The Role of Probiotics and Synbiotics on Hirsutism
Abstract
1. Introduction
1.1. Probiotics
1.2. Synbiotics
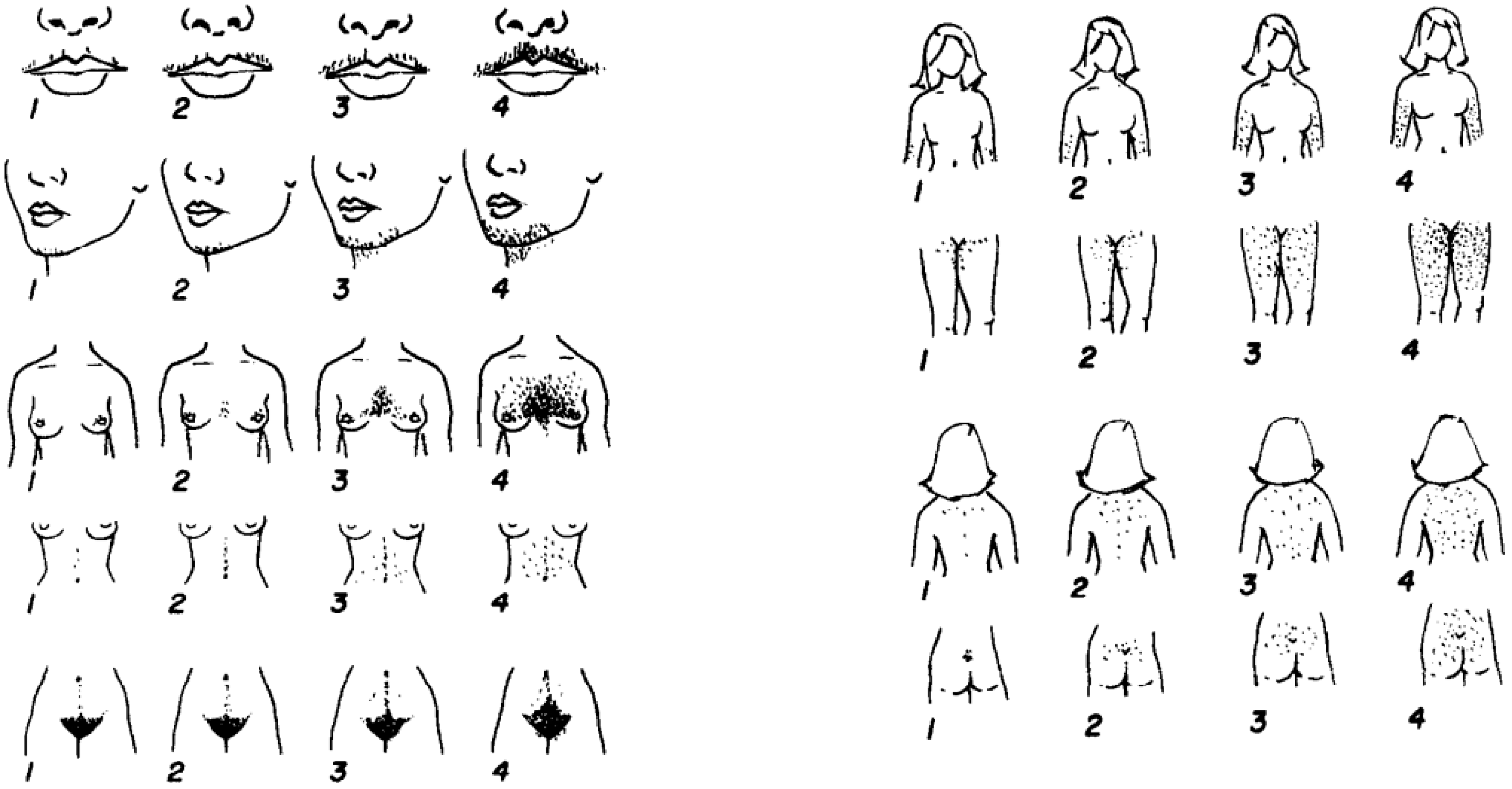
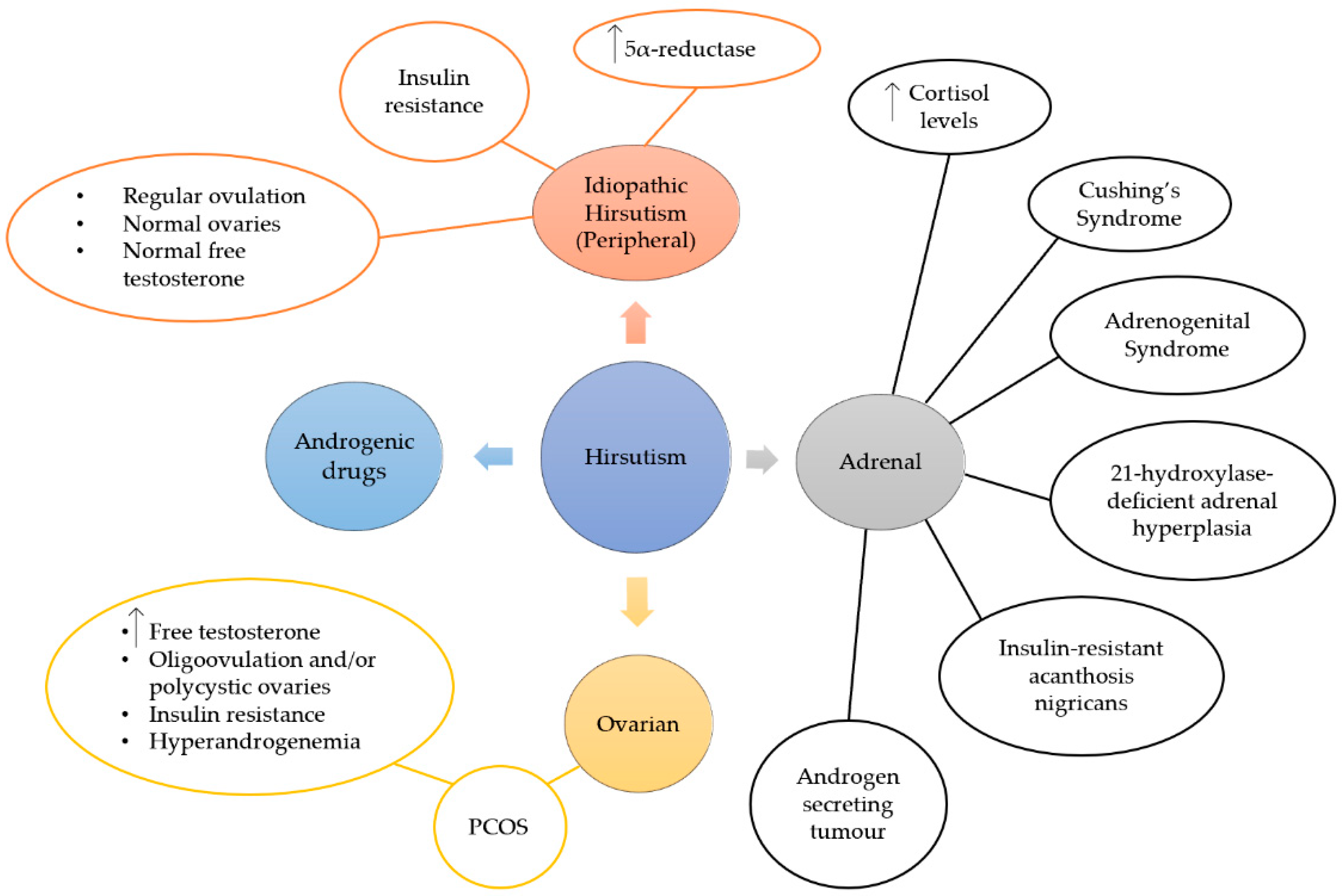
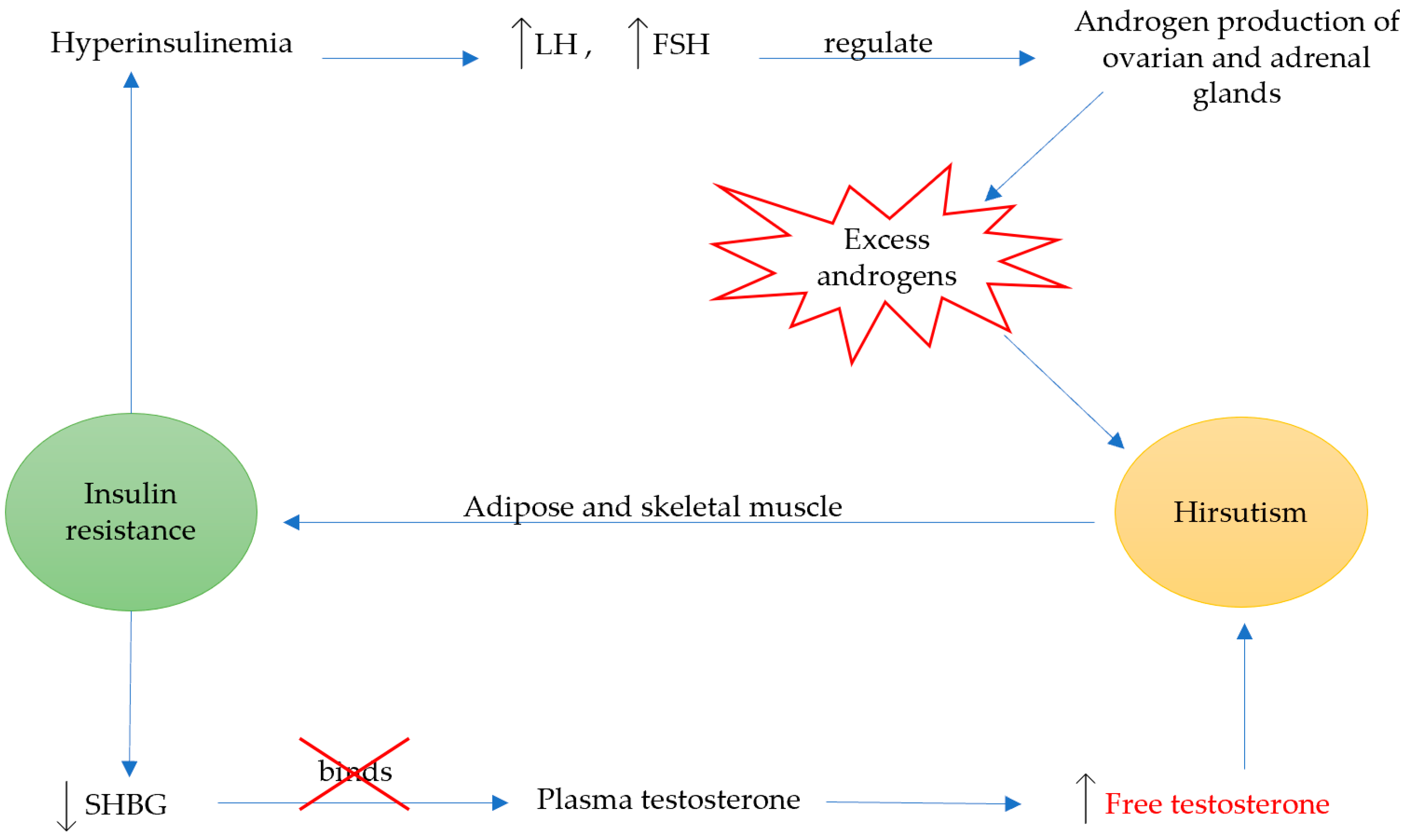
1.3. Hirsutism
2. Therapeutic Index
2.1. Chemically Derived Therapies
2.2. Naturally Derived Therapies
2.2.1. Probiotics and Hirsutism
2.2.2. Synbiotics and Hirsutism
3. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- McGovern, P.E.; Zhang, J.; Tang, J.; Zhang, Z.; Hall, G.R.; Moreau, R.A.; Nunez, A.; Butrym, E.D.; Richards, M.P.; Wang, C.-S.; et al. Fermented beverages of pre- and proto-historic China. Proc. Natl. Acad. Sci. USA 2004, 101, 17593–17598. [Google Scholar] [CrossRef] [PubMed]
- Sicard, D.; Legras, J.L. Bread, beer and wine: Yeast domestication in the Saccharomyces sensu stricto complex. Comptes Rendus -Biol. 2011, 334, 229–236. [Google Scholar] [CrossRef] [PubMed]
- Ozen, M.; Dinleyici, E.C. The history of probiotics: The untold story. Benef. Microbes 2015, 6, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Isolauri, E. Probiotics in human disease. Am. J. Clin. Nutr. 2001, 73, 1142S–1146S. [Google Scholar] [CrossRef] [PubMed]
- Vandenplas, Y.; Zakharova, I.; Dmitrieva, Y. Oligosaccharides in infant formula: More evidence to validate the role of prebiotics. Br. J. Nutr. 2015, 113, 1339–1344. [Google Scholar] [CrossRef] [PubMed]
- Gordon, S. Elie Metchnikoff: Father of natural immunity. Eur. J. Immunol. 2008, 38, 3257–3264. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, K.L.; Gaudino Caputo, L.R.; Tavares Carvalho, J.C.; Evangelista, J.; Schneedorf, J.M. Antimicrobial and healing activity of kefir and kefiran extract. Int. J. Antimicrob. Agents 2005, 25, 404–408. [Google Scholar] [CrossRef]
- Rahimzadeh, G.; Fazeli, M.R.; Mozafari, A.N.; Mesbahi, M. Evaluation of Anti-Microbial Activity and Wound Healing of Kefir | International Journal of Pharmaceutical Sciences and Research. Available online: http://ijpsr.com/bft-article/evaluation-of-anti-microbial-activity-and-wound-healing-of-kefir/?view=fulltext (accessed on 26 November 2018).
- Atalan, G.; Demirkan, I.; Yaman, H.; Cina, M. Effect of topical kefir application on open wound healing on in vivo study. Kafkas Univ. Vet. Fak. Dderg. 2003, 9, 43–47. [Google Scholar]
- Lolou, V.; Panayiotidis, M.I. Functional role of probiotics and prebiotics on skin health and disease. Fermentation 2019, 5, 41. [Google Scholar] [CrossRef]
- Sharifi, M.; Moridnia, A.; Mortazavi, D.; Salehi, M.; Bagheri, M.; Sheikhi, A. Kefir: A powerful probiotics with anticancer properties. Med. Oncol. 2017, 34, 183. [Google Scholar] [CrossRef]
- Chen, M.J.; Liu, J.R.; Sheu, J.F.; Lin, C.W.; Chuang, C.L. Study on skin care properties of milk kefir whey. Asian-Australasian J. Anim. Sci. 2006, 19, 905–908. [Google Scholar] [CrossRef]
- Collins, M.D.; Phillips, B.A.; Paolo, Z. Deozyribonucleic acid homology studies of lactobacillus casei etc. Collins 1989. Int. J. Syst. Bacteriol. 1989, 39, 105–108. [Google Scholar] [CrossRef]
- Report of a Joint FAO/WHO Working Group on Drafting Guidelines for the Evaluation of Probiotics in Food. Guidelines for the Evaluation of Probiotics in Food. 2002. Available online: https://www.who.int/foodsafety/fs_management/en/probiotic_guidelines.pdf (accessed on 11 January 2021).
- Goldin, B.R.; Swenson, L.; Dwyer, J.; Sexton, M.; Gorbach, S.L. Effect of diet and Lactobacillus acidophilus supplements on human fecal bacterial enzymes. J. Natl. Cancer Inst. 1980, 64, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Scholz-Ahrens, K.E.; Adolphi, B.; Rochat, F.; Barclay, D.V.; de Vrese, M.; Açil, Y.; Schrezenmeir, J. Effects of probiotics, prebiotics, and synbiotics on mineral metabolism in ovariectomized rats - impact of bacterial mass, intestinal absorptive area and reduction of bone turn-over. NFS J. 2016, 3, 41–50. [Google Scholar] [CrossRef]
- Milani, C.; Duranti, S.; Bottacini, F.; Casey, E.; Turroni, F.; Mahony, J.; Belzer, C.; Delgado Palacio, S.; Arboleya Montes, S.; Mancabelli, L.; et al. The First Microbial Colonizers of the Human Gut: Composition, Activities, and Health Implications of the Infant Gut Microbiota. Microbiol. Mol. Biol. Rev. 2017, 81, 1–67. [Google Scholar] [CrossRef]
- Talebi, S.; Karimifar, M.; Heidari, Z.; Mohammadi, H.; Askari, G. The effects of synbiotic supplementation on thyroid function and inflammation in hypothyroid patients: A randomized, double‑blind, placebo‑controlled trial. Complement. Ther. Med. 2020, 48. [Google Scholar] [CrossRef]
- Nasri, K.; Jamilian, M.; Rahmani, E.; Bahmani, F.; Tajabadi-Ebrahimi, M.; Asemi, Z. The effects of synbiotic supplementation on hormonal status, biomarkers of inflammation and oxidative stress in subjects with polycystic ovaryfile:///C:/Users/Vassoula/Downloads/29664663.nbib syndrome: A randomized, double-blind, placebo-controlled trial. BMC Endocr. Disord. 2018, 18, 1–8. [Google Scholar] [CrossRef]
- He, M.; Gao, J.; Wu, J.; Zhou, Y.; Fu, H.; Ke, S.; Yang, H.; Chen, C.; Huang, L. Host gender and androgen levels regulate gut bacterial taxa in pigs leading to sex-biased serum metabolite profiles. Front. Microbiol. 2019, 10, 1–13. [Google Scholar] [CrossRef]
- Yarak, S.; Brasil Parada, M.O.A.; Bagatin, E.; Talarico Filho, S.; Hassun, K.M. Hyperandrogenism and skin: Polycystic ovary syndrome and peripheral insulin resistance. An. Bras. Dermatol. 2005, 80, 395–410. [Google Scholar] [CrossRef]
- Carnevali, O.; Avella, M.A.; Gioacchini, G. Effects of probiotic administration on zebrafish development and reproduction. Gen. Comp. Endocrinol. 2012, 188, 297–302. [Google Scholar] [CrossRef]
- Sonal Sekhar, M.; Unnikrishnan, M.K.; Vijayanarayana, K.; Rodrigues, G.S.; Mukhopadhyay, C. Topical application/formulation of probiotics: Will it be a novel treatment approach for diabetic foot ulcer? Med. Hypotheses 2014, 82, 86–88. [Google Scholar] [CrossRef] [PubMed]
- Sikorska, H.; Smoragiewicz, W. Role of probiotics in the prevention and treatment of meticillin-resistant Staphylococcus aureus infections. Int. J. Antimicrob. Agents 2013, 42, 475–481. [Google Scholar] [CrossRef] [PubMed]
- Eggers, S.; Barker, A.; Valentine, S.; Hess, T.; Duster, M.; Safdar, N. Impact of Probiotics for Reducing Infections in Veterans (IMPROVE): Study protocol for a double-blind, randomized controlled trial to reduce carriage of Staphylococcus aureus. Contemp. Clin. Trials 2017, 52, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Frei, R.; Akdis, M.; O’mahony, L. Prebiotics, probiotics, synbiotics, and the immune system: Experimental data and clinical evidence. Curr. Opin. Gastroenterol. 2015, 31, 153–158. [Google Scholar] [CrossRef]
- Rajkumar, H.; Kumar, M.; Das, N.; Kumar, S.N.; Challa, H.R.; Nagpal, R. Effect of Probiotic Lactobacillus salivarius UBL S22 and Prebiotic Fructo-oligosaccharid on Serum Lipids, Inflammatory Markers, Insulin Sensitivity, and Gut Bacteria in Healthy Young Volunteers: A Randomized Controlled Single-Blind Pilot Study. J. Cardiovasc. Pharmacol. Ther. 2015, 20, 289–298. [Google Scholar] [CrossRef]
- Cozzolino, M.; Vitagliano, A.; Pellegrini, L.; Chiurazzi, M.; Andriasani, A.; Ambrosini, G.; Garrido, N. Therapy with probiotics and synbiotics for polycystic ovarian syndrome: A systematic review and meta-analysis. Eur. J. Nutr. 2020, 59, 2841–2856. [Google Scholar] [CrossRef]
- Pandey, K.R.; Naik, S.R.; Vakil, B.V. Probiotics, prebiotics and synbiotics—A review. J. Food Sci. Technol. 2015, 52, 7577–7587. [Google Scholar] [CrossRef]
- Azad, M.A.K.; Sarker, M.; Li, T.; Yin, J. Probiotic Species in the Modulation of Gut Microbiota: An Overview. Biomed Res. Int. 2018, 2018. [Google Scholar] [CrossRef]
- Mori, N.; Kano, M.; Masuoka, N.; Konno, T.; Suzuki, Y.; Miyazaki, K.; Ueki, Y. Effect of probiotic and prebiotic fermented milk on skin and intestinal conditions in healthy young female students. Biosci. Microbiota Food Health 2016, 35, 105–112. [Google Scholar] [CrossRef]
- Sánchez, B.; Delgado, S.; Blanco-Míguez, A.; Lourenço, A.; Gueimonde, M.; Margolles, A. Probiotics, gut microbiota, and their influence on host health and disease. Mol. Nutr. Food Res. 2017, 61, 1–15. [Google Scholar] [CrossRef]
- Britti, M.; Roselli, M.; Finamore, A.; Merendino, N.; Mengheri, E. Regulation of immune response at intestinal and peripheral sites by probiotics. Biologia (Bratisl) 2006, 61, 735–740. [Google Scholar] [CrossRef]
- Thomas, C.M.; Versalovic, J. Probiotics-host communication. Gut Microbes 2010, 1, 148–163. [Google Scholar] [CrossRef] [PubMed]
- Bansal, S.; Mangal, M.; Sharma, S.K.; Gupta, R.K. Non-dairy Based Probiotics: A Healthy Treat for Intestine. Crit. Rev. Food Sci. Nutr. 2016, 56, 1856–1867. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Farnell, Y.Z.; Peebles, E.D.; Kiess, A.S.; Wamsley, K.G.S.; Zhai, W. Effects of prebiotics, probiotics, and their combination on growth performance, small intestine morphology, and resident Lactobacillus of male broilers. Poult. Sci. 2016, 95, 1332–1340. [Google Scholar] [CrossRef] [PubMed]
- Friedrich, A.D.; Paz, M.L.; Leoni, J.; Maglio, D.H.G. Message in a bottle: Dialog between intestine and skin modulated by probiotics. Int. J. Mol. Sci. 2017, 18, 1067. [Google Scholar] [CrossRef] [PubMed]
- White, J.S.; Hoper, M.; Parks, R.W.; Clements, W.D.B.; Diamond, T.; Bengmark, S. The probiotic bacterium Lactobacillus plantarum species 299 reduces intestinal permeability in experimental biliary obstruction. Lett. Appl. Microbiol. 2006, 42, 19–23. [Google Scholar] [CrossRef]
- Yamada, T.; Nagata, S.; Kondo, S.; Bian, L.; Wang, C.; Asahara, T.; Ohta, T.; Nomoto, K.; Yamashiro, Y. Effect of Continuous Fermented Milk Intake Containing Lactobacillus casei Strain Shirota on Fever in Mass Infectious Gastroenteritis Rest Home Outbreak. Kansenshogaku Zasshi 2009, 83, 31–35. [Google Scholar] [CrossRef]
- Imaoka, A.; Shima, T.; Kato, K.; Mizuno, S.; Uehara, T.; Matsumoto, S.; Setoyana, H.; Hara, T.; Umesaki, Y. Anti-inflammatory activity of probiotic Bifidobacterium: Enhancement of IL-10 production in peripheral blood mononuclear cells from ulcerative colitis patients and inhibition of IL-8 secretion in HT-29 cells. World J. Gastroenterol. 2008, 14, 2511–2516. [Google Scholar] [CrossRef]
- Abdin, A.A.; Saeid, E.M. An experimental study on ulcerative colitis as a potential target for probiotic therapy by Lactobacillus acidophilus with or without “olsalazine”. J. Crohn’s Colitis 2008, 2, 296–303. [Google Scholar] [CrossRef]
- Amara, A.A.; Shibl, A. Role of Probiotics in health improvement, infection control and disease treatment and management. Saudi Pharm. J. 2015, 23, 107–114. [Google Scholar] [CrossRef]
- Mego, M.; Májek, J.; Končeková, R.; Ebringer, L.; Čierniková, S.; Rauko, P.; Kováč, M.; Trupl, J.; Slezák, P.; Zajac, V. Intramucosal bacteria in colon cancer and their elimination by probiotic strain Enterococcus faecium M-74 with organic selenium. Folia Microbiol. 2005, 50, 443–447. [Google Scholar] [CrossRef] [PubMed]
- Boudeau, J.; Glasser, A.L.; Julien, S.; Colombel, J.F.; Darfeuille-Michaud, A. Inhibitory effect of probiotic Escherichia coli strain Nissle 1917 on adhesion to and invasion of intestinal epithelial cells by adherent-invasive E.coli strains isolated from patients with Crohn’s disease. Aliment. Pharmacol. Ther. 2003, 18, 45–56. [Google Scholar] [CrossRef] [PubMed]
- Anukam, K.C.; Hayes, K.; Summers, K.; Reid, G. Probiotic Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14 may help downregulate TNF-alpha, IL-6, IL-8, IL-10 and IL-12 (p70) in the neurogenic bladder of spinal cord injured patient with urinary tract infections: A two-case study. Adv. Urol. 2009, 2009. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Thirabunyanon, M.; Boonprasom, P.; Niamsup, P. Probiotic potential of lactic acid bacteria isolated from fermented dairy milks on antiproliferation of colon cancer cells. Biotechnol. Lett. 2009, 31, 571–576. [Google Scholar] [CrossRef] [PubMed]
- Hacini-Rachinel, F.; Gheit, H.; Le Luduec, J.B.; Dif, F.; Nancey, S.; Kaiserlian, D. Oral probiotic control skin inflammation by acting on both effector and regulatory T cells. PLoS ONE 2009, 4, e4903. [Google Scholar] [CrossRef] [PubMed]
- Chapat, L.; Chemin, K.; Dubois, B.; Bourdet-Sicard, R.; Kaiserlian, D. Lactobacillus casei reduces CD8+T cell-mediated skin inflammation. Eur. J. Immunol. 2004, 34, 2520–2528. [Google Scholar] [CrossRef]
- Weise, C.; Zhu, Y.; Ernst, D.; Ku, A.A. Oral administration of Escherichia coli Nissle 1917 prevents allergen-induced dermatitis in mice. Exp. Dermatol. 2011, 20, 805–809. [Google Scholar] [CrossRef]
- Vaiserman, A.M.; Koliada, A.K.; Marotta, F. Gut microbiota: A player in aging and a target for anti-aging intervention. Ageing Res. Rev. 2017, 35, 36–45. [Google Scholar] [CrossRef]
- Musthaq, S.; Mazuy, A.; Jakus, J. The microbiome in dermatology. Clin. Dermatol. 2018, 36, 390–398. [Google Scholar] [CrossRef]
- Kalliomäki, M.; Salminen, S.; Poussa, T.; Isolauri, E. Probiotics during the First 7 Years of Life: A Cumulative Risk Reduction of Eczema in a Randomized, Placebo-Controlled Trial; Mosby: Maryland Heights, MI, USA, 2007; Volume 119. [Google Scholar]
- Huseini, H.F.; Rahimzadeh, G.; Fazeli, M.R.; Mehrazma, M.; Salehi, M. Evaluation of wound healing activities of kefir products. Burns 2012, 38, 719–723. [Google Scholar] [CrossRef]
- Nasrabadi, H. Study of cutaneous wound healing in rats treated with Lactobacillus plantarum on days 1, 3, 7, 14 and 21. Afr. J. Pharm. Pharmacol. 2011, 5, 2395–2401. [Google Scholar] [CrossRef]
- Jebur, M.S. Therapeutic efficacy of Lactobacillus acidophilus against bacterial isolates from burn wounds. N. Am. J. Med. Sci. 2010, 2, 586–591. [Google Scholar] [CrossRef] [PubMed]
- Tsiouris, C.G.; Tsiouri, M.G. Human microflora, probiotics and wound healing. Wound Med. 2017, 19, 33–38. [Google Scholar] [CrossRef]
- Rumbaugh, K.P.; Griswold, J.A.; Iglewski, B.H.; Hamood, A.N. Contribution of quorum sensing to the virulence of Pseudomonas aeruginosa in burn wound infections. Infect. Immun. 1999, 67, 5854–5862. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, G.L.V.; Leite, A.Z.; Higuchi, B.S.; Gonzaga, M.I.; Mariano, V.S. Intestinal dysbiosis and probiotic applications in autoimmune diseases. Immunology 2017, 152, 1–12. [Google Scholar] [CrossRef]
- Candon, S.; Perez-Arroyo, A.; Marquet, C.; Valette, F.; Foray, A.P.; Pelletier, B.; Milani, C.; Ventura, M.; Bach, J.F.; Chatenoud, L. Antibiotics in early life alter the gut microbiome and increase disease incidence in a spontaneous mouse model of autoimmune insulin-dependent diabetes. PLoS ONE 2015, 10, e0125448. [Google Scholar] [CrossRef]
- Hickson, M.; D’Souza, A.L.; Muthu, N.; Rogers, T.R.; Want, S.; Rajkumar, C.; Bulpitt, C.J. Use of probiotic Lactobacillus preparation to prevent diarrhoea associated with antibiotics: Randomised double blind placebo controlled trial. Br. Med. J. 2007, 335, 80–83. [Google Scholar] [CrossRef]
- He, C.; Cheng, D.; Peng, C.; Li, Y.; Zhu, Y.; Lu, N. High-fat diet induces dysbiosis of gastric microbiota prior to gut microbiota in association with metabolic disorders in mice. Front. Microbiol. 2018, 9, 1–9. [Google Scholar] [CrossRef]
- Ravussin, Y.; Koren, O.; Spor, A.; Leduc, C.; Gutman, R.; Stombaugh, J.; Knight, R.; Ley, R.E.; Leibel, R.L. Responses of gut microbiota to diet composition and weight loss in lean and obese mice. Obesity 2012, 20, 738–747. [Google Scholar] [CrossRef]
- Ochoa-Repáraz, J.; Kasper, L.H. The Second Brain: Is the Gut Microbiota a Link Between Obesity and Central Nervous System Disorders? Curr. Obes. Rep. 2016, 5, 51–64. [Google Scholar] [CrossRef]
- Calvani, R.; Picca, A.; Lo Monaco, M.R.; Landi, F.; Bernabei, R.; Marzetti, E. Of microbes and minds: A narrative review on the second brain aging. Front. Med. 2018, 5, 1–11. [Google Scholar] [CrossRef]
- Sokol, H.; Seksik, P.; Furet, J.P.; Firmesse, O.; Nion-Larmurier, I.; Beaugerie, L.; Cosnes, J.; Corthier, G.; Marteau, P.; Doraé, J. Low counts of faecalibacterium prausnitzii in colitis microbiota. Inflamm. Bowel Dis. 2009, 15, 1183–1189. [Google Scholar] [CrossRef] [PubMed]
- Sokol, H.; Pigneur, B.; Watterlot, L.; Lakhdari, O.; Bermudez-Humaran, L.G.; Gratadoux, J.-J.; Blugeon, S.; Bridonneau, C.; Furet, J.-P.; Corthier, G.; et al. Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium identified by gut microbiota analysis of Crohn disease patients. J. Pathol. 1990, 162, 323–327. [Google Scholar] [CrossRef] [PubMed]
- Partlow, J.; Blikslager, A.; Matthews, C.; Law, M.; Daniels, J.; Baker, R.; Labens, R. Effect of topically applied Saccharomyces boulardii on the healing of acute porcine wounds: A preliminary study. BMC Res. Notes 2016, 9. [Google Scholar] [CrossRef] [PubMed]
- Brouwer, M.L.; Wolt-Plompen, S.A.A.; Dubios, A.E.J.; Van Der Heide, S.; Jansen, D.F.; Hoijer, M.A.; Kauffman, H.F.; Duiverman, E.J. No effects of probiotics on atopic dermatitis in infancy: A randomized placebo-controlled trial. Clin. Exp. Allergy 2006, 36, 899–906. [Google Scholar] [CrossRef] [PubMed]
- Sugimoto, S.; Ishii, Y.; Izawa, N.; Masuoka, N.; Kano, M.; Sone, T.; Chiba, K.; Miyazaki, K.; Ishikawa, F. Photoprotective effects of Bifidobacterium breve supplementation against skin damage induced by ultraviolet irradiation in hairless mice. Photodermatol. Photoimmunol. Photomed. 2012, 28, 312–319. [Google Scholar] [CrossRef]
- Queipo-Ortuño, M.I.; Seoane, L.M.; Murri, M.; Pardo, M.; Gomez-Zumaquero, J.M.; Cardona, F.; Casanueva, F.; Tinahones, F.J. Gut Microbiota Composition in Male Rat Models under Different Nutritional Status and Physical Activity and Its Association with Serum Leptin and Ghrelin Levels. PLoS ONE 2013, 8. [Google Scholar] [CrossRef]
- Naruszewicz, M.; Johansson, M.L.; Zapolska-Downar, D.; Bukowska, H. Effect of Lactobacillus plantarum 299v on cardiovascular disease risk factors in smokers. Am. J. Clin. Nutr. 2002, 76, 1249–1255. [Google Scholar] [CrossRef]
- Messaoudi, M.; Lalonde, R.; Violle, N.; Javelot, H.; Desor, D.; Nejdi, A.; Bisson, J.F.; Rougeot, C.; Pichelin, M.; Cazaubiel, M.; et al. Assessment of psychotropic-like properties of a probiotic formulation (Lactobacillus helveticus R0052 and Bifidobacterium longum R0175) in rats and human subjects. Br. J. Nutr. 2011, 105, 755–764. [Google Scholar] [CrossRef]
- Karlsson, F.H.; Tremaroli, V.; Nookaew, I.; Bergström, G.; Behre, C.J.; Fagerberg, B.; Nielsen, J.; Bäckhed, F. Gut metagenome in European women with normal, impaired and diabetic glucose control. Nature 2013, 498, 99–103. [Google Scholar] [CrossRef]
- Vrieze, A.; Van Nood, E.; Holleman, F.; Salojärvi, J.; Kootte, R.S.; Bartelsman, J.F.W.M.; Dallinga-Thie, G.M.; Ackermans, M.T.; Serlie, M.J.; Oozeer, R.; et al. Transfer of intestinal microbiota from lean donors increases insulin sensitivity in individuals with metabolic syndrome. Gastroenterology 2012, 143, 913–916. [Google Scholar] [CrossRef] [PubMed]
- Adlercreutz, H.; Pulkkinen, M.O.; Hämäläinen, E.K.; Korpela, J.T. Studies on the role of intestinal bacteria in metabolism of synthetic and natural steroid hormones. J. Steroid Biochem. 1984, 20, 217–229. [Google Scholar] [CrossRef]
- Markle, J.G.M.; Frank, D.N.; Mortin-Toth, S.; Robertson, C.E.; Feazel, L.M.; Rolle-Kampczyk, U.; Von Bergen, M.; McCoy, K.D.; Macpherson, A.J.; Danska, J.S. Sex differences in the gut microbiome drive hormone-dependent regulation of autoimmunity. Science 2013, 339, 1084–1088. [Google Scholar] [CrossRef] [PubMed]
- Furrie, E.; Macfarlane, S.; Kennedy, A.; Cummings, J.H.; Walsh, S.V.; O’Neil, D.A.; Macfarlane, G.T. Synbiotic therapy (Bifidobacterium longum/Synergy 1) initiates resolution of inflammation in patients with active ulcerative colitis: A randomised controlled pilot trial. Gut 2005, 54, 242–249. [Google Scholar] [CrossRef] [PubMed]
- Liu, R.; Zhang, C.; Shi, Y.; Zhang, F.; Li, L.; Wang, X.; Ling, Y.; Fu, H.; Dong, W.; Shen, J.; et al. Dysbiosis of gut microbiota associated with clinical parameters in polycystic ovary syndrome. Front. Microbiol. 2017, 8, 1–12. [Google Scholar] [CrossRef]
- Hutkins, R.W.; Krumbeck, J.A.; Bindels, L.B.; Cani, P.D.; Fahey, G.; Goh, Y.J.; Hamaker, B.; Martens, E.C.; Mills, D.A.; Rastal, R.A.; et al. Prebiotics: Why definitions matter. Curr. Opin. Biotechnol. 2016, 37, 1–7. [Google Scholar] [CrossRef]
- Valenlia, K.B.; Morshedi, M.; Saghafi-Asl, M.; Shahabi, P.; Abbasi, M.M. Beneficial impacts of Lactobacillus plantarum and inulin on hypothalamic levels of insulin, leptin, and oxidative markers in diabetic rats. J. Funct. Foods 2018, 46, 529–537. [Google Scholar] [CrossRef]
- Jiang, S.; Mohammed, A.A.; Jacobs, J.A.; Cramer, T.A.; Cheng, H.W. Effect of synbiotics on thyroid hormones, intestinal histomorphology, and heat shock protein 70 expression in broiler chickens reared under cyclic heat stress. Poult. Sci. 2020, 99, 142–150. [Google Scholar] [CrossRef]
- Mofidi, F.; Poustchi, H.; Yari, Z.; Nourinayyer, B.; Merat, S.; Sharafkhah, M.; Malekzadeh, R.; Hekmatdoost, A. Synbiotic supplementation in lean patients with non-alcoholic fatty liver disease: A pilot, randomised, double-blind, placebo-controlled, clinical trial. Br. J. Nutr. 2017, 117, 662–668. [Google Scholar] [CrossRef]
- Eslamparast, T.; Poustchi, H.; Zamani, F.; Sharafkhah, M.; Malekzadeh, R.; Hekmatdoost, A. Synbiotic supplementation in nonalcoholic fatty liver disease: A randomized, double-blind, placebo-controlled pilot study. Am. J. Clin. Nutr. 2014, 99, 535–542. [Google Scholar] [CrossRef]
- Steed, H.; MacFarlane, G.T.; Blackett, K.L.; Bahrami, B.; Reynolds, N.; Walsh, S.V.; Cummings, J.H.; MacFarlane, S. Clinical trial: The microbiological and immunological effects of synbiotic consumption—A randomized double-blind placebo-controlled study in active Crohn’s disease. Aliment. Pharmacol. Ther. 2010, 32, 872–883. [Google Scholar] [CrossRef] [PubMed]
- Sivamaruthi, B.S. A comprehensive review on clinical outcome of probiotic and synbiotic therapy for inflammatory bowel diseases. Asian Pac. J. Trop. Biomed. 2018, 8, 179–186. [Google Scholar] [CrossRef]
- Westfall, S.; Lomis, N.; Prakash, S. A novel synbiotic delays Alzheimer’s disease onset via combinatorial gut-brain-axis signaling in Drosophila melanogaster. PLoS ONE 2019, 14, e0214985. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, H.; Matsumoto, S.; Ohashi, Y.; Imaoka, A.; Setoyama, H.; Umesaki, Y.; Tanaka, R.; Otani, T. Beneficial effects of probiotic Bifidobacterium and galacto-oligosaccharide in patients with ulcerative colitis: A randomized controlled study. Digestion 2011, 84, 128–133. [Google Scholar] [CrossRef] [PubMed]
- Hatch, R.; Rosenfield, R.L.; Kim, M.H.; Tredway, D. Hirsutism: Implications, etiology, and management. Am. J. Obstet. Gynecol. 1981, 140, 815–830. [Google Scholar] [CrossRef]
- Carmina, E. Prevalence of idiopathic hirsutism. Eur. J. Endocrinol. 1998, 139, 421–423. [Google Scholar] [CrossRef][Green Version]
- Azziz, R. The evaluation and management of hirsutism. Obstet. Gynecol. 2003, 101, 995–1007. [Google Scholar]
- Archer, J.S.; Chang, R.J. Hirsutism and acne in polycystic ovary syndrome. Best Pract. Res. Clin. Obstet. Gynaecol. 2004, 18, 737–754. [Google Scholar] [CrossRef]
- Franks, S. Diagnosis of polycystic ovarian syndrome: In defense of the Rotterdam criteria. J. Clin. Endocrinol. Metab. 2006, 91, 786–789. [Google Scholar] [CrossRef]
- Calvo, R.M.; Asunción, M.; Sancho, J.; San Millán, J.L.; Escobar-Morreale, H.F. The role of the CAG repeat polymorphism in the androgen receptor gene and of skewed X-chromosome inactivation, in the pathogenesis of hirsutism. J. Clin. Endocrinol. Metab. 2000, 85, 1735–1740. [Google Scholar] [CrossRef]
- Vottero, A.; Stratakis, C.A.; Ghizzoni, L.; Longui, C.A.; Karl, M.; Chrousos, G.P. Androgen receptor-mediated hypersensitivity to androgens in women with nonhyperandrogenic hirsutism: Skewing of X-chromosome inactivation. J. Clin. Endocrinol. Metab. 1999, 84, 1091–1095. [Google Scholar] [CrossRef]
- Ünlühizarci, K.; Karababa, Y.; Bayram, F.; Kelestimur, F. The investigation of insulin resistance in patients with idiopathic hirsutism. J. Clin. Endocrinol. Metab. 2004, 89, 2741–2744. [Google Scholar] [CrossRef] [PubMed]
- Talaei, A.; Adgi, Z.; Mohamadi Kelishadi, M. Idiopathic hirsutism and insulin resistance. Int. J. Endocrinol. 2013, 2013. [Google Scholar] [CrossRef]
- Barbieri, R.L.; Smith, S.; Ryan, K.J. The role of hyperinsulinemia in the pathogenesis of ovarian hyperandrogenism. Fertil. Steril. 1988, 50, 197–212. [Google Scholar] [CrossRef] [PubMed]
- Barrionuevo, P.; Nabhan, M.; Altayar, O.; Wang, Z.; Erwin, P.J.; Asi, N.; Martin, K.A.; Hassan Murad, M. Treatment Options for Hirsutism: A Systematic Review and Network Meta-Analysis. J. Clin. Endocrinol. Metab. 2018, 103, 1258–1264. [Google Scholar] [CrossRef] [PubMed]
- Moghetti, P.; Tosi, F.; Castello, R.; Magnani, C.M.; Negri, C.; Brun, E.; Furlani, L.; Caputo, M.; Muggeo, M. The insulin resistance in women with hyperandrogenism is partially reversed by antiandrogen treatment: Evidence that androgens impair insulin action in women. J. Clin. Endocrinol. Metab. 1996, 81, 952–960. [Google Scholar] [CrossRef]
- Corbould, A. Chronic testosterone treatment induces selective insulin resistance in subcutaneous adipocytes of women. J. Endocrinol. 2007, 192, 585–594. [Google Scholar] [CrossRef]
- Smith, S.; Ravnikar, V.A.; Barbieri, R.L. Androgen and insulin response to an oral glucose challenge in hyperandrogenic women. Fertil. Steril. 1987, 48, 72–77. [Google Scholar] [CrossRef]
- Mathur, R.S.; Moody, L.O.; Landgrebe, S.; Williamson, H.O. Plasma androgens and sex hormone-binding globulin in the evaluation of hirsute females. Fertil. Steril. 1981, 35, 29–35. [Google Scholar] [CrossRef]
- Dunaif, A.; Green, G.; Phelps, R.G.; Lebwohl, M.; Futterweit, W.; Lewy, L. Acanthosis Nigricans, Insulin Action, and Hyperandrogenism: Clinical, Histological, and Biochemical Findings*. J. Clin. Endocrinol. Metab. 1991, 73, 590–595. [Google Scholar] [CrossRef]
- Dunaif, A.; Graf, M.; Mandeli, J.; Laumas, V.; Dobrjansky, A. Characterization of groups of hyperaiidrogenic women with acanthosis nigricans, impaired glucose tolerance, and/or hyperinsulinemia. J. Clin. Endocrinol. Metab. 1987, 65, 499–507. [Google Scholar] [CrossRef]
- Azziz, R.; Carmina, E.; Sawaya, M.E. Idiopathic Hirsutism*. Endocr. Rev. 2000, 21, 347–362. [Google Scholar] [CrossRef] [PubMed]
- Escobar-Morreale, H.F.; Carmina, E.; Dewailly, D.; Gambineri, A.; Kelestimur, F.; Moghetti, P.; Pugeat, M.; Qiao, J.; Wijeyaratne, C.N.; Witchel, S.F.; et al. Epidemiology, diagnosis and management of hirsutism: A consensus statement by the androgen excess and polycystic ovary syndrome society. Hum. Reprod. Update 2012, 18, 146–170. [Google Scholar] [CrossRef] [PubMed]
- Irons, E.E. The clinical evaluation of drugs. J. Am. Med. Assoc. 1929, 93, 1523–1524. [Google Scholar] [CrossRef]
- Ibáñez, L.; de Zegher, F. Low-dose flutamide-metformin therapy for hyperinsulinemic hyperandrogenism in non-obese adolescents and women. Hum. Reprod. Update 2006, 12, 243–252. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ibáñez, L.; De Zegher, F. Low-dose combination of flutamide, metformin and an oral contraceptive for non-obese, young women with polycystic ovary syndrome. Hum. Reprod. 2003, 18, 57–60. [Google Scholar] [CrossRef][Green Version]
- Rautio, K.; Tapanainen, J.S.; Ruokonen, A.; Morin-Papunen, L.C. Effects of metformin and ethinyl estradiol-cyproterone acetate on lipid levels in obese and non-obese women with polycystic ovary syndrome. Eur. J. Endocrinol. 2005, 152, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Ibáñez, L.; De Zegher, F. Ethinylestradiol-drospirenone, flutamide-metformin, or both for adolescents and women with hyperinsulinemic hyperandrogenism: Opposite effects on adipocytokines and body adiposity. J. Clin. Endocrinol. Metab. 2004, 89, 1592–1597. [Google Scholar] [CrossRef]
- Harborne, L.; Fleming, R.; Lyall, H.; Sattar, N.; Norman, J. Metformin or antiandrogen in the treatment of hirsutism in polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 2003, 88, 4116–4123. [Google Scholar] [CrossRef]
- Diamanti-Kandarakis, E.; Kouli, C.; Tsianateli, T.; Bergiele, A. Therapeutic effects of metformin on insulin resistance and hyperandrogenism in polycystic ovary syndrome. Eur. J. Endocrinol. 1998, 138, 269–274. [Google Scholar] [CrossRef]
- Haas, J.; Bentov, Y. Should metformin be included in fertility treatment of PCOS patients? Med. Hypotheses 2017, 100, 54–58. [Google Scholar] [CrossRef] [PubMed]
- Dewis, P.; Petsos, P.; Newman, M.; Anderson, D.C. the Treatment of Hirsutism With a Combination of Desogestrel and Ethinyl Oestradiol. Clin. Endocrinol. 1985, 22, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Mastorakos, G.; Koliopoulos, C.; Creatsas, G. Androgen and lipid profiles in adolescents with polycystic ovary syndrome who were treated with two forms of combined oral contraceptives. Fertil. Steril. 2002, 77, 919–927. [Google Scholar] [CrossRef]
- Zeng, X.; Xie, Y.J.; Liu, Y.T.; Long, S.L.; Mo, Z. cheng Polycystic ovarian syndrome: Correlation between hyperandrogenism, insulin resistance and obesity. Clin. Chim. Acta 2020, 502, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Acbay, O.; Gundogdu, S. Can metformin reduce insulin resistance in polycystic ovary syndrome? Fertil. Steril. 1996, 65, 946–949. [Google Scholar] [CrossRef]
- Moghetti, P.; Castello, R.; Negri, C.; Tosi, F.; Perrone, F.; Caputo, M.; Zanolin, E.; Muggeo, M. Metformin effects on clinical features, endocrine and metabolic profiles, and insulin sensitivity in polycystic ovary syndrome: A randomized, double-blind, placebo-controlled 6-month trial, followed by open, long-term clinical evaluation. J. Clin. Endocrinol. Metab. 2000, 85, 139–146. [Google Scholar] [CrossRef]
- Kolodziejczyk, B.; Duleba, A.J.; Spaczynski, R.Z.; Pawelczyk, L. Metformin therapy decreases hyperandrogenism and hyperinsulinemia in women with polycystic ovary syndrome. Fertil. Steril. 2000, 73, 1149–1154. [Google Scholar] [CrossRef]
- Morin-Papunen, L.C.; Koivunen, R.M.; Ruokonen, A.; Martikainen, H.K. Metformin therapy improves the menstrual pattern with minimal endocrine and metabolic effects in women with polycystic ovary syndrome. Fertil. Steril. 1998, 69, 691–696. [Google Scholar] [CrossRef]
- Ibáñez, L.; De Zegher, F. Flutamide-Metformin Therapy to Reduce Fat Mass in Hyperinsulinemic Ovarian Hyperandrogenism: Effects in Adolescents and in Women on Third-Generation Oral Contraception. J. Clin. Endocrinol. Metab. 2003, 88, 4720–4724. [Google Scholar] [CrossRef][Green Version]
- Carmina, E. Anti-androgens for the treatment of hirsutism. Expert Opin. Investig. Drugs 2002, 11, 357–363. [Google Scholar] [CrossRef]
- Mowszowicz, I.; Wright, F.; Vincens, M.; Rigaud, C.; Nahoul, K.; Mavier, P.; Guillemant, S.; Kuttenn, F.; Mauvais-Jarvis, P. Androgen metabolism in hirsute patients treated with cyproterone acetate. J. Steroid Biochem. 1984, 20, 757–761. [Google Scholar] [CrossRef]
- Corvol, P.; Michaud, A.; Menard, J.; Freifeld, M.; Mahoudeau, J. Antiandrogenic effect of spirolactones: Mechanism of action. Endocrinology 1975, 97, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Gobinet, J.; Poujol, N.; Sultan, C. Molecular action of androgens. Mol. Cell. Endocrinol. 2002, 198, 15–24. [Google Scholar] [CrossRef]
- Dewhurst, C.J.; Underhill, R.; Goldman, S.; Mansfield, M. the Treatment of Hirsutism With Cyproterone Acetate (an Anti-Androgen). BJOG An Int. J. Obstet. Gynaecol. 1977, 84, 119–123. [Google Scholar] [CrossRef] [PubMed]
- Kuttenn, F.; Rigaud, C.; Wright, F.; Mauvais-Jarvis, P. Treatment of hirsutism by oral cyproterone acetate and percutaneous estradiol. J. Clin. Endocrinol. Metab. 1980, 51, 1107–1111. [Google Scholar] [CrossRef]
- Shapiro, G.; Evron, S. A novel use of spironolactone: Treatment of hirsutism. J. Clin. Endocrinol. Metab. 1980, 51, 429–432. [Google Scholar] [CrossRef]
- Jones, D.B.; Ibraham, I.; Edwards, C.R.W. Hair growth and androgen responses in hirsute women treated with continuous cyproterone acetate and cyclical ethinyl oestradiol. Acta Endocrinol. 1987, 116, 497–501. [Google Scholar] [CrossRef]
- Lobo, R.A.; Shoupe, D.; Serafini, P.; Brinton, D.; Horton, R. The effects of two doses of spironolactone on serum androgens and anagen hair in hirsute women. Fertil. Steril. 1985, 43, 200–205. [Google Scholar] [CrossRef]
- Pittaway, D.E.; Maxson, W.S.; Wentz, A.C. Spironolactone in combination drug therapy for unresponsive hirsutism. Fertil. Steril. 1985, 43, 878–882. [Google Scholar] [CrossRef]
- O’brien, R.C.; Cooper, M.E.; Murray, R.M.L.; Seeman, E.; Thomas, A.K.; Jerums, G. Comparison of sequential cyproterone acetate/estrogen versus spironolactone/oral contraceptive in the treatment of hirsutism. J. Clin. Endocrinol. Metab. 1991, 72, 1008–1013. [Google Scholar] [CrossRef]
- Cusan, L.; Dupont, A.; Gomez, J.L.; Tremblay, R.R.; Labrie, F. Comparison of flutamide and spironolactone in the treatment of hirsutism: A randomized controlled trial. Fertil. Steril. 1994, 61, 281–287. [Google Scholar] [CrossRef]
- Müderris, I.I.; Bayram, F.; Özçelik, B.; Güven, M. New alternative treatment in hirsutism: Bicalutamide 25 mg/day. Gynecol. Endocrinol. 2002, 16, 63–66. [Google Scholar] [CrossRef] [PubMed]
- Moretti, C.; Guccione, L.; Giacinto, P. Di; Simonelli, I.; Exacoustos, C.; Toscano, V.; Motta, C.; De Leo, V.; Petraglia, F.; Lenzi, A. Combined oral contraception and bicalutamide in polycystic ovary syndrome and severe hirsutism: A double-blind randomized controlled trial. J. Clin. Endocrinol. Metab. 2018, 103, 824–838. [Google Scholar] [CrossRef] [PubMed]
- Bahceci, M.; Tuzcu, A.; Canoruc, N.; Tuzun, Y.; Kidir, V.; Aslan, C. Serum C-reactive protein (CRP) levels and insulin resistance in non-obese women with polycystic ovarian syndrome, and effect of bicalutamide on hirsutism, CRP levels and insulin resistance. Horm. Res. 2004, 62, 283–287. [Google Scholar] [CrossRef] [PubMed]
- 138. Goswami, P.K.; Khale, A.; Ogale, S. O. Natural remedies for polycystic ovarian syndrome (PCOS): A review. Int. J. Pharm. Phytopharm. Res. 2012, 1, 396–402. [Google Scholar]
- Kolivand, M.; Keramat, A.; Khosravi, A. The Effect of Herbal Teas on Management of Polycystic Ovary Syndrome: A Systematic Review. J. Midwifery Reprod. Heal. 2017, 5, 1098–1106. [Google Scholar] [CrossRef]
- Akdoğan, M.; Tamer, M.N.; Cüre, E.; Cüre, M.C.; Köroğlu, B.K.; Delibaş, N. Effect of spearmint (Mentha spicata Labiatae) teas on androgen levels in women with hirsutism. Phyther. Res. 2007, 21, 444–447. [Google Scholar] [CrossRef]
- Grant, P.; Ramasamy, S. An update on plant derived anti-androgens. Int. J. Endocrinol. Metab. 2012, 10, 497–502. [Google Scholar] [CrossRef]
- Grant, P. Spearmint Herbal Tea has Signifi cant Anti-androgen Effects in Polycystic Ovarian Syndrome. A Randomized Controlled Trial. Phyther. Res. 2010, 24, 186–188. [Google Scholar] [CrossRef]
- Haj-Husein, I.; Tukan, S.; Alkazaleh, F. The effect of marjoram (Origanum majorana) tea on the hormonal profile of women with polycystic ovary syndrome: A randomised controlled pilot study. J. Hum. Nutr. Diet. 2016, 29, 105–111. [Google Scholar] [CrossRef]
- Phy, J.L.; Pohlmeier, A.M.; Cooper, J.A.; Watkins, P.; Spallholz, J.; Harris, K.S.; Berenson, A.B.; Boylan, M. Low Starch/Low Dairy Diet Results in Successful Treatment of Obesity and Co- Morbidities Linked to Polycystic Ovary Syndrome (PCOS). J. Obes. Weight Loss Ther. 2015, 5, 1–12. [Google Scholar] [CrossRef]
- Pohlmeier, A.M.; Phy, J.L.; Watkins, P.; Boylan, M.; Spallholz, J.; Harris, K.S.; Cooper, J.A. Effect of a low-starch/low-dairy diet on fat oxidation in overweight and obese women with polycystic ovary syndrome. Appl. Physiol. Nutr. Metab. 2014, 39, 1237–1244. [Google Scholar] [CrossRef] [PubMed]
- Janiszewska, J.; Ostrowska, J.; Szostak-Węgierek, D. Milk and Dairy Products and Their Impact on Carbohydrate Metabolism and Fertility-A Potential Role in the Diet of Women with Polycystic Ovary Syndrome. Nutrients 2020, 12. [Google Scholar] [CrossRef] [PubMed]
- Shamasbi, S.G.; Ghanbari-Homayi, S.; Mirghafourvand, M. The effect of probiotics, prebiotics, and synbiotics on hormonal and inflammatory indices in women with polycystic ovary syndrome: A systematic review and meta-analysis. Eur. J. Nutr. 2020, 59, 433–450. [Google Scholar] [CrossRef] [PubMed]
- Tabrizi, R.; Ostadmohammadi, V.; Akbari, M.; Lankarani, K.B.; Vakili, S.; Peymani, P.; Karamali, M.; Kolahdooz, F.; Asemi, Z. The Effects of Probiotic Supplementation on Clinical Symptom, Weight Loss, Glycemic Control, Lipid and Hormonal Profiles, Biomarkers of Inflammation, and Oxidative Stress in Women with Polycystic Ovary Syndrome: A Systematic Review and Meta-analysis of Ra. Probiotics Antimicrob. Proteins 2019. [Google Scholar] [CrossRef] [PubMed]
- Ostadmohammadi, V.; Jamilian, M.; Bahmani, F.; Asemi, Z. Vitamin D and probiotic co-supplementation affects mental health, hormonal, inflammatory and oxidative stress parameters in women with polycystic ovary syndrome. J. Ovarian Res. 2019, 12, 1–8. [Google Scholar] [CrossRef]
- Jamilian, M.; Mansury, S.; Bahmani, F.; Heidar, Z.; Amirani, E.; Asemi, Z. The effects of probiotic and selenium co-supplementation on parameters of mental health, hormonal profiles, and biomarkers of inflammation and oxidative stress in women with polycystic ovary syndrome 11 Medical and Health Sciences 1103 Clinical Sciences. J. Ovarian Res. 2018, 11, 1–7. [Google Scholar] [CrossRef]
- He, F.F.; Li, Y.M. Role of gut microbiota in the development of insulin resistance and the mechanism underlying polycystic ovary syndrome: A review. J. Ovarian Res. 2020, 13, 1–13. [Google Scholar] [CrossRef]
- Guevara, G.; Flores, Y.O.; De Las Heras, L.F.; Perera, J.; Navarro Llorens, J.M. Metabolic engineering of Rhodococcus ruber Chol-4: A cell factory for testosterone production. PLoS ONE 2019, 14. [Google Scholar] [CrossRef]
- Colldén, H.; Landin, A.; Wallenius, V.; Elebring, E.; Fändriks, L.; Nilsson, M.E.; Ryberg, H.; Poutanen, M.; Sjögren, K.; Vandenput, L.; et al. The gut microbiota is a major regulator of androgen metabolism in intestinal contents. Am. J. Physiol. Endocrinol. Metab. 2019, 317, E1182–E1192. [Google Scholar] [CrossRef]
- Tremellen, K.; Pearce, K. Dysbiosis of Gut Microbiota (DOGMA)—A novel theory for the development of Polycystic Ovarian Syndrome. Med. Hypotheses 2012, 79, 104–112. [Google Scholar] [CrossRef] [PubMed]
- Lindheim, L.; Bashir, M.; Münzker, J.; Trummer, C.; Zachhuber, V.; Leber, B.; Horvath, A.; Pieber, T.R.; Gorkiewicz, G.; Stadlbauer, V.; et al. Alterations in gut microbiome composition and barrier function are associated with reproductive and metabolic defects in women with polycystic ovary syndrome (PCOS): A pilot study. PLoS ONE 2017, 12, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Qi, Y.; Yang, X.; Zhao, L.; Wen, S.; Liu, Y.; Tang, L. Association between polycystic ovary syndrome and gut microbiota. PLoS ONE 2016, 11, e0153196. [Google Scholar] [CrossRef] [PubMed]
- Karamali, M.; Eghbalpour, S.; Rajabi, S.; Jamilian, M.; Bahmani, F.; Tajabadi-Ebrahimi, M.; Keneshlou, F.; Mirhashemi, S.M.; Chamani, M.; Hashem Gelougerdi, S.; et al. Effects of Probiotic Supplementation on Hormonal Profiles, Biomarkers of Inflammation and Oxidative Stress in Women With Polycystic Ovary Syndrome: A Randomized, Double-Blind, Placebo-Controlled Trial. Arch. Iran. Med. 2018, 21, 1–7. [Google Scholar] [PubMed]
- Maktabi, M.; Chamani, M.; Asemi, Z. The Effects of Vitamin D Supplementation on Metabolic Status of Patients with Polycystic Ovary Syndrome: A Randomized, Double-Blind, Placebo-Controlled Trial. Horm. Metab. Res. 2017, 49, 493–498. [Google Scholar] [CrossRef]
- Raja-Khan, N.; Shah, J.; Stetter, C.M.; Lott, M.E.J.; Kunselman, A.R.; Dodson, W.C.; Legro, R.S. High-dose vitamin D supplementation and measures of insulin sensitivity in polycystic ovary syndrome: A randomized, controlled pilot trial. Fertil. Steril. 2014, 101, 1740–1746. [Google Scholar] [CrossRef] [PubMed]
- Xue, Y.; Xu, P.; Xue, K.; Duan, X.; Cao, J.; Luan, T.; Li, Q.; Gu, L. Effect of vitamin D on biochemical parameters in polycystic ovary syndrome women: A meta-analysis. Arch. Gynecol. Obstet. 2017, 295, 487–496. [Google Scholar] [CrossRef]
- Liao, D.; Zhong, C.; Li, C.; Mo, L.; Liu, Y. Meta-analysis of the effects of probiotic supplementation on glycemia, lipidic profiles, weight loss and C-reactive protein in women with polycystic ovarian syndrome. Minerva Med. 2018, 109, 479–487. [Google Scholar] [CrossRef]
- Laganà, A.S.; Vitale, S.G.; Ban Frangež, H.; Vrtačnik-Bokal, E.; D’Anna, R. Vitamin D in human reproduction: The more, the better? An evidence-based critical appraisal. Eur. Rev. Med. Pharmacol. Sci. 2017, 21, 4243–4251. [Google Scholar]
- Monastra, G.; De Grazia, S.; De Luca, L.; Vittorio, S.; Unfer, V. Vitamin D: A steroid hormone with progesterone-like activity. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 2502–2512. [Google Scholar] [CrossRef]
- Akbari, M.; Ostadmohammadi, V.; Lankarani, K.B.; Tabrizi, R.; Kolahdooz, F.; Heydari, S.T.; Kavari, S.H.; Mirhosseini, N.; Mafi, A.; Dastorani, M.; et al. The Effects of Vitamin D Supplementation on Biomarkers of Inflammation and Oxidative Stress among Women with Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Horm. Metab. Res. 2018, 50, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Ma, T.; Cui, P.; Tamadon, A.; He, S.; Huo, C.; Yierfulati, G.; Xu, X.; Hu, W.; Li, X.; et al. Diversity of the gut microbiota in dihydrotestosterone-induced PCOS rats and the pharmacologic effects of diane-35, probiotics, and berberine. Front. Microbiol. 2019, 10, 175. [Google Scholar] [CrossRef] [PubMed]
- Kassaian, N.; Feizi, A.; Aminorroaya, A.; Jafari, P.; Ebrahimi, M.T.; Amini, M. The effects of probiotics and synbiotic supplementation on glucose and insulin metabolism in adults with prediabetes: A double-blind randomized clinical trial. Acta Diabetol. 2018, 55, 1019–1028. [Google Scholar] [CrossRef] [PubMed]
- Ahmadi, S.; Jamilian, M.; Karamali, M.; Tajabadi-Ebrahimi, M.; Jafari, P.; Taghizadeh, M.; Memarzadeh, M.R.; Asemi, Z. Probiotic supplementation and the effects on weight loss, glycaemia and lipid profiles in women with polycystic ovary syndrome: A randomized, double-blind, placebo-controlled trial. Hum. Fertil. 2017, 20, 254–261. [Google Scholar] [CrossRef] [PubMed]
- Laitinen, K.; Poussa, T.; Isolauri, E. Probiotics and dietary counselling contribute to glucose regulation during and after pregnancy: A randomised controlled trial. Br. J. Nutr. 2009, 101, 1679–1687. [Google Scholar] [CrossRef] [PubMed]
- Andreasen, A.S.; Larsen, N.; Pedersen-Skovsgaard, T.; Berg, R.M.G.; Mller, K.; Svendsen, K.D.; Jakobsen, M.; Pedersen, B.K. Effects of Lactobacillus acidophilus NCFM on insulin sensitivity and the systemic inflammatory response in human subjects. Br. J. Nutr. 2010, 104, 1831–1838. [Google Scholar] [CrossRef] [PubMed]
- Barreto, F.M.; Colado Simão, A.N.; Morimoto, H.K.; Batisti Lozovoy, M.A.; Dichi, I.; Helena da Silva Miglioranza, L. Beneficial effects of Lactobacillus plantarum on glycemia and homocysteine levels in postmenopausal women with metabolic syndrome. Nutrition 2014, 30, 939–942. [Google Scholar] [CrossRef]
- Kocsis, T.; Molnár, B.; Németh, D.; Hegyi, P.; Szakács, Z.; Bálint, A.; Garami, A.; Soós, A.; Márta, K.; Solymár, M. Probiotics have beneficial metabolic effects in patients with type 2 diabetes mellitus: A meta-analysis of randomized clinical trials. Sci. Rep. 2020, 10, 1–14. [Google Scholar] [CrossRef]
- Ardeshirlarijani, E.; Tabatabaei-Malazy, O.; Mohseni, S.; Qorbani, M.; Larijani, B.; Baradar Jalili, R. Effect of probiotics supplementation on glucose and oxidative stress in type 2 diabetes mellitus: A meta-analysis of randomized trials. DARU J. Pharm. Sci. 2019, 27, 827–837. [Google Scholar] [CrossRef]
- Shoaei, T.; Heidari-Beni, M.; Tehrani, H.G.; Feizi, A.; Esmaillzadeh, A.; Askari, G. Effects of probiotic supplementation on pancreatic β‑cell function and c‑reactive protein in women with polycystic ovary syndrome: A randomized double‑blind placebo‑controlled clinical trial. Int. J. Prev. Med. 2015, 6, 25–30. [Google Scholar] [CrossRef]
- Azziz, R. The hyperandrogenic-insulin-resistant acanthosis nigricans syndrome: Therapeutic response. Fertil. Steril. 1994, 61, 570–572. [Google Scholar] [CrossRef]
- Gulan, T.; Yeernuer, T.; Sui, S.; Mayinuer, N. A rat model of maternal polycystic ovary syndrome shows that exposure to androgens in utero results in dysbiosis of the intestinal microbiota and metabolic disorders of the newborn rat. Med. Sci. Monit. 2019, 25, 9377–9391. [Google Scholar] [CrossRef]
- Falcone, T.; Finegood, D.T.; Fantus, I.G.; Morris, D. Androgen response to endogenous insulin secretion during the frequently sampled intravenous glucose tolerance test in normal and hyperandrogenic women. J. Clin. Endocrinol. Metab. 1990, 71, 1653–1657. [Google Scholar] [CrossRef] [PubMed]
- Tosi, F.; Negri, C.; Brun, E.; Castello, R.; Faccini, G.; Bonora, E.; Muggeo, M.; Toscano, V.; Moghetti, P. Insulin enhances ACTH-stimulated androgen and glucocorticoid metabolism in hyperandrogenic women. Eur. J. Endocrinol. 2011, 164, 197–203. [Google Scholar] [CrossRef]
- Esmaeilinezhad, Z.; Babajafari, S.; Sohrabi, Z.; Eskandari, M.H.; Amooee, S.; Barati-Boldaji, R. Effect of synbiotic pomegranate juice on glycemic, sex hormone profile and anthropometric indices in PCOS: A randomized, triple blind, controlled trial. Nutr. Metab. Cardiovasc. Dis. 2019, 29, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Karimi, E.; Moini, A.; Yaseri, M.; Shirzad, N.; Sepidarkish, M.; Hossein-Boroujerdi, M.; Hosseinzadeh-Attar, M.J. Effects of synbiotic supplementation on metabolic parameters and apelin in women with polycystic ovary syndrome: A randomised double-blind placebo-controlled trial. Br. J. Nutr. 2018, 119, 398–406. [Google Scholar] [CrossRef] [PubMed]
- Samimi, M.; Dadkhah, A.; Haddad Kashani, H.; Tajabadi-Ebrahimi, M.; Hosseini, E.S.; Asemi, Z. The effects of Synbiotic Supplementation on Metabolic Status in Women With Polycystic Ovary Syndrome: A Randomized Double-Blind Clinical Trial. Probiotics Antimicro. Prot. 2019, 1355–1361. [Google Scholar] [CrossRef]
- Yang, J.; Huang, K.; Qin, S.; Wu, X.; Zhao, Z.; Chen, F. Antibacterial action of selenium-enriched probiotics against pathogenic escherichia coli. Dig. Dis. Sci. 2009, 54, 246–254. [Google Scholar] [CrossRef]
- Nido, S.A.; Shituleni, S.A.; Mengistu, B.M.; Liu, Y.; Khan, A.Z.; Gan, F.; Kumbhar, S.; Huang, K. Effects of Selenium-Enriched Probiotics on Lipid Metabolism, Antioxidative Status, Histopathological Lesions, and Related Gene Expression in Mice Fed a High-Fat Diet. Biol. Trace Elem. Res. 2016, 171, 399–409. [Google Scholar] [CrossRef]
- Molan, A.L. Antioxidant and prebiotic activities of selenium-containing green tea. Nutrition 2013, 29, 476–477. [Google Scholar] [CrossRef]
- Razavi, M.; Jamilian, M.; Kashan, Z.F.; Heidar, Z.; Mohseni, M.; Ghandi, Y.; Bagherian, T.; Asemi, Z. Selenium Supplementation and the Effects on Reproductive Outcomes, Biomarkers of Inflammation, and Oxidative Stress in Women with Polycystic Ovary Syndrome. Horm. Metab. Res. 2016, 48, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Mohammad Hosseinzadeh, F.; Hosseinzadeh-Attar, M.J.; Yekaninejad, M.S.; Rashidi, B. Effects of selenium supplementation on glucose homeostasis and free androgen index in women with polycystic ovary syndrome: A randomized, double blinded, placebo controlled clinical trial. J. Trace Elem. Med. Biol. 2016, 34, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Shabani, A.; Noshadian, M.; Jamilian, M.; Chamani, M.; Mohammadi, S.; Asemi, Z. The effects of a novel combination of selenium and probiotic on weight loss, glycemic control and markers of cardio-metabolic risk in women with polycystic ovary syndrome. J. Funct. Foods 2018, 46, 329–334. [Google Scholar] [CrossRef]
- Faghihi, T.; Radfar, M.; Barmal, M.; Amini, P.; Qorbani, M.; Abdollahi, M.; Larijani, B. A randomized, placebo-controlled trial of selenium supplementation in patients with type 2 diabetes: Effects on glucose homeostasis, oxidative stress, and lipid profile. Am. J. Ther. 2014, 21, 491–495. [Google Scholar] [CrossRef]
- Asemi, Z.; Zare, Z.; Shakeri, H.; Sabihi, S.S.; Esmaillzadeh, A. Effect of multispecies probiotic supplements on metabolic profiles, hs-CRP, and oxidative stress in patients with type 2 diabetes. Ann. Nutr. Metab. 2013, 63, 1–9. [Google Scholar] [CrossRef]
- Ahmadi, S.; Jamilian, M.; Tajabadi-Ebrahimi, M.; Jafari, P.; Asemi, Z. The effects of synbiotic supplementation on markers of insulin metabolism and lipid profiles in gestational diabetes: A randomised, double-blind, placebo-controlled trial. Br. J. Nutr. 2016, 116, 1394–1401. [Google Scholar] [CrossRef]
- Fitzpatrick, L.R.; Small, J.; Hoerr, R.A.; Bostwick, E.F.; Maines, L.; Koltun, W.A. In vitro and in vivo effects of the probiotic Escherichia coli strain M-17: Immunomodulation and attenuation of murine colitis. Br. J. Nutr. 2008, 100, 530–541. [Google Scholar] [CrossRef]
- Farnworth, E.R. Kefir a complex probiotic. Food Sci. Technol. Bull. Funct. Foods 2006, 2, 1–17. [Google Scholar] [CrossRef]
- Serafini, F.; Turroni, F.; Ruas-Madiedo, P.; Lugli, G.A.; Milani, C.; Duranti, S.; Zamboni, N.; Bottacini, F.; van Sinderen, D.; Margolles, A.; et al. Kefir fermented milk and kefiran promote growth of Bifidobacterium bifidum PRL2010 and modulate its gene expression. Int. J. Food Microbiol. 2014, 178, 50–59. [Google Scholar] [CrossRef]
- Sonino, N.; Faval, G.A.; Mani, E.; Belluardo, P.; Boscaro, M. Quality of life of hirsute women. Postgrad. Med. J. 1993, 69, 186–189. [Google Scholar] [CrossRef]
- Wild, R.A. Lipid metabolism and hyperandrogenism. Clin. Obstet. Gynecol. 1991, 34, 864–871. [Google Scholar] [CrossRef] [PubMed]
- Wild, R.A.; Alaupovic, P.; Parker, I.J. Lipid and apolipoprotein abnormalities in hirsute women: I. The association with insulin resistance. Am. J. Obstet. Gynecol. 1992, 166, 1191–1197. [Google Scholar] [CrossRef]
- Laughlin, G.A.; Barrett-Connor, E.; Bergstrom, J. Low serum testosterone and mortality in older men. J. Clin. Endocrinol. Metab. 2008, 93, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Araujo, A.B.; Dixon, J.M.; Suarez, E.A.; Murad, M.H.; Guey, L.T.; Wittert, G.A. Endogenous testosterone and mortality in men: A systematic review and meta-analysis. J. Clin. Endocrinol. Metab. 2011, 96, 3007–3019. [Google Scholar] [CrossRef] [PubMed]
- Corona, G.; Rastrelli, G.; Monami, M.; Guay, A.; Buvat, J.; Sforza, A.; Forti, G.; Mannucci, E.; Maggi, M. Hypogonadism as a risk factor for cardiovascular mortality in men: A meta-analytic study. Eur. J. Endocrinol. 2011, 165, 687–701. [Google Scholar] [CrossRef] [PubMed]
- Ruige, J.B.; Mahmoud, A.M.; De Bacquer, D.; Kaufman, J.M. Endogenous testosterone and cardiovascular disease in healthy men: A meta-analysis. Heart 2011, 97, 870–875. [Google Scholar] [CrossRef] [PubMed]
- Penn, C.A.; Chan, J.; Mesaros, C.; Snyder, N.W.; Rader, D.J.; Sammel, M.D.; Dokras, A. Association of serum androgens and coronary artery calcium scores in women. Fertil. Steril. 2019, 112, 586–593. [Google Scholar] [CrossRef]
- Diamondf, M.P.; Grainger, D.A.; Laudano, A.J.; Starick-Zych, K.; Defronzo, R.A. Effect of acute physiological elevations of insulin on circulating androgen levels in nonobese women. J. Clin. Endocrinol. Metab. 1991, 72, 883–887. [Google Scholar] [CrossRef]
- Kim, Y.A.; Keogh, J.B.; Clifton, P.M. Probiotics, prebiotics, synbiotics and insulin sensitivity. Nutr. Res. Rev. 2017, 31, 35–51. [Google Scholar] [CrossRef]
- Raygan, F.; Ostadmohammadi, V.; Asemi, Z. The effects of probiotic and selenium co-supplementation on mental health parameters and metabolic profiles in type 2 diabetic patients with coronary heart disease: A randomized, double-blind, placebo-controlled trial. Clin. Nutr. 2019, 38, 1594–1598. [Google Scholar] [CrossRef]
| Treatment | Study Population | Relevant Outcomes | Reference |
|---|---|---|---|
| Lactobacillus | PCOS 1 rats | Improvement on estrous cycles, reduction of androgen biosynthesis, normalization of ovaries, GM 2 restoration, reduction of Prevotella | [156] |
| L. acidophilus, L. casei, B. bifidum | PCOS women | Reduction of total testosterone, increase of SHBG 3, decrease of m-FG scores | [157] |
| L. acidophilus, L. reuteri, B. bifidum and Vitamin D | PCOS women | Reduction of total testosterone and hirsutism | [149] |
| E. faecali, L. reuteri, Bifidobacterium | PCOS rats | Improvement in reproductive function and GM restoration | [165] |
| L. acidophilus, L. casei, B. bifidum | PCOS women | Reduced fasting plasma glucose, insulin concentrations and insulin resistance. Increased insulin sensitivity | [167] |
| L. acidophilus, L. casei, L. rhamnosus, L. bulgaricus, L. breve, B. longum, S. thermophiles | PCOS women | Reduced FBS 4, reduced insulin levels and reduced insulin resistance | [173] |
| L. plantarum | Postmenopausal women | Reduced glucose levels | [170] |
| L. rhamnosus, B. lactis | Postpartum period women | Reduced blood glucose concentrations, improved glucose tolerance, reduced insulin concentrations and increased insulin sensitivity | [168] |
| Treatment | Study Population | Relevant Outcomes | Reference |
|---|---|---|---|
| Lactobacillus and pomegranate juice | PCOS 1 women | Reduced testosterone levels, increased insulin resistance and improved anthropometric measurements | [178] |
| L. bifidum, L. acidophilus, L. casei and inulin | PCOS women | Reduced m-FG scores but did not affect the clinical picture of hirsutism | [19] |
| Lactobacillus, Bifidobacterium and Selenium | PCOS women | Reduced total testosterone and hirsutism | [150] |
| L. bifidum, L. acidophilus, L. casei and inulin | PCOS women | Improved insulin metabolism markers but did not influence FBS 2 | [180] |
| Lactobacillus, Bifidobacterium and inulin | Prediabetics | Decreased fasting insulin levels and fasting plasma glucose | [166] |
| L. plantarum and inulin | Diabetic rats | Improved insulin resistance, hypothalamic levels of insulin and leptin | [80] |
| L. salivarius UBL S22 and fructo-oligosaccharides | Healthy participants | Improved insulin sensitivity | [27] |
| L. bulgaricus, L. acidophilus, L. casei, L. rhamnosus, B. longum, B. breve, S. thermophilus and inulin | PCOS women | No effects on fasting insulin levels | [179] |
| L. acidophilus, L. reuteri, L. fermentum, B. bifidum and selenium | PCOS women | Reduced insulin levels and insulin resistance. Increased insulin sensitivity | [186] |
| L. acidophilus, L. casei, B. bifidum and inulin | Gestational diabetics | Decreased insulin levels and insulin resistance. Increased insulin sensitivity | [189] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lolou, V. The Role of Probiotics and Synbiotics on Hirsutism. Fermentation 2021, 7, 10. https://doi.org/10.3390/fermentation7010010
Lolou V. The Role of Probiotics and Synbiotics on Hirsutism. Fermentation. 2021; 7(1):10. https://doi.org/10.3390/fermentation7010010
Chicago/Turabian StyleLolou, Vasiliki. 2021. "The Role of Probiotics and Synbiotics on Hirsutism" Fermentation 7, no. 1: 10. https://doi.org/10.3390/fermentation7010010
APA StyleLolou, V. (2021). The Role of Probiotics and Synbiotics on Hirsutism. Fermentation, 7(1), 10. https://doi.org/10.3390/fermentation7010010





