Artificial Intelligence Dystocia Algorithm (AIDA) as a Decision Support System in Transverse Fetal Head Position
Abstract
1. Introduction
- The first comprehensive AI-based assessment of transverse fetal head positions using four integrated ultrasound parameters (MLA, AoP, HSD, AD).
- A novel risk stratification system that categorized transverse positions into three clinically meaningful subcategories.
- Superior predictive accuracy compared to traditional methods.
- Multi-algorithm validation using Random Forest, SVM, and MLP to ensure robustness.
- Objective quantification of transverse malposition severity.
- Evidence-based cut-off values derived from decision tree analysis
- Personalized labor management enabling tailored interventions.
- Early identification of futile cases to prevent prolonged labor.
- Reduction of unnecessary interventions through accurate risk stratification.
2. Materials and Methods
2.1. Study Population and Inclusion Criteria
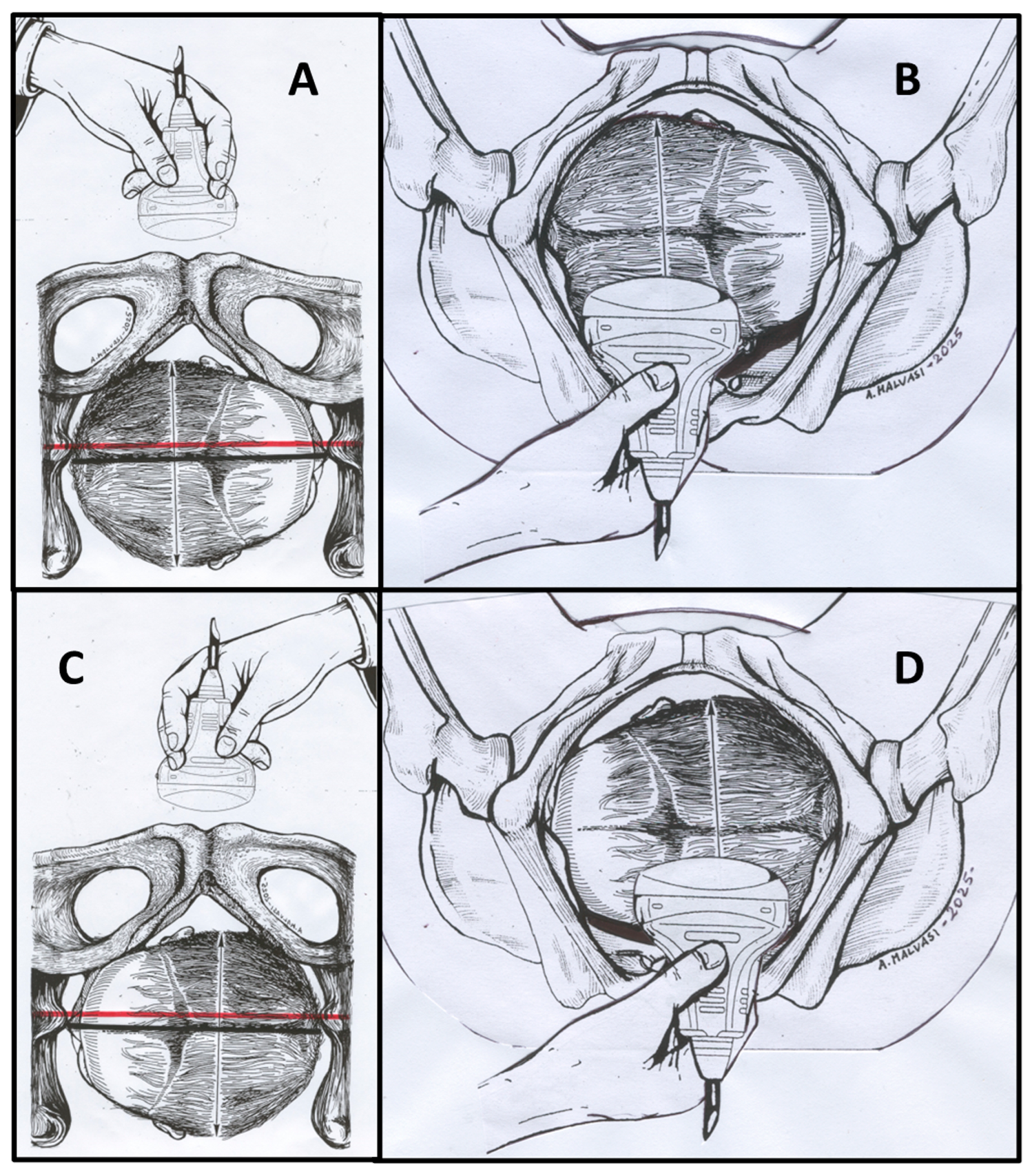
2.2. Ultrasound Assessment and Parameter Measurement
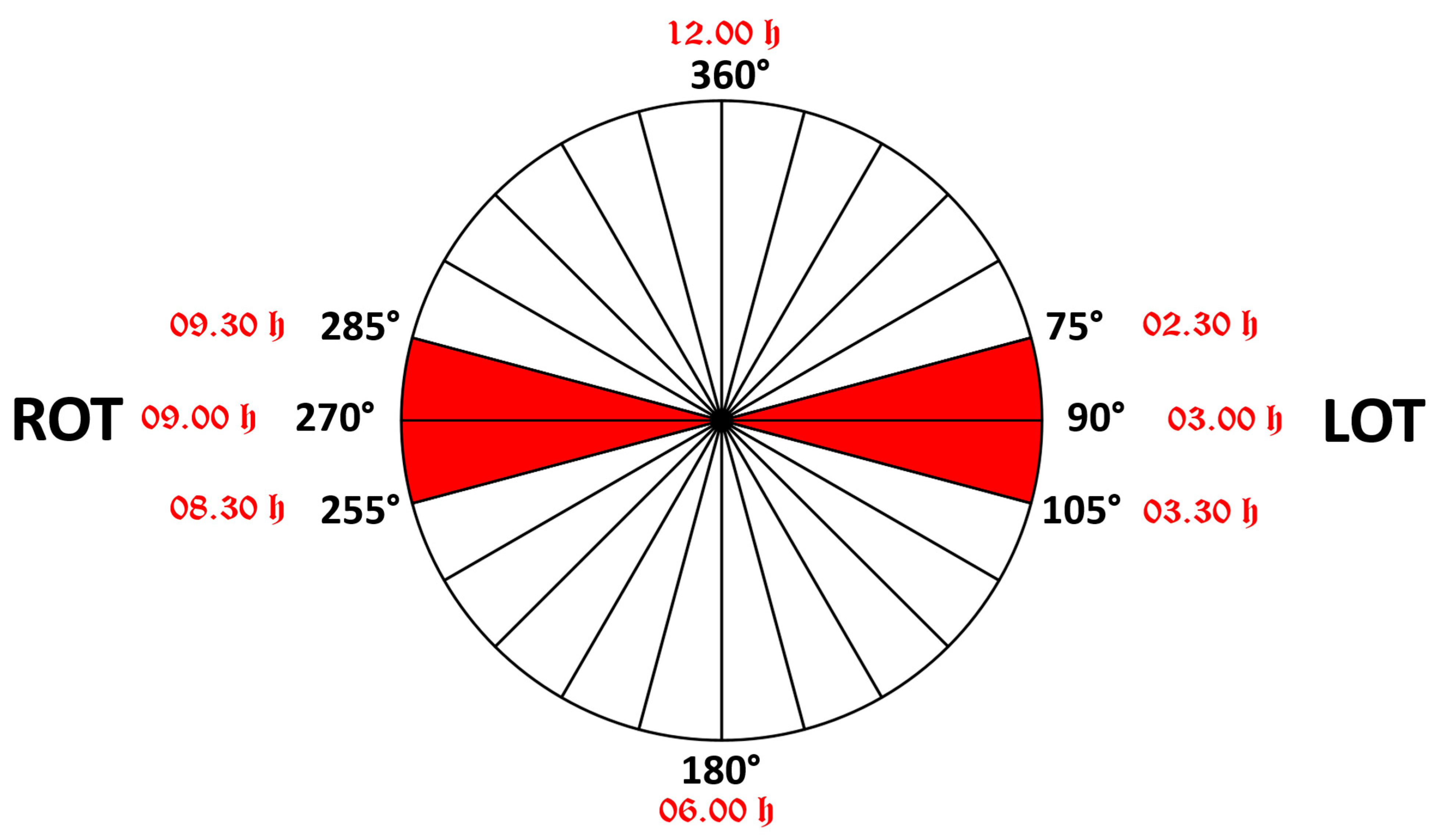
2.3. Expanded Analysis of Transverse Positions
2.4. Machine Learning Analysis
- Accuracy = (TP + TN)/(TP + TN + FP + FN)
- Sensitivity = TP/(TP + FN)
- Specificity = TN/(TN + FP)
- Positive Predictive Value (PPV) = TP/(TP + FP)
- Negative Predictive Value (NPV) = TN/(TN + FN)
- F1 Score = 2 × (Precision × Recall)/(Precision + Recall)
- Area Under ROC Curve (AUC)
2.5. Statistical Analysis
3. Results
3.1. Delivery Outcomes by Position Category
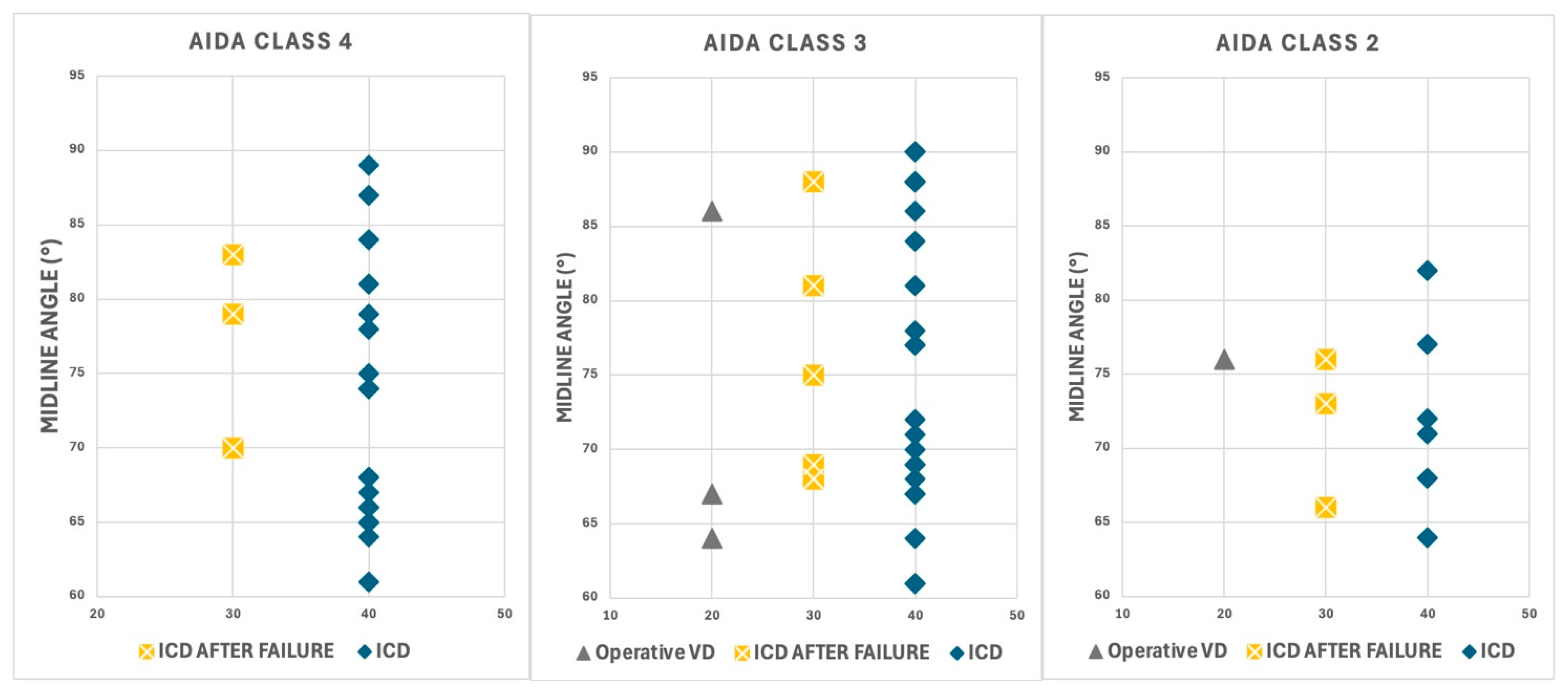
3.2. AIDA Classification Results
3.3. Machine Learning Algorithm Performance
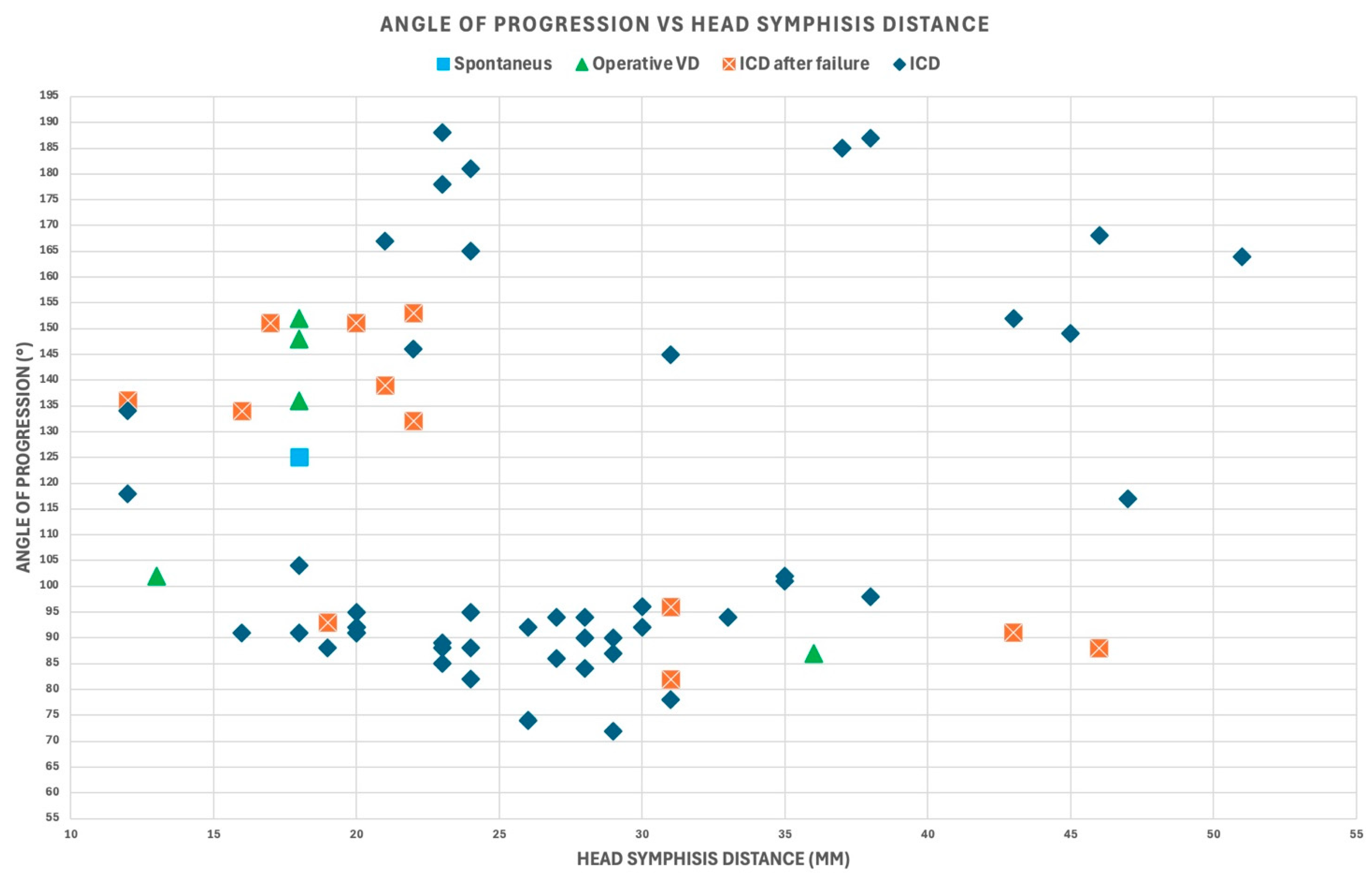
3.4. Parameter Analysis
3.5. Statistical Significance
3.5.1. Algorithm Comparison Results
3.5.2. Confidence Interval Analysis
3.5.3. Clinical Significance
3.5.4. AIDA Class-Specific Analysis
3.5.5. Pearson’s Correlation Significance
4. Discussion
4.1. Principal Findings
4.2. Results in the Context of the Existing Literature
4.3. Clinical Implications
4.4. Potential Clinical Applications
- Early identification of high-risk cases: accurate prediction of ICD likelihood in AIDA class 4 cases could facilitate timely intervention.
- Reduction in unnecessary interventions: reliable identification of low-risk cases (AIDA class 0) could help avoid unnecessary cesarean deliveries.
- Personalized labor management: integration of multiple parameters allowed for more nuanced assessment of individual cases.
- Targeted interventions: understanding the degree of malposition could guide specific interventions.
- Optimized timing of interventions: earlier decision-making for cesarean delivery could potentially reduce risks associated with prolonged labor.
4.5. Study Limitations and Future Research Directions
- Develop comprehensive SHAP (SHapley Additive exPlanations) value interpretations for AIDA Class 1 and Class 2.
- Investigate the predictive significance of partially RED-classified parameters.
- Generate advanced visualization techniques to communicate parameter importance and model interpretability.
- Explore the intricate interactions between geometric parameters in intermediate classification scenarios.
- Conduct large-scale, multi-center studies involving 5000–10,000 patients across 10–15 centers.
- Explore diverse geographical regions, healthcare systems, and patient populations.
- Incorporate varied healthcare settings, including Academic medical centers, Community hospitals, and Private practice environments.
- Validate the AIDA method’s performance across different clinical contexts.
- Assess the generalizability and robustness of the classification system.
- Implement sophisticated machine learning techniques to enhance understanding of complex classification scenarios.
- Develop advanced algorithms for handling partial parameter classifications.
- Explore integration of additional geometric and clinical parameters.
- Investigate machine learning approaches capable of capturing subtle parameter interactions.
- Develop more nuanced risk stratification methodologies.
- Assess the real-world implementation of the AIDA decision support system
- Conduct prospective studies analyzing modifications in clinical decision-making processes, impact on cesarean delivery rates, and maternal and fetal health outcomes.
- Evaluate the system’s potential to reduce unnecessary interventions.
- Compare AIDA-guided management with standard care approaches.
- Investigate long-term clinical implications of AI-assisted labor management.
- Conduct comprehensive cost-effectiveness analyses.
- Compare AIDA-guided interventions with traditional management strategies.
- Assess economic implications across diverse healthcare settings.
- Analyze direct medical costs, potential reduction in unnecessary interventions, and long-term healthcare resource utilization.
- Develop economic models incorporating the AIDA decision support system.
- Investigate AIDA’s performance across diverse patient populations.
- Assess potential for reducing healthcare disparities.
- Evaluate and mitigate potential algorithmic biases.
- Conduct detailed analyses of performance across different demographic groups, potential systemic biases in parameter classification, and equitable application of the decision support system.
- Develop strategies to ensure fair and unbiased AI-assisted clinical decision-making.
- Collecting a sufficiently large sample of cases in AIDA classes 1 and 2.
- Developing advanced model interpretation techniques.
- Providing a more comprehensive analysis of intermediate classification scenarios.
- Overcoming the limitations of the initial retrospective study’s small sample size.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ACOG | American College of Obstetricians and Gynecologists |
| AD | Asynclitism Degree |
| AI | Artificial Intelligence |
| AIDA | Artificial Intelligence Dystocia Algorithm |
| AoP | Angle of Progression |
| AUC | Area Under Curve |
| BMI | Body Mass Index |
| CI | Confidence Interval |
| CSP | Cavum Septum Pellucidum |
| DT | Decision Tree |
| FN | False Negative |
| FP | False Positive |
| HSD | Head-Symphysis Distance |
| ICD | Intrapartum Cesarean Delivery |
| ISUOG | International Society of Ultrasound in Obstetrics and Gynecology |
| IU | Intrapartum Ultrasound |
| LOT | Left Occiput Transverse |
| MLA | Midline Angle |
| MLP | Multi-Layer Perceptron |
| NPV | Negative Predictive Value |
| OAP | Occiput Anterior Position |
| OPP | Occiput Posterior Position |
| OTP | Occiput Transverse Position |
| OVD | Operative Vaginal Delivery |
| PPV | Positive Predictive Value |
| RF | Random Forest |
| ROC | Receiver Operating Characteristic |
| ROT | Right Occiput Transverse |
| SVM | Support Vector Machine |
| TN | True Negative |
| TP | True Positive |
| XAI | Explainable Artificial Intelligence |
References
- American College of Obstetrics and Gynecology Committee on Practice Bulletins-Obstetrics. ACOG Practice Bulletin Number 49, December 2003: Dystocia and augmentation of labor. Obstet. Gynecol. 2003, 102, 1445–1454. [Google Scholar] [CrossRef] [PubMed]
- Friedman, E. The graphic analysis of labor. Am. J. Obstet. Gynecol. 1954, 68, 1568–1575. [Google Scholar] [CrossRef] [PubMed]
- Usman, S.; Hanidu, A.; Kovalenko, M.; Hassan, W.A.; Lees, C. The sonopartogram. Am. J. Obstet. Gynecol. 2023, 228, S997–S1016. [Google Scholar] [CrossRef]
- Cahill, A.G.; Raghuraman, N.; Gandhi, M.; Kaimal, A.J. First and Second Stage Labor Management: ACOG Clinical Practice Guideline No. 8. Obstet. Gynecol. 2024, 143, 144–162. [Google Scholar] [CrossRef]
- Yano, E.; Sayama, S.; Iriyama, T.; Ariyoshi, Y.; Akiba, N.; Ichinose, M.; Toshimitsu, M.; Seyama, T.; Kumasawa, K.; Nakayama, T.; et al. Prediction of spontaneous vaginal delivery in the prolonged second stage using the delta angle of progression. Am. J. Obstet. Gynecol. MFM 2024, 6, 101403. [Google Scholar] [CrossRef]
- Iversen, J.K.; Kahrs, B.H.; Eggebø, T.M. There are 4, not 7, cardinal movements in labor. Am. J. Obstet. Gynecol. MFM 2021, 3, 100436. [Google Scholar] [CrossRef]
- Kamel, R.; Negm, S.; Badr, I.; Kahrs, B.H.; Eggebø, T.M.; Iversen, J.K. Fetal head descent assessed by transabdominal ultrasound: A prospective observational study. Am. J. Obstet. Gynecol. 2022, 226, 112.e1–112.e10. [Google Scholar] [CrossRef]
- Eggebø, T.M.; Hjartardottir, H. Descent of the presenting part assessed with ultrasound. Am. J. Obstet. Gynecol. 2024, 230, S901–S912. [Google Scholar] [CrossRef]
- Skinner, S.M.; Giles-Clark, H.J.; Higgins, C.; Mol, B.W.; Rolnik, D.L. Prognostic accuracy of ultrasound measures of fetal head descent to predict outcome of operative vaginal birth: A comparative systematic review and meta-analysis. Am. J. Obstet. Gynecol. 2023, 229, 10–22.e10. [Google Scholar] [CrossRef]
- Rizzo, G.; Mattioli, C.; Mappa, I.; Bitsadze, V.; Khizroeva, J.; Makatsariya, A.; D’Antonio, F. Antepartum ultrasound prediction of failed vacuum-assisted operative delivery: A prospective cohort study. J. Matern. Fetal Neonatal Med. 2021, 34, 3323–3329. [Google Scholar] [CrossRef]
- Mappa, I.; Tartaglia, S.; Maqina, P.; Makatsariya, A.; Ghi, T.; Rizzo, G.; D’Antonio, F. Ultrasound vs routine care before instrumental vaginal delivery: A systematic review and meta-analysis. Acta Obstet. Gynecol. Scand. 2021, 100, 1941–1948. [Google Scholar] [CrossRef] [PubMed]
- Pilliod, R.A.; Caughey, A.B. Fetal Malpresentation and Malposition: Diagnosis and Management. Obstet. Gynecol. Clin. N. Am. 2017, 44, 631–643. [Google Scholar] [CrossRef] [PubMed]
- Malvasi, A.; Raimondo, P.; Beck, R.; Tinelli, A.; Kuczkowski, K.M. Intrapartum ultrasound monitoring of malposition and malrotation during labor neuraxial analgesia: Maternal outcomes. J. Matern. Fetal Neonatal Med. 2020, 33, 3584–3590. [Google Scholar] [CrossRef]
- Malvasi, A.; Barbera, A.; Di Vagno, G.; Gimovsky, A.; Berghella, V.; Ghi, T.; Di Renzo, G.C.; Tinelli, A. Asynclitism: A literature review of an often forgotten clinical condition. J. Matern. Fetal Neonatal Med. 2015, 28, 1890–1894. [Google Scholar] [CrossRef]
- Bellussi, F.; Livi, A.; Cataneo, I.; Salsi, G.; Lenzi, J.; Pilu, G. Sonographic diagnosis of fetal head deflexion and the risk of cesarean delivery. Am. J. Obstet. Gynecol. MFM 2020, 2, 100217. [Google Scholar] [CrossRef]
- Malvasi, A.; Giacci, F.; Gustapane, S.; Sparic, R.; Barbera, A.; Tinelli, A. Intrapartum sonographic signs: New diagnostic tools in malposition and malrotation. J. Matern. Fetal Neonatal Med. 2016, 29, 2408–2413. [Google Scholar] [CrossRef] [PubMed]
- Foggin, H.H.; Albert, A.Y.; Minielly, N.C.; Lisonkova, S.; Koenig, N.A.; Jacobs, E.N.; Cundiff, G.W. Labor and delivery outcomes by delivery method in term deliveries in occiput posterior position: A population-based retrospective cohort study. AJOG Glob. Rep. 2022, 2, 100080. [Google Scholar] [CrossRef]
- Tempest, N.; Lane, S.; Hapangama, D.; UK Audit Ressearch Trainee Collaborative in Obstetrics, Gynecology (UK-ARCOG). Babies in occiput posterior position are significantly more likely to require an emergency cesarean birth compared with babies in occiput transverse position in the second stage of labor: A prospective observational study. Acta Obstet. Gynecol. Scand. 2020, 99, 537–545. [Google Scholar] [CrossRef]
- Wiafe, Y.A.; Whitehead, B.; Venables, H.; Dassah, E.T. Comparing intrapartum ultrasound and clinical examination in the assessment of fetal head position in African women. J. Ultrason. 2019, 19, 249–254. [Google Scholar] [CrossRef]
- Barrowclough, J.; Kool, B.; Crowther, C. Fetal malposition in labour and health outcomes for women and their newborn infants: A retrospective cohort study. PLoS ONE 2022, 17, e0276406. [Google Scholar] [CrossRef]
- Phipps, H.; Hyett, J.A.; Graham, K.; Carseldine, W.J.; Tooher, J.; de Vries, B. Is there an association between sonographically determined occipito-transverse position in the second stage of labor and operative delivery? Acta Obstet. Gynecol. Scand. 2014, 93, 1018–1024. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Wang, H.; Jia, L.; Qing, W.; Li, F.; Zhou, J. The impact of stage of labor on adverse maternal and neonatal outcomes in multiparous women: A retrospective cohort study. BMC Pregnancy Childbirth 2020, 20, 596. [Google Scholar] [CrossRef] [PubMed]
- ACOG. Practice Bulletin No. 154: Operative Vaginal Delivery. Obstet. Gynecol. 2015, 126, e56–e65. [Google Scholar] [CrossRef] [PubMed]
- Bellussi, F.; Ghi, T.; Youssef, A.; Salsi, G.; Giorgetta, F.; Parma, D.; Simonazzi, G.; Pilu, G. The use of intrapartum ultrasound to diagnose malpositions and cephalic malpresentations. Am. J. Obstet. Gynecol. 2017, 217, 633–641. [Google Scholar] [CrossRef]
- Malvasi, A.; Gustapane, S.; Malvasi, M.; Vinciguerra, M.; Tinelli, A.; Beck, R. Semeiotics of Intrapartum Ultrasonography: New Diagnostic Sonographic Sign of Fetal Malpositions and Malrotations. In Intrapartum Ultrasonography for Labor Management: Labor, Delivery and Puerperium; Springer: Berlin/Heidelberg, Germany, 2021; pp. 251–273. ISBN 978-3-030-57594-6. [Google Scholar]
- Malvasi, A.; Stark, M.; Ghi, T.; Farine, D.; Guido, M.; Tinelli, A. Intrapartum sonography for fetal head asynclitism and transverse position: Sonographic signs and comparison of diagnostic performance between transvaginal and digital examination. J. Matern. Fetal Neonatal Med. 2012, 25, 508–512. [Google Scholar] [CrossRef]
- Chou, M.R.; Kreiser, D.; Taslimi, M.M.; Druzin, M.L.; El-Sayed, Y.Y. Vaginal versus ultrasound examination of fetal occiput position during the second stage of labor. Am. J. Obstet. Gynecol. 2004, 191, 521–524. [Google Scholar] [CrossRef]
- Zahalka, N.; Sadan, O.; Malinger, G.; Liberati, M.; Boaz, M.; Glezerman, M.; Rotmensch, S. Comparison of transvaginal sonography with digital examination and transabdominal sonography for the determination of fetal head position in the second stage of labor. Am. J. Obstet. Gynecol. 2005, 193, 381–386. [Google Scholar] [CrossRef]
- Ghi, T.; Eggebø, T.; Lees, C.; Kalache, K.; Rozenberg, P.; Youssef, A.; Salomon, L.J.; Tutschek, B. ISUOG Practice Guidelines: Intrapartum ultrasound. Ultrasound Obstet. Gynecol. 2018, 52, 128–139. [Google Scholar] [CrossRef]
- Mittal, P.; Verma, M.; Bachani, S. Correlation of Digital Vaginal Examination with Transabdominal Ultrasound to Assess Fetal Head Position during Active Labor. J. South Asian Fed. Obstet. Gynaecol. 2019, 11, 375–380. [Google Scholar] [CrossRef]
- Nizard, J.; Haberman, S.; Paltieli, Y.; Gonen, R.; Ohel, G.; Le Bourthe, Y.; Ville, Y. Determination of fetal head station and position during labor: A new technique that combines ultrasound and a position-tracking system. Am. J. Obstet. Gynecol. 2009, 200, 404.e1–404.e5. [Google Scholar] [CrossRef]
- Malvasi, A.; Bochicchio, M.; Vaira, L.; Longo, A.; Pacella, E.; Tinelli, A. The fetal head evaluation during labor in the occiput posterior position: The ESA (evaluation by simulation algorithm) approach. J. Matern. Fetal Neonatal Med. 2014, 27, 1151–1157. [Google Scholar] [CrossRef]
- Malvasi, A.; Malgieri, L.E.; Cicinelli, E.; Vimercati, A.; D’Amato, A.; Dellino, M.; Trojano, G.; Difonzo, T.; Beck, R.; Tinelli, A. Artificial Intelligence, Intrapartum Ultrasound and Dystocic Delivery: AIDA (Artificial Intelligence Dystocia Algorithm), a Promising Helping Decision Support System. J. Imaging 2024, 10, 107. [Google Scholar] [CrossRef]
- Malgieri, L.E. Ontologies, Machine Learning and Deep Learning in Obstetrics. In Practical Guide to Simulation in Delivery Room Emergencies; Cinnella, G., Beck, R., Malvasi, A., Eds.; Springer International Publishing: Cham, Switzerland, 2023; pp. 29–64. ISBN 978-3-031-10067-3. [Google Scholar]
- Malvasi, A.; Malgieri, L.E.; Cicinelli, E.; Vimercati, A.; Achiron, R.; Sparić, R.; D’Amato, A.; Baldini, G.M.; Dellino, M.; Trojano, G.; et al. AIDA (Artificial Intelligence Dystocia Algorithm) in Prolonged Dystocic Labor: Focus on Asynclitism Degree. J. Imaging 2024, 10, 194. [Google Scholar] [CrossRef] [PubMed]
- Malvasi, A.; Malgieri, L.E.; Stark, M.; Tinelli, A. Dystocia, Delivery, and Artificial Intelligence in Labor Management: Perspectives and Future Directions. J. Clin. Med. 2024, 13, 6410. [Google Scholar] [CrossRef] [PubMed]
- Malvasi, A.; Tinelli, A.; Brizzi, A.; Guido, M.; Laterza, F.; De Nunzio, G.; Bochicchio, M.; Ghi, T.; Stark, M.; Benhamou, D.; et al. Intrapartum sonography head transverse and asynclitic diagnosis with and without epidural analgesia initiated early during the first stage of labor. Eur. Rev. Med. Pharmacol. Sci. 2011, 15, 518–523. [Google Scholar] [PubMed]
- Hinkson, L.; Henrich, W.; Tutschek, B. Intrapartum ultrasound during rotational forceps delivery: A novel tool for safety, quality control, and teaching. Am. J. Obstet. Gynecol. 2021, 224, 93.e1–93.e7. [Google Scholar] [CrossRef]
- Rizzo, G.; Ghi, T.; Henrich, W.; Tutschek, B.; Kamel, R.; Lees, C.C.; Mappa, I.; Kovalenko, M.; Lau, W.; Eggebo, T.; et al. Ultrasound in labor: Clinical practice guideline and recommendation by the WAPM-World Association of Perinatal Medicine and the PMF-Perinatal Medicine Foundation. J. Perinat. Med. 2022, 50, 1007–1029. [Google Scholar] [CrossRef]




| MLA (°) | ID Patient | Delivery Outcome | AIDA MLA | AIDA AoP | AIDA SPD | AIDA AD | Predicted Outcome (SVM) | Predicted Outcome (RF) | Predicted Outcome (MLP) |
|---|---|---|---|---|---|---|---|---|---|
| AIDA Class 2 | |||||||||
| 76 | 116 | ICD | RED | GREEN | GREEN | RED | ICD | ICD | NOICD |
| 76 | 128 | NO ICD | RED | GREEN | GREEN | YELLOW | ICD | ICD | ICD |
| 77 | 76 | ICD | RED | GREEN | GREEN | RED | ICD | ICD | ICD |
| 82 | 65 | ICD | RED | GREEN | RED | GREEN | ICD | ICD | ICD |
| AIDA Class 3 | |||||||||
| 75 | 110 | ICD | RED | RED | GREEN | RED | ICD | ICD | ICD |
| 77 | 12 | ICD | RED | RED | RED | GREEN | ICD | ICD | ICD |
| 77 | 50 | ICD | RED | RED | RED | GREEN | ICD | ICD | ICD |
| 78 | 7 | ICD | RED | RED | RED | GREEN | ICD | ICD | ICD |
| 81 | 9 | ICD | RED | RED | RED | GREEN | ICD | ICD | ICD |
| 81 | 63 | ICD | RED | RED | RED | GREEN | ICD | ICD | ICD |
| 84 | 10 | ICD | RED | RED | RED | GREEN | ICD | ICD | ICD |
| 86 | 24 | NO ICD | RED | RED | RED | GREEN | ICD | ICD | ICD |
| 86 | 11 | ICD | RED | RED | RED | GREEN | ICD | ICD | ICD |
| 88 | 94 | ICD | RED | RED | RED | GREEN | ICD | ICD | ICD |
| 88 | 20 | ICD | RED | RED | RED | GREEN | ICD | ICD | ICD |
| 88 | 43 | ICD | RED | RED | RED | GREEN | ICD | ICD | ICD |
| 88 | 118 | ICD | RED | RED | RED | GREEN | ICD | ICD | ICD |
| 88 | 52 | ICD | RED | RED | RED | GREEN | ICD | ICD | ICD |
| 90 | 46 | ICD | RED | RED | RED | GREEN | ICD | ICD | ICD |
| 90 | 28 | ICD | RED | RED | RED | GREEN | ICD | ICD | ICD |
| AIDA Class 4 | |||||||||
| 75 | 18 | ICD | RED | RED | RED | RED | ICD | ICD | ICD |
| 78 | 71 | ICD | RED | RED | RED | RED | ICD | ICD | ICD |
| 79 | 85 | ICD | RED | RED | RED | RED | ICD | ICD | ICD |
| 79 | 60 | ICD | RED | RED | RED | YELLOW | ICD | ICD | ICD |
| 81 | 4 | ICD | RED | RED | RED | YELLOW | ICD | ICD | ICD |
| 83 | 83 | ICD | RED | RED | RED | RED | ICD | ICD | ICD |
| 84 | 13 | ICD | RED | RED | RED | YELLOW | ICD | ICD | ICD |
| 87 | 114 | ICD | RED | RED | RED | RED | ICD | ICD | ICD |
| 89 | 78 | ICD | RED | RED | RED | RED | ICD | ICD | ICD |
| MLA (°) | ID Patient | Delivery Outcome | AIDA MLA | AIDA AoP | AIDA SPD | AIDA AD | Predicted Outcome (SVM) | Predicted Outcome (RF) | Predicted Outcome (MLP) |
|---|---|---|---|---|---|---|---|---|---|
| AIDA Class 2 | |||||||||
| 71 | 101 | ICD | RED | GREEN | GREEN | RED | ICD | ICD | ICD |
| 72 | 8 | ICD | RED | RED | GREEN | GREEN | ICD | ICD | ICD |
| 73 | 91 | ICD | RED | GREEN | GREEN | RED | ICD | ICD | ICD |
| AIDA Class 3 | |||||||||
| 70 | 42 | ICD | RED | RED | RED | GREEN | ICD | ICD | ICD |
| 71 | 26 | ICD | RED | RED | RED | GREEN | ICD | ICD | ICD |
| 72 | 51 | ICD | RED | RED | RED | GREEN | ICD | ICD | ICD |
| AIDA Class 4 | |||||||||
| 70 | 122 | ICD | RED | RED | RED | RED | ICD | ICD | ICD |
| 74 | 69 | ICD | RED | RED | RED | YELLOW | ICD | ICD | ICD |
| 74 | 84 | ICD | RED | RED | RED | RED | ICD | ICD | ICD |
| MLA (°) | ID Patient | Delivery Outcome | AIDA MLA | AIDA AoP | AIDA SPD | AIDA AD | Predicted Outcome (SVM) | Predicted Outcome (RF) | Predicted Outcome (MLP) |
|---|---|---|---|---|---|---|---|---|---|
| AIDA Class 0 | |||||||||
| 60 | 104 | NO ICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| AIDA Class 1 | |||||||||
| 64 | 53 | ICD | RED | GREEN | GREEN | GREEN | ICD | NOICD | ICD |
| 67 | 112 | NO ICD | RED | GREEN | GREEN | GREEN | NOICD | NOICD | ICD |
| AIDA Class 2 | |||||||||
| 64 | 25 | ICD | RED | GREEN | RED | GREEN | ICD | ICD | ICD |
| 66 | 113 | ICD | RED | GREEN | RED | GREEN | NOICD | ICD | NOICD |
| 68 | 55 | ICD | RED | RED | GREEN | GREEN | ICD | ICD | ICD |
| AIDA Class 3 | |||||||||
| 61 | 44 | ICD | YELLOW | RED | RED | GREEN | ICD | ICD | ICD |
| 61 | 57 | ICD | YELLOW | RED | RED | GREEN | ICD | ICD | ICD |
| 64 | 115 | NO ICD | RED | RED | GREEN | RED | ICD | NOICD | ICD |
| 64 | 33 | ICD | RED | RED | RED | GREEN | ICD | ICD | ICD |
| 67 | 77 | ICD | RED | RED | RED | GREEN | ICD | ICD | ICD |
| 67 | 100 | NO ICD | RED | RED | GREEN | RED | ICD | ICD | ICD |
| 67 | 39 | ICD | RED | RED | RED | GREEN | ICD | ICD | ICD |
| 68 | 126 | ICD | RED | RED | GREEN | RED | ICD | ICD | ICD |
| 68 | 64 | ICD | RED | RED | RED | GREEN | ICD | ICD | ICD |
| 68 | 29 | ICD | RED | RED | RED | GREEN | ICD | ICD | ICD |
| 69 | 96 | ICD | RED | RED | RED | GREEN | ICD | ICD | ICD |
| 69 | 99 | ICD | RED | GREEN | RED | RED | ICD | ICD | ICD |
| 69 | 135 | ICD | RED | RED | GREEN | RED | ICD | ICD | NOICD |
| AIDA Class 4 | |||||||||
| 61 | 2 | ICD | YELLOW | RED | RED | YELLOW | ICD | ICD | ICD |
| 64 | 74 | ICD | RED | RED | RED | RED | ICD | ICD | ICD |
| 65 | 93 | ICD | RED | RED | RED | RED | ICD | ICD | NOICD |
| 65 | 102 | ICD | RED | RED | RED | RED | ICD | ICD | ICD |
| 66 | 22 | ICD | RED | RED | RED | RED | ICD | ICD | ICD |
| 66 | 121 | ICD | RED | RED | RED | RED | ICD | ICD | ICD |
| 67 | 117 | ICD | RED | RED | RED | RED | ICD | ICD | ICD |
| 68 | 70 | ICD | RED | RED | RED | YELLOW | ICD | ICD | ICD |
| 68 | 67 | ICD | RED | RED | RED | RED | ICD | ICD | ICD |
| AIDA Class | Delivery Outcome | MLA ≥ 75° | MLA ≥ 70° <75° | MLA ≥ 60° <70° | AIDA Class Total |
|---|---|---|---|---|---|
| AIDA Class 0 | OPERATIVE VD | 1 | 1 | ||
| AIDA Class 1 | ICD | 1 | 2 | ||
| SPONTANEOUS | 1 | ||||
| AIDA Class 2 | ICD | 2 | 2 | 2 | 10 |
| ICD AFTER FAILURE | 1 | 1 | 1 | ||
| OPERATIVE VD | 1 | ||||
| AIDA Class 3 | ICD | 12 | 3 | 8 | 32 |
| ICD AFTER FAILURE | 3 | 3 | |||
| OPERATIVE VD | 1 | 2 | |||
| AIDA Class 4 | ICD | 7 | 2 | 9 | 21 |
| ICD AFTER FAILURE | 2 | 1 | |||
| TOTAL | 29 | 9 | 28 | 66 |
| Algorithm | Accuracy (95% CI) | Sensitivity | Specificity | PPV | NPV | F1 Score | AUC |
|---|---|---|---|---|---|---|---|
| Random Forest | 0.955 (0.91–0.98) | 0.97 | 0.92 | 0.94 | 0.96 | 0.95 | 0.97 |
| SVM | 0.933 (0.88–0.97) | 0.94 | 0.89 | 0.91 | 0.93 | 0.93 | 0.95 |
| MLP | 0.897 (0.84–0.94) | 0.91 | 0.85 | 0.88 | 0.89 | 0.89 | 0.92 |
| Method | Accuracy | Sensitivity | Specificity | Study |
|---|---|---|---|---|
| Digital Examination Alone | 65–75% | Variable | Variable | Literature Review |
| Single Parameter US (AoP only) | 78–85% | 80–90% | 70–80% | Previous Studies |
| AIDA (4 parameters) | 93–97% | 95–98% | 88–94% | Current Study |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malvasi, A.; Malgieri, L.E.; Difonzo, T.; Achiron, R.; Tinelli, A.; Baldini, G.M.; Vasciaveo, L.; Beck, R.; Mappa, I.; Rizzo, G. Artificial Intelligence Dystocia Algorithm (AIDA) as a Decision Support System in Transverse Fetal Head Position. J. Imaging 2025, 11, 223. https://doi.org/10.3390/jimaging11070223
Malvasi A, Malgieri LE, Difonzo T, Achiron R, Tinelli A, Baldini GM, Vasciaveo L, Beck R, Mappa I, Rizzo G. Artificial Intelligence Dystocia Algorithm (AIDA) as a Decision Support System in Transverse Fetal Head Position. Journal of Imaging. 2025; 11(7):223. https://doi.org/10.3390/jimaging11070223
Chicago/Turabian StyleMalvasi, Antonio, Lorenzo E. Malgieri, Tommaso Difonzo, Reuven Achiron, Andrea Tinelli, Giorgio Maria Baldini, Lorenzo Vasciaveo, Renata Beck, Ilenia Mappa, and Giuseppe Rizzo. 2025. "Artificial Intelligence Dystocia Algorithm (AIDA) as a Decision Support System in Transverse Fetal Head Position" Journal of Imaging 11, no. 7: 223. https://doi.org/10.3390/jimaging11070223
APA StyleMalvasi, A., Malgieri, L. E., Difonzo, T., Achiron, R., Tinelli, A., Baldini, G. M., Vasciaveo, L., Beck, R., Mappa, I., & Rizzo, G. (2025). Artificial Intelligence Dystocia Algorithm (AIDA) as a Decision Support System in Transverse Fetal Head Position. Journal of Imaging, 11(7), 223. https://doi.org/10.3390/jimaging11070223










