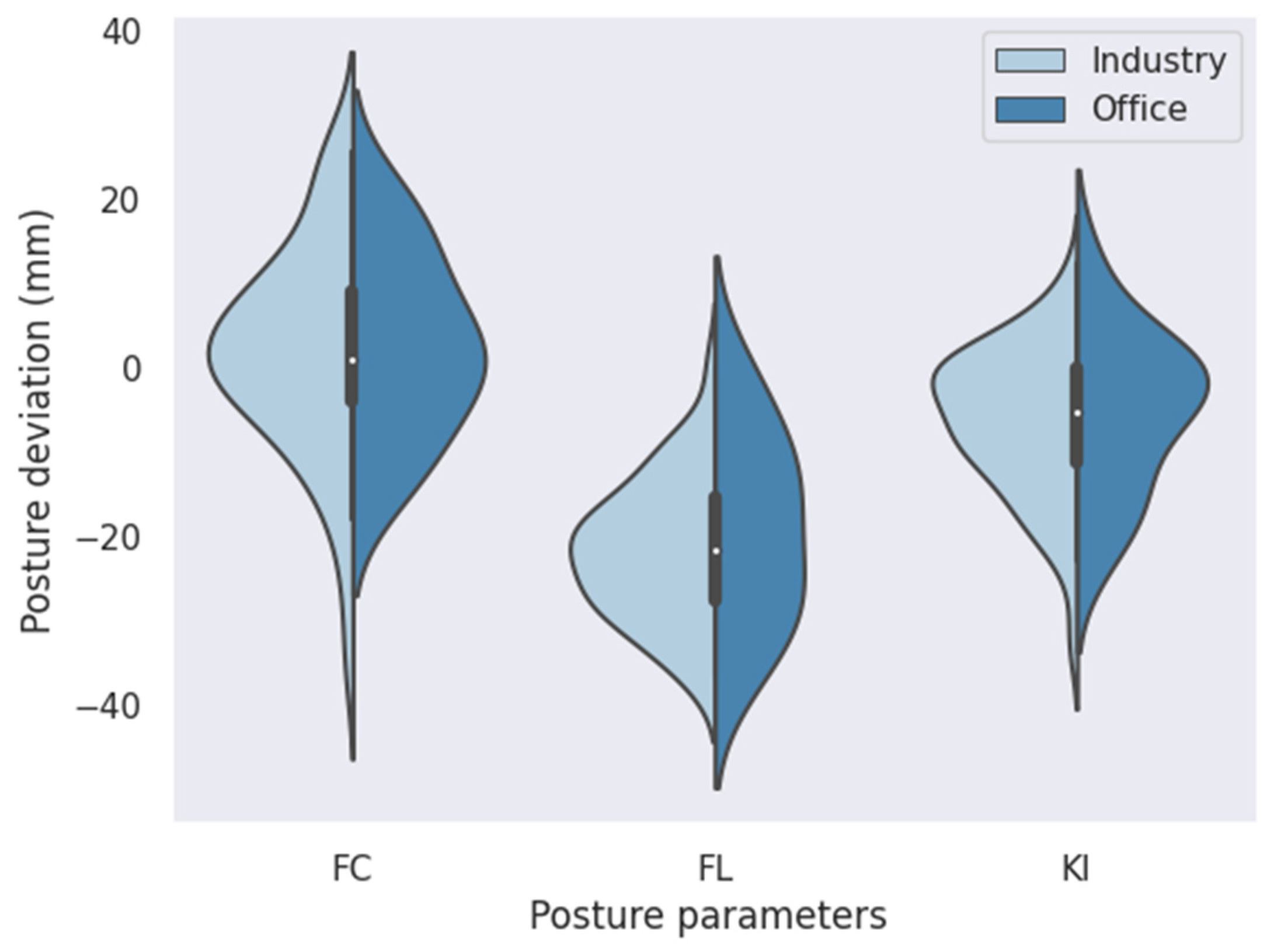
- (4) Group differences between production and office workers
3. Results
3.1. Physical Exertion and Musculoskeletal Discomfort
3.2. Upper-Body Posture, RULA, and Musculoskeletal Discomfort
4. Discussion
4.1. Results
4.2. Methods
4.3. Strengths and Limitations of This Study
4.4. Future Work
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Maulik, S.; Iqbal, R.; De, A.; Chandra, A.M. Evaluation of the working posture and prevalence of musculoskeletal symptoms among medical laboratory technicians. J. Back Musculoskelet. Rehabil. 2014, 27, 453–461. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Di, N.; Guo, W.-W.; Ding, W.-B.; Jia, N.; Zhang, H.; Li, D.; Wang, D.; Wang, R.; Zhang, D. The prevalence and risk factors of work related musculoskeletal disorders among electronics manufacturing workers: A cross-sectional analytical study in China. BMC Public Health 2023, 23, 10. [Google Scholar] [CrossRef] [PubMed]
- Daneshmandi, H.; Kee, D.; Kamalinia, M.; Oliaei, M.; Mohammadi, H. An ergonomic intervention to relieve musculoskeletal symptoms of assembly line workers at an electronic parts manufacturer in Iran. Work 2018, 61, 515–521. [Google Scholar] [CrossRef] [PubMed]
- Bonfiglioli, R.; Caraballo-Arias, Y.; Salmen-Navarro, A. Epidemiology of work-related musculoskeletal disorders. Curr. Opin. Epidemiol. Public Health 2022, 1, 18–24. [Google Scholar] [CrossRef]
- Havet, N.; Fournier, J.; Stefanelli, J.; Plantier, M.; Penot, A. Disparate exposure to physically demanding working conditions in France. Rev. D’épidémiol. Santé Publique 2020, 68, 327–336. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Xiao, L.; Zhou, H.; Xie, C.; Huang, L. An analysis of work-related musculoskeletal disorders and ergonomic loads in male welders in shipbuilding industry. Chin. J. Ind. Hyg. Occup. Dis. 2019, 37, 201–206. [Google Scholar]
- Vieira, E.R.; Kumar, S. Working postures: A literature review. J. Occup. Rehabil. 2004, 14, 143–159. [Google Scholar] [CrossRef] [PubMed]
- Hamberg-van Reenen, H.H.; van der Beek, A.J.; Blatter, B.M.; van der Grinten, M.P.; van Mechelen, W.; Bongers, P.M. Does musculoskeletal discomfort at work predict future musculoskeletal pain? Ergonomics 2008, 51, 637–648. [Google Scholar] [CrossRef]
- Hellig, T.; Johnen, L.; Mertens, A.; Nitsch, V.; Brandl, C. Prediction model of the effect of postural interactions on muscular activity and perceived exertion. Ergonomics 2020, 63, 593–606. [Google Scholar] [CrossRef]
- Åhsberg, E.; Gamberale, F. Perceived fatigue during physical work: An experimental evaluation of a fatigue inventory. Int. J. Ind. Ergon. 1998, 21, 117–131. [Google Scholar] [CrossRef]
- Ribeiro, R.P.; Sedrez, J.A.; Candotti, C.T.; Vieira, A. Relationship between chronic non-specific low back pain with disability, static posture and flexibility. Fisioter. E Pesqui. 2018, 25, 425–431. [Google Scholar] [CrossRef]
- Walker-Bone, K.; Linaker, C. Prediction of prognosis for people off sick with upper extremity musculoskeletal disorders. Occup. Environ. Med. 2016, 73, 805–806. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bontrup, C.; Taylor, W.R.; Fliesser, M.; Visscher, R.; Green, T.; Wippert, P.-M.; Zemp, R. Low back pain and its relationship with sitting behaviour among sedentary office workers. Appl. Ergon. 2019, 81, 102894. [Google Scholar] [CrossRef] [PubMed]
- Jun, D.; Zoe, M.; Johnston, V.; O’Leary, S. Physical risk factors for developing non-specific neck pain in office workers: A systematic review and meta-analysis. Int. Arch. Occup. Environ. Health 2017, 90, 373–410. [Google Scholar] [CrossRef] [PubMed]
- Odebiyi, D.O.; Okafor, U.A.C. Musculoskeletal Disorders, Workplace Ergonomics and Injury Prevention. In Ergonomics—New Insights; IntechOpen: Rijeka, Croatia, 2023. [Google Scholar]
- Huthwelker, J.; Konradi, J.; Wolf, C.; Westphal, R.; Schmidtmann, I.; Drees, P.; Betz, U. Reference Values for 3D Spinal Posture Based on Videorasterstereographic Analyses of Healthy Adults. Bioengineering 2022, 9, 809. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, O.; Dindorf, C.; Kelm, J.; Simon, S.; Nimmrichter, F.; Fröhlich, M. Reference Values for Sagittal Clinical Posture Assessment in People Aged 10 to 69 Years. Int. J. Environ. Res. Public Health 2023, 20, 4131. [Google Scholar] [CrossRef] [PubMed]
- Dindorf, C.; Konradi, J.; Wolf, C.; Taetz, B.; Bleser, G.; Huthwelker, J.; Werthmann, F.; Bartaguiz, E.; Kniepert, J.; Drees, P. Classification and automated interpretation of spinal posture data using a pathology-independent classifier and explainable artificial intelligence (Xai). Sensors 2021, 21, 6323. [Google Scholar] [CrossRef] [PubMed]
- Ohlendorf, D.; Avaniadi, I.; Adjami, F.; Christian, W.; Doerry, C.; Fay, V.; Fisch, V.; Gerez, A.; Goecke, J.; Kaya, U. Standard values of the upper body posture in healthy adults with special regard to age, sex and BMI. Sci. Rep. 2023, 13, 873. [Google Scholar] [CrossRef]
- Czaprowski, D.; Stoliński, Ł.; Tyrakowski, M.; Kozinoga, M.; Kotwicki, T. Non-structural misalignments of body posture in the sagittal plane. Scoliosis Spinal Disord. 2018, 13, 6. [Google Scholar] [CrossRef]
- Fortin, C.; Ehrmann Feldman, D.; Cheriet, F.; Labelle, H. Clinical methods for quantifying body segment posture: A literature review. Disabil. Rehabil. 2011, 33, 367–383. [Google Scholar] [CrossRef]
- Walicka-Cupryś, K.; Wyszyńska, J.; Podgórska-Bednarz, J.; Drzał-Grabiec, J. Concurrent validity of photogrammetric and inclinometric techniques based on assessment of anteroposterior spinal curvatures. Eur. Spine J. 2018, 27, 497–507. [Google Scholar] [CrossRef] [PubMed]
- Singla, D.; Veqar, Z.; Hussain, M.E. Photogrammetric assessment of upper body posture using postural angles: A literature review. J. Chiropr. Med. 2017, 16, 131–138. [Google Scholar] [CrossRef] [PubMed]
- D’Amico, M.; Kinel, E.; Roncoletta, P. Normative 3D opto-electronic stereo-photogrammetric posture and spine morphology data in young healthy adult population. PLoS ONE 2017, 12, e0179619. [Google Scholar] [CrossRef] [PubMed]
- Ohlendorf, D.; Sosnov, P.; Keller, J.; Wanke, E.M.; Oremek, G.; Ackermann, H.; Groneberg, D.A. Standard reference values of the upper body posture in healthy middle-aged female adults in Germany. Sci. Rep. 2021, 11, 2359. [Google Scholar] [CrossRef] [PubMed]
- Ohlendorf, D.; Gerez, A.; Porsch, L.; Holzgreve, F.; Maltry, L.; Ackermann, H.; Groneberg, D.A. Standard reference values of the upper body posture in healthy male adults aged between 41 and 50 years in Germany. Sci. Rep. 2020, 10, 3823. [Google Scholar] [CrossRef] [PubMed]
- Ohlendorf, D.; Fisch, V.; Doerry, C.; Schamberger, S.; Oremek, G.; Ackermann, H.; Schulze, J. Standard reference values of the upper body posture in healthy young female adults in Germany: An observational study. BMJ Open 2018, 8, e022236. [Google Scholar] [CrossRef] [PubMed]
- Wolf, C.; Betz, U.; Huthwelker, J.; Konradi, J.; Westphal, R.S.; Cerpa, M.; Lenke, L.; Drees, P. Evaluation of 3D vertebral and pelvic position by surface topography in asymptomatic females: Presentation of normative reference data. J. Orthop. Surg. Res. 2021, 16, 703. [Google Scholar] [CrossRef]
- Lowe, B.D.; Dempsey, P.G.; Jones, E.M. Ergonomics assessment methods used by ergonomics professionals. Appl. Ergon. 2019, 81, 102882. [Google Scholar] [CrossRef]
- Roman-Liu, D. Comparison of concepts in easy-to-use methods for MSD risk assessment. Appl. Ergon. 2014, 45, 420–427. [Google Scholar] [CrossRef]
- Kee, D. Systematic comparison of OWAS, RULA, and REBA based on a literature review. Int. J. Environ. Res. Public Health 2022, 19, 595. [Google Scholar] [CrossRef]
- Maltry, L.; Holzgreve, F.; Maurer, C.; Wanke, E.; Ohlendorf, D. Improved ergonomic risk assessment through the combination of inertial sensors and observational methods exemplified by RULA. Zentralblatt Arbeitsmedizin Arbeitsschutz Ergon. 2020, 70, 236–239. [Google Scholar] [CrossRef]
- Charles, R.L.; Nixon, J. Measuring mental workload using physiological measures: A systematic review. Appl. Ergon. 2019, 74, 221–232. [Google Scholar] [CrossRef] [PubMed]
- Hellig, T.; Rick, V.; Mertens, A.; Nitsch, V.; Brandl, C. Investigation of observational methods assessing workload of static working postures based on surface electromyography. Work 2019, 62, 185–195. [Google Scholar] [CrossRef] [PubMed]
- Village, J.; Frazer, M.; Cohen, M.; Leyland, A.; Park, I.; Yassi, A. Electromyography as a measure of peak and cumulative workload in intermediate care and its relationship to musculoskeletal injury: An exploratory ergonomic study. Appl. Ergon. 2005, 36, 609–618. [Google Scholar] [CrossRef] [PubMed]
- Chander, H.; Burch, R.F.; Talegaonkar, P.; Saucier, D.; Luczak, T.; Ball, J.E.; Turner, A.; Kodithuwakku Arachchige, S.N.; Carroll, W.; Smith, B.K. Wearable stretch sensors for human movement monitoring and fall detection in ergonomics. Int. J. Environ. Res. Public Health 2020, 17, 3554. [Google Scholar] [CrossRef] [PubMed]
- Maurer-Grubinger, C.; Holzgreve, F.; Fraeulin, L.; Betz, W.; Erbe, C.; Brueggmann, D.; Wanke, E.M.; Nienhaus, A.; Groneberg, D.A.; Ohlendorf, D. Combining ergonomic risk assessment (RULA) with inertial motion capture technology in dentistry—Using the benefits from two worlds. Sensors 2021, 21, 4077. [Google Scholar] [CrossRef] [PubMed]
- McAtamney, L.; Corlett, E.N. RULA: A survey method for the investigation of work-related upper limb disorders. Appl. Ergon. 1993, 24, 91–99. [Google Scholar] [CrossRef]
- Lim, S.; D’Souza, C. A narrative review on contemporary and emerging uses of inertial sensing in occupational ergonomics. Int. J. Ind. Ergon. 2020, 76, 102937. [Google Scholar] [CrossRef]
- Brandl, C.; Bonin, D.; Mertens, A.; Wischniewski, S.; Schlick, C.M. Methodik zur Unterstützung des ergonomischen Interventionsprozesses am Beispiel einer automatisierten OWAS-basierten Generierung von Vorschlägen zur technischen Gestaltung von Arbeitsplätzen. In Arbeit in Komplexen Systemen. Digital, Vernetzt, Human?! Bericht zum 62. Arbeitswissenschaftlichen Kongress vom 2.–4. März 2016; RWTH Aachen University, Institut für Arbeitswissenschaft (IAW) Dortmund, GfA-Press: Aachen, Germany, 2016; ISBN 978-3-936804-20-1. Seiten 5, Projektnummer: F 2348. [Google Scholar]
- Crecan, C.M.; Peștean, C.P. Inertial Sensor Technologies—Their Role in Equine Gait Analysis, a Review. Sensors 2023, 23, 6301. [Google Scholar] [CrossRef]
- Teufl, W.; Lorenz, M.; Miezal, M.; Taetz, B.; Fröhlich, M.; Bleser, G. Towards inertial sensor based mobile gait analysis: Event-detection and spatio-temporal parameters. Sensors 2018, 19, 38. [Google Scholar] [CrossRef]
- Humadi, A.; Nazarahari, M.; Ahmad, R.; Rouhani, H. Instrumented ergonomic risk assessment using wearable inertial measurement units: Impact of joint angle convention. IEEE Access 2020, 9, 7293–7305. [Google Scholar] [CrossRef]
- Zhang, X.; Schall, M.C., Jr.; Chen, H.; Gallagher, S.; Davis, G.A.; Sesek, R. Manufacturing worker perceptions of using wearable inertial sensors for multiple work shifts. Appl. Ergon. 2022, 98, 103579. [Google Scholar] [CrossRef] [PubMed]
- Humadi, A.; Nazarahari, M.; Ahmad, R.; Rouhani, H. In-field instrumented ergonomic risk assessment: Inertial measurement units versus Kinect V2. Int. J. Ind. Ergon. 2021, 84, 103147. [Google Scholar] [CrossRef]
- Lobo, D.; Anuarbe, P.; López-Higuera, J.M.; Viera, J.; Castillo, N.; Megía, R. Estimation of surgeons’ ergonomic dynamics with a structured light system during endoscopic surgery. Int. Forum Allergy Rhinol. 2019, 9, 857–864. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Buckle, P. Current techniques for assessing physical exposure to work-related musculoskeletal risks, with emphasis on posture-based methods. Ergonomics 1999, 42, 674–695. [Google Scholar] [CrossRef] [PubMed]
- Ezzatvar, Y.; Calatayud, J.; Andersen, L.L.; Aiguadé, R.; Benítez, J.; Casaña, J. Professional experience, work setting, work posture and workload influence the risk for musculoskeletal pain among physical therapists: A cross-sectional study. Int. Arch. Occup. Environ. Health 2020, 93, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Kreuzfeld, S.; Seibt, R.; Kumar, M.; Rieger, A.; Stoll, R. German version of the Cornell Musculoskeletal Discomfort Questionnaire (CMDQ): Translation and validation. J. Occup. Med. Toxicol. 2016, 11, 13. [Google Scholar] [CrossRef]
- Bandyopadhyay, S.; Bandyopadhyay, L.; Dasgupta, A.; Paul, B.; Roy, S.; Kumar, M. Quantification of Musculoskeletal Discomfort among Automobile Garage Workers: A Cross-sectional Analytical Study in Chetla, Kolkata, West Bengal. J. Clin. Diagn. Res. 2021, 15, 1. [Google Scholar] [CrossRef]
- Tischer, T.; Oye, S.; Wolf, A.; Feldhege, F.; Jacksteit, R.; Mittelmeier, W.; Bader, R.; Mau-Moeller, A. Measuring lower limb circumference and volume–introduction of a novel optical 3D volumetric measurement system. Biomed. Eng. Biomed. Technol. 2020, 65, 237–241. [Google Scholar] [CrossRef]
- Paul, S.M.; Chamberlin, A.P.; Hatt, C.; Nayak, A.V.; Danoff, J.V. Reliability, validity, and precision of an active stereophotogrammetry system for three-dimensional evaluation of the human torso. Med. Eng. Phys. 2009, 31, 1337–1342. [Google Scholar] [CrossRef]
- Allier, F.; Monnet, S. Mesure des flèches vertébrales par le télémètre laser. Évaluation de la fiabilité de la mesure de la flèche lombaire. Kinésithérapie Rev. 2013, 13, 41–46. [Google Scholar] [CrossRef]
- Roetenberg, D.; Luinge, H.; Slycke, P. Xsens MVN: Full 6DOF human motion tracking using miniature inertial sensors. Xsens Motion Technol. BV Technol. Rep 2009, 1, 1–7. [Google Scholar]
- Tognetti, A.; Lorussi, F.; Mura, G.D.; Carbonaro, N.; Pacelli, M.; Paradiso, R.; Rossi, D.D. New generation of wearable goniometers for motion capture systems. J. Neuroeng. Rehabil. 2014, 11, 56. [Google Scholar] [CrossRef] [PubMed]
- Picerno, P.; Cereatti, A.; Cappozzo, A. Joint kinematics estimate using wearable inertial and magnetic sensing modules. Gait Posture 2008, 28, 588–595. [Google Scholar] [CrossRef] [PubMed]
- Borg, G. Psychophysical scaling with applications in physical work and the perception of exertion. Scand. J. Work. Environ. Health 1990, 16, 55–58. [Google Scholar] [CrossRef]
- Waongenngarm, P.; van der Beek, A.J.; Janwantanakul, P.; Akkarakittichoke, N.; Coenen, P. Can the Borg CR-10 scale for neck and low back discomfort predict future neck and low back pain among high-risk office workers? Int. Arch. Occup. Environ. Health 2022, 95, 1881–1889. [Google Scholar] [CrossRef]
- Unfallversicherung, D.G. DGUV Grundsätze für Arbeitsmedizinische Vorsorgeuntersuchungen. 5. Vollst. neu Bearb. Aufl; Gentner: Stuttgart, Germany, 2010. [Google Scholar]
- Waskom, M.L. Seaborn: Statistical data visualization. J. Open Source Softw. 2021, 6, 3021. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge: New York, NY, USA, 1988; Volume 2, p. 567. [Google Scholar]
- Balogh, I.; Örbaek, P.; Ohlsson, K.; Nordander, C.; Unge, J.; Winkel, J.; Hansson, G.-Å.; Group, M.S.N.S. Self-assessed and directly measured occupational physical activities—Influence of musculoskeletal complaints, age and gender. Appl. Ergon. 2004, 35, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Jakobsen, M.D.; Sundstrup, E.; Persson, R.; Andersen, C.H.; Andersen, L.L. Is Borg’s perceived exertion scale a useful indicator of muscular and cardiovascular load in blue-collar workers with lifting tasks? A cross-sectional workplace study. Eur. J. Appl. Physiol. 2014, 114, 425–434. [Google Scholar] [CrossRef]
- Koskelo, R.; Vuorikari, K.; Hänninen, O. Sitting and standing postures are corrected by adjustable furniture with lowered muscle tension in high-school students. Ergonomics 2007, 50, 1643–1656. [Google Scholar] [CrossRef]
- Rodrigues, M.S.A.; Leite, R.D.V.; Lelis, C.M.; Chaves, T.C. Differences in ergonomic and workstation factors between computer office workers with and without reported musculoskeletal pain. Work 2017, 57, 563–572. [Google Scholar] [CrossRef]




| Age (Years) | Height (m) | Weight (kg) | BMI (kg/m2) | Job Experience (Years) | |||
|---|---|---|---|---|---|---|---|
| production n = 49 | male n = 36 | mean | 39.25 | 1.76 | 82.86 | 26.60 | 8.86 |
| SD | 10.42 | 0.07 | 13.00 | 3.68 | 8.65 | ||
| min | 22 | 1.63 | 60.30 | 20.76 | 1.00 | ||
| max | 61 | 1.88 | 115.20 | 41.40 | 38.00 | ||
| female n = 13 | mean | 48.92 | 1.63 | 69.23 | 26.03 | 17.19 | |
| SD | 14.02 | 0.05 | 13.48 | 4.78 | 13.35 | ||
| min | 25 | 1.56 | 49.40 | 19.14 | 1.50 | ||
| max | 63 | 1.73 | 93.00 | 34.38 | 35.00 | ||
| office n = 15 | male n = 8 | mean | 40.13 | 1.83 | 93.13 | 27.77 | 7.69 |
| SD | 6.66 | 0.10 | 18.77 | 4.01 | 5.89 | ||
| min | 30 | 1.68 | 73.50 | 20.01 | 1.00 | ||
| max | 52 | 1.99 | 132.00 | 33.33 | 18.00 | ||
| female n = 7 | mean | 48.00 | 1.69 | 74.71 | 26.11 | 19.86 | |
| SD | 13.52 | 0.03 | 12.16 | 3.51 | 15.76 | ||
| min | 28 | 1.64 | 57.40 | 21.19 | 1.00 | ||
| max | 62 | 1.73 | 92.20 | 30.80 | 42.00 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Simon, S.; Dully, J.; Dindorf, C.; Bartaguiz, E.; Walle, O.; Roschlock-Sachs, I.; Fröhlich, M. Inertial Motion Capturing in Ergonomic Workplace Analysis: Assessing the Correlation between RULA, Upper-Body Posture Deviations and Musculoskeletal Discomfort. Safety 2024, 10, 16. https://doi.org/10.3390/safety10010016
Simon S, Dully J, Dindorf C, Bartaguiz E, Walle O, Roschlock-Sachs I, Fröhlich M. Inertial Motion Capturing in Ergonomic Workplace Analysis: Assessing the Correlation between RULA, Upper-Body Posture Deviations and Musculoskeletal Discomfort. Safety. 2024; 10(1):16. https://doi.org/10.3390/safety10010016
Chicago/Turabian StyleSimon, Steven, Jonas Dully, Carlo Dindorf, Eva Bartaguiz, Oliver Walle, Ilsemarie Roschlock-Sachs, and Michael Fröhlich. 2024. "Inertial Motion Capturing in Ergonomic Workplace Analysis: Assessing the Correlation between RULA, Upper-Body Posture Deviations and Musculoskeletal Discomfort" Safety 10, no. 1: 16. https://doi.org/10.3390/safety10010016
APA StyleSimon, S., Dully, J., Dindorf, C., Bartaguiz, E., Walle, O., Roschlock-Sachs, I., & Fröhlich, M. (2024). Inertial Motion Capturing in Ergonomic Workplace Analysis: Assessing the Correlation between RULA, Upper-Body Posture Deviations and Musculoskeletal Discomfort. Safety, 10(1), 16. https://doi.org/10.3390/safety10010016








