Z2-γ: An Application of Zienkiewicz-Zhu Error Estimator to Brain Tumor Detection in MR Images
Abstract
1. Introduction
- A suitable correction is applied to pre-process the data;
- The use of finite-elements and Z2 error estimator with isotropic mesh refinement allows for automatically detecting the anomalous areas, if present;
- A post-processing phase, based on the use of morphological transformations, allows for getting rid of the cortex and better locating the anomalous tissues, if present.
2. Mathematical Framework
A Metastatic Brain Tumor Example
3. Experimental Results
3.1. Pre-Processing
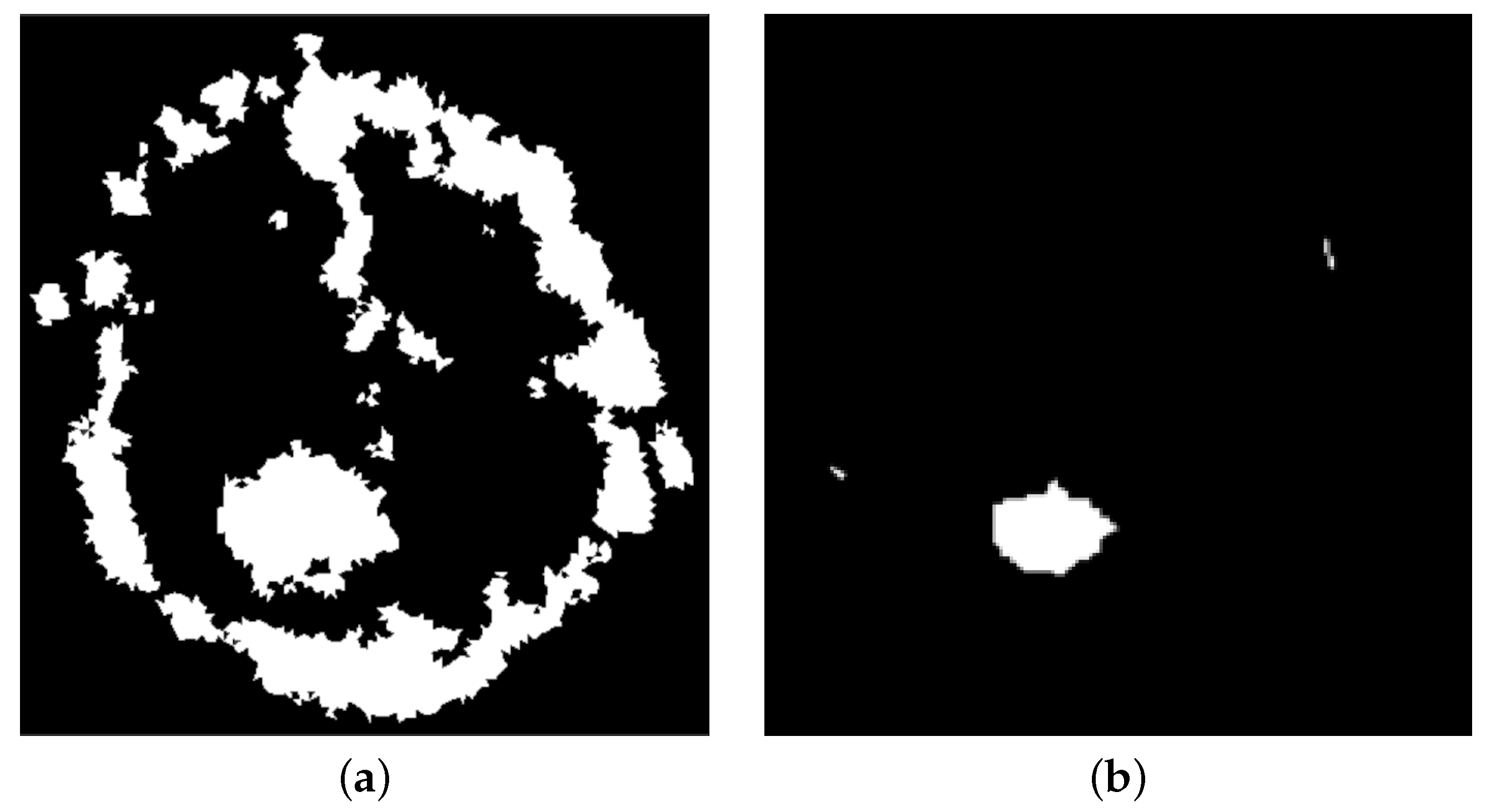
3.2. Post-Processing
3.3. Correction
4. Discussion
- TP: true positive, i.e., affected brains correctly classified;
- TN: true negative, i.e., healthy brains correctly classified;
- FP: false positive, i.e., healthy brains mistakenly classified as affected;
- FN: false negative, i.e., affected brains wrongly classified as healthy;
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| MRI | Magnetic Resonance Imaging |
| T1 | Longitudinal relaxation time |
| T2 | Transversal relaxation time |
| RT | Repetition time |
| RE | Time to echo |
| Z2 | Zienkiewicz–Zhu error estimator |
| OA | Overall accuracy (or simply accuracy) |
| F_1 | F_1 score |
References
- Zienkiewicz, O.C.; Zhu, J.Z. A simple error estimator and adaptive procedure for practical engineerng analysis. Int. J. Numer. Methods Eng. 1987, 24, 337–357. [Google Scholar] [CrossRef]
- Zienkiewicz, O.C.; Zhu, J.Z. The superconvergent patch recovery and a posteriori error estimates. Part 1: The recovery technique. Int. J. Numer. Methods Eng. 1992, 33, 1331–1364. [Google Scholar] [CrossRef]
- Zienkiewicz, O.C.; Zhu, J.Z. The superconvergent patch recovery and a posteriori error estimates. Part 2: Error estimates and adaptivity. Int. J. Numer. Methods Eng. 1992, 33, 1365–1382. [Google Scholar] [CrossRef]
- Bourdin, B. Image segmentation with a finite element method. ESAIM Math. Model. Numer. Anal. 1999, 33, 229–244. [Google Scholar] [CrossRef]
- Chiappa, A.S.; Micheletti, S.; Peli, R.; Perotto, S. Mesh adaptation-aided image segmentation. Commun. Nonlinear Sci. Numer. Simul. 2019, 74, 147–166. [Google Scholar] [CrossRef]
- Clerici, F.; Ferro, N.; Marconi, S.; Micheletti, S.; Negrello, E.; Perotto, S. Anisotropic adapted meshes for image segmentation: Application to three-dimensional medical data. SIAM J. Imaging Sci. 2020, 13, 2189–2212. [Google Scholar] [CrossRef]
- Giacomini, M.; Perotto, S. Anisotropic mesh adaptation for region-based segmentation accounting for image spatial information. Comput. Math. Appl. 2022, 121, 1–17. [Google Scholar] [CrossRef]
- Yaacobson, F.S.; Givoli, D. An adaptive finite element procedure for the image segmentation problem. Commun. Numer. Methods Eng. 1998, 14, 621–632. [Google Scholar] [CrossRef]
- Amin, J.; Sharif, M.; Raza, M.; Saba, T.; Anjum, M.A. Brain tumor detection using statistical and machine learning method. Comput. Methods Programs Biomed. 2019, 177, 69–79. [Google Scholar] [CrossRef]
- Sharif, M.; Amin, J.; Raza, M.; Anjum, M.A.; Afzal, H.; Shad, S.A. Brain tumor detection based on extreme learning. Neural Comput. Appl. 2020, 32, 15975–15987. [Google Scholar] [CrossRef]
- Seetha, J.; Raja, S.S. Brain tumor classification using convolutional neural networks. Biomed. Pharmacol. J. 2018, 11, 1457. [Google Scholar] [CrossRef]
- Othman, M.F.; Basri, M.A.M. Probabilistic neural network for brain tumor classification. In Proceedings of the 2011 Second International Conference on Intelligent Systems, Modelling and Simulation, Phnom Penh, Cambodia, 25–27 January 2011; pp. 136–138. [Google Scholar]
- Sapra, P.; Singh, R.; Khurana, S. Brain tumor detection using neural network. Int. J. Sci. Mod. Eng. (IJISME) 2013, 1, 2319–6386. [Google Scholar]
- Amin, J.; Sharif, M.; Yasmin, M.; Fernandes, S.L. Big data analysis for brain tumor detection: Deep convolutional neural networks. Future Gener. Comput. Syst. 2018, 87, 290–297. [Google Scholar] [CrossRef]
- Dong, H.; Yang, G.; Liu, F.; Mo, Y.; Guo, Y. Automatic brain tumor detection and segmentation using U-Net based fully convolutional networks. In Proceedings of the Annual Conference on Medical Image Understanding and Analysis, Edinburgh, UK, 11–13 July 2017; pp. 506–517. [Google Scholar]
- Zhang, W.; Wu, Y.; Yang, B.; Hu, S.; Wu, L.; Dhelim, S. Overview of multi-modal brain tumor mr image segmentation. Healthcare 2021, 9, 1051. [Google Scholar] [CrossRef]
- Abdel-Maksoud, E.; Elmogy, M.; Al-Awadi, R. Brain tumor segmentation based on a hybrid clustering technique. Egypt. Inform. J. 2015, 16, 71–81. [Google Scholar] [CrossRef]
- Alam, M.S.; Rahman, M.M.; Hossain, M.A.; Islam, M.K.; Ahmed, K.M.; Ahmed, K.T.; Singh, B.C.; Miah, M.S. Automatic human brain tumor detection in MRI image using template-based K means and improved fuzzy C means clustering algorithm. Big Data Cogn. Comput. 2019, 3, 27. [Google Scholar] [CrossRef]
- Islam, M.K.; Ali, M.S.; Miah, M.S.; Rahman, M.M.; Alam, M.S.; Hossain, M.A. Brain tumor detection in MR image using superpixels, principal component analysis and template based K-means clustering algorithm. Mach. Learn. Appl. 2021, 5, 100044. [Google Scholar]
- Kaur, N.; Sharma, M. Brain tumor detection using self-adaptive K-means clustering. In Proceedings of the 2017 International Conference on Energy, Communication, Data Analytics and Soft Computing (ICECDS), Chennai, India, 1–2 August 2017; pp. 1861–1865. [Google Scholar]
- Malathi, M.; Sinthia, P. MRI brain tumour segmentation using hybrid clustering and classification by back propagation algorithm. Asian Pac. J. Cancer Prev. APJCP 2018, 19, 3257. [Google Scholar]
- Selvy, P.T.; Palanisamy, V.; Purusothaman, T. Performance analysis of clustering algorithms in brain tumor detection of MR images. Eur. J. Sci. Res. 2011, 62, 321–330. [Google Scholar]
- Akram, M.U.; Usman, A. Computer aided system for brain tumor detection and segmentation. In Proceedings of the International Conference on Computer Networks and Information Technology, Abbottabad, Pakistan, 11–13 July 2011; pp. 299–302. [Google Scholar]
- Amin, J.; Sharif, M.; Yasmin, M.; Fernandes, S.L. A distinctive approach in brain tumor detection and classification using MRI. Pattern Recognit. Lett. 2020, 139, 118–127. [Google Scholar] [CrossRef]
- Hedberg, H.; Kristensen, F.; Nilsson, P.; Owall, V. A low complexity architecture for binary image erosion and dilation using structuring element decomposition. In Proceedings of the 2005 IEEE International Symposium on Circuits and Systems, Kobe, Japan, 23–26 May 2005; pp. 3431–3434. [Google Scholar]
- Lemieux, L.; Hagemann, G.; Krakow, K.; Woermann, F.G. Fast, accurate, and reproducible automatic segmentation of the brain in T1-weighted volume MRI data. Magn. Reson. Med. Off. J. Int. Soc. Magn. Reson. Med. 1999, 42, 127–135. [Google Scholar] [CrossRef]
- Mustaqeem, A.; Javed, A.; Fatima, T. An efficient brain tumor detection algorithm using watershed & thresholding based segmentation. Int. J. Image Graph. Signal Process. 2012, 4, 34. [Google Scholar]
- Prajapati, S.J.; Jadhav, K.R. Brain tumor detection by various image segmentation techniques with introduction to non negative matrix factorization. Brain 2015, 4, 600–603. [Google Scholar]
- Nabizadeh, N.; John, N.; Wright, C. Histogram-based gravitational optimization algorithm on single MR modality for automatic brain lesion detection and segmentation. Expert Syst. Appl. 2014, 41, 7820–7836. [Google Scholar] [CrossRef]
- Nabizadeh, N.; Kubat, M. Brain tumors detection and segmentation in MR images: Gabor wavelet vs. statistical features. Comput. Electr. Eng. 2015, 45, 286–301. [Google Scholar] [CrossRef]
- Borole, V.Y.; Nimbhore, S.S.; Kawthekar, D.S.S. Image processing techniques for brain tumor detection: A review. Int. J. Emerg. Trends Technol. Comput. Sci. (IJETTCS) 2015, 4, 2. [Google Scholar]
- Baur, C.; Wiestler, B.; Albarqouni, S.; Navab, N. Deep autoencoding models for unsupervised anomaly segmentation in brain MR images. In Proceedings of the International MICCAI Brainlesion Workshop, Granada, Spain, 16 September 2018; pp. 161–169. [Google Scholar]
- Baur, C.; Wiestler, B.; Albarqouni, S.; Navab, N. Bayesian skip-autoencoders for unsupervised hyperintense anomaly detection in high resolution brain MRI. In Proceedings of the 2020 IEEE 17th International Symposium on Biomedical Imaging (ISBI), Iowa City, IA, USA, 3–7 April 2020; pp. 1905–1909. [Google Scholar]
- Chen, X.; You, S.; Tezcan, K.C.; Konukoglu, E. Unsupervised lesion detection via image restoration with a normative prior. Med. Image Anal. 2020, 64, 101713. [Google Scholar] [CrossRef]
- Han, C.; Rundo, L.; Murao, K.; Noguchi, T.; Shimahara, Y.; Milacski, Z.Á.; Koshino, S.; Sala, E.; Nakayama, H.; Satoh, S. MADGAN: Unsupervised medical anomaly detection GAN using multiple adjacent brain MRI slice reconstruction. BMC Bioinform. 2021, 22, 31. [Google Scholar] [CrossRef]
- Zhou, K.; Li, J.; Luo, W.; Li, Z.; Yang, J.; Fu, H.; Cheng, J.; Liu, J.; Gao, S. Proxy-bridged Image Reconstruction Network for Anomaly Detection in Medical Images. IEEE Trans. Med. Imaging 2021, 41, 582–594. [Google Scholar] [CrossRef]
- Zimmerer, D.; Isensee, F.; Petersen, J.; Kohl, S.; Maier-Hein, K. Unsupervised anomaly localization using variational auto-encoders. In Proceedings of the International Conference on Medical Image Computing and Computer-Assisted Intervention, Shenzhen, China, 13–17 October 2019; pp. 289–297. [Google Scholar]
- Atia, N.; Benzaoui, A.; Jacques, S.; Hamiane, M.; Kourd, K.E.; Bouakaz, A.; Ouahabi, A. Particle Swarm Optimization and Two-Way Fixed-Effects Analysis of Variance for Efficient Brain Tumor Segmentation. Cancers 2022, 14, 4399. [Google Scholar] [CrossRef]
- Michael Mahesh, K.; Arokia Renjit, J. Evolutionary intelligence for brain tumor recognition from MRI images: A critical study and review. Evol. Intell. 2018, 11, 19–30. [Google Scholar] [CrossRef]
- Dörfler, W. A convergent adaptive algorithm for Poisson’s equation. SIAM J. Numer. Anal. 1996, 33, 1106–1124. [Google Scholar] [CrossRef]
- Morin, P.; Nochetto, R.H.; Siebert, K.G. Data oscillation and convergence of adaptive FEM. SIAM J. Numer. Anal. 2000, 38, 466–488. [Google Scholar] [CrossRef]
- Ding, S.; Shao, G.; Huang, Y.; Shi, H. The superconvergence gradient recovery method for linear finite element method with polygons. Int. J. Numer. Methods Eng. 2021, 122, 4154–4171. [Google Scholar] [CrossRef]
- Maisano, G.; Micheletti, S.; Perotto, S.; Bottasso, C.L. On some new recovery-based a posteriori error estimators. Comput. Methods Appl. Mech. Eng. 2006, 195, 4794–4815. [Google Scholar] [CrossRef]
- Rodríguez, R. Some remarks on Zienkiewicz–Zhu estimator. Numer. Methods Partial. Differ. Equations 1994, 10, 625–635. [Google Scholar] [CrossRef]
- Zhang, Z.; Naga, A. A new finite element gradient recovery method: Superconvergence property. SIAM J. Sci. Comput. 2005, 26, 1192–1213. [Google Scholar] [CrossRef]
- Acharya, U.K.; Kumar, S. Particle swarm optimized texture based histogram equalization (PSOTHE) for MRI brain image enhancement. Optik 2020, 224, 165760. [Google Scholar] [CrossRef]
- Rundo, L.; Tangherloni, A.; Cazzaniga, P.; Nobile, M.S.; Russo, G.; Gilardi, M.C.; Vitabile, S.; Mauri, G.; Besozzi, D.; Militello, C. A novel framework for MR image segmentation and quantification by using MedGA. Comput. Methods Programs Biomed. 2019, 176, 159–172. [Google Scholar] [CrossRef]
- Haralick, R.M.; Shapiro, L.G. Computer and Robot Vision; Addison-Wesley Reading: Boston, MA, USA, 1992; Volume 1. [Google Scholar]
- Hecht, F. New development in FreeFem++. J. Numer. Math. 2012, 20, 251–265. [Google Scholar] [CrossRef]
- Lisanti, C.; Carlin, C.; Banks, K.P.; Wang, D. Normal MRI appearance and motion-related phenomena of CSF. Am. J. Roentgenol. 2007, 188, 716–725. [Google Scholar] [CrossRef] [PubMed]
- Gong, D.; Liu, L.; Le, V.; Saha, B.; Mansour, M.R.; Venkatesh, S.; Hengel, A.V.D. Memorizing normality to detect anomaly: Memory-augmented deep autoencoder for unsupervised anomaly detection. In Proceedings of the IEEE/CVF International Conference on Computer Vision, Seoul, Korea, 27 October–2 November 2019; pp. 1705–1714. [Google Scholar]
- Schlegl, T.; Seeböck, P.; Waldstein, S.M.; Schmidt-Erfurth, U.; Langs, G. Unsupervised anomaly detection with generative adversarial networks to guide marker discovery. In Proceedings of the International Conference on Information Processing in Medical Imaging, Boone, NC, USA, 25–30 June 2017; pp. 146–157. [Google Scholar]
- Schlegl, T.; Seeböck, P.; Waldstein, S.M.; Langs, G.; Schmidt-Erfurth, U. f-AnoGAN: Fast unsupervised anomaly detection with generative adversarial networks. Med. Image Anal. 2019, 54, 30–44. [Google Scholar] [CrossRef] [PubMed]
- Akcay, S.; Atapour-Abarghouei, A.; Breckon, T.P. Ganomaly: Semi-supervised anomaly detection via adversarial training. In Proceedings of the Asian Conference on Computer Vision, Perth, Australia, 2–6 December 2018; pp. 622–637. [Google Scholar]
- Zhou, K.; Gao, S.; Cheng, J.; Gu, Z.; Fu, H.; Tu, Z.; Yang, J.; Zhao, Y.; Liu, J. Sparse-gan: Sparsity-constrained generative adversarial network for anomaly detection in retinal oct image. In Proceedings of the 2020 IEEE 17th International Symposium on Biomedical Imaging (ISBI), Iowa City, IA, USA, 3–7 April 2020; pp. 1227–1231. [Google Scholar]
- Isola, P.; Zhu, J.Y.; Zhou, T.; Efros, A.A. Image-to-image translation with conditional adversarial networks. In Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition, Honolulu, HI, USA, 21–26 July 2017; pp. 1125–1134. [Google Scholar]
- Zhu, J.Y.; Park, T.; Isola, P.; Efros, A.A. Unpaired image-to-image translation using cycle-consistent adversarial networks. In Proceedings of the IEEE International Conference on Computer Vision, Venice, Italy, 22–29 October 2017; pp. 2223–2232. [Google Scholar]
- Liu, J.; Li, M.; Wang, J.; Wu, F.; Liu, T.; Pan, Y. A survey of MRI-based brain tumor segmentation methods. Tsinghua Sci. Technol. 2014, 19, 578–595. [Google Scholar]
- Tiwari, A.; Srivastava, S.; Pant, M. Brain tumor segmentation and classification from magnetic resonance images: Review of selected methods from 2014 to 2019. Pattern Recognit. Lett. 2020, 131, 244–260. [Google Scholar] [CrossRef]
- Wadhwa, A.; Bhardwaj, A.; Verma, V.S. A review on brain tumor segmentation of MRI images. Magn. Reson. Imaging 2019, 61, 247–259. [Google Scholar] [CrossRef]
- De Nunzio, G.; Pastore, G.; Donativi, M.; Castellano, A.; Falini, A. A CAD system for cerebral glioma based on texture features in DT-MR images. Nucl. Instrum. Methods Phys. Res. Sect. Accel. Spectrometers Detect. Assoc. Equip. 2011, 648, S100–S102. [Google Scholar] [CrossRef]
- Militello, C.; Rundo, L.; Dimarco, M.; Orlando, A.; Conti, V.; Woitek, R.; D’Angelo, I.; Bartolotta, T.V.; Russo, G. Semi-automated and interactive segmentation of contrast-enhancing masses on breast DCE-MRI using spatial fuzzy clustering. Biomed. Signal Process. Control. 2022, 71, 103113. [Google Scholar] [CrossRef]







| Index | Affected | Healthy |
|---|---|---|
| Sensitivity | ||
| Miss rate |
| Methods | OA | |
|---|---|---|
| Z2- | 0.846 | 0.880 |
| Auto-Encoder | 0.714 | 0.674 |
| MemAE | 0.789 | 0.722 |
| AnoGAN | 0.757 | 0.691 |
| f-AnoGAN | 0.764 | 0.675 |
| GANomaly | 0.798 | 0.667 |
| Sparse-GAN | 0.791 | 0.645 |
| pix2pix | 0.737 | 0.617 |
| Cycle-GAN | 0.752 | 0.712 |
| Proxy-Bridged | 0.805 | 0.709 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Falini, A. Z2-γ: An Application of Zienkiewicz-Zhu Error Estimator to Brain Tumor Detection in MR Images. J. Imaging 2022, 8, 301. https://doi.org/10.3390/jimaging8110301
Falini A. Z2-γ: An Application of Zienkiewicz-Zhu Error Estimator to Brain Tumor Detection in MR Images. Journal of Imaging. 2022; 8(11):301. https://doi.org/10.3390/jimaging8110301
Chicago/Turabian StyleFalini, Antonella. 2022. "Z2-γ: An Application of Zienkiewicz-Zhu Error Estimator to Brain Tumor Detection in MR Images" Journal of Imaging 8, no. 11: 301. https://doi.org/10.3390/jimaging8110301
APA StyleFalini, A. (2022). Z2-γ: An Application of Zienkiewicz-Zhu Error Estimator to Brain Tumor Detection in MR Images. Journal of Imaging, 8(11), 301. https://doi.org/10.3390/jimaging8110301











