Natural Bletilla striata Polysaccharide-Based Hydrogels for Accelerating Hemostasis
Abstract
1. Introduction
2. Results and Discussion
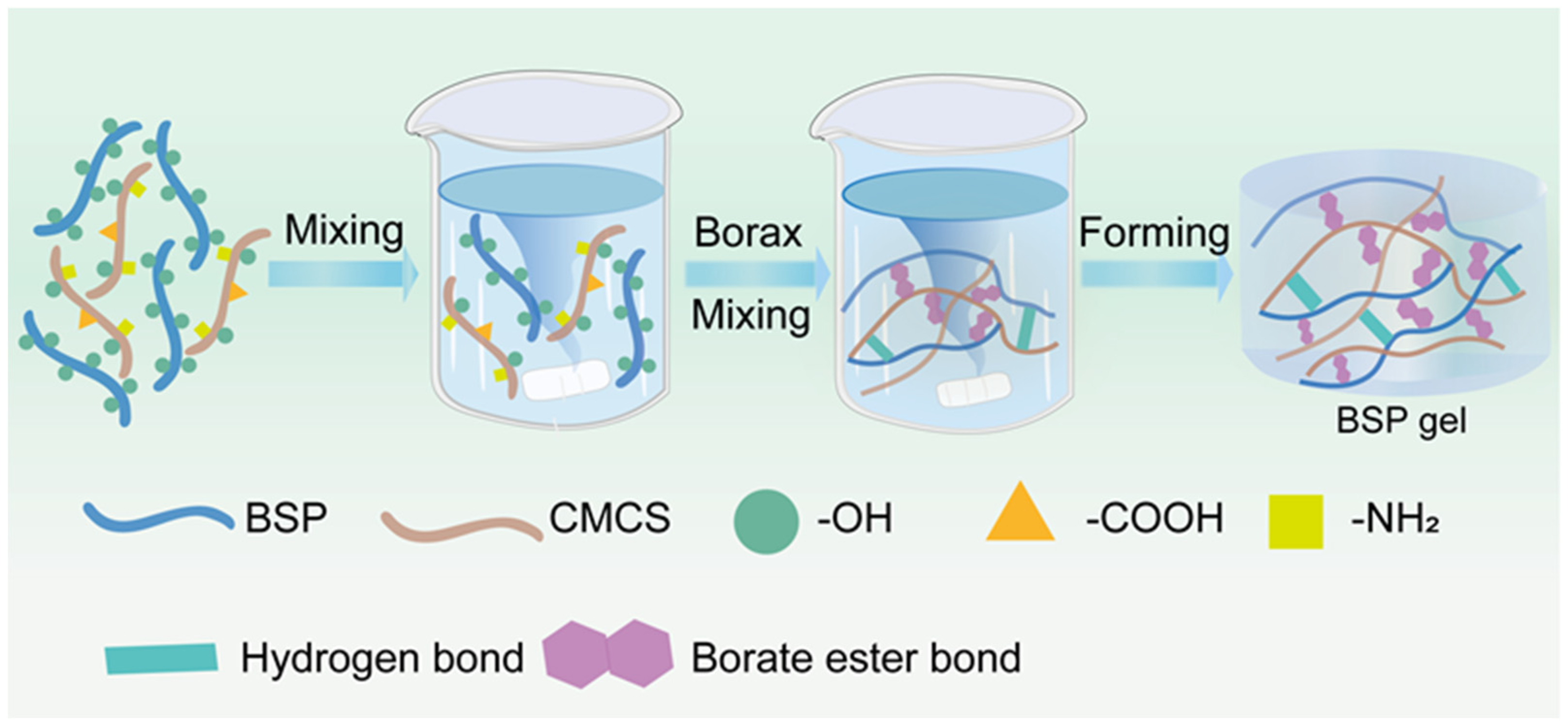
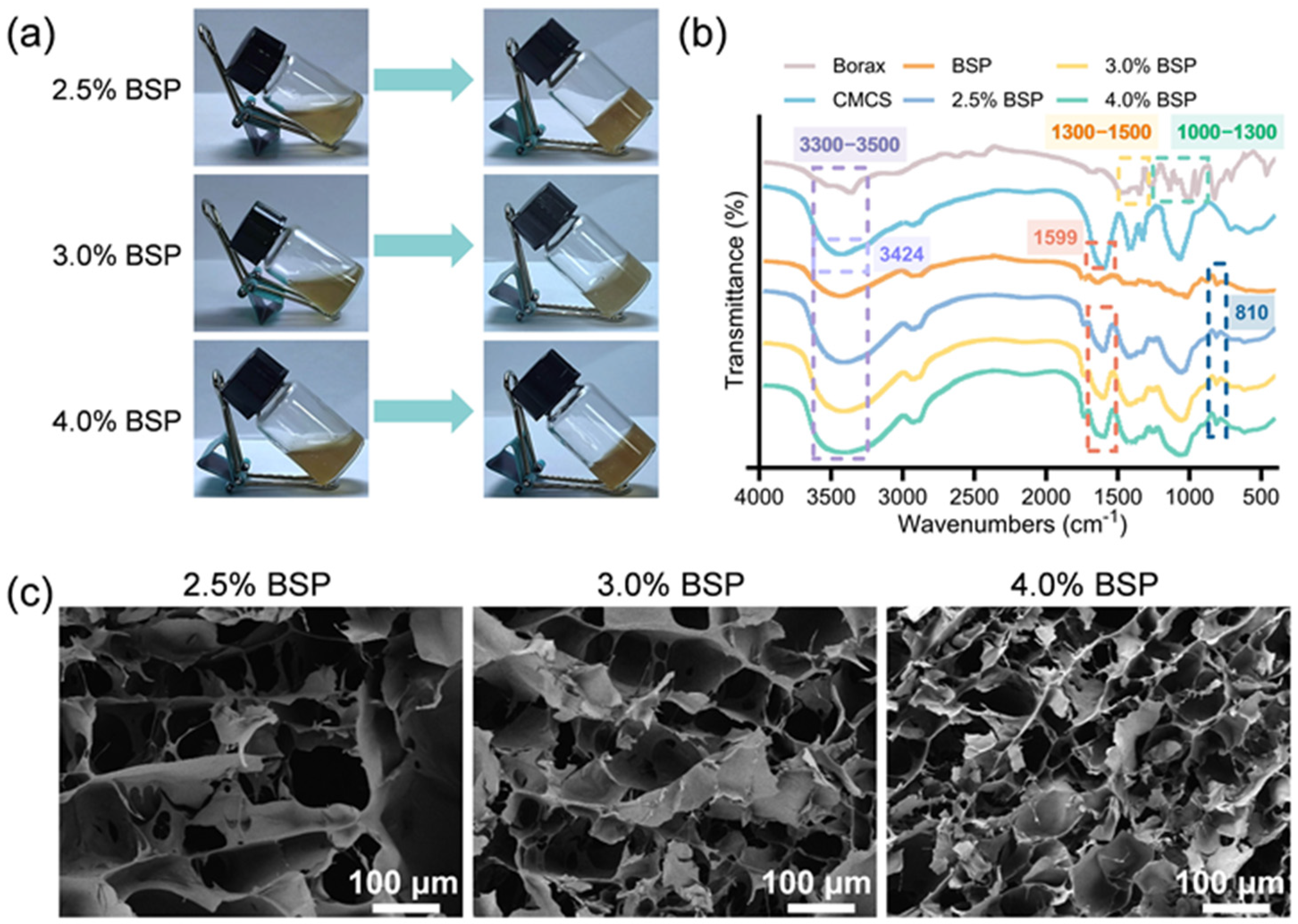
2.1. Synthesis and Characterization of BSP Hydrogel
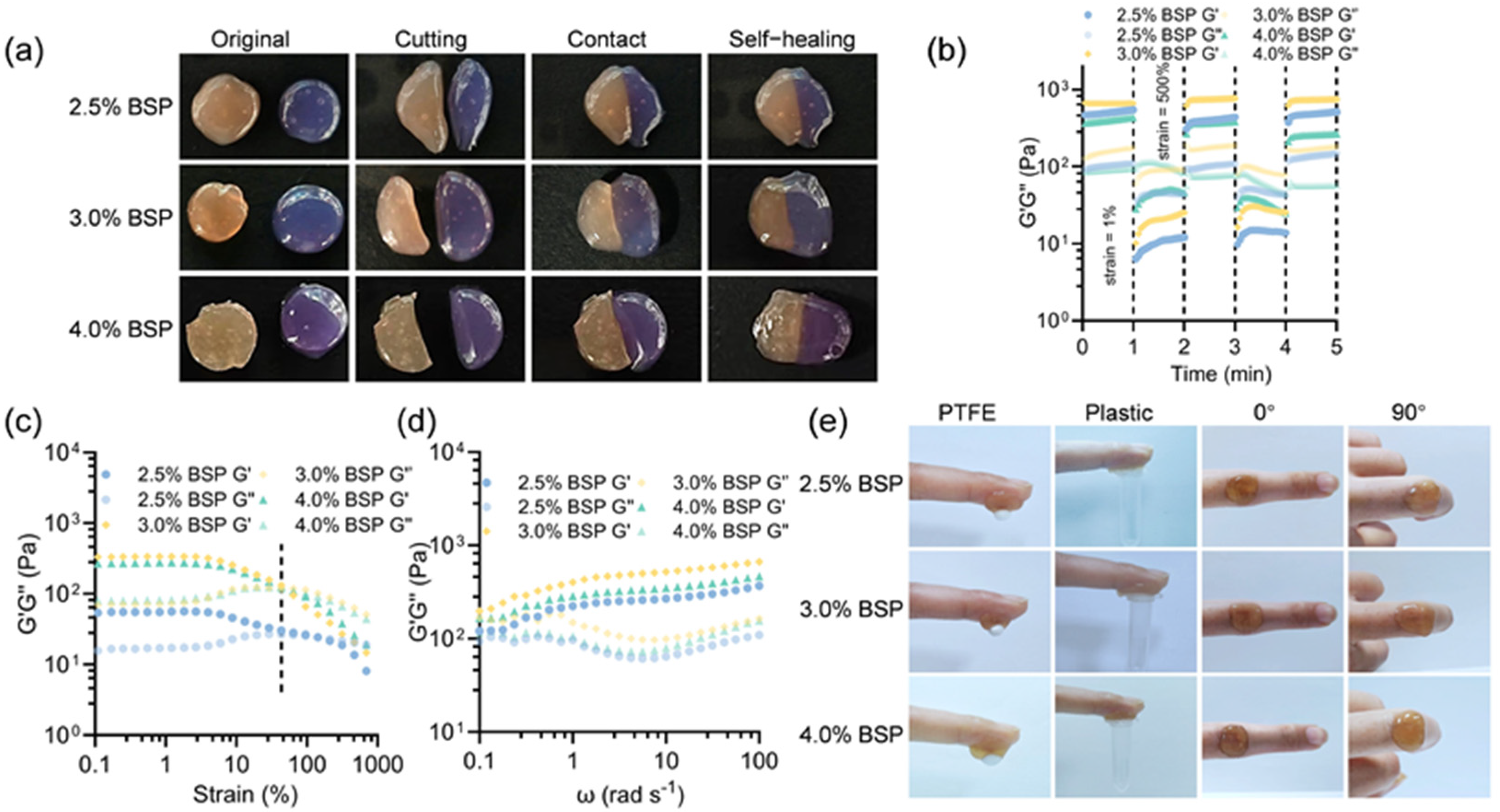
2.2. Rheological Behaviors of BSP Hydrogels
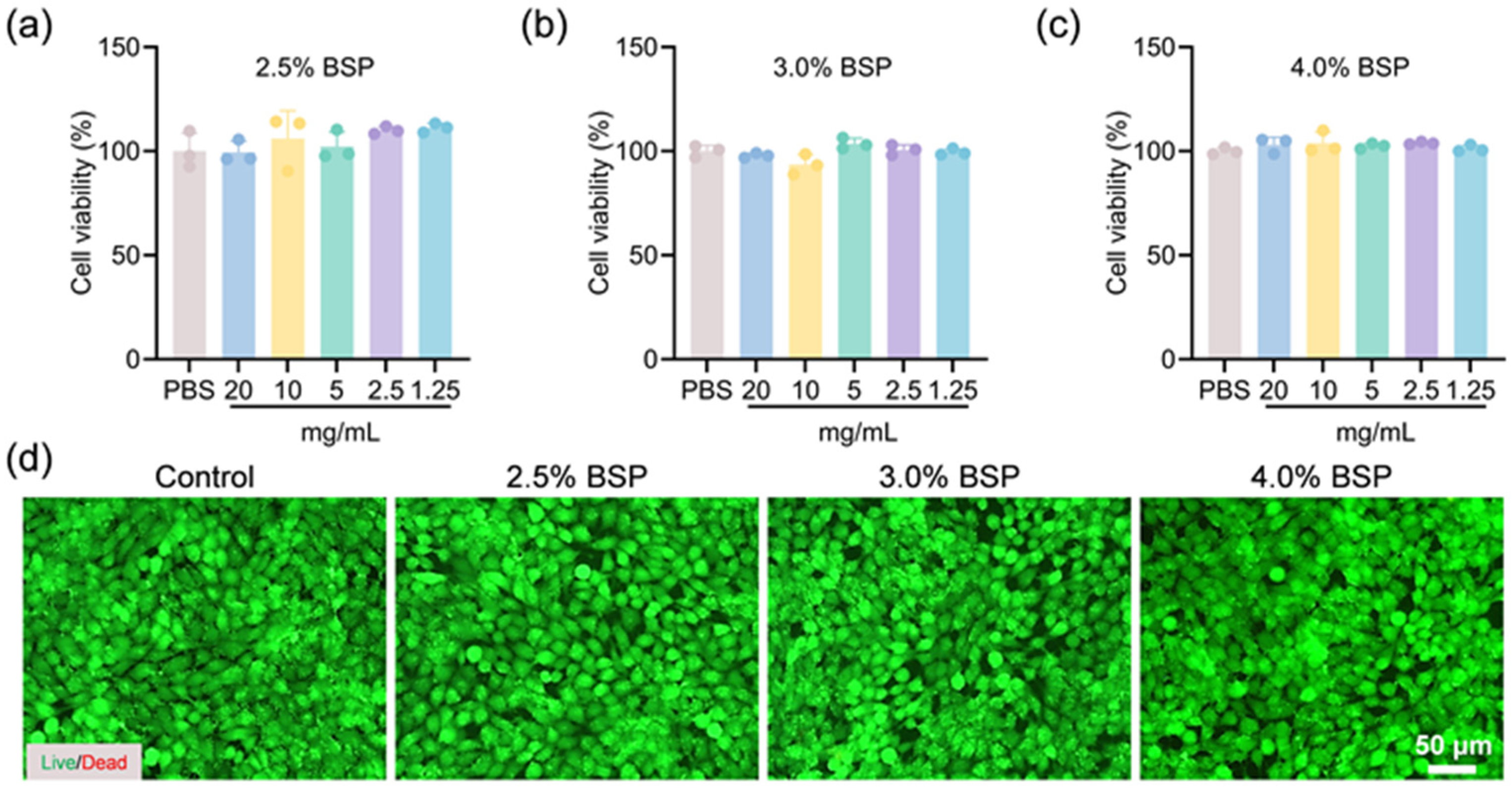
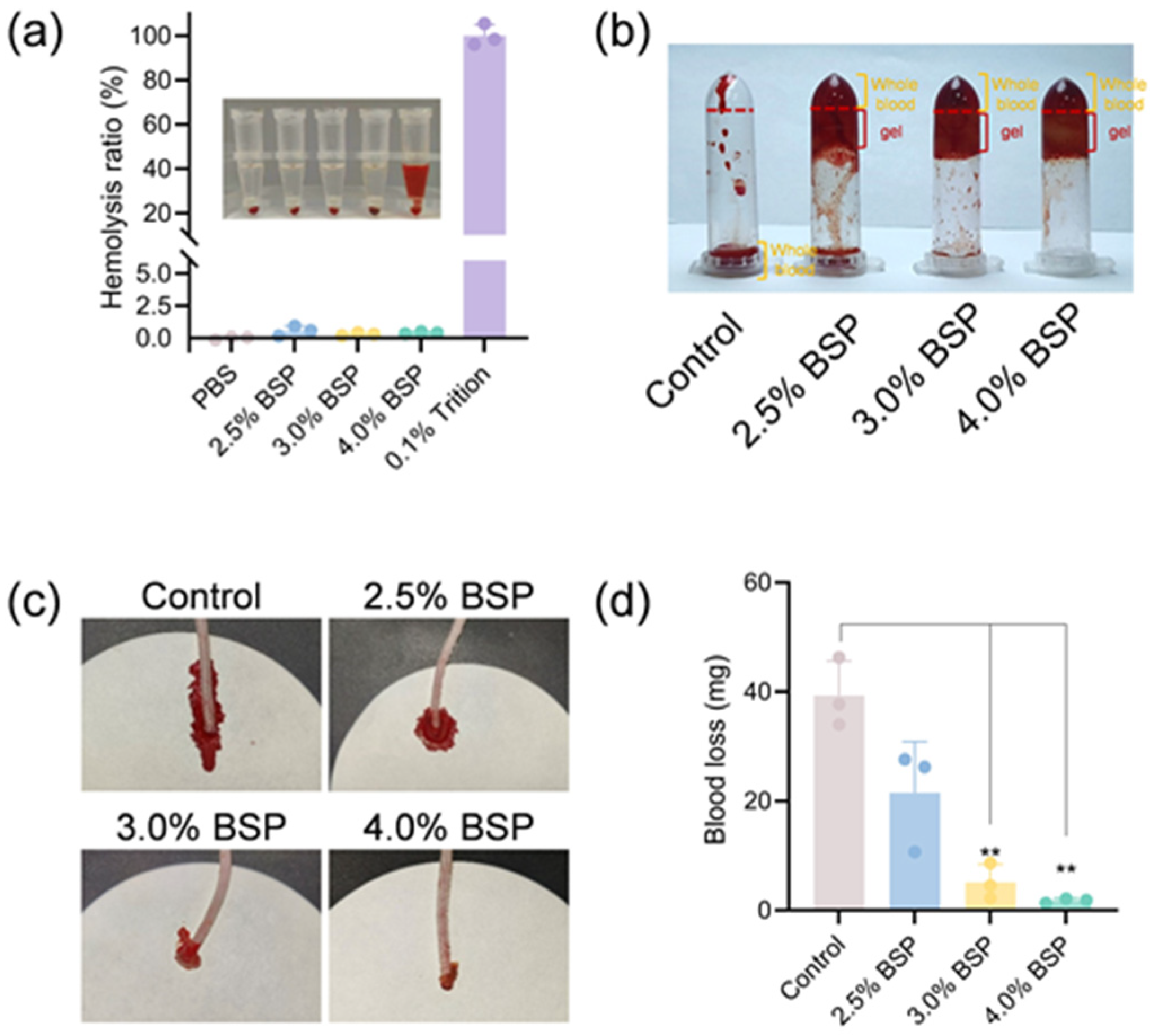
2.3. In Vitro Biocompatibility of BSP Hydrogels
2.4. In Vitro Whole Blood Clotting Test and In Vivo Hemostasis of Hydrogels
3. Conclusions
4. Materials and Methods
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yang, Y.; Liang, Y.; Chen, J.; Duan, X.; Guo, B. Mussel-inspired adhesive antioxidant antibacterial hemostatic composite hydrogel wound dressing via photo-polymerization for infected skin wound healing. Bioact. Mater. 2022, 8, 341–354. [Google Scholar] [CrossRef] [PubMed]
- Sari, M.H.M.; Cobre, A.F.; Pontarolo, R.; Ferreira, L.M. Status and Future Scope of Soft Nanoparticles-Based Hydrogel in Wound Healing. Pharmaceutics 2023, 15, 874. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Cheng, L.; He, Y.; Wei, X. Extraction, characterization, utilization as wound dressing and drug delivery of Bletilla striata polysaccharide: A review. Int. J. Biol. Macromol. 2018, 120, 2076–2085. [Google Scholar] [CrossRef]
- Li, W.; Yang, X.; Lai, P.; Shang, L. Bio-inspired adhesive hydrogel for biomedicine-principles and design strategies. Smart Med. 2022, 1, e20220024. [Google Scholar] [CrossRef]
- Li, N.; Zhan, A.; Jiang, Y.; Liu, H. A novel matrix metalloproteinases-cleavable hydrogel loading deferoxamine accelerates diabetic wound healing. Int. J. Biol. Macromol. 2022, 222, 1551–1559. [Google Scholar] [CrossRef]
- Zhong, Y.; Xiao, H.; Seidi, F.; Jin, Y. Natural Polymer-Based Antimicrobial Hydrogels without Synthetic Antibiotics as Wound Dressings. Biomacromolecules 2020, 21, 2983–3006. [Google Scholar] [CrossRef]
- Ma, H.; Axi, Y.; Lu, Y.; Dai, C.; Huang, S.; Kong, Z.; Jimo, R.; Li, H.; Chen, G.; Li, P.; et al. A dual network cross-linked hydrogel with multifunctional Bletilla striata polysaccharide/gelatin/tea polyphenol for wound healing promotion. Int. J. Biol. Macromol. 2024, 265, 130780. [Google Scholar] [CrossRef]
- Sui, J.; Tang, C.; Ke, C.Q.; Ye, Y. Dimeric 9,10-dihydrophenanthrene derivatives from Bletilla striata and their atropisomeric nature. Fitoterapia 2021, 152, 104919. [Google Scholar] [CrossRef]
- Chen, C.; Zhou, P.; Huang, C.; Zeng, R.; Yang, L.; Han, Z.; Qu, Y.; Zhang, C. Photothermal-promoted multi-functional dual network polysaccharide hydrogel adhesive for infected and susceptible wound healing. Carbohydr. Polym. 2021, 273, 118557. [Google Scholar] [CrossRef]
- He, X.; Wang, X.; Fang, J.; Zhao, Z.; Huang, L.; Guo, H.; Zheng, X. Bletilla striata: Medicinal uses, phytochemistry and pharmacological activities. J. Ethnopharmacol. 2017, 195, 20–38. [Google Scholar] [CrossRef]
- He, X.; Liu, L.; Gu, F.; Huang, R.; Liu, L.; Nian, Y.; Zhang, Y.; Song, C. Exploration of the anti-inflammatory, analgesic, and wound healing activities of Bletilla Striata polysaccharide. Int. J. Biol. Macromol. 2024, 261, 129874. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Wu, Y.; Gong, H.; Xiong, Y.; Chen, Y.; Li, L.; Zhi, B.; Lv, S.; Peng, T.; Zhang, H. A Multifunctional Herb-Derived Glycopeptide Hydrogel for Chronic Wound Healing. Small 2024, 20, e2400516. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Qi, C.; Wang, H.; Xiao, X.; Zhuang, Y.; Gu, S.; Zhou, Y.; Wang, L.; Yang, H.; Xu, W. Biocompatible and degradable Bletilla striata polysaccharide hemostasis sponges constructed from natural medicinal herb Bletilla striata. Carbohydr. Polym. 2019, 226, 115304. [Google Scholar] [CrossRef]
- Gou, K.; Li, Y.; Qu, Y.; Li, H.; Zeng, R. Advances and prospects of Bletilla striata polysaccharide as promising multifunctional biomedical materials. Mater. Des. 2022, 223, 111198. [Google Scholar] [CrossRef]
- Jiang, F.; Li, M.; Wang, H.; Ding, B.; Zhang, C.; Ding, Z.; Yu, X.; Lv, G. Coelonin, an Anti-Inflammation Active Component of Bletilla striata and Its Potential Mechanism. Int. J. Mol. Sci. 2019, 20, 4422. [Google Scholar] [CrossRef]
- Cao, X.; Wang, Y.; Wu, X.; Wang, J.; Ren, H.; Zhao, Y. Multifunctional structural color Chinese herb hydrogel patches for wound management. Chem. Eng. J. 2024, 485, 149957. [Google Scholar] [CrossRef]
- Tang, Z.; Dan, N.; Chen, Y. Utilizing epoxy Bletilla striata polysaccharide collagen sponge for hemostatic care and wound healing. Int. J. Biol. Macromol. 2024, 259 Pt 1, 128389. [Google Scholar] [CrossRef]
- Chen, X.; Hu, Z.; Zhao, K.; Rao, X.; Shen, C.; Chen, Y.; Ye, X.; Fang, C.; Zhou, F.; Ding, Z.; et al. Microenvironment-responsive, multimodulated herbal polysaccharide hydrogel for diabetic foot ulcer healing. Sci. Rep. 2024, 14, 22135. [Google Scholar] [CrossRef]
- Akihiro, H.; Hang Thi, T.; Naotsugu, N.; Toshiaki, Y.; Masao, T. Metal adsorption of carboxymethyl cellulose/carboxymethyl chitosan blend hydrogels prepared by Gamma irradiation. Radiat. Phys. Chem. 2009, 78, 1076–1080. [Google Scholar]
- Jing, H.; Huang, X.; Du, X.; Mo, L.; Ma, C.; Wang, H. Facile synthesis of pH-responsive sodium alginate/carboxymethyl chitosan hydrogel beads promoted by hydrogen bond. Carbohydr. Polym. 2022, 278, 118993. [Google Scholar] [CrossRef]
- Zhang, B.; Jiang, Z.; Li, X.; Wu, Z.; Liu, Y.; Hu, J.; Zhang, C.; Chen, J.; Zhou, Y.; Rao, J.; et al. Facile preparation of biocompatible and antibacterial water-soluble films using polyvinyl alcohol/carboxymethyl chitosan blend fibers via centrifugal spinning. Carbohydr. Polym. 2023, 317, 121062. [Google Scholar] [CrossRef] [PubMed]
- Thombare, N.; Jha, U.; Mishra, S.; Siddiqui, M.Z. Borax cross-linked guar gum hydrogels as potential adsorbents for water purification. Carbohydr. Polym. 2017, 168, 274–281. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Fu, R.; Duan, Z.; Zhu, C.; Fan, D. Construction of multifunctional hydrogel based on the tannic acid-metal coating decorated MoS2 dual nanozyme for bacteria-infected wound healing. Bioact. Mater. 2022, 9, 461–474. [Google Scholar] [CrossRef] [PubMed]
- Mehdi, A.; Mohammad, S.; Long, J.; Yasaman, B.; Ali Reza, Z.; Gholam Reza, M.; Mostafa, A. Incorporation of dynamic boronate links and Ag nanoparticles into PVA hydrogels for pH-Regulated and prolonged release of methotrexate. J. Drug Deliv. Sci. Technol. 2021, 63, 102502. [Google Scholar]
- Zhang, X.; Mu, Y.; Zhao, L.; Hong, Y.; Shen, L. Self-healing, antioxidant, and antibacterial Bletilla striata polysaccharide-tannic acid dual dynamic crosslinked hydrogels for tissue adhesion and rapid hemostasis. Int. J. Biol. Macromol. 2024, 270, 132182. [Google Scholar] [CrossRef]
- Han, X.; Saengow, C.; Ju, L.; Ren, W.; Ewoldt, R.H.; Irudayaraj, J. Exosome-coated oxygen nanobubble-laden hydrogel augments intracellular delivery of exosomes for enhanced wound healing. Nat. Commun. 2024, 15, 3435. [Google Scholar] [CrossRef]
- Zhen, N.; Kelin, P.; Lizhi, L.; Jueying, Y.; Zhekun, C.; Qiang, G.; Yu, C.; Changgen, F. A conductive hydrogel based on nature polymer agar with self-healing ability and stretchability for flexible sensors. Chem. Eng. J. 2023, 454, 139843. [Google Scholar]
- Yang, J.; Chen, Y.; Zhao, L.; Feng, Z.; Peng, K.; Wei, A. Preparation of a chitosan/carboxymethyl chitosan/AgNPs polyelectrolyte composite physical hydrogel with self-healing ability, antibacterial properties, and good biosafety simultaneously, and its application as a wound dressing. Compos. Part B 2020, 197, 108139. [Google Scholar] [CrossRef]
- Zhang, N.; Xue, L.; Younas, A.; Liu, F.; Sun, J.; Dong, Z.; Zhao, Y. Co-delivery of triamcinolone acetonide and verapamil for synergistic treatment of hypertrophic scars via carboxymethyl chitosan and Bletilla striata polysaccharide-based microneedles. Carbohydr. Polym. 2022, 284, 119219. [Google Scholar] [CrossRef]
- Bai, L.; Wang, T.; Deng, Q.; Zheng, W.; Li, X.; Yang, H.; Tong, R.; Yu, D.; Shi, J. Dual properties of pharmacological activities and preparation excipient: Bletilla striata polysaccharides. Int. J. Biol. Macromol. 2024, 254 Pt 1, 127643. [Google Scholar] [CrossRef]
- Palungan, J.; Luthfiyah, W.; Mustopa, A.Z.; Nurfatwa, M.; Rahman, L.; Yulianty, R.; Wathoni, N.; Yoo, J.W.; Hasan, N. The Formulation and Characterization of Wound Dressing Releasing S-Nitrosoglutathione from Polyvinyl Alcohol/Borax Reinforced Carboxymethyl Chitosan Self-Healing Hydrogel. Pharmaceutics 2024, 16, 344. [Google Scholar] [CrossRef] [PubMed]
- Tan, Y.; Xu, C.; Liu, Y.; Bai, Y.; Li, X.; Wang, X. Sprayable and self-healing chitosan-based hydrogels for promoting healing of infected wound via anti-bacteria, anti-inflammation and angiogenesis. Carbohydr. Polym. 2024, 337, 122147. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Wu, H.; Guo, B.; Dong, R.; Qiu, Y.; Ma, P.X. Antibacterial anti-oxidant electroactive injectable hydrogel as self-healing wound dressing with hemostasis and adhesiveness for cutaneous wound healing. Biomaterials 2017, 122, 34–47. [Google Scholar] [CrossRef] [PubMed]
- Yan, Q.; Long, X.; Zhang, P.; Lei, W.; Sun, D.; Ye, X. Oxidized Bletilla rhizome polysaccharide-based aerogel with synergistic antibiosis and hemostasis for wound healing. Carbohydr. Polym. 2022, 293, 119696. [Google Scholar] [CrossRef]
- Ningrum, D.R.; Hanif, W.; Mardhian, D.F.; Asri, L.A.T.W. In Vitro Biocompatibility of Hydrogel Polyvinyl Alcohol/Moringa oleifera Leaf Extract/Graphene Oxide for Wound Dressing. Polymers 2023, 15, 468. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, H.-F.; Wang, Y.-Y.; Liu, F.-Z.; Yang, Z.-W.; Cui, H.; Hu, S.-Y.; Li, F.-H.; Pan, P. Natural Bletilla striata Polysaccharide-Based Hydrogels for Accelerating Hemostasis. Gels 2025, 11, 48. https://doi.org/10.3390/gels11010048
Lin H-F, Wang Y-Y, Liu F-Z, Yang Z-W, Cui H, Hu S-Y, Li F-H, Pan P. Natural Bletilla striata Polysaccharide-Based Hydrogels for Accelerating Hemostasis. Gels. 2025; 11(1):48. https://doi.org/10.3390/gels11010048
Chicago/Turabian StyleLin, Hui-Fang, Yue-Yue Wang, Feng-Zhen Liu, Zi-Wei Yang, Hao Cui, Si-Yu Hu, Feng-He Li, and Pei Pan. 2025. "Natural Bletilla striata Polysaccharide-Based Hydrogels for Accelerating Hemostasis" Gels 11, no. 1: 48. https://doi.org/10.3390/gels11010048
APA StyleLin, H.-F., Wang, Y.-Y., Liu, F.-Z., Yang, Z.-W., Cui, H., Hu, S.-Y., Li, F.-H., & Pan, P. (2025). Natural Bletilla striata Polysaccharide-Based Hydrogels for Accelerating Hemostasis. Gels, 11(1), 48. https://doi.org/10.3390/gels11010048






