Photodynamic Therapy with Natural Photosensitizers in the Management of Periodontal Disease Induced in Rats
Abstract
1. Introduction
2. Results and Discussion
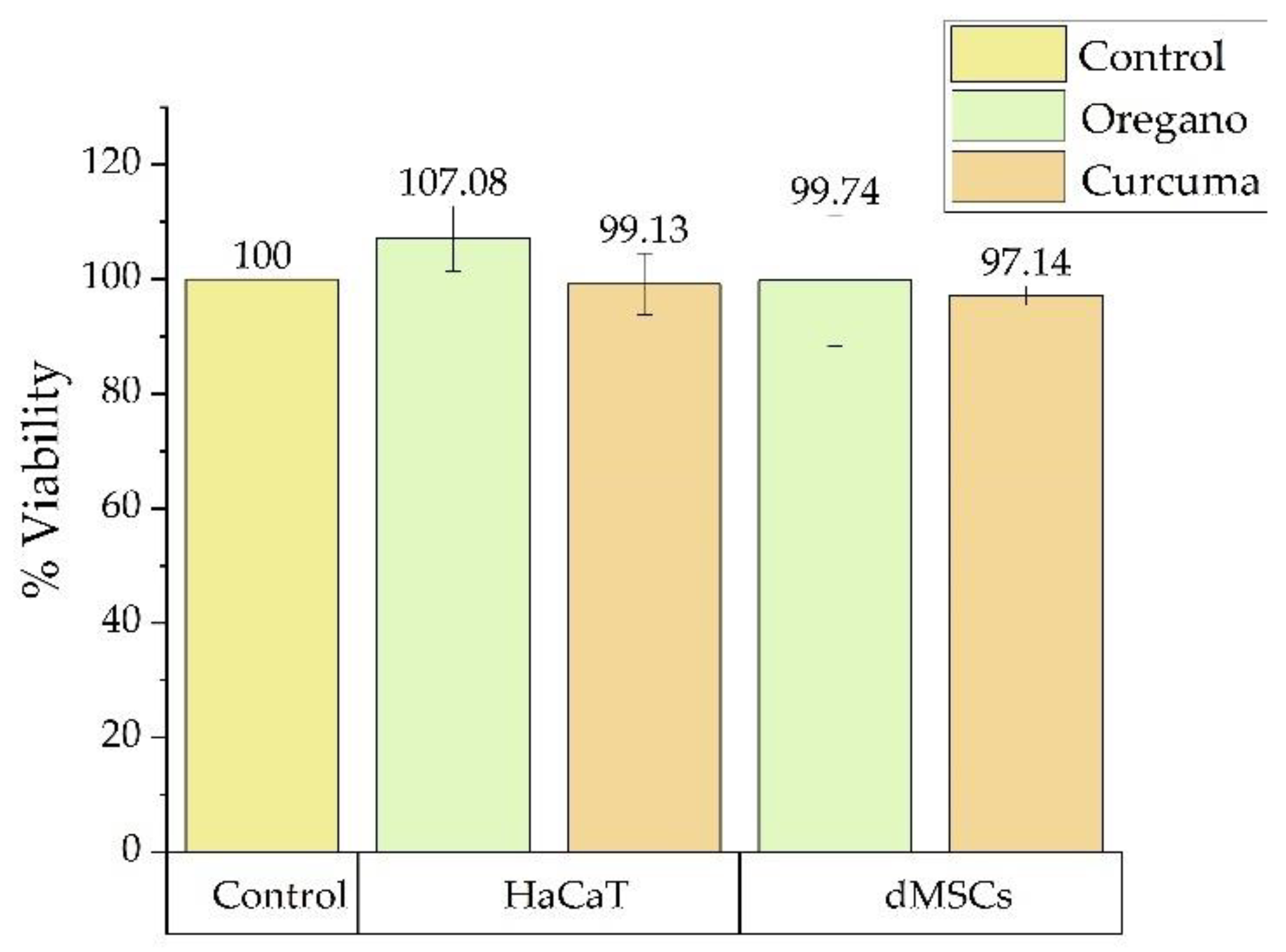
2.1. Cytotoxicity
2.2. Clinical Evaluation
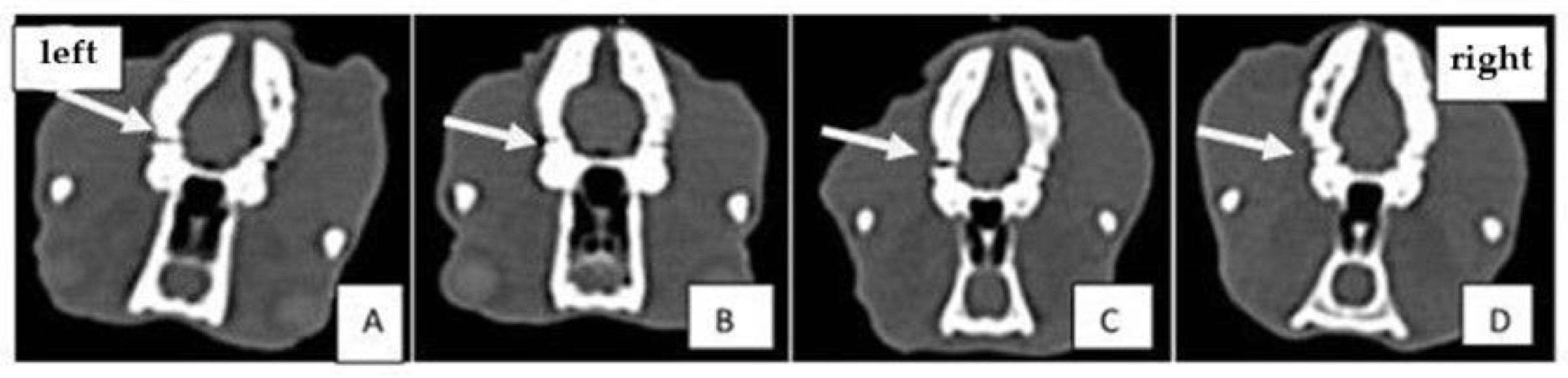
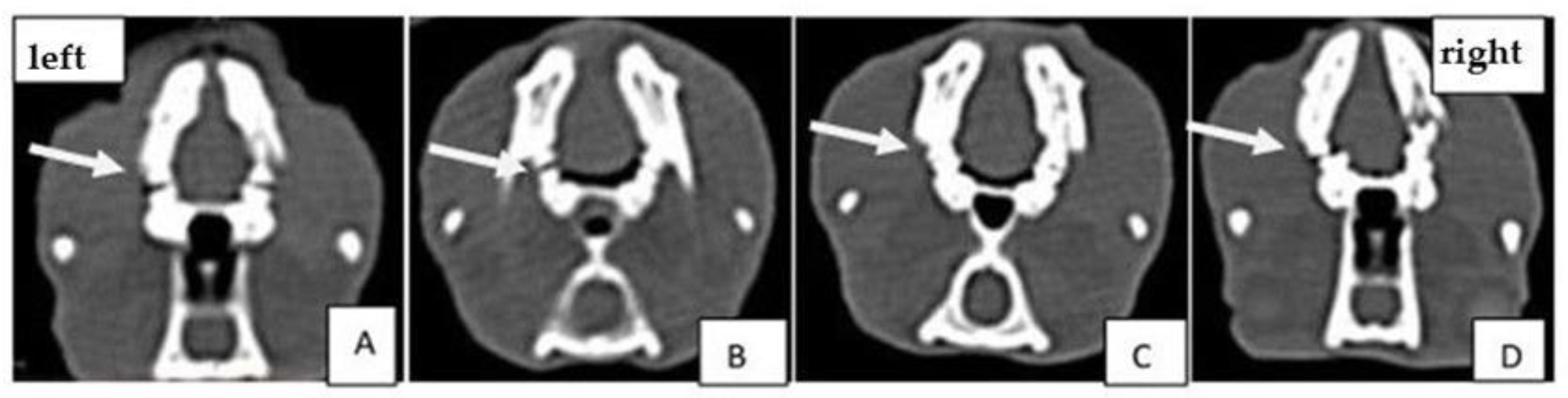
2.3. Computed Tomography (CT) Analysis
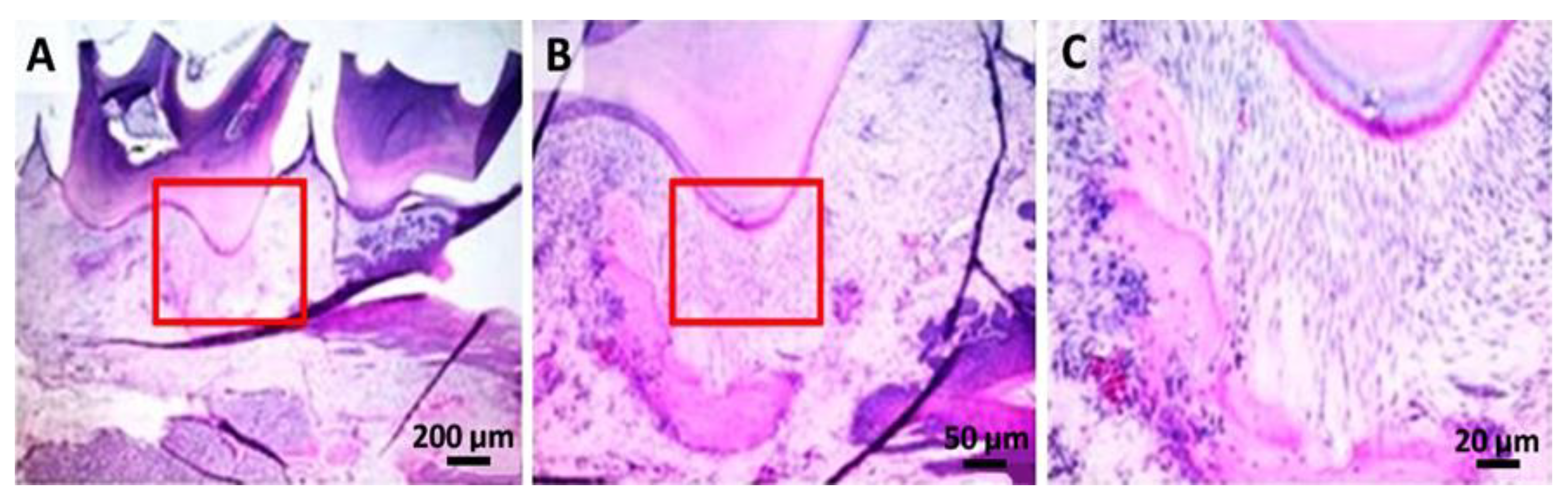
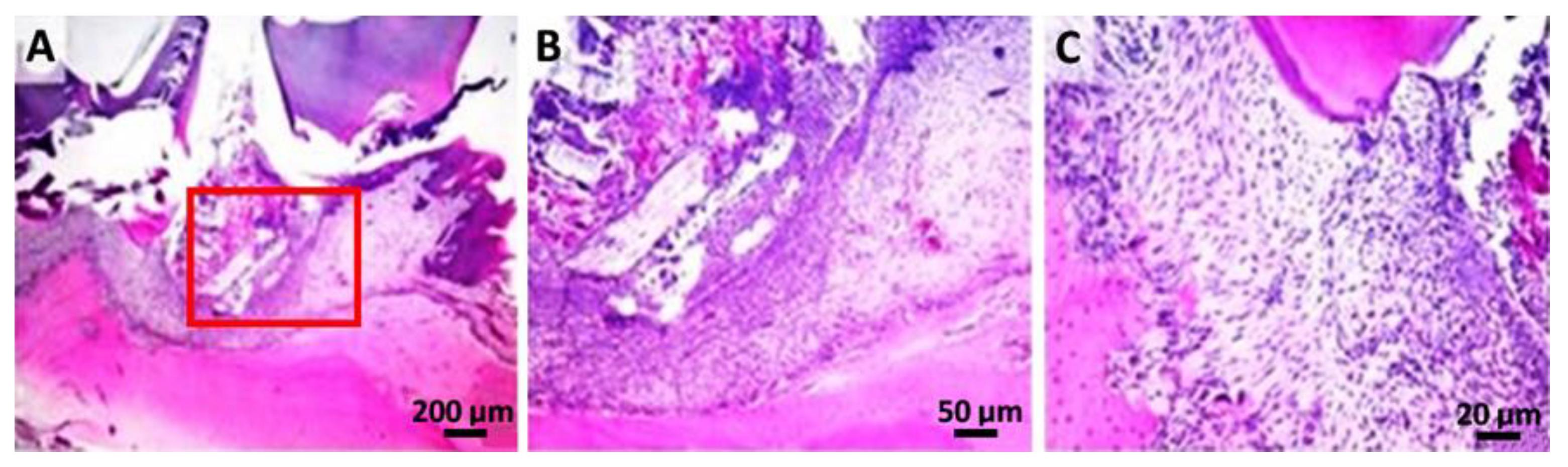
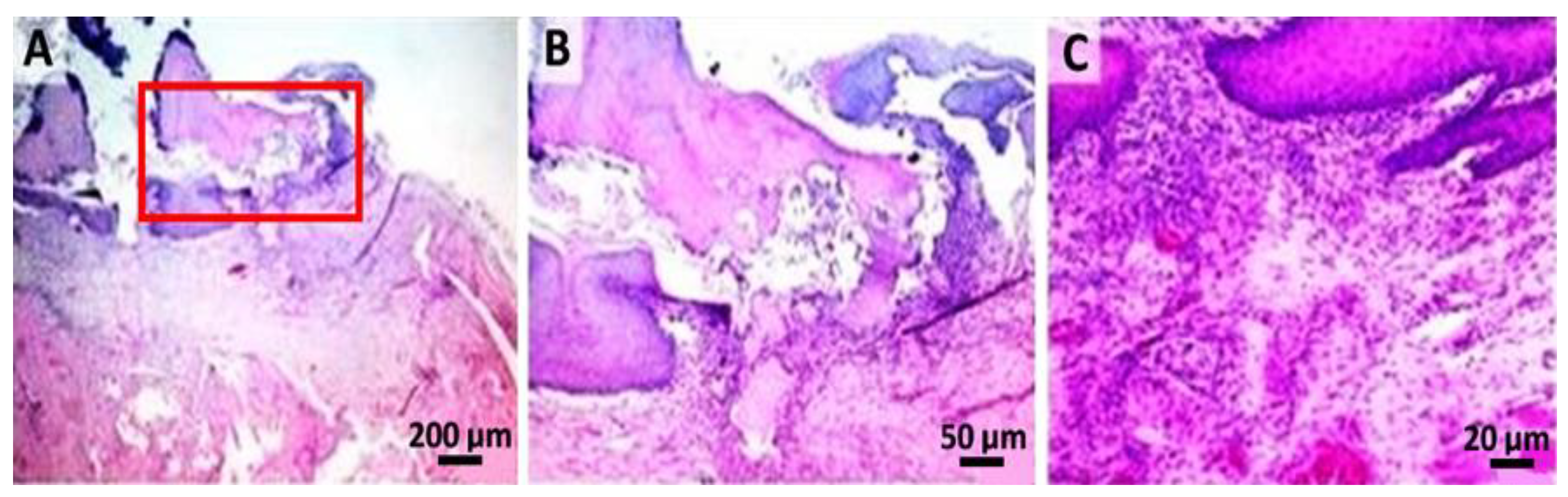
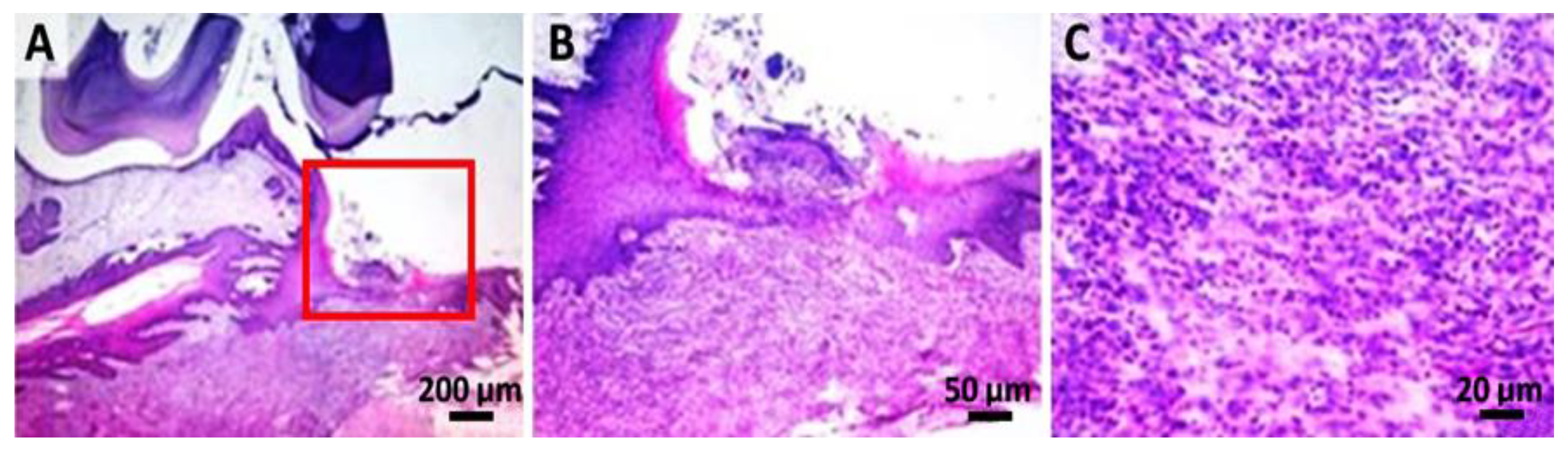
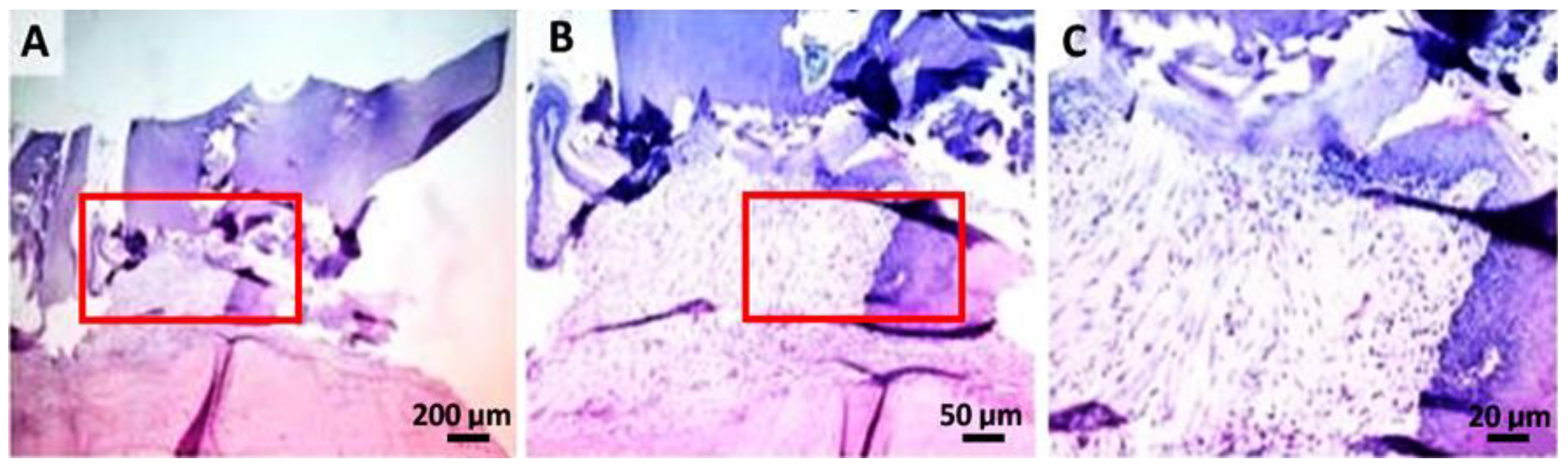
2.4. Histological Analysis
2.5. Complete Blood Count
3. Conclusions
4. Materials and Methods
4.1. Statistical Analysis
4.2. Pre-Clinical Study
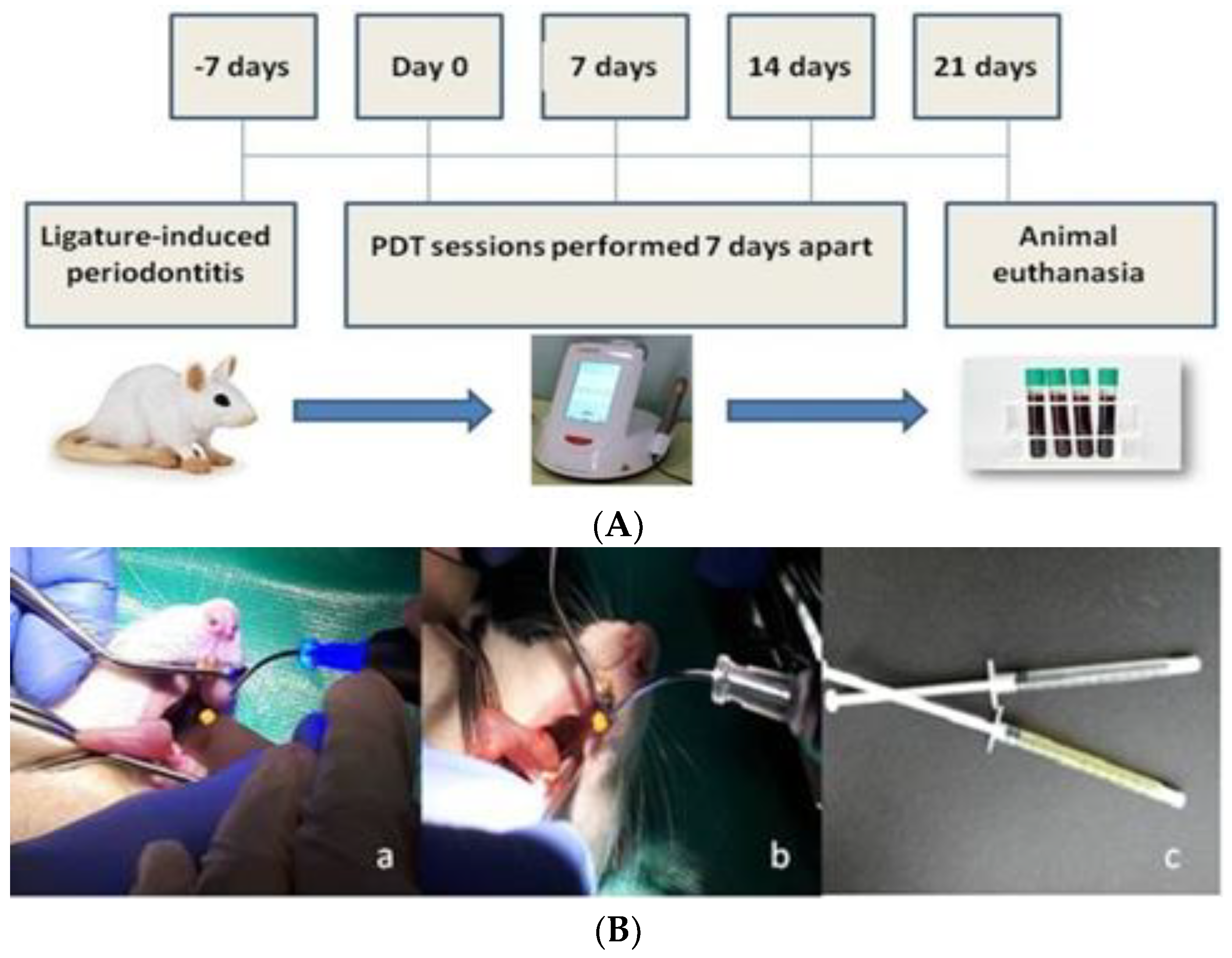
4.3. Experimental Design
4.4. Computed Tomography (CT) Analysis
4.5. Complete Blood Count and Biochemistry
4.6. Histological Analysis
4.7. Statistical Analysis of the Data
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kömerik, N.; Nakanishi, H.; MacRobert, A.J.; Henderson, B.; Speight, P.; Wilson, M. In Vivo Killing of Porphyromonas gingivalis by Toluidine Blue-Mediated Photosensitization in an Animal Model. Antimicrob. Agents Chemother. 2003, 47, 932–940. [Google Scholar] [CrossRef] [PubMed]
- Rajapakse, P.S.; O’Brien-Simpson, N.M.; Slakeski, N.; Hoffmann, B.; Reynolds, E.C. Immunization with the RgpA-Kgp Proteinase-Adhesin Complexes of Porphyromonas gingivalis Protects against Periodontal Bone Loss in the Rat Periodontitis Model. Infect. Immun. 2002, 70, 2480–2486. [Google Scholar] [CrossRef] [PubMed]
- Nessa, N.; Kobara, M.; Toba, H.; Adachi, T.; Yamamoto, T.; Kanamura, N.; Pezzotti, G.; Nakata, T. Febuxostat Attenuates the Progression of Periodontitis in Rats. Pharmacology 2021, 106, 294–304. [Google Scholar] [CrossRef] [PubMed]
- Prates, R.A.; Yamada, A.M.; Suzuki, L.C.; França, C.M.; Cai, S.; Mayer, M.P.A.; Ribeiro, A.C.; Ribeiro, M.S. Histomorphometric and Microbiological Assessment of Photodynamic Therapy as an Adjuvant Treatment for Periodontitis: A Short-Term Evaluation of Inflammatory Periodontal Conditions and Bacterial Reduction in a Rat Model. Photomed. Laser Surg. 2011, 29, 835–844. [Google Scholar] [CrossRef]
- Graves, D.T.; Fine, D.; Teng, Y.T.A.; Van Dyke, T.E.; Hajishengallis, G. The use of rodent models to investigate host-bacteria interactions related to periodontal diseases. J. Clin. Periodontol. 2008, 35, 89–105. [Google Scholar] [CrossRef]
- Wang, H.H.; Lee, H.M.; Raja, V.; Hou, W.; Iacono, V.J.; Scaduto, J.; Johnson, F.; Golub, L.M.; Gu, Y. Enhanced Efficacy of Chemically Modified Curcumin in Experimental Periodontitis: Systemic Implications. J. Exp. Pharmacol. 2019, 11, 1–14. [Google Scholar] [CrossRef]
- Birang, E.; Talebi Ardekani, M.R.; Rajabzadeh, M.; Sarmadi, G.; Birang, R.; Gutknecht, N. Comparison of Er:YAG Laser andUltrasonic Scaler in the Treatment of Moderate Chronic Periodontitis: A Randomized Clinical Trial. J. Lasers Med. Sci. 2017, 8, 136–142. [Google Scholar] [CrossRef]
- Hosseini, N.; Yazdanpanah, S.; Saki, M.; Rezazadeh, F.; Ghapanchi, J.; Zomorodian, K. Susceptibility of Candida albicans and Candida dubliniensis to photodynamic therapy using four dyes as the photosensitizer. J. Dent. 2016, 17, 354–360. [Google Scholar]
- Sperandio, F.; Huang, Y.Y.; Hamblin, M. Antimicrobial photodynamic therapy to kill Gram-negative bacteria. Recent Pat. Anti-Infect. Drug Discov. 2013, 8, 108–120. [Google Scholar] [CrossRef]
- Lara Alves, L.V.G.; Curylofo-Zotti, F.A.; Borsatto, M.C.; de Souza Salvador, S.L.; Valério, R.A.; Souza-Gabriel, A.E. Influence of antimicrobial photodynamic therapy in carious lesion. Randomized split-mouth clinical trial in primary molar. Photodiagnosis Photodyn. Ther. 2019, 26, 124–130. [Google Scholar] [CrossRef]
- Ishiyama, K.; Nakamura, K.; Kano, T.; Niwano, Y. Bactericidal Action of Photodynamic Antimicrobial Chemotherapy (PACT) with Photosensitizers Used as Plaque-Disclosing Agents against Experimental Biofilm. Biocontrol Sci. 2016, 21, 187–191. [Google Scholar] [CrossRef][Green Version]
- Misba, L.; Zaidi, S.; Khan, A.U. A comparison of antibacterial and antibiofilm efficacy of phenothiazinium dyes between Gram positive and Gram negative bacterial biofilm. Photodiagnosis Photodyn. Ther. 2017, 18, 24–33. [Google Scholar] [CrossRef]
- Dascalu (Rusu), M.L.; Sarosi, C.; Moldovan, M.; Badea, M.E. A Study on Revealing Agents in the Context of Photodynamic Therapy in Dental Medicine—A Literature Review. Defect Diffus. Forum 2017, 376, 54–65. [Google Scholar] [CrossRef]
- Dascalu (Rusu), L.M.; Moldovan, M.; Prodan, D.; Ciotlaus, I.; Popescu, V.; Baldea, I.; Carpa, R.; Sava, S.; Chifor, R.; Badea, M.E. Assessment and Characterization of Some New Photosensitizers for Antimicrobial Photodynamic Therapy (aPDT). Materials 2020, 13, 3012. [Google Scholar] [CrossRef]
- Mang, T.S.; Tayal, D.P.; Baier, R. Photodynamic therapy as an alternative treatment for disinfection of bacteria in oral biofilms. Lasers Surg. Med. 2012, 44, 588–596. [Google Scholar] [CrossRef] [PubMed]
- Garcez, A.S.; Ribeiro, M.S.; Tegos, G.P.; Núñez, S.C.; Jorge, A.O.C.; Hamblin, M.R. Antimicrobial photodynamic therapy combined with conventional endodontic treatment to eliminate root canal biofilm infection. Lasers Surg. Med. 2007, 39, 59–66. [Google Scholar] [CrossRef]
- De Almeida, J.M.; Theodoro, L.H.; Bosco, A.F.; Nagata, M.J.H.; Oshiiwa, M.; Garcia, V.G. In vivo effect of photodynamic therapy on periodontal bone loss in dental furcations. J. Periodontol. 2008, 79, 1081–1088. [Google Scholar] [CrossRef] [PubMed]
- Wood, S.; Nattress, B.; Kirkham, J.; Shore, R.; Brookes, S.; Griffiths, J. An in vitro study of the use of photodynamic therapy for the treatment of natural oral plaque biofilms formed in vivo. J. Photochem. Photobiol. B Biol. 1999, 50, 1–7. [Google Scholar] [CrossRef]
- Ghasemi, M.; Etemadi, A.; Nedaei, M.; Chiniforush, N.; Pourhajibagher, M. Antimicrobial efficacy of photodynamic therapy using two different light sources on the titanium-adherent biofilms of Aggregatibacter actinomycetemcomitans: An in vitro study. Photodiagnosis Photodyn. Ther. 2019, 26, 85–89. [Google Scholar] [CrossRef]
- Tokubo, L.M.; Rosalen, P.L.; de Cássia Orlandi Sardi, J.; Freires, I.A.; Fujimaki, M.; Umeda, J.E. Antimicrobial effect of photodynamic therapy using erythrosine/methylene blue combination on Streptococcus mutans biofilm. Photodiagnosis Photodyn. Ther. 2018, 23, 94–98. [Google Scholar] [CrossRef] [PubMed]
- Fang-Yen, C.; Gabel, C.V.; Samuel, A.D.T.; Bargmann, C.I.; Avery, L. Laser microsurgery in Caenorhabditis elegans. Methods Cell Biol. 2012, 107, 177–206. [Google Scholar] [PubMed]
- Cieplik, F.; Tabenski, L.; Buchalla, W.; Maisch, T. Antimicrobial photodynamic therapy for inactivation of biofilms formed by oral key pathogens. Front. Microbiol. 2014, 5, 405. [Google Scholar] [CrossRef] [PubMed]
- Yan, S.; Huang, Q.; Song, X.; Chen, Z.; Huang, M.; Zhang, J. A series of photosensitizers with incremental positive electric charges for photodynamic antitumor therapy. RSC Adv. 2019, 9, 24560–24567. [Google Scholar] [CrossRef]
- Yoo, J.O.; Ha, K.S. New insights into the mechanisms for photodynamic therapy-induced cancer cell death. Int. Rev. Cell. Mol. Biol. 2012, 295, 139–174. [Google Scholar]
- Jurenka, J.S. Anti-inflammatory properties of curcumin, a major constituent of Curcuma longa: A review of preclinical and clinical research. Altern. Med. Rev. 2009, 14, 141–153. [Google Scholar]
- Akbik, D.; Ghadiri, M.; Chrzanowski, W.; Rohanizadeh, R. Curcumin as a wound healing agent. Life Sci. 2014, 116, 1–7. [Google Scholar] [CrossRef]
- Mohanty, C.; Sahoo, S.K. Curcumin and its topical formulations for wound healing applications. Drug Discov. Today 2017, 22, 1582–1592. [Google Scholar] [CrossRef]
- Zhang, Y.; McClain, S.A.; Lee, H.M. A Novel Chemically Modified Curcumin “Normalizes” Wound-Healing in Rats with Experimentally Induced Type I Diabetes: Initial Studies. J. Diabetes Res. 2016, 2016, 5782904. [Google Scholar] [CrossRef]
- Nasri, H.; Sahinfard, N.; Rafieian, M.; Rafieian, S.; Shirzad, M.; Rafieian-Kopaei, M. Turmeric: A spice with multifunctional medicinal properties. J. HerbMed Pharmacol. 2014, 3, 5–8. [Google Scholar]
- Xiao, C.J.; Yu, J.; Xie, J.L.; Liu, S.; Li, S. Protective effect and related mechanisms of curcumin in rat experimental periodontitis. Head Face Med. 2018, 14, 12. [Google Scholar] [CrossRef]
- Judžentien, A.; Būdienė, J. Analysis of the chemical composition of flower essential oils from Arnica montana of Lithuanian origin. Chemija 2009, 20, 190–194. [Google Scholar]
- Rostro-Alanis, M.; Báez-González, J.; Torres-Alvarez, C.; Parra-Saldívar, R.; Rodriguez-Rodriguez, J.; Castillo, S. Chemical Composition and Biological Activities of Oregano Essential Oil and Its Fractions Obtained by Vacuum Distillation. Molecules 2019, 24, 1904. [Google Scholar] [CrossRef] [PubMed]
- Etemadi, A.; Hamidain, M.; Parker, S.; Chiniforush, N. Blue Light Photodynamic Therapy with Curcumin and Riboflavin in the Management of Periodontitis: A Systematic Review. J. Lasers Med. Sci. 2021, 12, e15. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira Carvalho, I.; Aparecida Purgato, G.; Soares Píccolo, M.; Ramos Pizziolo, V.; Ribeiro Coelho, R.; Diaz-Muñoz, G.; Alves Nogueira Diaz, M. In vitro anticariogenic and antibiofilm activities of toothpastes formulated with essential oils. Arch. Oral Biol. 2020, 117, 104834. [Google Scholar] [CrossRef] [PubMed]
- Sharifi-Rad, M.; Varoni, E.M.; Iriti, M.; Martore, M.; Setzer, W.N.; Contreras, M.; Salehi, B.; Soltani-Nejad, A.; Rajabi, S.; Tajbakhsh, M.; et al. Carvacrol and human health: A comprehensive review. Phytother. Res. 2018, 32, 1675–1687. [Google Scholar]
- Leyva-López, N.; Gutiérrez-Grijalva, E.P.; Vazquez-Olivo, G.; Heredia, J.B. Essential Oils of Oregano: Biological Activity beyond Their Antimicrobial Properties. Molecules 2017, 22, 989. [Google Scholar] [CrossRef]
- Belinello-Souza, E.L.; Alvarenga, L.H.; Lima-Leal, C.; Almeida, P.; Leite, C.G.; Lima, T.R. Antimicrobial photodynamic therapy combined to periodontal treatment: Experimental model. Photodiagnosis Photodyn. Ther. 2017, 18, 275–278. [Google Scholar] [CrossRef]
- Uslu, M.Ö.; Eltas, A.; Marakoğlu, I.; Dündar, S.; Şahin, K.; Özercan, I.H. Effects of diode laser application on inflammation and mpo in periodontal tissues in a rat model. J. Appl. Oral Sci. 2018, 26, e20170266. [Google Scholar] [CrossRef]
- Lin, P.; Niimi, H.; Ohsugi, Y.; Tsuchiya, Y.; Shimohira, T.; Komatsu, K.; Liu, A.; Shiba, T.; Aoki, A.; Iwata, T.; et al. Application of Ligature-Induced Periodontitis in Mice to Explore the Molecular Mechanism of Periodontal Disease. Int. J. Mol. Sci. 2021, 22, 8900. [Google Scholar] [CrossRef]
- Fernandes, L.A.; Theodoro, L.H.; Martins, T.M.; de Almeida, J.M.; Garcia, V.G. J Effects of diode laser application on inflammation and mpo in periodontal tissues in a rat model. Appl. Oral Sci. 2010, 18, 237–243. [Google Scholar] [CrossRef]
- Robinson, M.; Hart, D.; Pigott, G.H. The effects of diet on the incidence of periodontitis in rats. Lab. Anim. 1991, 25, 247–253. [Google Scholar] [CrossRef]
- Toth, L.A.; Gardiner, T.W. Food and water restriction protocols: Physiological and behavioral considerations. Contemp. Top. Lab. Anim. Sci. 2000, 39, 9–17. [Google Scholar] [PubMed]
- Smith, C.; Jarecki, A. Atlas of Comparative Diagnostic and Experimental Hematology, 2nd ed.; Wiley-Blackwell: Hoboken, NJ, USA, 2013. [Google Scholar]
- Giknis, M.L.A.; Charles, B.; Clifford, D.V.M. Clinical Laboratory Parameters for Crl:CD(SD) Rats; Charles River Lab: Middlesex County, MA, USA, 2008. [Google Scholar]
- Carvalho, A.S.; Napimoga, M.H.; Coelho-Campos, J.; Silva-Filho, V.J.; Thedei, G. Photodynamic therapy reduces bone resorption and decreases inflammatory response in an experimental rat periodontal model. Photomed. Laser Surg. 2011, 29, 735–740. [Google Scholar] [CrossRef] [PubMed]
- Graves, D.T.; Kang, J.; Andriankaja, O.; Wada, K.; Rossa, C. Animal models to study host-bacteria interactions involved in periodontitis. Front. Oral Biol. 2012, 15, 117–132. [Google Scholar]
- Faot, F.; de Camargos G, C.; Duyck, J.; Vandamme, K. Micro-CT analysis of the rodent jaw bone micro-architecture: A systematic review. Bone Rep. 2015, 2, 14–24. [Google Scholar] [CrossRef] [PubMed]
- Garcia, V.G.; Knoll, L.R.; Longo, M.; Novaes, V.C.N.; Assem, N.Z.; Ervolino, E. Effect of the probiotic Saccharomyces cerevisiae on ligature-induced periodontitis in rats. J. Periodontal Res. 2016, 51, 26–37. [Google Scholar] [CrossRef] [PubMed]
- Garcia, V.G.; Erivan, C.G.V.; Fernandes, L.A.; Bosco, A.F.; Nagata, H.M.; Casatti, A.C.; Ervolino, E.; Theodoro, L.H. Adjunctive antimicrobial photodynamic treatment of experimentally induced periodontitis in rats with ovariectomy. J. Periodontol. 2013, 84, 556–565. [Google Scholar] [CrossRef]
- Flecknell, P. Laboratory Animal Anaesthesia, 3rd ed.; Academic Press: Cambridge, MA, USA, 2009. [Google Scholar]

| Body Weight | ||||
|---|---|---|---|---|
| Crt. No. | Groups | Initially (g) | Final (g) | Weight Gain (%) |
| 1. | Control group (M) | 452 ± 32.71 | 551 ± 24.14 | 21.9 |
| 2. | Periodontitis group (P) | 491.4 ± 25.47 | 530.2 ± 29.07 | 7.85 |
| 3. | Curcuma group (GC) | 475.6 ± 10.8 | 570 ± 14.85 **, ^^ | 19.84 |
| 4. | Oregano group (GO) | 516 ± 17.92 | 576.4 ± 26.73 *, ^^ | 11.70 |
| 5. | Laser group (L) | 438 ± 10.74 | 513.2 ± 27.39 | 17.16 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dascalu, L.M.; Moldovan, M.; Sarosi, C.; Sava, S.; Dreanca, A.; Repciuc, C.; Purdoiu, R.; Nagy, A.; Badea, M.E.; Paun, A.G.; et al. Photodynamic Therapy with Natural Photosensitizers in the Management of Periodontal Disease Induced in Rats. Gels 2022, 8, 134. https://doi.org/10.3390/gels8020134
Dascalu LM, Moldovan M, Sarosi C, Sava S, Dreanca A, Repciuc C, Purdoiu R, Nagy A, Badea ME, Paun AG, et al. Photodynamic Therapy with Natural Photosensitizers in the Management of Periodontal Disease Induced in Rats. Gels. 2022; 8(2):134. https://doi.org/10.3390/gels8020134
Chicago/Turabian StyleDascalu (Rusu), Laura Monica, Marioara Moldovan, Codruta Sarosi, Sorina Sava, Alexandra Dreanca, Calin Repciuc, Robert Purdoiu, Andras Nagy, Mîndra Eugenia Badea, Ariadna Georgiana Paun, and et al. 2022. "Photodynamic Therapy with Natural Photosensitizers in the Management of Periodontal Disease Induced in Rats" Gels 8, no. 2: 134. https://doi.org/10.3390/gels8020134
APA StyleDascalu, L. M., Moldovan, M., Sarosi, C., Sava, S., Dreanca, A., Repciuc, C., Purdoiu, R., Nagy, A., Badea, M. E., Paun, A. G., Badea, I. C., & Chifor, R. (2022). Photodynamic Therapy with Natural Photosensitizers in the Management of Periodontal Disease Induced in Rats. Gels, 8(2), 134. https://doi.org/10.3390/gels8020134







