Recurrent Scedosporium apiospermum Cutaneous Infection in a Patient with Rheumatoid Arthritis: The Potent Role of IL-6 Signaling Pathway Blockade: A Case-Based Review
Abstract
1. Introduction
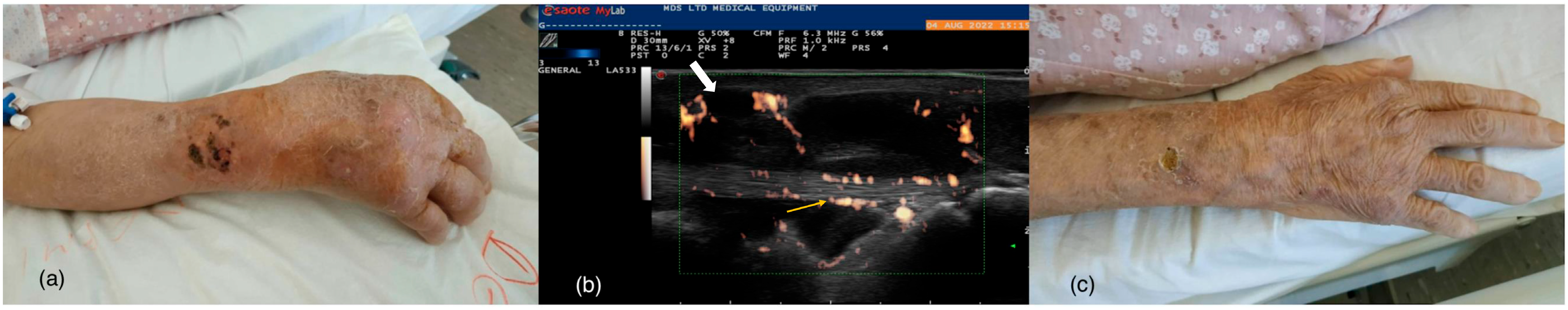
2. Case Report
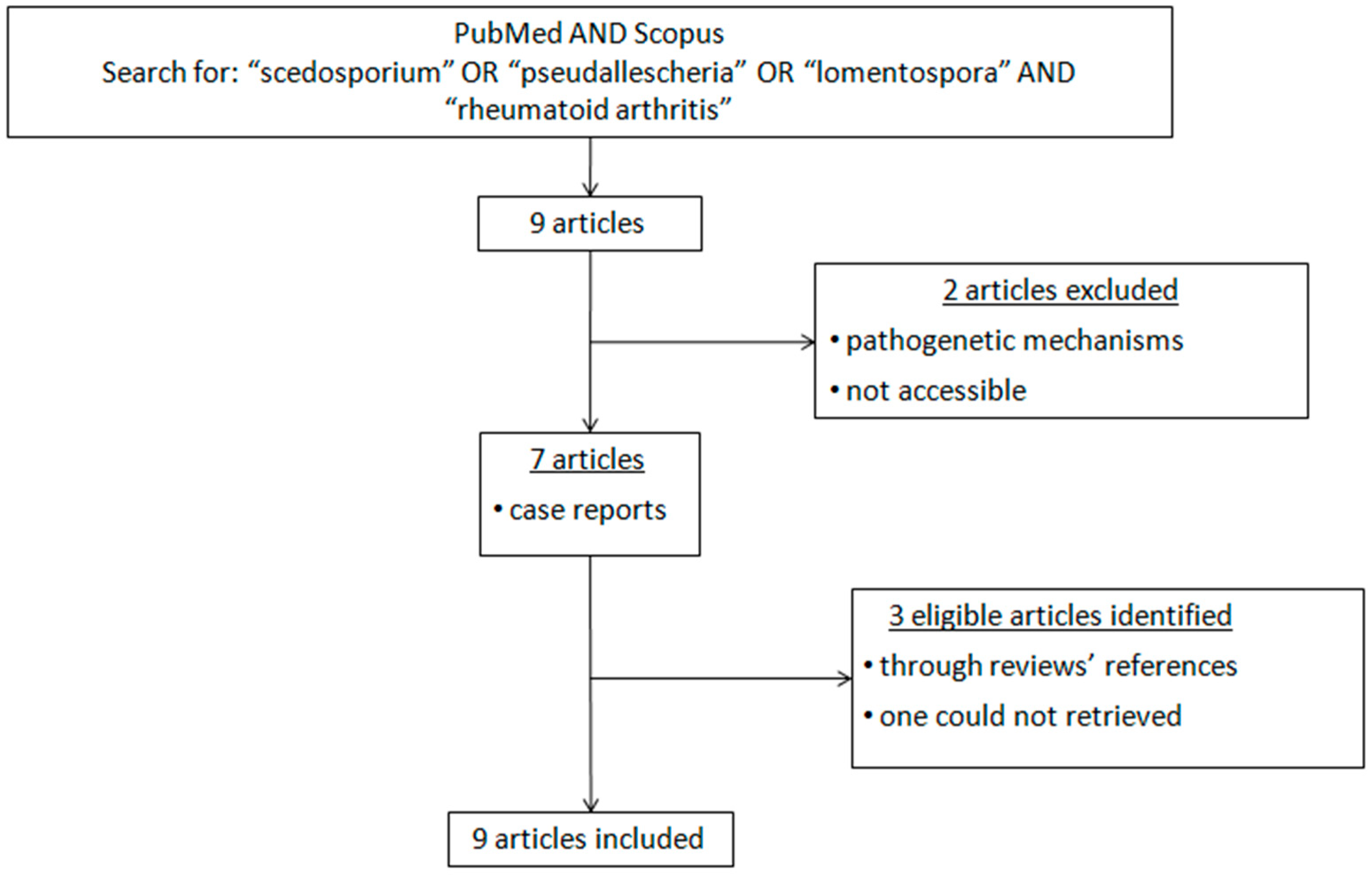
3. Materials and Methods
4. Results
5. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Smolen, J.S.; Aletaha, D.; Barton, A.; Burmester, G.R.; Emery, P.; Firestein, G.S.; Kavanaugh, A.; McInnes, I.B.; Solomon, D.H.; Strand, V.; et al. Rheumatoid arthritis. Nat. Rev. Dis. Prim. 2018, 4, 18001. [Google Scholar] [CrossRef] [PubMed]
- Alamanos, Y.; Drosos, A.A. Epidemiology of adult rheumatoid arthritis. Autoimmun. Rev. 2005, 4, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Venetsanopoulou, A.I.; Alamanos, Y.; Voulgari, P.V.; Drosos, A.A. Epidemiology of rheumatoid arthritis: Genetic and environmental influences. Expert. Rev. Clin. Immunol. 2022, 18, 923–931. [Google Scholar] [CrossRef] [PubMed]
- Venetsanopoulou, A.I.; Voulgari, P.V.; Drosos, A.A. Janus kinase versus TNF inhibitors: Where we stand today in rheumatoid arthritis. Expert. Rev. Clin. Immunol. 2022, 18, 485–493. [Google Scholar] [CrossRef]
- Vallabhaneni, S.; Chiller, T.M. Fungal Infections and New Biologic Therapies. Curr. Rheumatol. Rep. 2016, 18, 29. [Google Scholar] [CrossRef]
- Dixon, W.G.; Suissa, S.; Hudson, M. The association between systemic glucocorticoid therapy and the risk of infection in patients with rheumatoid arthritis: Systematic review and meta-analyses. Arthritis Res. Ther. 2011, 13, R139. [Google Scholar] [CrossRef]
- Tan, Z.; Mok, M.M.H.; Soe, W.M.; Thamboo, T.P.; Goh, J.D.; Sam, Q.H.; Osato, M.; Ravikumar, S.; Chai, L.Y.A. Tocilizumab Induces IL-10-Mediated Immune Tolerance in Invasive Candidiasis. J. Fungi 2021, 7, 656. [Google Scholar] [CrossRef]
- Steinbach, W.J.; Perfect, J.R. Scedosporium species infections and treatments. J. Chemother. 2003, 15 (Suppl. 2), 16–27. [Google Scholar] [CrossRef]
- Tarozzi, G. Ricercheanatomo-patologiehe, baceriologiehet e sperimentali sopra un caso di actinomicosi del piede. Arch. Perle Sc. Med. 1909, 33, 553–632. [Google Scholar]
- Luna-Rodríguez, C.E.; Rogelio, J.T.-R.; Montoya, A.M.; Becerril-García, M.A.; Andrade, A.; González, G.M. Scedosporium spp.: Chronicle of an emerging pathogen. Med. Univ. 2019, 21, 4–13. [Google Scholar] [CrossRef]
- Kidd, S.E.; Abdolrasouli, A.; Hagen, F. Fungal Nomenclature: Managing Change is the Name of the Game. Open. Forum Infect. Dis. 2023, 10, ofac559. [Google Scholar] [CrossRef]
- Guarro, J.; Kantarcioglu, A.S.; Horré, R.; Rodriguez-Tudela, J.L.; Estrella, M.C.; Berenguer, J.; De Hoog, G.S. Scedosporium apiospermum: Changing clinical spectrum of a therapy-refractory opportunist. Med. Mycol. 2006, 44, 295–327. [Google Scholar] [CrossRef]
- Cortez, K.J.; Roilides, E.; Quiroz-Telles, F.; Meletiadis, J.; Antachopoulos, C.; Knudsen, T.; Buchanan, W.; Milanovich, J.; Sutton, D.A.; Fothergill, A.; et al. Infections caused by Scedosporium spp. Clin. Microbiol. Rev. 2008, 21, 157–197. [Google Scholar] [CrossRef]
- Saadah, H.A.; Dixon, T. Petriellidium boydii (Allescheria boydii): Necrotizing pneumonia in a normal host. JAMA 1981, 245, 605–606. [Google Scholar] [CrossRef]
- Salitan, M.L.; Lawson, W.; Som, P.M.; Bottone, E.J.; Biller, H.F. Pseudallescheria sinusitis with intracranial extension in a nonimmunocompromised host. Otolaryngol. Head Neck Surg. 1990, 102, 745–750. [Google Scholar] [CrossRef]
- Nucci, M. Emerging moulds: Fusarium, Scedosporium and Zygomycetes in transplant recipients. Curr. Opin. Infect. Dis. 2003, 16, 607612. [Google Scholar] [CrossRef]
- Cimon, B.; Carrère, J.; Vinatier, J.F.; Chazalette, J.P.; Chabasse, D.; Bouchara, J.P. Clinical significance of Scedosporium apiospermum in patients with cystic fibrosis. Eur. J. Clin. Microbiol. Infect. Dis. 2000, 19, 53–56. [Google Scholar] [CrossRef]
- Russell, G.K.; Gadhok, R.; Simmonds, N.J. The destructive combination of Scediosporium apiosperum lung disease and exuberant inflammation in cystic fibrosis. Paediatr. Respir. Rev. 2013, 14 (Suppl. 1), 22–25. [Google Scholar] [CrossRef]
- Ramirez-Garcia, A.; Pellon, A.; Rementeria, A.; Buldain, I.; Barreto-Bergter, E.; Rollin-Pinheiro, R.; de Meirelles, J.V.; Xisto, M.I.D.S.; Ranque, S.; Havlicek, V.; et al. Scedosporium and Lomentospora: An updated overview of underrated opportunists. Med. Mycol. 2018, 56 (Suppl. 1), S102–S125. [Google Scholar] [CrossRef]
- Shinohara, M.M.; George, E. Scedosporium apiospermum: An emerging opportunistic pathogen that must be distinguished from Aspergillus and other hyalohyphomycetes. J. Cutan. Pathol. 2009, 36 (Suppl. 1), 39–41. [Google Scholar] [CrossRef]
- Kleinschmidt-DeMasters, B.K. Central nervous system aspergillosis: A 20-year retrospective series. Hum. Pathol. 2002, 33, 116–124. [Google Scholar] [CrossRef] [PubMed]
- Lopez, F.A.; Crowley, R.S.; Wastila, L.; Valantine, H.A.; Remington, J.S. Scedosporium apiospermum (Pseudallescheria boydii) infection in a heart transplant recipient: A case of mistaken identity. J. Heart Lung Transpl. 1998, 17, 321324. [Google Scholar]
- Guarro, J.; Gene, J. Acrophialophora fusispora misidentified as Scedosporium prolificans. J. Clin. Microbiol. 2002, 40, 3544. [Google Scholar] [CrossRef] [PubMed]
- Walts, A.E. Pseudallescheria: An underdiagnosed fungus? Diagn. Cytopathol. 2001, 25, 153157. [Google Scholar] [CrossRef]
- Hoenigl, M.; Salmanton-García, J.; Walsh, T.J.; Nucci, M.; Neoh, C.F.; Jenks, J.D.; Lackner, M.; Sprute, R.; Al-Hatmi, A.M.S.; Bassetti, M.; et al. Global guideline for the diagnosis and management of rare mouldinfections: An initiative of the European Confederation of Medical Mycology in cooperation with the International Society for Human and Animal Mycology and the American Society for Microbiology. Lancet Infect. Dis. 2021, 21, e246–e257. [Google Scholar] [CrossRef] [PubMed]
- Bernhard, M.; Zautner, A.E.; Steinmann, J.; Weig, M.; Groß, U.; Bader, O. Towards proteomic species barcoding of fungi—An example using Scedosporium/Pseudallescheria complex isolates. Fungal Biol. 2016, 120, 162–165. [Google Scholar] [CrossRef]
- Lackner, M.; de Hoog, G.S.; Verweij, P.E.; Najafzadeh, M.J.; Curfs-Breuker, I.; Klaassen, C.H.; Meis, J.F. Species-specific antifungal susceptibility patterns of Scedosporium and Pseudallescheria species. Antimicrob. Agents Chemother. 2012, 56, 2635–2642. [Google Scholar] [CrossRef]
- Troke, P.; Aguirrebengoa, K.; Arteaga, C.; Ellis, D.; Heath, C.H.; Lutsar, I.; Rovira, M.; Nguyen, Q.; Slavin, M.; Chen, S.C.A.; et al. Treatment of scedosporiosis with voriconazole: Clinical experience with 107 patients. Antimicrob. Agents Chemother. 2008, 52, 1743–1750. [Google Scholar] [CrossRef]
- Gil-Lamaignere, C.; Roilides, E.; Lyman, C.A.; Simitsopoulou, M.; Stergiopoulou, T.; Maloukou, A.; Walsh, T.J. Human phagocytic cell responses to Scedosporium apiospermum (Pseudallescheria boydii): Variable susceptibility to oxidative injury. Infect. Immun. 2003, 71, 6472–6478. [Google Scholar] [CrossRef]
- Gil-Lamaignere, C.; Simitsopoulou, M.; Roilides, E.; Maloukou, A.; Winn, R.M.; Walsh, T.J. Interferon gamma and granulocyte-macrophage colony-stimulating factor augment the antifungal activity of human polymorphonuclear leukocytes against Scedosporium spp.: Comparison with Aspergillus spp. Med. Mycol. 2005, 43, 253260. [Google Scholar] [CrossRef]
- Murayama, T.; Amitani, R.; Tsuyuguchi, K.; Watanabe, I.; Kimoto, T.; Suzuki, K.; Tanaka, E.; Kamei, K.; Nishimura, K. Polypoid bronchial lesions due to Scedosporium apiospermum in a patient with Mycobacterium avium complex pulmonary disease. Eur. Respir. J. 1998, 12, 745–747. [Google Scholar] [CrossRef]
- Khan, S.A. A fatal pseudallescheria boydii brain abscess. Neurosciences 2000, 5, 125–127. [Google Scholar]
- Fays, S.; Di Cesare, M.P.; Antunes, A.; Truchetet, F. Infection cutanée et ostéoarticulaire à Scedosporium apiospermum [Cutaneous and osteoarticular Scedosporium apiospermum infection]. Ann. Med. Interne 2002, 153, 537–539. [Google Scholar]
- Chaveiro, M.A.; Vieira, R.; Cardoso, J.; Afonso, A. Cutaneous infection due to Scedosporium apiospermum in an immunosuppressed patient. J. Eur. Acad. Dermatol. Venereol. 2003, 17, 47–49. [Google Scholar] [CrossRef]
- Gottesman-Yekutieli, T.; Shwartz, O.; Edelman, A.; Hendel, D.; Dan, M. Pseudallescheria boydii infection of a prosthetic hip joint—An uncommon infection in a rare location. Am. J. Med. Sci. 2011, 342, 250–253. [Google Scholar] [CrossRef]
- Canet, J.J.; Pagerols, X.; Sánchez, C.; Vives, P.; Garau, J. Lymphocutaneous syndrome due to Scedosporium apiospermum. Clin. Microbiol. Infect. 2001, 7, 648–650. [Google Scholar] [CrossRef]
- Sakata, Y.; Taga, F.; Ushigami, T.; Takeda, K.; Anzawa, K.; Nishibu, A.; Mochizuki, T. A Case of Cutaneous Mycosis Caused by Scedosporium dehoogii on an Immunocompromised Patient. Mycopathologia 2018, 183, 465–470. [Google Scholar] [CrossRef]
- Lee, J.; Wilson, M.; Casey, N. Eradication of Lomentospora prolificans Osteomyelitis of the Wrist with Combination Antifungal Therapy, Voriconazole Bone Cement, and Surgical Debridement. Case Rep. Orthop. 2020, 2020, 8271471. [Google Scholar] [CrossRef]
- Palma-Fernández, R.; Montecinos-Astorga, A.; Fica, A.; Godoy-Martínez, P.; Aguilera, I.; Pinar-Pacheco, C. Infección ocular invasorapor Scedosporium apioespermum en un paciente inmunocomprometido [Invasive ocular fungal infection by Scedosporium apiospermum in an immunocompromised patient]. Rev. Chil. Infectol. 2021, 38, 568–573. [Google Scholar] [CrossRef]
- Doran, M.F.; Crowson, C.S.; Pond, G.R.; O’Fallon, W.M.; Gabriel, S.E. Frequency of infection in patients with rheumatoid arthritis compared with controls: A population-based study. Arthritis Rheum. 2002, 46, 2287–2293. [Google Scholar] [CrossRef]
- Peng, L.; Zhong, J.; Xiao, Y.; Wang, B.; Li, S.; Deng, Y.; He, D.; Yuan, J. Therapeutic effects of an anti-IL-6 antibody in fungal keratitis: Macrophage inhibition and T cell subset regulation. Int. Immunopharmacol. 2020, 85, 106649. [Google Scholar] [CrossRef] [PubMed]
- Chalaris, A.; Rabe, B.; Paliga, K.; Lange, H.; Laskay, T.; Fielding, C.A.; Jones, S.A.; Rose-John, S.; Scheller, J. Apoptosis is a natural stimulus of IL6R shedding and contributes to the proinflammatory trans-signaling function of neutrophils. Blood 2007, 110, 1748–1755. [Google Scholar] [CrossRef] [PubMed]
- Mesquida, M.; Leszczynska, A.; Llorenç, V.; Adan, A. Interleukin-6 blockade in ocular inflammatory diseases. Clin. Exp. Immunol. 2014, 176, 301–309. [Google Scholar] [CrossRef] [PubMed]
- Adan, A.; Mesquida, M.; Llorenç, V.; Espinosa, G.; Molins, B.; Hernández, M.V.; Pelegrin, L. Tocilizumab treatment for refractory uveitis-related cystoid macular edema. Graefes Arch. Clin. Exp. Ophthalmol. 2013, 251, 2627–2632. [Google Scholar] [CrossRef] [PubMed]
- Zink, A.; Manger, B.; Kaufmann, J.; Eisterhues, C.; Krause, A.; Listing, J.; Strangfeld, A. Evaluation of the rabbit risk score for serious infections. Ann. Rheum. Dis. 2014, 73, 1673–1676. [Google Scholar] [CrossRef]
- Genovese, M.C.; Fleischmann, R.; Genovese, M.C.; Fleischmann, R.; Furst, D.; Janssen, N.; Carter, J.; Dasgupta, B.; Bryson, J.; Duncan, B.; et al. Efficacy and safety of olokizumab in patients with rheumatoid arthritis with an inadequate response to TNF inhibitor therapy: Outcomes of a randomised phase IIb study. Ann. Rheum. Dis. 2014, 73, 1607–1615. [Google Scholar] [CrossRef]
- Rutherford, A.I.; Subesinghe, S.; Hyrich, K.L.; Galloway, J.B. Serious infection across biologic treated patients with rheumatoid arthritis: Results from the british Society for rheumatology biologics register for rheumatoid arthritis. Ann. Rheum. Dis. 2018, 77, 905–910. [Google Scholar] [CrossRef]
- Pawar, A.; Desai, R.J.; Solomon, D.H.; Santiago Ortiz, A.J.; Gale, S.; Bao, M.; Sarsour, K.; Schneeweiss, S.; Kim, S.C. Risk of serious infections in tocilizumab versus other biologic drugs in patients with rheumatoid arthritis: A multidatabase cohort study. Ann. Rheum. Dis. 2019, 78, 456–464. [Google Scholar] [CrossRef]
- McCarty, D.; Robinson, A. Efficacy and safety of sarilumab in patients with active rheumatoid arthritis. Ther. Adv. Musculoskelet. Dis. 2018, 10, 61–67. [Google Scholar] [CrossRef]
- Kopf, M.; Baumann, H.; Freer, G.; Freudenberg, M.; Lamers, M.; Kishimoto, T.; Zinkernagel, R.; Bluethmann, H.; Kohler, G. Impaired immune and acute-phase responses in interleukin-6-deficient mice. Nature 1994, 368, 339–342. [Google Scholar] [CrossRef]
- Wang, J.E.; Warris, A.; Ellingsen, E.A.; Jorgensen, P.F.; Flo, T.H.; Espevik, T.; Solberg, R.; Verweij, P.E.; Aasen, A.O. Involvement of CD14 and toll-like receptors in activation of human monocytes by Aspergillus fumigatus hyphae. Infect. Immun. 2001, 69, 2402–2406. [Google Scholar] [CrossRef]
- Nishioka, H.; Takegawa, H.; Kamei, H. Disseminated cryptococcosis in a patient taking tocilizumab for Castleman’s disease. J. Infect. Chemother. 2018, 24, 138–141. [Google Scholar] [CrossRef]
- Schiff, M.H.; Kremer, J.M.; Jahreis, A.; Vernon, E.; Isaacs, J.D.; van Vollenhoven, R.F. Integrated safety in tocilizumab clinical trials. Arthritis Res. Ther. 2011, 13, R141. [Google Scholar] [CrossRef]
- Campbell, L.; Chen, C.; Bhagat, S.S.; Parker, R.A.; Ostor, A.J.K. Risk of adverse events including serious infections in rheumatoid arthritis patients treated with tocilizumab: A systematic literature review and meta-analysis of randomized controlled trials. Rheumatology 2011, 50, 552–562. [Google Scholar] [CrossRef]
- Rose-John, S.; Winthrop, K.; Calabrese, L. The role of IL-6 in host defence against infections: Immunobiology and clinical implications. Nat. Rev. Rheumatol. 2017, 13, 399–409. [Google Scholar] [CrossRef]
- Koike, T.; Harigai, M.; Inokuma, S.; Ishiguro, N.; Ryu, J.; Takeuchi, T.; Takei, S.; Tanaka, Y.; Ito, K.; Yamanaka, H. Postmarketing surveillance of tocilizumab for rheumatoid arthritis in Japan: Interim analysis of 3881 patients. Ann. Rheum. Dis. 2011, 70, 2148–2151. [Google Scholar] [CrossRef]
- Sah, S.K.; Shariff, A.; Pathakamuri, N.; Ramaswamy, S.; Ramesh, M.; Undela, K.; Srikanth, M.S.; Kumar, T.M.P. Antifungal therapy in the management of fungal secondary infections in COVID-19 patients: A systematic review and meta-analysis. PLoS ONE 2022, 17, e0271795. [Google Scholar] [CrossRef]
- Goldman, C.; Akiyama, M.J.; Torres, J.; Louie, E.; Meehan, S.A. Scedosporium apiospermum infections and the role of combination antifungal therapy and GM-CSF: A case report and review of the literature. Med. Mycol. Case Rep. 2016, 11, 40–43. [Google Scholar] [CrossRef]
- Capilla, J.; Guarro, J. Correlation between in vitro susceptibility of Scedosporium apiospermum to voriconazole and in vivo outcome of scedosporiosis in guinea pigs. Antimicrob. Agents Chemother. 2004, 48, 4009–4011. [Google Scholar] [CrossRef]
- Ellis, D. Amphotericin B: Spectrum and resistance. J. Antimicrob. Chemother. 2002, 49 (Suppl. 1), 7–10. [Google Scholar] [CrossRef]
- Ahmed, J.; Ditmars, D.M.; Sheppard, T.; del Busto, R.; Venkat, K.K.; Parasuraman, R. Recurrence of Scedosporium apiospermum infection following renal re-transplantation. Am. J. Transplant. 2004, 4, 1720–1724. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, S.; Anzawa, K.; Mochizuki, T.T. Hepatic dysfunction caused by systemic voliconazole for treating a mycotic cyst caused by Scedosporium apiospermum. J. Dermatol. 2017, 44, e296–e297. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, K.; Ikawa, K.; Abematsu, K.; Fukunaga, N.; Nishida, K.; Fukamizu, T.; Shimodozonoa, Y.; Morikawa, N.; Takeda, Y.; Yamada, K. Correlation between voriconazole trough plasma concentration and hepatotoxicity in patients with different CYP2C19 genotypes. Int. J. Antimicrob. Agents 2009, 34, 91–94. [Google Scholar] [CrossRef] [PubMed]
- Abzug, M.J.; Walsh, T.J. Interferon-gamma and colony-stimulating factors as adjuvant therapy for refractory fungal infections in children. Pediatr. Infect. Dis. J. 2004, 23, 769–7733. [Google Scholar] [CrossRef]
- Castiglioni, B.; Sutton, D.A.; Rinaldi, M.G.; Fung, J.; Kusne, S. Pseudoallescheria boydii (anamorph Scedosporium apiospermum) infection in solid organ transplant recipients in a tertiary medical center and review of the literature. Medicine 2002, 81, 333–348. [Google Scholar] [CrossRef]
- Mitsuoka, Y.; Soma, T.; Maruyama, K.; Nishida, K. Fusarium infection complicating rheumatic keratitis that acutely progressed to endophthalmitis during regular infusion of tocilizumab: A case report. BMC Ophthalmol. 2021, 21, 224. [Google Scholar] [CrossRef]
- Honda, H.; Kida, H.; Yoshida, M.; Tomita, T.; Fujii, M.; Ihara, S.; Goya, S.; Tachibana, I.; Kawase, I. Recurrent allergic bronchopulmonary aspergillosis in a patient with rheumatoid arthritis treated with etanercept and tocilizumab. Mod. Rheumatol. 2011, 21, 660–664. [Google Scholar] [CrossRef]

| Author, y | Age (y)/Sex | Underlying Disease | Therapy at Presentation | Pathogen | Organ Involvement | Treatment | Outcome |
|---|---|---|---|---|---|---|---|
| Murayama T. et al. (1998) [31] | 69/F | RA, tuberculous pleurisy, and gold-induced interstitial pneumonia | MPz 4 mg/d, bucillamine | Scedosporium apiospermum | Lungs | MPz discontinuation | Stable; no recurrence reported |
| Khan S.A. (2000) [32] | Middle aged/F | RA | Pz; unknown dose | Pseudallescheria boydii | Central nervous system (brain abcess) | Surgical excision and IV antifungal agent (not determined) | Death |
| Fays S. et al. (2002) [33] | 65/M | RA | MPz; unknown dose | Scedosporium apiospermum | Skin and bone | ITZ | Successfully treated; no recurrence reported |
| Chaveiro M.A. et al. (2003) [34] | 63/F | RA and diabetes mellitus | MPz 10 mg/d and Cyclosporin 100 mg/d | Scedosporium apiospermum | Skin | ITZ 400 mg/d Cyclosporin | Almost total resolution at 4 weeks; no recurrence reported |
| Gottesman-Yekutieli T. et al. (2011) [35] | 56/F | RA and hip replacement | Pz 20 mg/d MTX | Pseudallescheria boydii | Bone | Removal of the prosthetic joint; cement spacer impregnated with ITZ; oral VCZ 800 mg on Day1 → 400 mg/d | Recurrence 6 weeks later while on VCZ; hip reoperation VCZ for 10 months |
| Canet J.J. et al. (2011) [36] | 69/F | RA, Sjoegren syndrome, arterial hypertension, chronic renal failure, and chronic hepatitis C | Pz 10 mg/d | Scedosporium apiospermum | Subcutaneous | Surgical drainage and ITZ 200 mg/d | Almost total resolution at 10 weeks; no recurrences reported |
| Sakata Y. et al. (2017) [37] | 77/M | RA | Betamethasone 1.25 mg/d and Tacrolimus 3 mg/d | Scedosporium dehoogii | Skin | Oral VCZ 400 mg/d and local hyperthermia | Improvement, but VCZ- induced liver dysfunction; switch to ITZ 200 mg/d, but worsened; add on terbinafine 125 mg/d for 10 months (ITZ for 6 months) |
| Lee J. et al. (2020) [38] | 68/M | RA | Pz 7.5 mg/d, HCQ 200 mg/d, and MTX 10 mg/wk Etanercept 50 mg/wk | Lomentospora prolificans | Skin and bone | Oral VCZ 250 mg BD and terbinafine 250 mg BD VCZ bone cement and surgical debridement | Improvement; no recurrence; VCZ and terbinafine for at least 12 months |
| Palma-Fernández R. et al. (2021) [39] | 78/F | RA | Pz 10 mg/d and Azathioprine 100 mg/d | Scedosporium apiospermum | Eye | Surgical debridements; topical eye solution; systemic therapy with VCZ and steroids | Improvement; reccurence;–second therapeutic course for 12 months |
| Present case | 81/F | RA, atrial fibrillation, mitral valve regurgitation, arterial hypertension, dyslipidemia, and osteoporosis | MPz 6 mg/d | Scedosporium apiospermum | Skin | IV VCZ 400 mg/d; Switch to PO VCZ 200 mg/d (due to VCZ-induced liver dysfunction) for 1 month | Reccurence; ITZ 200 mg/d |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pieta, A.; Venetsanopoulou, A.I.; Kittas, C.; Christaki, E.; Voulgari, P.V. Recurrent Scedosporium apiospermum Cutaneous Infection in a Patient with Rheumatoid Arthritis: The Potent Role of IL-6 Signaling Pathway Blockade: A Case-Based Review. J. Fungi 2023, 9, 683. https://doi.org/10.3390/jof9060683
Pieta A, Venetsanopoulou AI, Kittas C, Christaki E, Voulgari PV. Recurrent Scedosporium apiospermum Cutaneous Infection in a Patient with Rheumatoid Arthritis: The Potent Role of IL-6 Signaling Pathway Blockade: A Case-Based Review. Journal of Fungi. 2023; 9(6):683. https://doi.org/10.3390/jof9060683
Chicago/Turabian StylePieta, Antigone, Aliki I. Venetsanopoulou, Christos Kittas, Eirini Christaki, and Paraskevi V. Voulgari. 2023. "Recurrent Scedosporium apiospermum Cutaneous Infection in a Patient with Rheumatoid Arthritis: The Potent Role of IL-6 Signaling Pathway Blockade: A Case-Based Review" Journal of Fungi 9, no. 6: 683. https://doi.org/10.3390/jof9060683
APA StylePieta, A., Venetsanopoulou, A. I., Kittas, C., Christaki, E., & Voulgari, P. V. (2023). Recurrent Scedosporium apiospermum Cutaneous Infection in a Patient with Rheumatoid Arthritis: The Potent Role of IL-6 Signaling Pathway Blockade: A Case-Based Review. Journal of Fungi, 9(6), 683. https://doi.org/10.3390/jof9060683










