Incorporation of Superparamagnetic Magnetic–Fluorescent Iron Oxide Nanoparticles Increases Proliferation of Human Mesenchymal Stem Cells
Abstract
1. Introduction
2. Materials and Methods
2.1. Cell Isolation and Characterization
2.2. Characterization of MIRB NPs
2.3. Labeling of Cells with MIRB
2.4. Internalization of MIRB in hADSCs
2.5. Evaluation of Labeling Efficacy
2.6. Effect of MIRB on Viability
2.7. Quantification of hADSCs
2.8. Differentiation Potential of hADSCs
2.8.1. Adipogenic Differentiation
2.8.2. Osteogenic Differentiation
2.8.3. Chondrogenic Differentiation
2.9. Immunocytochemistry
2.10. Statistical Analysis
3. Results
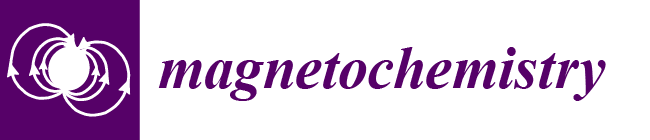
3.1. Characterization of MIRB Nanoparticles
3.2. Characterization of hADSCs in Flow Cytometry
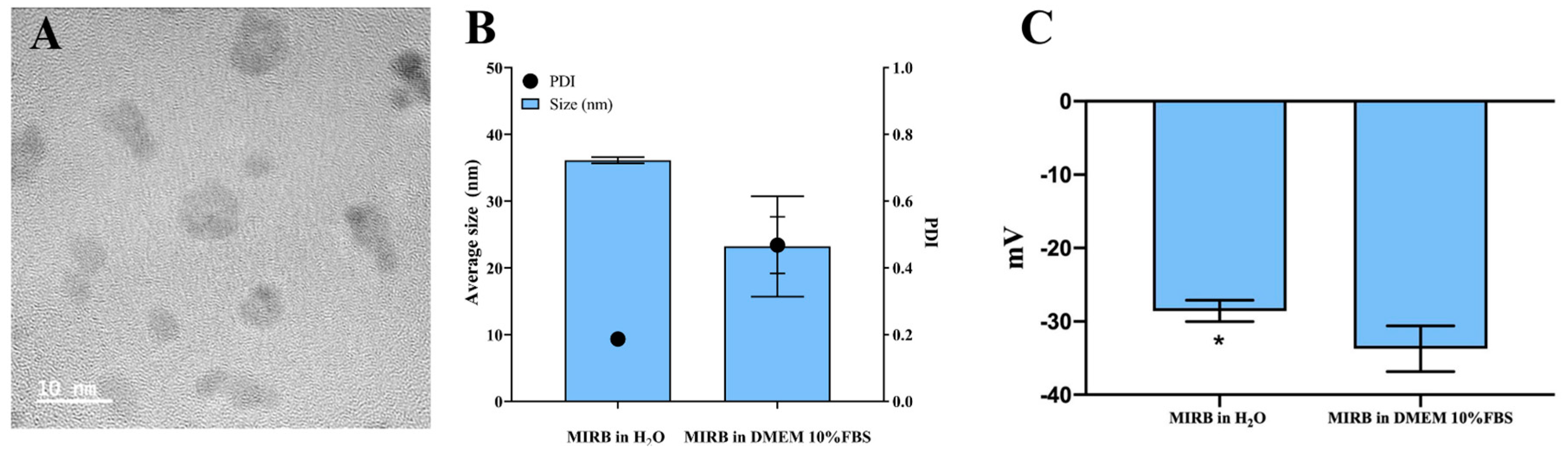
3.3. Labeling and Internalization of MIRB
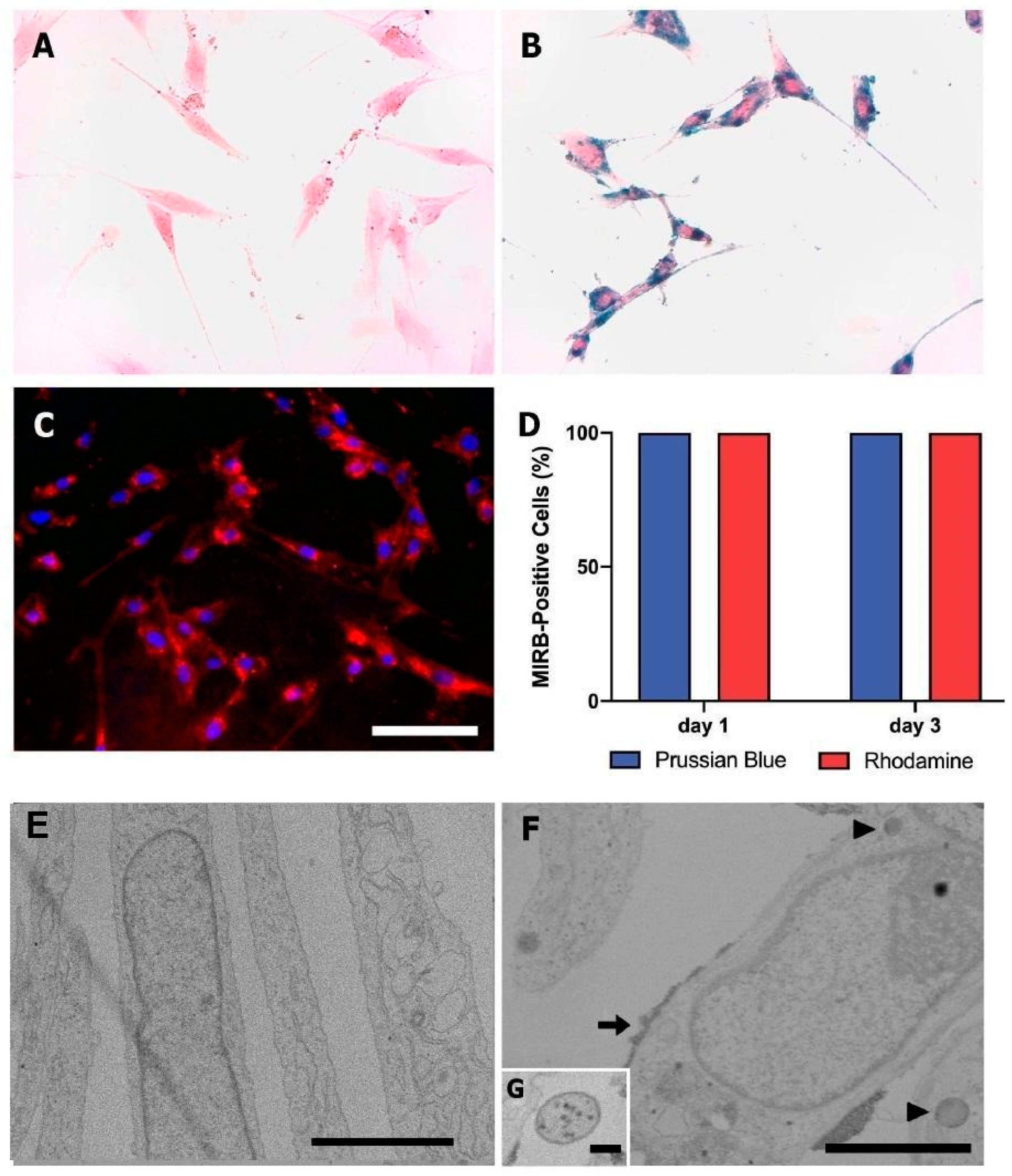
3.4. Cellular Viability
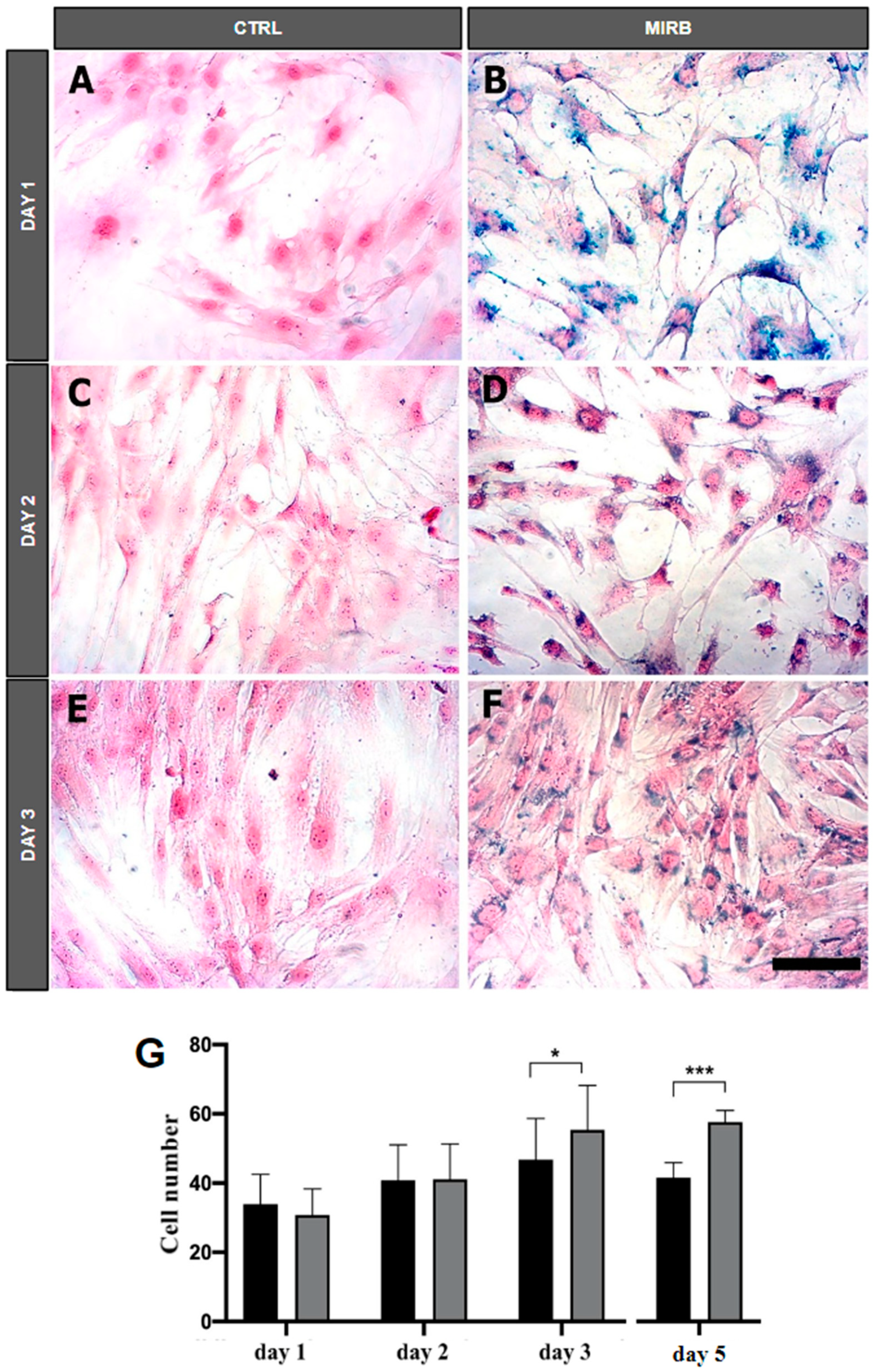
3.5. Quantification of hADSCs after Treatment with MIRB
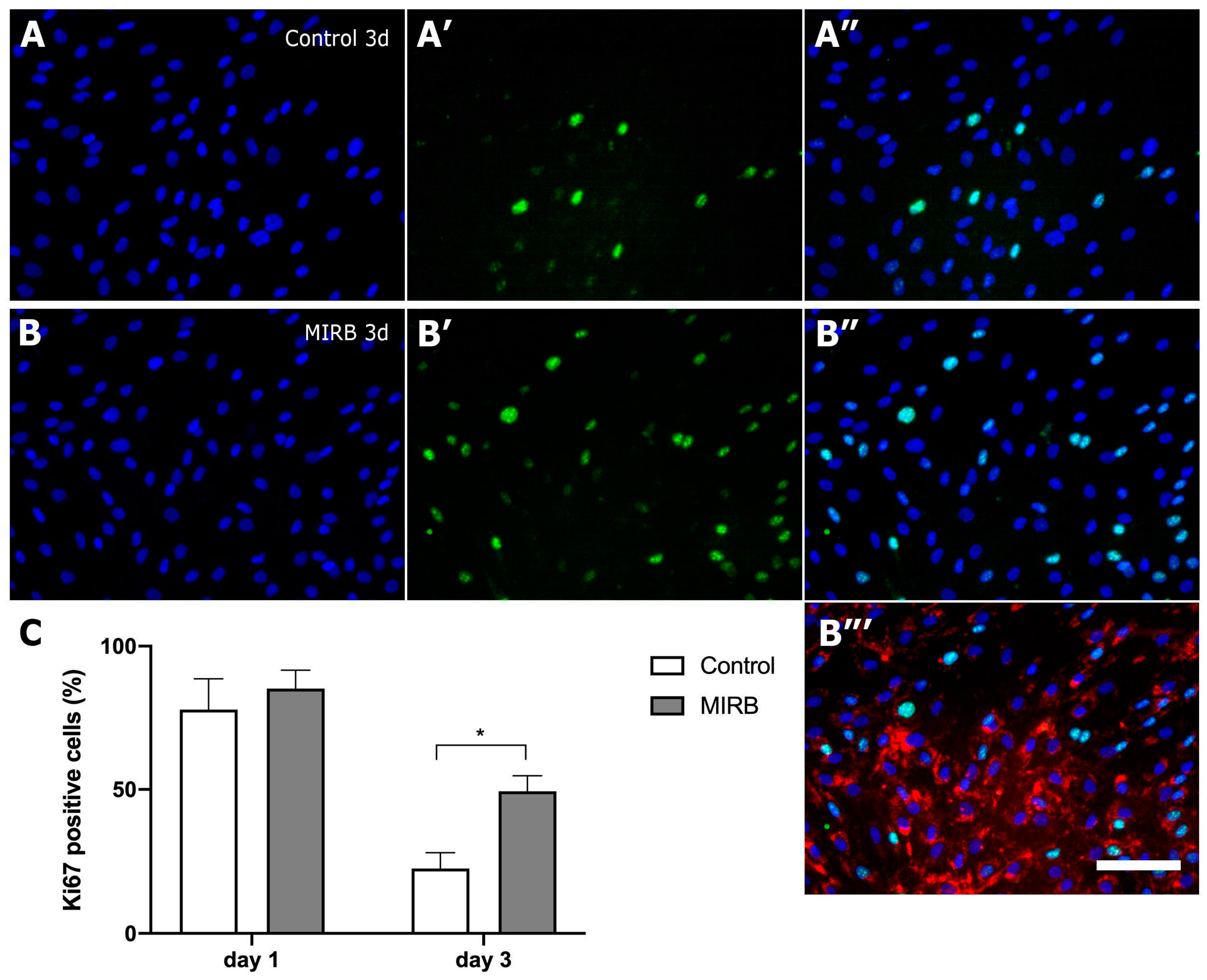
3.6. Proliferation of hADSCs after Exposure to MIRB
3.7. Differentiation Potential of hADSCs
3.7.1. Adipogenic Differentiation
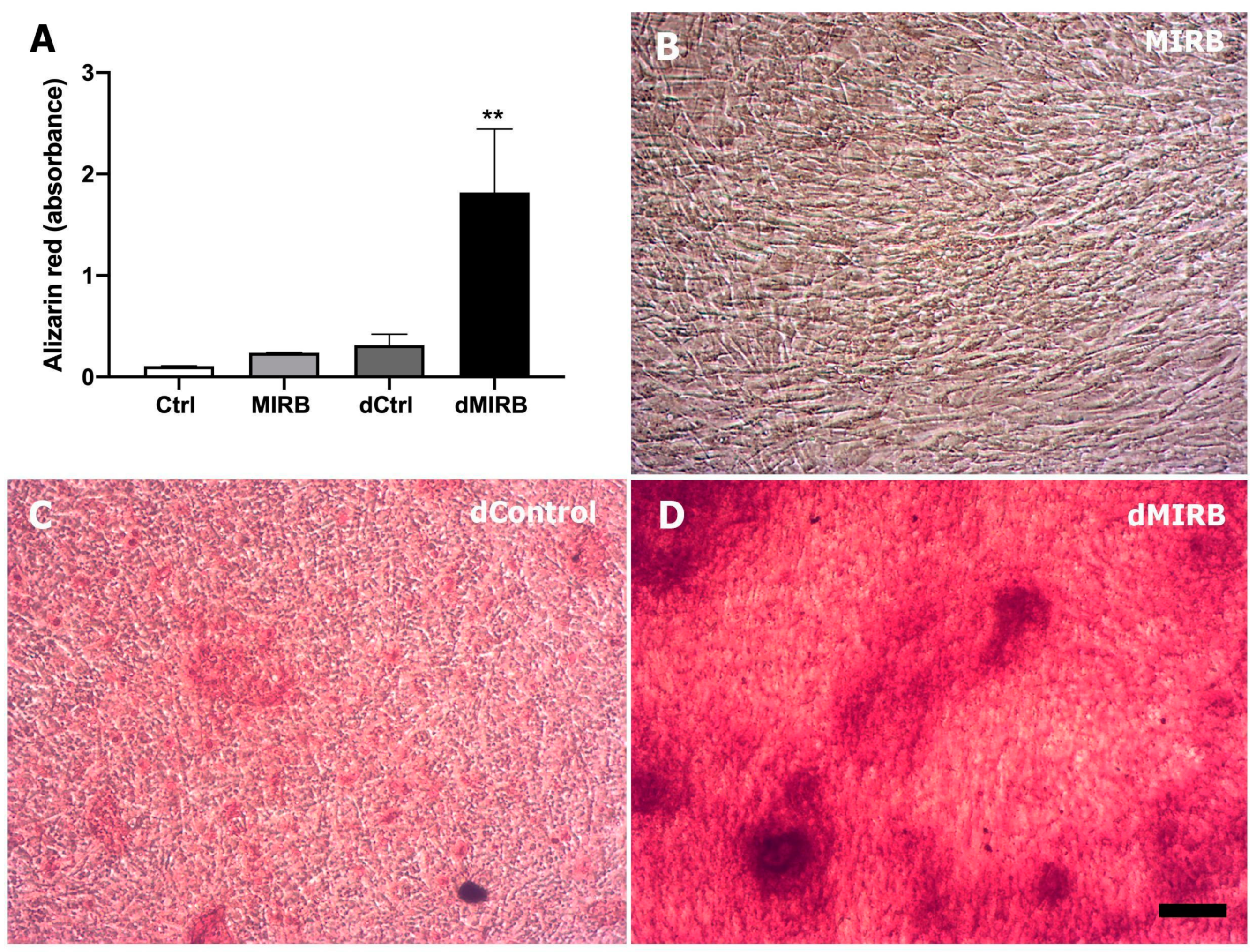
3.7.2. Osteogenic Differentiation
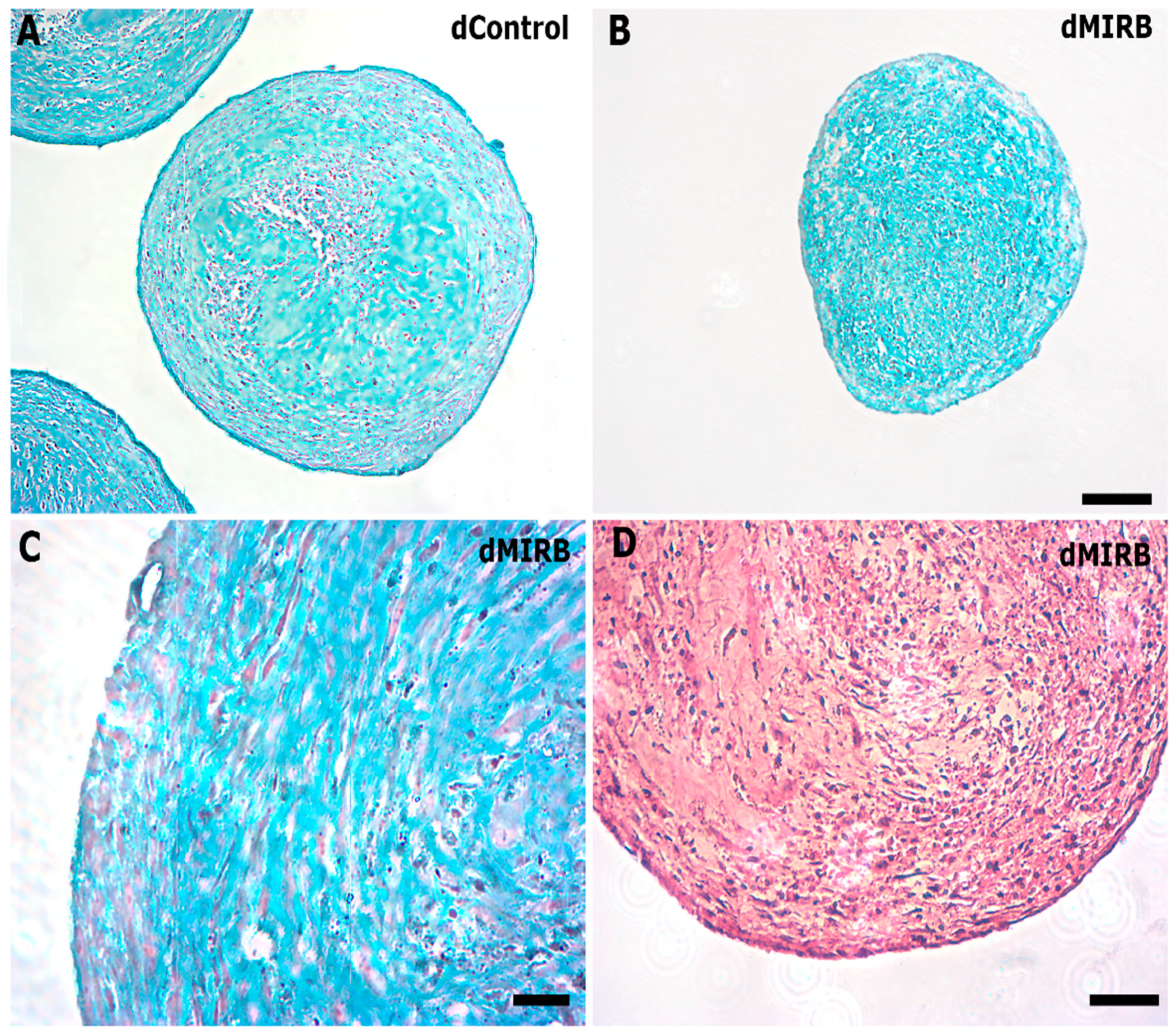
3.7.3. Chondrogenic Differentiation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zou, M.; Liu, S.; Sun, Z.; Wu, J.; Yuan, Z.; Teng, Y.; Feng, Y.; Yuan, F. Insights into the Role of Adipose-derived Stem Cells: Wound Healing and Clinical Regenerative Potential. J. Cell Physiol. 2021, 236, 2290–2297. [Google Scholar] [CrossRef] [PubMed]
- Mizuno, H. Adipose-Derived Stem Cells for Regenerative Medicine in the Field of Plastic and Reconstructive Surgery. J. Oral Biosci. 2013, 55, 132–136. [Google Scholar] [CrossRef]
- Bacakova, L.; Zarubova, J.; Travnickova, M.; Musilkova, J.; Pajorova, J.; Slepicka, P.; Kasalkova, N.S.; Svorcik, V.; Kolska, Z.; Motarjemi, H.; et al. Stem Cells: Their Source, Potency and Use in Regenerative Therapies with Focus on Adipose-Derived Stem Cells—A Review. Biotechnol. Adv. 2018, 36, 1111–1126. [Google Scholar] [CrossRef] [PubMed]
- Mun, C.H.; Kang, M.-I.; Shin, Y.D.; Kim, Y.; Park, Y.-B. The Expression of Immunomodulation-Related Cytokines and Genes of Adipose- and Bone Marrow-Derived Human Mesenchymal Stromal Cells from Early to Late Passages. Tissue Eng. Regen. Med. 2018, 15, 771–779. [Google Scholar] [CrossRef]
- Gomez-Salazar, M.; Gonzalez-Galofre, Z.N.; Casamitjana, J.; Crisan, M.; James, A.W.; Péault, B. Five Decades Later, Are Mesenchymal Stem Cells Still Relevant? Front. Bioeng. Biotechnol. 2020, 8, 148. [Google Scholar] [CrossRef] [PubMed]
- Vissers, C.; Ming, G.; Song, H. Nanoparticle Technology and Stem Cell Therapy Team up against Neurodegenerative Disorders. Adv. Drug Deliv. Rev. 2019, 148, 239–251. [Google Scholar] [CrossRef]
- Kappes, M.; Friedrich, B.; Pfister, F.; Huber, C.; Friedrich, R.P.; Stein, R.; Braun, C.; Band, J.; Schreiber, E.; Alexiou, C.; et al. Superparamagnetic Iron Oxide Nanoparticles for Targeted Cell Seeding: Magnetic Patterning and Magnetic 3D Cell Culture. Adv. Funct. Mater. 2022, 32, 2203672. [Google Scholar] [CrossRef]
- Dadfar, S.M.; Camozzi, D.; Darguzyte, M.; Roemhild, K.; Varvarà, P.; Metselaar, J.; Banala, S.; Straub, M.; Güvener, N.; Engelmann, U. Size-Isolation of Superparamagnetic Iron Oxide Nanoparticles Improves MRI, MPI and Hyperthermia Performance. J. Nanobiotechnol. 2020, 18, 22. [Google Scholar] [CrossRef]
- Labusca, L.; Herea, D.D.; Minuti, A.E.; Stavila, C.; Danceanu, C.; Grigoras, M.; Ababei, G.; Chiriac, H.; Lupu, N. Magnetic Nanoparticle Loaded Human Adipose Derived Mesenchymal Cells Spheroids in Levitated Culture. J. Biomed. Mater. Res. Part B Appl. Biomater. 2021, 109, 630–642. [Google Scholar] [CrossRef]
- Gnanadevi, R.; Ramesh, G.; Thandavan Arthanari, K.; William, J. In Vitro Internalization of Moldey Ion Rhodamine B in Ovine Mesenchymal Stem Cell: A Comparative Study. J. Entomol. Zool. Stud. 2019, 7, 747–749. [Google Scholar]
- Zhang, N.; Xu, L.; Song, H.; Bu, C.; Kang, J.; Zhang, C.; Yang, X.; Han, F. Tracking of Stem Cells from Human Exfoliated Deciduous Teeth Labeled with Molday ION Rhodamine-B during Periodontal Bone Regeneration in Rats. Int. J. Stem Cells 2022, 16, 93–107. [Google Scholar] [CrossRef]
- Gnanadevi, R.G.; Ramesh, G.; Kannan, T.A.; William, B.J.; Parthiban, M.; Sathyan, G. Labelling of Ovine Adipose-Derived Mesenchymal Stem Cells (oADMSCs) and Tracking Using MRI Technique. Maced. Vet. Rev. 2017, 40, 137–142. [Google Scholar] [CrossRef]
- Azevedo-Pereira, R.L.; Rangel, B.; Tovar-Moll, F.; Gasparetto, E.L.; Attias, M.; Zaverucha-do-Valle, C.; Mendez-Otero, R. Superparamagnetic Iron Oxide Nanoparticles as a Tool to Track Mouse Neural Stem Cells in Vivo. Mol. Biol. Rep. 2019, 46, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Jasmin; Souza, G.T.; Andrade Louzada, R.; Rosado-de-Castro, P.H.; Mendez-Otero, R.; Carvalho, A.C.C. Tracking Stem Cells with Superparamagnetic Iron Oxide Nanoparticles: Perspectives and Considerations. IJN 2017, 12, 779–793. [Google Scholar] [CrossRef] [PubMed]
- Charles-de-Sá, L.; Gontijo-de-Amorim, N.F.; Rigotti, G.; Sbarbati, A.; Bernardi, P.; Benati, D.; Bizon Vieira Carias, R.; Maeda Takiya, C.; Borojevic, R. Photoaged Skin Therapy with Adipose-Derived Stem Cells. Plast. Reconstr. Surg. 2020, 145, 1037e. [Google Scholar] [CrossRef] [PubMed]
- Miyaki, L.A.M.; Sibov, T.T.; Pavon, L.F.; Mamani, J.B.; Gamarra, L.F. Study of Internalization and Viability of Multimodal Nanoparticles for Labeling of Human Umbilical Cord Mesenchymal Stem Cells. Einstein 2012, 10, 189–196. [Google Scholar] [CrossRef]
- Dominici, M.; Le Blanc, K.; Mueller, I.; Slaper-Cortenbach, I.; Marini, F.C.; Krause, D.S.; Deans, R.J.; Keating, A.; Prockop, D.J.; Horwitz, E.M. Minimal Criteria for Defining Multipotent Mesenchymal Stromal Cells. The International Society for Cellular Therapy Position Statement. Cytotherapy 2006, 8, 315–317. [Google Scholar] [CrossRef]
- Safi, M.; Courtois, J.; Seigneuret, M.; Conjeaud, H.; Berret, J.-F. The Effects of Aggregation and Protein Corona on the Cellular Internalization of Iron Oxide Nanoparticles. Biomaterials 2011, 32, 9353–9363. [Google Scholar] [CrossRef]
- Andrzejewska, A.; Jablonska, A.; Seta, M.; Dabrowska, S.; Walczak, P.; Janowski, M.; Lukomska, B. Labeling of Human Mesenchymal Stem Cells with Different Classes of Vital Stains: Robustness and Toxicity. Stem Cell Res. Ther. 2019, 10, 187. [Google Scholar] [CrossRef]
- Nan, H.; Huang, J.; Li, H.; Li, Q.; Liu, D. Assessment of Biological Characteristics of Adipose Tissue-Derived Stem Cells Co-Labeled with Molday ION Rhodamine BTM and Green Fluorescent Protein in Vitro. Mol. Med. Rep. 2013, 8, 1446–1452. [Google Scholar] [CrossRef]
- Addicott, B.; Willman, M.; Rodriguez, J.; Padgett, K.; Han, D.; Berman, D.; Hare, J.M.; Kenyon, N.S. Mesenchymal Stem Cell Labeling and in Vitro MR Characterization at 1.5 T of New SPIO Contrast Agent: Molday ION Rhodamine-BTM. Contrast Media Mol. Imaging 2011, 6, 7–18. [Google Scholar] [CrossRef] [PubMed]
- Dabrowska, S.; Del Fattore, A.; Karnas, E.; Frontczak-Baniewicz, M.; Kozlowska, H.; Muraca, M.; Janowski, M.; Lukomska, B. Imaging of Extracellular Vesicles Derived from Human Bone Marrow Mesenchymal Stem Cells Using Fluorescent and Magnetic Labels. Int. J. Nanomed. 2018, 13, 1653–1664. [Google Scholar] [CrossRef] [PubMed]
- Delling, U.; Brehm, W.; Metzger, M.; Ludewig, E.; Winter, K.; Jülke, H. In Vivo Tracking and Fate of Intra-Articularly Injected Superparamagnetic Iron Oxide Particle-Labeled Multipotent Stromal Cells in an Ovine Model of Osteoarthritis. Cell Transplant. 2015, 24, 2379–2390. [Google Scholar] [CrossRef]
- Ren, Z.; Wang, J.; Zou, C.; Guan, Y.; Zhang, Y.A. Labeling of Cynomolgus Monkey Bone Marrow-Derived Mesenchymal Stem Cells for Cell Tracking by Multimodality Imaging. Sci. China Life Sci. 2011, 54, 981–987. [Google Scholar] [CrossRef] [PubMed]
- Badman, R.P.; Moore, S.L.; Killian, J.L.; Feng, T.; Cleland, T.A.; Hu, F.; Wang, M.D. Dextran-Coated Iron Oxide Nanoparticle-Induced Nanotoxicity in Neuron Cultures. Sci. Rep. 2020, 10, 11239. [Google Scholar] [CrossRef]
- Cores, J.; Caranasos, T.G.; Cheng, K. Magnetically Targeted Stem Cell Delivery for Regenerative Medicine. J. Funct. Biomater. 2015, 6, 526–546. [Google Scholar] [CrossRef]
- Schäfer, R.; Kehlbach, R.; Wiskirchen, J.; Bantleon, R.; Pintaske, J.; Brehm, B.R.; Gerber, A.; Wolburg, H.; Claussen, C.D.; Northoff, H. Transferrin Receptor Upregulation: In Vitro Labeling of Rat Mesenchymal Stem Cells with Superparamagnetic Iron Oxide1. Radiology 2007, 244, 514–523. [Google Scholar] [CrossRef]
- Spira, D.; Bantleon, R.; Wolburg, H.; Schick, F.; Groezinger, G.; Wiskirchen, J.; Wiesinger, B. Labeling Human Melanoma Cells with SPIO: In Vitro Observations. Mol. Imaging 2016, 15, 1536012115624915. [Google Scholar] [CrossRef] [PubMed]
- Berg, J.M.; Romoser, A.; Banerjee, N.; Zebda, R.; Sayes, C.M. The Relationship between pH and Zeta Potential of ∼ 30 Nm Metal Oxide Nanoparticle Suspensions Relevant to in Vitro Toxicological Evaluations. Nanotoxicology 2009, 3, 276–283. [Google Scholar] [CrossRef]
- Zhang, Y.; Chen, Y.; Westerhoff, P.; Crittenden, J. Impact of Natural Organic Matter and Divalent Cations on the Stability of Aqueous Nanoparticles. Water Res. 2009, 43, 4249–4257. [Google Scholar] [CrossRef]
- Patravale, V.B.; Date, A.A.; Kulkarni, R.M. Nanosuspensions: A Promising Drug Delivery Strategy. J. Pharm. Pharmacol. 2004, 56, 827–840. [Google Scholar] [CrossRef] [PubMed]
- Sakulkhu, U.; Mahmoudi, M.; Maurizi, L.; Salaklang, J.; Hofmann, H. Protein Corona Composition of Superparamagnetic Iron Oxide Nanoparticles with Various Physico-Chemical Properties and Coatings. Sci. Rep. 2014, 4, 5020. [Google Scholar] [CrossRef] [PubMed]
- Walkey, C.D.; Chan, W.C.W. Understanding and Controlling the Interaction of Nanomaterials with Proteins in a Physiological Environment. Chem. Soc. Rev. 2012, 41, 2780–2799. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.K.; Choi, E.-J.; Webster, T.J.; Kim, S.-H.; Khang, D. Effect of the Protein Corona on Nanoparticles For Modulating Cytotoxicity and Immunotoxicity. IJN 2014, 10, 97–113. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, A.R.; Gemini-Piperni, S.; Travassos, R.; Lemgruber, L.; Silva, R.C.; Rossi, A.L.; Farina, M.; Anselme, K.; Shokuhfar, T.; Shahbazian-Yassar, R.; et al. Trojan-Like Internalization of Anatase Titanium Dioxide Nanoparticles by Human Osteoblast Cells. Sci. Rep. 2016, 6, 23615. [Google Scholar] [CrossRef]
- Moore, T.L.; Rodriguez-Lorenzo, L.; Hirsch, V.; Balog, S.; Urban, D.; Jud, C.; Rothen-Rutishauser, B.; Lattuada, M.; Petri-Fink, A. Nanoparticle Colloidal Stability in Cell Culture Media and Impact on Cellular Interactions. Chem. Soc. Rev. 2015, 44, 6287–6305. [Google Scholar] [CrossRef]
- Maiorano, G.; Sabella, S.; Sorce, B.; Brunetti, V.; Malvindi, M.A.; Cingolani, R.; Pompa, P.P. Effects of Cell Culture Media on the Dynamic Formation of Protein−Nanoparticle Complexes and Influence on the Cellular Response. ACS Nano 2010, 4, 7481–7491. [Google Scholar] [CrossRef]
- Arbab, A.S.; Yocum, G.T.; Kalish, H.; Jordan, E.K.; Anderson, S.A.; Khakoo, A.Y.; Read, E.J.; Frank, J.A. Efficient Magnetic Cell Labeling with Protamine Sulfate Complexed to Ferumoxides for Cellular MRI. Blood 2004, 104, 1217–1223. [Google Scholar] [CrossRef]
- Ma, L.; Li, M.-W.; Bai, Y.; Guo, H.-H.; Wang, S.-C.; Yu, Q. Biological Characteristics of Fluorescent Superparamagnetic Iron Oxide Labeled Human Dental Pulp Stem Cells. Stem Cells Int. 2017, 2017, 4837503. [Google Scholar] [CrossRef]
- Peng, C.; Yang, K.; Xiang, P.; Zhang, C.; Zou, L.; Wu, X.; Gao, Y.; Kang, Z.; He, K.; Liu, J.; et al. Effect of Transplantation with Autologous Bone Marrow Stem Cells on Acute Myocardial Infarction. Int. J. Cardiol. 2013, 162, 158–165. [Google Scholar] [CrossRef]
- Ghanbarei, S.; Sattarahmady, N.; Zarghampoor, F.; Azarpira, N.; Hossein-Aghdaie, M. Effects of Labeling Human Mesenchymal Stem Cells with Superparamagnetic Zinc–Nickel Ferrite Nanoparticles on Cellular Characteristics and Adipogenesis/Osteogenesis Differentiation. Biotechnol. Lett. 2021, 43, 1659–1673. [Google Scholar] [CrossRef] [PubMed]
- Huang, D.-M.; Hsiao, J.-K.; Chen, Y.-C.; Chien, L.-Y.; Yao, M.; Chen, Y.-K.; Ko, B.-S.; Hsu, S.-C.; Tai, L.-A.; Cheng, H.-Y.; et al. The Promotion of Human Mesenchymal Stem Cell Proliferation by Superparamagnetic Iron Oxide Nanoparticles. Biomaterials 2009, 30, 3645–3651. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, J.-K.; Tai, M.-F.; Chu, H.-H.; Chen, S.-T.; Li, H.; Lai, D.-M.; Hsieh, S.-T.; Wang, J.-L.; Liu, H.-M. Magnetic Nanoparticle Labeling of Mesenchymal Stem Cells without Transfection Agent: Cellular Behavior and Capability of Detection with Clinical 1.5 T Magnetic Resonance at the Single Cell Level. Magn. Reson. Med. Off. J. Int. Soc. Magn. Reson. Med. 2007, 58, 717–724. [Google Scholar] [CrossRef]
- Zare, S.; Mehrabani, D.; Jalli, R.; Saeedi Moghadam, M.; Manafi, N.; Mehrabani, G.; Jamhiri, I.; Ahadian, S. MRI-Tracking of Dental Pulp Stem Cells In Vitro and In Vivo Using Dextran-Coated Superparamagnetic Iron Oxide Nanoparticles. J. Clin. Med. 2019, 8, 1418. [Google Scholar] [CrossRef]
- Zhang, L.; Tan, S.; Liu, Y.; Xie, H.; Luo, B.; Wang, J. In Vitro Inhibition of Tumor Growth by Low-Dose Iron Oxide Nanoparticles Activating Macrophages. J. Biomater. Appl. 2019, 33, 935–945. [Google Scholar] [CrossRef] [PubMed]
- Botta, A.; Delteil, F.; Mettouchi, A.; Vieira, A.; Estrach, S.; Négroni, L.; Stefani, C.; Lemichez, E.; Meneguzzi, G.; Gagnoux-Palacios, L. Confluence Switch Signaling Regulates ECM Composition and the Plasmin Proteolytic Cascade in Keratinocytes. J. Cell Sci. 2012, 125, 4241–4252. [Google Scholar] [CrossRef]
- Jasmin; Torres, A.L.M.; Nunes, H.M.P.; Passipieri, J.A.; Jelicks, L.A.; Gasparetto, E.L.; Spray, D.C.; Campos de Carvalho, A.C.; Mendez-Otero, R. Optimized Labeling of Bone Marrow Mesenchymal Cells with Superparamagnetic Iron Oxide Nanoparticles and in Vivo Visualization by Magnetic Resonance Imaging. J. Nanobiotechnol. 2011, 9, 4. [Google Scholar] [CrossRef]
- Weis, C.; Blank, F.; West, A.; Black, G.; Woodward, R.C.; Carroll, M.R.J.; Mainka, A.; Kartmann, R.; Brandl, A.; Bruns, H.; et al. Labeling of Cancer Cells with Magnetic Nanoparticles for Magnetic Resonance Imaging. Magn. Reson. Med. 2014, 71, 1896–1905. [Google Scholar] [CrossRef]
- Mesentier-Louro, L.A.; Teixeira-Pinheiro, L.C.; Gubert, F.; Vasques, J.F.; Silva-Junior, A.J.; Chimeli-Ormonde, L.; Nascimento-dos-Santos, G.; Mendez-Otero, R.; Santiago, M.F. Long-Term Neuronal Survival, Regeneration, and Transient Target Reconnection after Optic Nerve Crush and Mesenchymal Stem Cell Transplantation. Stem Cell Res. Ther. 2019, 10, 121. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Becker, W.P.; Dáu, J.B.T.; Souza, W.d.; Mendez-Otero, R.; Carias, R.B.V.; Jasmin. Incorporation of Superparamagnetic Magnetic–Fluorescent Iron Oxide Nanoparticles Increases Proliferation of Human Mesenchymal Stem Cells. Magnetochemistry 2024, 10, 77. https://doi.org/10.3390/magnetochemistry10100077
Becker WP, Dáu JBT, Souza Wd, Mendez-Otero R, Carias RBV, Jasmin. Incorporation of Superparamagnetic Magnetic–Fluorescent Iron Oxide Nanoparticles Increases Proliferation of Human Mesenchymal Stem Cells. Magnetochemistry. 2024; 10(10):77. https://doi.org/10.3390/magnetochemistry10100077
Chicago/Turabian StyleBecker, Willian Pinheiro, Juliana Barbosa Torreão Dáu, Wanderson de Souza, Rosalia Mendez-Otero, Rosana Bizon Vieira Carias, and Jasmin. 2024. "Incorporation of Superparamagnetic Magnetic–Fluorescent Iron Oxide Nanoparticles Increases Proliferation of Human Mesenchymal Stem Cells" Magnetochemistry 10, no. 10: 77. https://doi.org/10.3390/magnetochemistry10100077
APA StyleBecker, W. P., Dáu, J. B. T., Souza, W. d., Mendez-Otero, R., Carias, R. B. V., & Jasmin. (2024). Incorporation of Superparamagnetic Magnetic–Fluorescent Iron Oxide Nanoparticles Increases Proliferation of Human Mesenchymal Stem Cells. Magnetochemistry, 10(10), 77. https://doi.org/10.3390/magnetochemistry10100077