Abstract
Coccidioidomycosis (Valley fever) has been a known health threat in the United States (US) since the 1930s, though not all states are currently required to report disease cases. Texas, one of the non-reporting states, is an example of where both historical and contemporary scientific evidence define the region as endemic, but we don’t know disease incidence in the state. Mandating coccidioidomycosis as a reportable disease across more US states would increase disease awareness, improve clinical outcomes, and help antifungal drug and vaccine development. It would also increase our understanding of where the disease is endemic and the relationships between environmental conditions and disease cases. This is true for other nations in North and South America that are also likely endemic for coccidioidomycosis, especially Mexico. This commentary advocates for US state and territory epidemiologists to define coccidioidomycosis as a reportable disease and encourages disease surveillance in other endemic regions across North and South America in order to protect human health and reduce disease burden.
1. Introduction
Coccidioidomycosis, commonly known as Valley fever, is an infectious fungal disease that has gained attention in the United States (US) due to increasing case counts [1]. Humans can contract coccidioidomycosis when they inhale Coccidioides spp. fungal spores. It is estimated that 40% of people who inhale the fungus will become symptomatic, with initial symptoms presenting similar to other causes of pneumonia like bacterial and viral infections [2,3]. Approximately 1–5% of coccidioidomycosis patients have severe disseminated forms of the disease spreading from the lung to the skin, lymph nodes, bone, joints, and/or central nervous system, which can lead to life-threatening meningitis [4]. Approximately 200 people in the US die each year from coccidioidomycosis [1]. Coccidioidomycosis can infect a variety of animals, and has been reported in wildlife (e.g., rodents, armadillos, mountain lions, dolphins, sea lions); livestock (e.g., pigs, cattle, sheep, and llamas); companion animals (e.g., dogs, cats, horses); and non-native animals in captivity (e.g., primates, tigers, rhinoceros, kangaroo) [5]. There are currently two species of Coccidioides defined: C. immitis and C. posadasii, though no clinical differences have been noted between the species [6]. Due to underreporting and under-ascertainment, the true number of coccidioidomycosis cases is thought to be much higher [1]. Moreover, the absence of nationwide coccidioidomycosis surveillance limits our understanding of true disease burden and the progress in studying other fundamental research questions, such as the geographical extent of Coccidioides.
Though coccidioidomycosis has been a known health threat in the US since the 1930s, not all states are currently report disease cases [7,8]. From 1995–2009 and 2011-current, coccidioidomycosis has been defined in the US as a nationally notifiable disease by the US Centers for Disease Control and Prevention (CDC) and the Council of State and Territorial Epidemiologists (CSTE) [9]. A notifiable disease means there is a standardized case definition and health departments voluntarily submit case count data to the CDC’s National Notifiable Disease Surveillance System; it does not mandate health departments to report the disease. Federally funded facilities and tribal governments are not required to report cases to local health agencies, either [10]. Serological testing for coccidioidomycosis is primarily performed in large commercial laboratories that automatically report laboratory-positive cases to public health agencies, so cases in these communities may still be reported. Some local lawmakers and state health departments have gone a step further to define coccidioidomycosis as a reportable disease in their state; this requires healthcare professionals and laboratories to notify public health departments of cases that meet the coccidioidomycosis CSTE case definition [8]. Currently, 26 US states and the District of Columbia are required to report coccidioidomycosis cases (Figure 1), though the states reporting likely doesn’t encompass the current estimated endemic area.
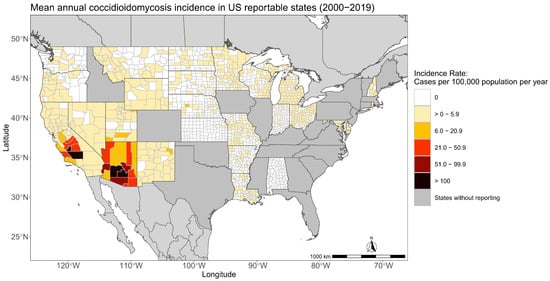
Figure 1.
States in the US where coccidioidomycosis is a reportable disease have case incidence in color. Coccidioidomycosis is not reportable in gray states.
The CDC and other researchers estimate the area endemic to coccidioidomycosis stretches across the arid to semi-arid portions of the western US [7,8,11]. In the US, the CDC currently estimates Coccidioides may live in 12 states (Arizona, California, Colorado, Idaho, New Mexico, Nevada, Oklahoma, Oregon, Texas, Utah, Washington, and Wyoming), but highlights the potential range across 5 more states in the western US (Kansas, Montana, Nebraska, North Dakota, and South Dakota) [7]. A recently developed climate-constrained niche model also estimates 12 states may currently be endemic, but differs slightly from the CDC estimate of where Coccidioides may live in that it defines a portion of Kansas and the extreme southwest corner of Nebraska as endemic [11]. Both estimates consider Coccidioides to be living in Arizona, California, Colorado, Idaho, Nevada, New Mexico, Oklahoma, Texas, Utah, and Washington. Four states where either the CDC or the climate-constrained niche model estimate Coccidioides to be living that do not report coccidioidomycosis cases are Colorado, Idaho, Oklahoma, and Texas. The disease is also endemic to Latin America and cases have been reported in México, Guatemala, Honduras, Colombia, Venezuela, Brazil, Paraguay, Bolivia, and Argentina [12].
Texas is a prime example of where scientific evidence has long supported the state as likely endemic, but coccidioidomycosis is not reportable. Coccidioidomycosis cases have been documented in Texas since the 1930s [13]. Outbreaks of coccidioidomycosis cases were documented in the 1960s in Texas, too: one outbreak in 1965 in El Paso, TX was associated with exposure to a rodent burrow, while a second outbreak was reported in 1966 in Beeville, TX [14,15]. A historical skin test study from the 1950s indicating exposure to Coccidioides indicated parts of western Texas to be just as endemic as Kern County, California, with some areas in western Texas presenting with 50–70% of people reacting positive to coccidioidin [16]. Later, one of the first Coccidioides niche maps highlighted portions of western Texas as suitable for the fungi [17] and a recently developed habitat suitability map shows much of the western half of Texas as moderate to highly favorable for Coccidioides growth [18]. Recent disease surveillance studies support Texas as endemic, though it is difficult to estimate the severity of endemicity compared to other endemic states [19,20]. Despite this information, coccidioidomycosis is currently reported only by El Paso County, the westernmost county in Texas.
The absence of coccidioidomycosis case reporting in Texas, and other likely endemic areas in North and South America, threatens public health by reducing awareness of this disease among the community and physicians, likely leading to a higher disease burden. This commentary advocates for all US states, especially those in or nearby current endemic regions, to define coccidioidomycosis as a reportable disease and encourages disease surveillance across other endemic regions in North and South America. We exemplify the need for reporting coccidioidomycosis in other endemic regions outside of the US by examining the history of case reporting in Mexico. This is a call to action to use our scientific knowledge of coccidioidomycosis and Coccidioides in order to mitigate the national and international health impacts of this disease. Doing so will help advance the science and outstanding questions on coccidioidomycosis, including shortening the time to diagnosis, improving antifungal drug and vaccine development, determining where the disease is endemic, identifying the environmental drivers of interannual disease variability, and understanding the severity of endemicity outside the US.
2. Clinical Benefits of Coccidioidomycosis as a Reportable Disease
One of the most important public health mechanisms for recognizing, managing, and preventing infectious diseases entails surveillance and reporting of cases. Disease surveillance can increase disease awareness among physicians, which can reduce the time to diagnosis [21]. It is a well-recognized phenomenon in clinical medicine that diseases recognized early have a better chance of good outcome than those recognized belatedly [22]. This is true for coccidioidomycosis [23]. In the highly endemic region of Tucson, Arizona, over 40% of patients with coccidioidomycosis had a diagnosis delay >1 month and many delays resulted in unnecessary courses of antibiotics [23]. The median time among 276 patients between onset of symptoms and coccidioidomycosis diagnosis in this highly endemic region was 23 days [23]. This substantial delay is even greater in non-endemic areas. In an enhanced surveillance study in 14 states outside of the highest endemic regions or in areas considered not endemic (Louisiana, Michigan, Minnesota, Missouri, Montana, Nevada, New Mexico, North Dakota, Ohio, Oregon, Pennsylvania, Utah, Wisconsin, and Wyoming), the median time among 186 patients between seeking healthcare and coccidioidomycosis diagnosis was roughly two weeks longer (38 days), with an incredible range from 1–1654 days [24]. 70% of the patients were originally misdiagnosed and 84% of patients were incorrectly prescribed antibiotics [24]. In a study of coccidioidomycosis case outcomes from 2006–2015 in Utah, approximately one-third of patients were diagnosed with coccidioidomycosis as a workup for malignancy [25], suggesting there should be additional awareness efforts for diagnosing coccidioidomycosis. A first-step action for increasing disease awareness, shortening the time to diagnosis, avoiding unnecessary courses of antibiotics, and avoiding the costs associated with these outcomes is mandatory disease reporting.
Coccidioidomycosis is also endemic to specific regions of the US that are frequently a destination for travel, especially by older people, and result in travel-associated cases [26]. Disease awareness through reporting may help clinicians, especially those practicing outside of endemic areas, consider coccidioidomycosis in their differential diagnosis if they have some understanding of disease prevalence [21]. Prevalence data are produced when there is a reporting mechanism in place.
It is logistically impossible to require the reporting of every infectious disease, so what determines which conditions are reportable? In general, the main considerations include the severity of disease, the cost of managing the disease, acquisition and transmission mechanisms, and what measures are available to mitigate risk.
Persons most at risk for coccidioidomycosis include those with underlying co-morbid disease, such as diabetes, and immunosuppressed patients, particularly those after bone or organ transplantation, those on immunomodulating therapy for autoimmune diseases, and persons with advanced HIV. Pregnancy may also pose increased risk of disease [27]. The proportion of the population with these conditions is increasing, which means the number of persons at risk for severe coccidioidomycosis is also on the rise [28]. Apart from host status, severe disease does occur in people with no recognized immunocompromising disorder, too [29]. The potential for severe outcomes, especially among the increasing numbers of vulnerable and immunocompromised populations, is amplified when the diagnosis is delayed.
For a 2000–2015 baseline time period, the estimated annual medical costs, lost income, and economic welfare losses for coccidioidomycosis in the US were USD 400,000 per case, and the annual average total cost was USD 3.9 billion per year [30]. For 10,359 patients diagnosed in Arizona in 2019, a University of Arizona Health Sciences study estimated total lifetime costs at USD 736 million [31]. That estimate did not include non-hospital medical costs, demands on limited primary care resources, loss of work, and the potential for long term co-morbidities associated with this disease. These cost estimates highlight the impact of the disease on the US economy and the community, especially the highly endemic states such as Arizona.
Since the primary transmission pathway for Coccidioides is in the natural environment via soil disturbance and dust, there is relatively little that can be done to mitigate the risk of this disease. The California Division of Occupational Safety and Health (Cal/OSHA) lists numerous recommendations such as training workers on the risk of coccidioidomycosis, limiting worker exposure to dust, wearing respiratory protection with particulate filters rated as N95, N99, N100, P100, or HEPA, and reporting potential symptoms of coccidioidomycosis immediately to a supervisor [32]. For dust mitigation, Cal/OSHA recommends actions such as minimizing disturbing soil, using water or a soil stabilizer to limit dust, suspending work during high winds, and providing enclosed air-conditioned cabs for vehicles that generate dust [32]. The CDC informational webpage on coccidioidomycosis prevention acknowledges that, “it’s very difficult to avoid breathing in the fungus Coccidioides in areas where it’s common in the environment” [33].
From the combination of increasing morbidity and mortality from coccidioidomycosis, the high economic and health impact of the disease, and limited mechanisms to mitigate the risk of contracting coccidioidomycosis, it is a compelling case for all US states to define coccidioidomycosis as reportable disease for the clinical benefits alone. The majority of these benefits extend to the veterinary sector, too. Clinical animal cases are likely highly underreported and limited knowledge of the potential for locally acquired infection may delay diagnosis [34]. Sharing surveillance data between veterinary and human medicine could help raise disease awareness, especially since animals can act as early indicators for a biothreat [35].
3. Understanding the Public Health Impact of Valley Fever Can Better Justify Antifungal Drug and Vaccine Development
Patients can benefit from an antifungal and/or other immune therapeutics before the onset of disseminated coccidioidomycosis, so early diagnosis of this disease is crucial. Coccidioidomycosis cases are currently confirmed as positive by serology tests. Diagnostic methods of coccidioidomycosis and clinical practice have been well reviewed [36]. Human genetic variations can contribute to high incidence rates of disseminated disease among specific populations, such as African Americans, Asian/Pacific Islanders, and Latinos, compared to European Americans [27,37,38,39]. Furthermore, allelic variations of immune factors of the IL-12-IFN-γ signaling, innate immune sensing, NFκB signaling, and IL-17 signaling molecules have been predicted to associate with the severity of coccidioidomycosis [40,41]. Altogether, those genetic correlation studies suggest that nationwide surveillance may facilitate the rapid identification of coccidioidomycosis patients with any at-risk conditions.
A more complete estimate of the national burden of coccidioidomycosis through nationwide surveillance would further justify the development of novel antifungal drugs. The Infectious Diseases Society of America clinical practice guidelines recommend antifungal chemotherapy for patients at risk for complications, such as moderate to severe pulmonary or disseminated disease [42]. Fluconazole, triazole compounds, and Amphotericin B are the most frequently prescribed antifungal agents for long-term and short-term treatment of moderate to disseminated disease. Fluconazole interacts with 14-demethylase, a cytochrome P450 enzyme that is responsible for catalyzing the conversion of lanosterol to ergosterol, thereby disrupting the stability of the fungal cell membrane [43]. Surprisingly, increased resistance to fluconazole (>16 µg/mL) is documented in >37% of clinical Coccidioides isolates [44]. The parasitic lifecycle of Coccidioides is unique amongst the medically important fungi as they grow into multinucleated spherules (estimated to be over 1000 nuclei). The fungal cell wall is surrounded by layers of the spherule outer wall (SOW) that is composed of >60% phospholipids/lipids [45,46]. Perhaps the unique cell wall structure and chemical components partly contribute to fluconazole drug resistance. However, it remains unclear how Coccidioides resistance to fluconazole correlates to clinical therapeutic outcomes. Amphotericin B is an effective antifungal, but the acute and long-term nephrotoxicity and hepatotoxicity raise concerns. Additionally, there are several promising drug candidates in late-stage clinical development [47,48]. Current drug screening efforts employ a repurposing strategy to identify clinically approved drugs with novel antifungal activity [49]. It is estimated that the cost of drug development from research to clinical use can take USD 314 million to USD 2.8 billion [50]. The screening of repurposing drug libraries can shorten the development time, and it also reduces the cost. Surveillance of coccidioidomycosis cases can provide information on the patient market needs and serve as better justification for anti-Coccidioides drug development.
Surveillance data showing the steady rise of coccidioidomycosis cases support the need to develop prophylactic and immunotherapeutic vaccines to manage this disease. Prophylactic vaccines can be administered to naïve individuals who have yet encountered Coccidioides to prevent contracting coccidioidomycosis. Immunotherapeutic vaccination can be deployed to coccidioidomycosis patients to enhance their immune responses against this disease. Copious data justify that a vaccine against coccidioidomycosis is feasible, as those who recover from coccidioidomycosis often develop life-long protective immunity [51]. The National Institute of Allergy and Infectious Diseases (NIAID) has set forth a strategic plan to have a human vaccine for coccidioidomycosis undergo clinical trials by 2030 [52]. A whole cell vaccine using formalin-killed spherules (FKS) has been evaluated in a clinical phase III trial against coccidioidomycosis. However, the development of FKS for clinical use was halted due to lack of protective efficacy [53]. Live-attenuated ∆T and the ∆CPS1 vaccines have been created and both of those vaccines show great protective efficacies against pulmonary coccidioidomycosis in animal models [54,55,56,57]. The live attenuated vaccines are excellent tools for exploring the immune protective mechanisms against Coccidioides and they may be developed into veterinary vaccines. Despite the apparent ability of a live-attenuated vaccine to elicit and maintain long-term protective memory responses to Coccidioides infection, it poses significant concerns for individuals with underlying conditions of compromised cell-mediated immune systems. Generation of a subunit vaccine using recombinant proteins or mRNA molecules of Coccidioides antigens are a safer strategy in the design of a clinically acceptable reagent. Most subunit vaccines are chemically defined and pure. Many investigators have focused on identifying Coccidioides antigens which can be used in the development of subunit vaccines [58,59,60]. Additional critical barriers to progress towards the development of a subunit vaccine against coccidioidomycosis are (i) understanding the fundamental knowledge of protective immunity against Coccidioides infection; (ii) obtaining protective efficacy and safety data; (iii) reducing the cost by developing a multivalent vaccine that can confer protection against both C. posadasii and C. immitis; (iv) establishing a translational vaccine platform that can be easily scaled up for vaccine production; and (v) identifying who should get vaccinated for coccidioidomycosis. Nationwide disease surveillance would help identify novel risk factors, describing specific eligibility criteria for an effective design of future vaccine and drug clinical trials. Furthermore, determining fungal susceptibility would allow clinicians to decide the use of prophylactic or immunotherapeutic vaccination for patients based on their history of Coccidioides.
4. Delineating the Environmental Drivers of Coccidioides and Coccidioidomycosis Disease Dynamics and an Estimate of the Current Endemic Area
Reporting coccidioidomycosis cases would help lead to a clearer delineation of the endemic area for this disease, any emergent changes in endemicity, and insight on the environmental conditions that support the endemic area. Comprehensive soil sampling campaigns for the presence of Coccidioides are time and labor-intensive, and unless such campaigns are extremely intensive, they may be unreliable due to the patchy distribution of Coccidioides in soil [61]. Disease surveillance acts as a proxy for the presence of the fungi and the transmissibility of the fungi to humans. Disease surveillance would be most beneficial in areas where climate or soil conditions are estimated to currently permit endemicity, yet the state or region is not currently reporting [11,18]. In the US, Texas is a large state with basic climate patterns of annual mean temperatures increasing from north to south and precipitation increasing from west to east [62]. These patterns offer a natural experiment in analyzing how coccidioidomycosis case counts, and by proxy the presence of Coccidioides, vary with climate conditions. Disease surveillance across the Americas as a whole could help define differing environmental controls on Coccidioides and coccidioidomycosis disease dynamics, especially in light of different Coccidioides species.
Disease surveillance may act as an early indicator of the shift in the geographical extent of Coccidioides and spread of coccidioidomycosis in response to climate change. As temperatures warm and precipitation levels stay dry in the western US, the endemic area for coccidioidomycosis is expected to expand northward [11]. Proactive surveillance in areas projected to be endemic in the future will help raise disease awareness among physicians and track what new communities may be at risk for contracting coccidioidomycosis.
Outside the US, there is less knowledge on the endemic area for coccidioidomycosis, but understanding the environmental controls on US disease cases may provide insight for future studies. We used the methods developed in Gorris et al. (2019) to estimate the regions across North and South America that may be currently endemic to coccidioidomycosis, and therefore, areas we encourage to create disease surveillance programs (Figure 2) [11]. We used mean annual temperature and precipitation from TerraClimate [63] at its native 4 km grid mesh averaged from 2000–2020. We plotted areas in purple that meet the two climate thresholds for endemicity: mean annual temperatures above 10.7 °C and mean annual precipitation levels below 600 mm/year. The resultant endemicity map shows 12 countries as potentially endemic to coccidioidomycosis: the United States, the United Mexican States, Argentina, Bolivia, Brazil, Chile, Colombia, Dominican Republic, Ecuador, Paraguay, Peru, and Venezuela.
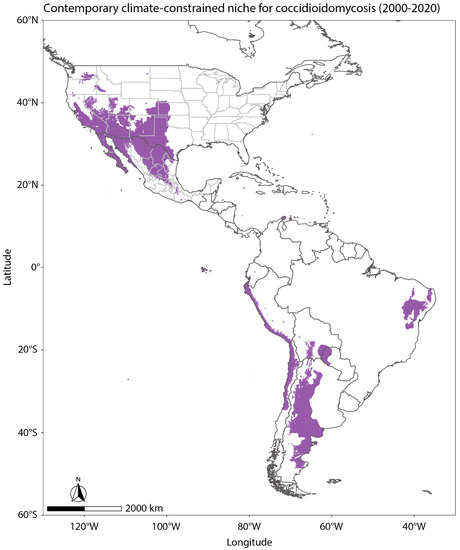
Figure 2.
Using the methods from Gorris et al. (2019) [11] and mean annual temperature and precipitation from TerraClimate [63] averaged from 2000–2020, areas plotted in purple meet the two climate thresholds for endemicity: mean annual temperature above 10.7 °C and mean annual precipitation below 600 mm/year. The resultant endemicity map shows 12 countries as potentially endemic to coccidioidomycosis: the United States, the United Mexican States, Argentina, Bolivia, Brazil, Chile, Colombia, Dominican Republic, Ecuador, Paraguay, Peru, and Venezuela.
Confidence in relating outbreaks of coccidioidomycosis to environmental drivers, like dust storms, requires detailed disease surveillance [64,65]. Although the ability of humans to be infected by Coccidioides through wind-eroded dust, and under what conditions it may happen, is subject to debate [65,66], dust exposure has long been hypothesized as a primary mechanism for contracting coccidioidomycosis [67]. A well-known outbreak of coccidioidomycosis occurred in 1977 following a large dust storm originating in the San Joaquin Valley of California [68,69]. The Chihuahuan Desert, an endemic area for Coccidioides, experiences some of the highest frequencies of windblown dust in the Western Hemisphere [70], with dust originating from southeastern Arizona across southern New Mexico and far west Texas, as well as from sources in Chihuahua, Mexico [71,72,73,74] (Figure 3). Many dust events originate upwind of Texas and blow into the state, such as from the Chihuahuan Desert regions of New Mexico, Chihuahua (Mexico), and southeastern Arizona [71,72,73,74,75] (Figure 3), and the southwestern Great Plains of eastern New Mexico [76,77]–all hypothesized coccidioidomycosis endemic regions. Dust originating in or upwind of the drylands of western Texas can be transported downwind to the Texas population centers of San Antonio [73], Dallas-Fort Worth [78,79], and Houston [80], and further beyond into neighboring states such as Oklahoma and Kansas [76,78,81,82] (Figure 3) and as far as the northeastern United States and Canada [81,83]. The desert regions of the southwestern US are not only endemic for coccidioidomycosis, but could also cause long-range transport of Coccidioides if the fungus remains viable. Enhanced, nationwide coccidioidomycosis surveillance will help us to better understand the mechanisms of population exposure to dust and Coccidioides and communicate the risk associated with dust exposure [65].
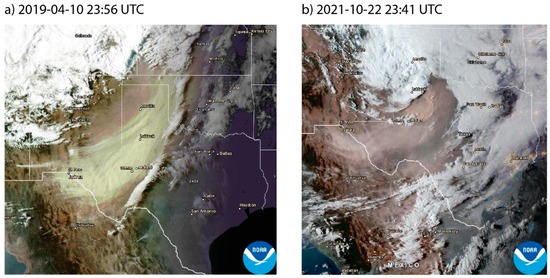
Figure 3.
Two examples of recent dust events in Texas and the surrounding region on (a) 10 April 2019 at 23:56 UTC and (b) 22 October 2021 at 23:41 UTC, captured by the GOES-16 satellite and obtained from AerosolWatch (https://www.star.nesdis.noaa.gov/smcd/spb/aq/AerosolWatch/, accessed on 21 August 2022), showing dust transport from Mexico into Texas (a,b) and from Texas into Oklahoma and Kansas (a).
5. Beyond Borders: Reporting Coccidioidomycosis in Mexico
The United Mexican States (Mexico) is another highly endemic area for coccidioidomycosis, though case reporting in the country hasn’t been uniform and it’s thought to be highly underreported. Coccidioidomycosis is the largest systemic fungal infection in Mexico with the first case having been reported in 1945 [12]. Since then, case reporting practices have varied through time. In 1979, the Ministry of Health (MH) of Mexico started weekly announcements of new disease cases. In this registry, coccidioidomycosis cases were only reported from 1989 to 1994 (Figure 4). Starting in 1995, the MH began to operate the National Epidemiological Surveillance System (SINAVE, in Spanish). SINAVE reports 143 diseases subject to conventional surveillance; however, it does not include coccidioidomycosis. Later, in 2000, the MH established a dynamic information consultation service, based on a Multidimensional Online Analytical Processing (MOLAP) technology called Dynamic Cubes, which produces non-obligatory daily reports that record all the diagnoses made by doctors, whether or not they are subject to epidemiological surveillance. Coccidioidomycosis appears again in this database.
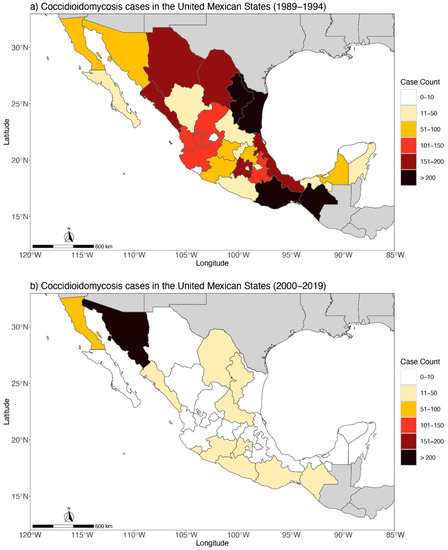
Figure 4.
(a) Distribution of the 3691 human coccidioidomycosis cases in the United Mexican States from 1989 to 1994 and (b) 766 human coccidioidomycosis cases in the United Mexican States from 2000 to 2019.
It is important to recognize the work of González-Ochoa in the history of coccidioidomycosis reporting, who was a medical mycologist dedicated to studying diseases in the Mexican population, especially in the 1970s and early 1980s. Both González-Ochoa’s extensive research, as well as his administrative position, were instrumental for the recognition of mycotic infections in the Mexican national health system, which probably motivated the extensive recording of cases in the period 1989–1994. From 1989 to 1994, there were 3691 cases of coccidioidomycosis documented in the MH annual reports in Mexico (Figure 4a). Unfortunately, these annual reports do not mention if the diagnosis was made through clinical, microbiology, or immunology tools.
After González-Ochoa’s retirement, for six years, cases of coccidioidomycosis were not recorded. Case reporting began again in 2000. The case data obtained from 2000 to 2019 do not record how the diagnosis was made, but it does show that morbidity decreased by approximately 80% compared to the previous period (1989–1994). Further, the distribution of cases is practically confined to just two states: Sonora and Baja California (Figure 4b). The data are paradoxical because current literature mentions the southern states of the US and the northern states of Mexico as the main global endemic area for coccidioidomycosis. This bias in the data suggests coccidioidomycosis could be a diminishing health concern in Mexico. However, since the clinical symptoms of coccidioidomycosis are very frequently confused with other respiratory tract conditions, there is likely an underreporting of cases in Mexico, which is also supported by the following data:
- An epidemiological surveillance program has never been implemented to control or prevent this infection
- From 2010 to 2012, a sub-national survey of intradermal reaction with coccidioidin was carried out in 1081 people from 9 states, and 29.5% of people tested positive for the antigen [84]. The percentage of infection is not negligible, especially if one takes into account that the samples were taken from states with environmental conditions not associated with the presence of Coccidioides
- There are frequent national medical publications of case studies of disseminated coccidioidomycosis in both children and adults [12,85,86], especially in the states of Sonora, Baja California, Coahuila, and Nuevo León
- The Dynamic Cubes [87] of the National Health System continues to register deaths whose diagnosis is coccidioidomycosis
From inconsistencies in case reporting, it is difficult to draw conclusions on the geographic distribution of coccidioidomycosis in Mexico. Coccidioidin antigen studies carried out in Sonora show that more than 50% of the population react positively [88]. In Baja California, surveys with coccidioidin carried out in 4 municipalities during 2018–2020 showed that 8% of the population is positive for the antigen [89]. In the Dynamic Cubes model, both the place of diagnosis and the origin of the patient are recorded. From these data, we observe that the vast majority of cases recorded in Sonora and Baja California are patients who reside in those same states. Around half of Mexico, especially in northern states, has a dry to very dry climate, conditions that support the presence of coccidioidomycosis throughout the country; however, Chiapas, Oaxaca, and Veracruz are states with large areas of tropical and temperate climates, environments not associated with the presence of Coccidioides. For this reason, cases reported in this region are likely where the diagnoses were made, but the fungus is not endemic.
In Mexico, the MH has, because of an established mandate, both the duty to collect, integrate, and disseminate health information necessary for planning, programming, budgeting, and controlling the national health system as well as the duty to know the status and progression of public health. Regrettably, coccidioidomycosis in Mexico is a neglected disease. The quantitative and qualitative concepts that should be used by epidemiologists to study coccidioidomycosis in Mexico to make pertinent decisions are unknown. A more comprehensive method of diagnosing, reporting, collecting, and publishing the case reports of coccidioidomycosis in Mexico would help address these issues, especially delineating the endemic regions in Mexico.
6. Discussion
While coccidioidomycosis case counts are already subject to underreporting and under-ascertainment, the lack of uniformity in US states reporting coccidioidomycosis cases, especially those in endemic areas, further exacerbates an underestimation in disease risk. In turn, this underestimation is translated into uncertainties in current research on disease dynamics. Underreporting and under-ascertainment, processes known as imperfect detection, conflate with non-uniform disease surveillance. When creating statistical models of disease counts, some regions may be estimated to have minimal disease counts when they actually could have similar levels of disease with lower rates of reporting. Another issue that arises is that cases can be reported in states where the environmental risk is very low. Oftentimes, this is associated with people that have traveled to a region with high coccidioidomycosis presence and are diagnosed after traveling. This can lead to inflated disease rates in areas where Coccidioides is less likely to exist. Eliminating the complications that arise from a lack of uniform disease surveillance will help improve our models of disease burden of coccidioidomycosis.
Of course, there are logistical hurdles for each state defining coccidioidomycosis as a reportable disease. The biggest hurdle is the time and energy of the reporting provider. First, the list of reportable diseases is long and may be challenging for providers to remember which diseases they must report. Second, submitting the appropriate provider report requires time and energy. However, many of the laboratory confirmed tests for coccidioidomycosis automatically send to public health agencies, eliminating the need for providers to submit paperwork. Also, the providers that are more likely to diagnose a coccidioidomycosis case are likely well versed on how to report cases since they are likely dealing with other reportable infectious diseases like tuberculosis.
We return again to discuss the case of Texas, where incidence of coccidioidomycosis in the state is unknown since it’s not a reportable disease, but numerous lines of evidence support Texas as a highly endemic area. Almost 9% of the US population lives in Texas and the state accounts for nearly a third of population growth in the country [90]. Based on historical population growth, in 2022 the population of Texas will be approaching 30 million people [91]. If one assumes the incidence rate in Texas is only 10% of that reported in Arizona during 2019 (14 cases per 100,000 population, a very conservative estimate) [1,92], then approximately 4200 cases of coccidioidomycosis may have been reported in Texas. In another comparison, since historical coccidioidin reactivity rates in western Texas were similar to Kern County, CA, and one assumes the incidence rate of Texas is 10% that of Kern County in 2019 (37 cases per 100,000 population), then approximately 11,100 cases of coccidioidomycosis may have been reported in Texas. The total number of reported coccidioidomycosis cases across states reporting in 2019 was 20,003, so implementing disease surveillance in Texas could very well drastically increase the number of reported cases in the US as a whole.
In addition to population growth, there is evidence certain occupations, such as workers in the oil and gas industry, a growth sector in Texas, may be at increased risk of infection [20]. Conversely, brucellosis and babesiosis ARE reportable diseases in Texas. In 2018, there were 18 cases of brucellosis and 2 cases of babesiosis reported [93]. Both of these conditions are generally more innocuous than coccidioidomycosis in terms of morbidity and mortality, and brucellosis is now nearly eliminated in livestock via a vaccine, so risk to humans is lower as well [94].
Idaho and Colorado are two other states where disease surveillance would be beneficial to understand if there is local acquisition of coccidioidomycosis. Though Idaho is generally considered to be far outside of the traditionally recognized endemic area of the southwestern US, environmental conditions in areas throughout the state are similar to other endemic regions for Coccidioides. Coccidioides has been isolated over six years in a nearby area in southeastern Washington State [95,96]. The higher resolution climate-constrained niche model for Coccidioides (Figure 2) indicates areas extending eastward into Idaho from the endemic region in southeastern Washington State may be suitable for Coccidioides, as well as areas in the western Snake River Plain. This includes Boise, the most populous city in Idaho. In Colorado, almost a quarter of the state is highlighted as potentially suitable for Coccidioides in the climate-constrained niche model, mostly in the plains area east of the Rocky Mountains (Figure 2). This area is abundant in grass and pastureland [97] and if cattle or other livestock heavily graze, there can be increased soil erosion [98] which could lead to exposure of dust-borne Coccidioides spores.
Since population growth in endemic regions of the USA is high, more US states reporting coccidioidomycosis cases is not only important from a healthcare and economic standpoint, it is the “right thing to do” to equip clinicians as they care for patients. As our climate changes and the potential endemic region for coccidioidomycosis expands northward, surveillance programs will help track the geographical expansion of the disease and alert naïve communities when they are at risk of contracting coccidioidomycosis. Understanding the burden of case counts will help support antifungal drug and vaccine development, especially as new populations become exposed to Coccidioides. Using our scientific knowledge of coccidioidomycosis and recognizing the numerous benefits in reporting cases, we advocate that coccidioidomycosis becomes a reportable condition in the US and highly recommend surveillance programs in other endemic areas outside of the US to reduce the health effects from coccidioidomycosis.
Author Contributions
Conceptualization, M.E.G. and K.A.K.; All authors contributed to both writing—original draft preparation and review and editing; visualization, M.E.G., K.A-D. and A.G. All authors have read and agreed to the published version of the manuscript.
Funding
M. E. Gorris, A. Greene, and K. A. Kaufeld gratefully acknowledge support from the Laboratory Directed Research and Development (LDRD) program at Los Alamos National Laboratory (Grant XXH6). T. E. Gill acknowledges support from NASA grant 80NSSC19K0195.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Restrictions apply to the availability of these data since they are public health data from the CDC and Ministry of Health of Mexico. Please contact the corresponding author for more information.
Acknowledgments
We thank the CDC for their support in sharing Valley fever case data. This work is approved for distribution under LA-UR-22-30718. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of their affiliations, including Los Alamos National Laboratory (LANL). LANL, an affirmative action/equal opportunity employer, is managed by Triad National Security, for the National Nuclear Security Administration of the USA Department of Energy under contract 89233218CNA000001. The funders had no role in the study design, data analysis, decision to publish, or preparation of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Centers for Disease Control and Prevention. Valley Fever (Coccidioidomycosis) Statistics. 2022. Available online: https://www.cdc.gov/fungal/diseases/coccidioidomycosis/statistics.html (accessed on 1 December 2022).
- Benedict, K.; Kobayashi, M.; Garg, S.; Chiller, T.; Jackson, B.R. Symptoms in blastomycosis, coccidioidomycosis, and histoplasmosis versus other respiratory illnesses in commercially insured adult outpatients—United States, 2016–2017. Clin. Infect. Dis. 2021, 73, e4336–e4344. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.E.; Whiting, E.G.; Baker, E.E.; Rosenberger, H.G.; Beard, R.R.; Saito, M.T. The use of coccidioidin. Am. Rev. Tuberc. 1948, 57, 330–360. [Google Scholar] [CrossRef] [PubMed]
- Bays, D.J.; Thompson, G.R. Coccidioidomycosis. Infect. Dis. Clin. 2021, 35, 453–469. [Google Scholar] [CrossRef] [PubMed]
- Barker, B.M. Coccidioidomycosis in animals. In Emerging and Epizootic Fungal Infections in Animals; Seyedmousavi, S., de Hoog, G.S., Guillot, J., Verweij, P.E., Eds.; Springer International Publishing: Berlin/Heidelberg, Germany, 2018; pp. 81–114. [Google Scholar] [CrossRef]
- Kollath, D.R.; Miller, K.J.; Barker, B.M. The mysterious desert dwellers: Coccidioides immitis and Coccidioides posadasii, causative fungal agents of coccidioidomycosis. Virulence 2019, 10, 222–233. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Valley Fever Maps. 2020. Available online: https://www.cdc.gov/fungal/diseases/coccidioidomycosis/maps.html (accessed on 1 December 2022).
- Williams, S.L.; Chiller, T. Update on the epidemiology, diagnosis, and treatment of coccidioidomycosis. J. Fungi 2022, 8, 666. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Coccidioidomycosis/Valley Fever (Coccidioides spp.). 2021. Available online: https://ndc.services.cdc.gov/conditions/coccidioidomycosis/ (accessed on 1 December 2022).
- McCotter, O.; Kennedy, J.; McCollum, J.; Bartholomew, M.; Iralu, J.; Jackson, B.R.; Haberling, D.; Benedict, K. Coccidioidomycosis among American Indians and Alaska Natives, 2001–2014. Open Forum Infect. Dis. 2019, 6, ofz052. [Google Scholar] [CrossRef]
- Gorris, M.E.; Treseder, K.K.; Zender, C.S.; Randerson, J.T. Expansion of coccidioidomycosis endemic regions in the United States in response to climate change. GeoHealth 2019, 3, 10. [Google Scholar] [CrossRef]
- Laniado-Laborín, R.; Arathoon, E.G.; Canteros, C.; Muñiz-Salazar, R.; Rendon, A. Coccidioidomycosis in Latin America. Med. Mycol. 2019, 57 (Suppl. 1), S46–S55. [Google Scholar] [CrossRef]
- Caldwell, C.T. Coccidioidal granuloma: A report of three cases recognized in Texas. Tex. State J. Med. 1932, 28, 327–333. [Google Scholar]
- Roberts, P.L.; Lisciandro, R.C. A community epidemic of coccidioidomycosis. Am. Rev. Respir. Dis. 1967, 96, 766–772. [Google Scholar] [CrossRef]
- Teel, K.W.; Yow, M.D.; Williams, T.W. A localized outbreak of coccidioidomycosis in southern Texas. J. Pediatr. 1970, 77, 65–73. [Google Scholar] [CrossRef]
- Edwards, P.Q.; Palmer, C.E. Prevalence of sensitivity to coccidioidin, with special reference to specific and nonspecific reactions to coccidioidin and to histoplasmin. Dis. Chest 1957, 31, 35–60. [Google Scholar] [CrossRef] [PubMed]
- Baptista-Rosas, R.C.; Hinojosa, A.; Riquelme, M. Ecological niche modeling of Coccidioides spp. in western North American deserts. Ann. N. Y. Acad. Sci. 2007, 1111, 35–46. [Google Scholar] [CrossRef] [PubMed]
- Dobos, R.R.; Benedict, K.; Jackson, B.R.; McCotter, O.Z. Using soil survey data to model potential Coccidioides soil habitat and inform Valley fever epidemiology. PLoS ONE 2021, 16, e0247263. [Google Scholar] [CrossRef]
- Pena-Ruiz, M.A.; Meza, A.D.; Mulla, Z. Coccidioidomycosis infection in a predominantly Hispanic population. Ann. N. Y. Acad. Sci. 2007, 1111, 122–128. [Google Scholar] [CrossRef] [PubMed]
- Peterson, C.; Chu, V.; Lovelace, J.; Almekdash, M.H.; Lacy, M. Coccidioidomycosis cases at a regional referral center, West Texas, USA, 2013–2019. Emerg. Infect. Dis. 2022, 4, 848. [Google Scholar] [CrossRef]
- Croskerry, P. The importance of cognitive errors in diagnosis and strategies to minimize them. Acad. Med. 2003, 78, 775–780. [Google Scholar] [CrossRef]
- Pruinelli, L.; Westra, B.L.; Yadav, P.; Hoff, A.; Steinbach, M.; Kumar, V.; Delaney, C.W.; Simon, G. Delay within the 3-Hour surviving sepsis campaign guideline on mortality for patients with severe sepsis and septic shock. Crit. Care Med. 2018, 46, 500–505. [Google Scholar] [CrossRef]
- Donovan, F.M.; Wightman, P.; Zong, Y.; Gabe, L.; Majeed, A.; Ynosencio, T.; Bedrick, E.J.; Galgiani, J.N. Delays in coccidioidomycosis diagnosis and associated healthcare utilization, Tucson, Arizona, USA. Emerg. Infect. Dis. 2019, 25, 1745. [Google Scholar] [CrossRef]
- Benedict, K.; Ireland, M.; Weinberg, M.P.; Gruninger, R.J.; Weigand, J.; Chen, L.; Perez-Lockett, K.; Bledsoe, C.; Denny, L.; Cibulskas, K.; et al. Enhanced surveillance for coccidioidomycosis, 14 US States, 2016. Emerg. Infect. Dis. 2018, 24, 1444–1452. [Google Scholar] [CrossRef]
- Carey, A.; Gorris, M.E.; Chiller, T.; Jackson, B.; Beadles, W.; Webb, B.J. Epidemiology, clinical features, and outcomes of coccidioidomycosis, Utah, 2006–2015. Emerg. Infect. Dis. 2021, 27, 2269–2277. [Google Scholar] [CrossRef] [PubMed]
- Diaz, J.H. Travel-related risk factors for coccidioidomycosis. J. Travel Med. 2018, 25, tay027. [Google Scholar] [CrossRef] [PubMed]
- Odio, C.D.; Marciano, B.E.; Galgiani, J.N.; Holland, S.M. Riskfactors for disseminated coccidioidomycosis, United States. Emerg. Infect. Dis. 2017, 23, 308–311. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Trends in aging—United States and worldwide. MMWR. Morb. Mortal. Wkly. Rep. 2003, 52, 101–104, 106. [Google Scholar]
- Fatima, M.; Patel, R.S.; Brunworth, J.R.; Gupta, K.A.; Roach, W.E.; Webeler, P.L.; Mundelein, C.R.; Mansour, M. A case of rapidly progressive coccidioidal meningitis in an immunocompetent patient. Cureus 2022, 14, e28643. [Google Scholar] [CrossRef] [PubMed]
- Gorris, M.E.; Neumann, J.E.; Kinney, P.L.; Sheahan, M.; Sarofim, M.C. Economic valuation of coccidioidomycosis (Valley fever) projections in the United States in response to climate change. Weather. Clim. Soc. 2021, 13, 1. [Google Scholar] [CrossRef]
- Grizzle, A.J.; Wilson, L.; Nix, D.E.; Galgiani, J.N. Clinical and economic burden of Valley fever in Arizona: An incidence-based cost-of-illness analysis. Open Forum Infect. Dis. 2021, 8, ofaa623. [Google Scholar] [CrossRef]
- State of California. Protection from Valley Fever. 2022. Available online: https://www.dir.ca.gov/dosh/valley-fever-home.html (accessed on 1 August 2022).
- Centers for Disease Control and Prevention. Valley Fever (Coccidioidomycosis) Risk & Prevention. 2022. Available online: https://www.cdc.gov/fungal/diseases/coccidioidomycosis/risk-prevention.html (accessed on 1 December 2022).
- James, A.E.; McCall, J.R.; Petersen, K.R.; Wohrle, R.D.; Oltean, H.N. A survey of veterinarians’ knowledge, attitudes and practices regarding an emerging disease: Coccidioidomycosis in Washington state. Zoonoses Public Health 2020, 67, 25–34. [Google Scholar] [CrossRef]
- Gubernot, D.M.; Boyer, B.L.; Moses, M.S. Animals as early detectors of bioevents: Veterinary tools and a framework for animal-human integrated zoonotic disease surveillance. Public Health Rep. 2008, 123, 300–315. [Google Scholar] [CrossRef]
- Johnson, R.H.; Sharma, R.; Kuran, R.; Fong, I.; Heidari, A. Coccidioidomycosis: A review. J. Investig. Med. Off. Publ. Am. Fed. Clin. Res. 2021, 69, 316–323. [Google Scholar] [CrossRef]
- Krogstad, P.; Johnson, R.; Garcia-Lloret, M.I.; Heidari, A.; Butte, M.J. Host-pathogen interactions in coccidioidomycosis: Prognostic clues and opportunities for novel therapies. Clin. Ther. 2019, 41, 1939–1954.e1. [Google Scholar] [CrossRef] [PubMed]
- Louie, L.; Ng, S.; Hajjeh, R.; Johnson, R.; Vugia, D.; Werner, S.B.; Talbot, R.; Klitz, W. Influence of host genetics on the severity of coccidioidomycosis. Emerg. Infect. Dis. 1999, 5, 672–680. [Google Scholar] [CrossRef] [PubMed]
- Seitz, A.E.; Prevots, D.R.; Holland, S.M. Hospitalizations associated with disseminated coccidioidomycosis, Arizona and California, USA. Emerg. Infect. Dis. 2012, 18, 1476–1479. [Google Scholar] [CrossRef] [PubMed]
- Hsu, A.P.; Korzeniowska, A.; Aguilar, C.C.; Gu, J.; Karlins, E.; Oler, A.J.; Chen, G.; Reynoso, G.V.; Davis, J.; Chaput, A.; et al. Immunogenetics associated with severe coccidioidomycosis. JCI Insight 2022, 7, e159491. [Google Scholar] [CrossRef] [PubMed]
- Hung, C.-Y.; Hsu, A.P.; Holland, S.M.; Fierer, J. A review of innate and adaptive immunity to coccidioidomycosis. Med. Mycol. 2019, 57 (Suppl. 1), S85–S92. [Google Scholar] [CrossRef]
- Galgiani, J.N.; Ampel, N.M.; Blair, J.E.; Catanzaro, A.; Geertsma, F.; Hoover, S.E.; Johnson, R.H.; Kusne, S.; Lisse, J.; MacDonald, J.D.; et al. Executive summary: 2016 Infectious Diseases Society of America (IDSA) Clinical Practice Guideline for the Treatment of Coccidioidomycosis. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2016, 63, 717–722. [Google Scholar] [CrossRef]
- Van den Bossche, H.; Willemsens, G.; Cools, W.; Lauwers, W.F.; Le Jeune, L. Biochemical effects of miconazole on fungi. II. Inhibition of ergosterol biosynthesis in Candida albicans. Chem.-Biol. Interact. 1978, 21, 59–78. [Google Scholar] [CrossRef]
- Thompson, G.R.; Barker, B.M.; Wiederhold, N.P. Large-scale evaluation of in vitro Amphotericin B, triazole, and echinocandin activity against Coccidioides species from U.S. institutions. Antimicrob. Agents Chemother. 2017, 61, e02634-16. [Google Scholar] [CrossRef]
- Hung, C.-Y.; Yu, J.-J.; Seshan, K.R.; Reichard, U.; Cole, G.T. A parasitic phase-specific adhesin of Coccidioides immitis contributes to the virulence of this respiratory Fungal pathogen. Infect. Immun. 2002, 70, 3443–3456. [Google Scholar] [CrossRef]
- Peláez-Jaramillo, C.A.; Jiménez-Alzate MD, P.; Araque-Marin, P.; Hung, C.-Y.; Castro-Lopez, N.; Cole, G.T. Lipid secretion by parasitic cells of Coccidioides contributes to disseminated disease. Front. Cell. Infect. Microbiol. 2021, 11, 592826. [Google Scholar] [CrossRef]
- Hoenigl, M.; Sprute, R.; Egger, M.; Arastehfar, A.; Cornely, O.A.; Krause, R.; Lass-Flörl, C.; Prattes, J.; Spec, A.; Thompson, G.R.; et al. The antifungal pipeline: Fosmanogepix, Ibrexafungerp, Olorofim, Opelconazole, and Rezafungin. Drugs 2021, 81, 1703–1729. [Google Scholar] [CrossRef] [PubMed]
- Thompson, G.R.; Lewis, J.S.; Nix, D.E.; Patterson, T.F. Current concepts and future directions in the pharmacology and treatment of coccidioidomycosis. Med. Mycol. 2019, 57 (Suppl. 1), S76–S84. [Google Scholar] [CrossRef] [PubMed]
- Wall, G.; Lopez-Ribot, J.L. Screening repurposing libraries for identification of drugs with novel antifungal activity. Antimicrob. Agents Chemother. 2020, 64, e00924-20. [Google Scholar] [CrossRef] [PubMed]
- Wouters, O.J.; McKee, M.; Luyten, J. Estimated research and development investment needed to bring a new medicine to market, 2009–2018. JAMA 2020, 323, 844–853. [Google Scholar] [CrossRef]
- Castro-Lopez, N.; Hung, C.-Y. Immune response to coccidioidomycosis and the development of a vaccine. Microorganisms 2017, 5, 13. [Google Scholar] [CrossRef]
- NIAID Valley Fever Research Working Group. NIAID Strategic Plan for Research to Develop a Valley Fever Vaccine. National Institute of Allergy and Infectious Disease. 2022; pp. 1–21. Available online: https://www.niaid.nih.gov/sites/default/files/niaid-strategic-plan-for-research-to-develop-a-valley-fever-vaccine9.9.22.pdf (accessed on 1 December 2022).
- Pappagianis, D. Evaluation of the protective efficacy of the killed Coccidioides immitis spherule vaccine in humans. The Valley Fever Vaccine Study Group. Am. Rev. Respir. Dis. 1993, 148, 656–660. [Google Scholar] [CrossRef]
- Hung, C.-Y.; Gonzalez, A.; Wüthrich, M.; Klein, B.S.; Cole, G.T. Vaccine immunity to coccidioidomycosis occurs by early activation of three signal pathways of T helper cell response (Th1, Th2, and Th17). Infect. Immun. 2011, 79, 4511–4522. [Google Scholar] [CrossRef]
- Narra, H.P.; Shubitz, L.F.; Mandel, M.A.; Trinh, H.T.; Griffin, K.; Buntzman, A.S.; Frelinger, J.A.; Galgiani, J.N.; Orbach, M.J. A Coccidioides posadasii CPS1 deletion mutant is avirulent and protects mice from lethal infection. Infect. Immun. 2016, 84, 3007–3016. [Google Scholar] [CrossRef]
- Shubitz, L.F.; Robb, E.J.; Powell, D.A.; Bowen, R.A.; Bosco-Lauth, A.; Hartwig, A.; Porter, S.M.; Trinh, H.; Moale, H.; Bielefeldt-Ohmann, H.; et al. Δcps1 vaccine protects dogs against experimentally induced coccidioidomycosis. Vaccine 2021, 39, 6894–6901. [Google Scholar] [CrossRef]
- Xue, J.; Chen, X.; Selby, D.; Hung, C.-Y.; Yu, J.-J.; Cole, G.T. A genetically engineered live attenuated vaccine of Coccidioides posadasii protects BALB/c mice against coccidioidomycosis. Infect. Immun. 2009, 77, 3196–3208. [Google Scholar] [CrossRef]
- Campuzano, A.; Zhang, H.; Ostroff, G.R.; Dos Santos Dias, L.; Wüthrich, M.; Klein, B.S.; Yu, J.-J.; Lara, H.H.; Lopez-Ribot, J.L.; Hung, C.-Y. CARD9-associated Dectin-1 and Dectin-2 are required for protective immunity of a multivalent vaccine against Coccidioides posadasii infection. J. Immunol. 1950, 204, 3296–3306. [Google Scholar] [CrossRef] [PubMed]
- Hung, C.-Y.; Zhang, H.; Castro-Lopez, N.; Ostroff, G.R.; Khoshlenar, P.; Abraham, A.; Cole, G.T.; Negron, A.; Forsthuber, T.; Peng, T.; et al. Glucan-chitin particles enhance Th17 response and improve protective efficacy of a multivalent antigen (rCpa1) against pulmonary Coccidioides posadasii infection. Infect. Immun. 2018, 86, e00070-18. [Google Scholar] [CrossRef] [PubMed]
- Hurtgen, B.J.; Hung, C.-Y.; Ostroff, G.R.; Levitz, S.M.; Cole, G.T. Construction and evaluation of a novel recombinant T cell epitope-based vaccine against coccidioidomycosis. Infect. Immun. 2012, 80, 3960–3974. [Google Scholar] [CrossRef] [PubMed]
- Das, R.; McNary, J.; Fitzsimmons, K.; Dobraca, D.; Cummings, K.; Mohle-Boetani, J.; Wheeler, C.; McDowell, A.; Iossifova, Y.; Bailey, R.; et al. Occupational coccidioidomycosis in California: Outbreak investigation, respirator recommendations, and surveillance findings. J. Occup. Environ. Med. 2012, 54, 564–571. [Google Scholar] [CrossRef]
- Nielsen-Gammon, J.W. The changing climate of Texas. In The Impact of Global Warming on Texas; University of Texas Press: Austin, TX, USA, 2011; Available online: http://www.jstor.org/stable/10.7560/723306 (accessed on 1 December 2022).
- Abatzoglou, J.T.; Dobrowski, S.Z.; Parks, S.A.; Hegewisch, K.C. TerraClimate, a high-resolution global dataset of monthly climate and climatic water balance from 1958–2015. Sci. Data 2018, 5, 1. [Google Scholar] [CrossRef]
- Sprigg, W.A.; Nickovic, S.; Galgiani, J.N.; Pejanovic, G.; Petkovic, S.; Vujadinovic, M.; Vukovic, A.; Dacic, M.; DiBiase, S.; Prasad, A.; et al. Regional dust storm modeling for health services: The case of valley fever. Aeolian Res. 2014, 14, 53–73. [Google Scholar] [CrossRef]
- Tong, D.Q.; Gorris, M.E.; Gill, T.E.; Ardon-Dryer, K.; Wang, J.; Ren, L. Dust storms, Valley fever, and public awareness. GeoHealth 2022, 6, e2022GH000642. [Google Scholar] [CrossRef]
- Comrie, A.C. No consistent link between dust storms and Valley fever (voccidioidomycosis). GeoHealth 2021, 5, e2021GH000504. [Google Scholar] [CrossRef]
- Smith, C.E.; Beard, R.R.; Rosenberger, H.G.; Whiting, E.G. Effect of season and dust control on coccidioidomycosis. J. Am. Med. Assoc. 1946, 132, 833–838. [Google Scholar] [CrossRef]
- Pappagianis, D.; Einstein, H. Tempest from Tehachapi takes toll or Coccidioides conveyed aloft and afar. West. J. Med. 1978, 129, 527–530. [Google Scholar]
- Williams, P.L.; Sable, D.L.; Mendez, P.; Smyth, L.T. Symptomatic coccidioidomycosis following a severe natural dust storm. An outbreak at the Naval Air Station, Lemoore, Calif. Chest 1979, 76, 566–570. [Google Scholar] [CrossRef] [PubMed]
- Prospero, J.M.; Ginoux, P.; Torres, O.; Nicholson, S.E.; Gill, T.E. Environmental characterization of global sources of atmospheric soil dust identified with the Nimbus 7 Total Ozone Mapping Spectrometer (TOMS) absorbing aerosol product. Rev. Geophys. 2002, 40, 2-1–2-31. [Google Scholar] [CrossRef]
- Baddock, M.C.; Bryant, R.G.; Acosta, M.D.; Gill, T.E. Understanding dust sources through remote sensing: Making a case for CubeSats. J. Arid Environ. 2021, 184, 104335. [Google Scholar] [CrossRef]
- Baddock, M.C.; Gill, T.E.; Bullard, J.E.; Acosta, M.D.; Rivera Rivera, N.I. Geomorphology of the Chihuahuan Desert based on potential dust emissions. J. Maps 2011, 7, 249–259. [Google Scholar] [CrossRef]
- Lee, J.A.; Gill, T.E.; Mulligan, K.R.; Dominguez Acosta, M.; Perez, A.E. Land use/land cover and point sources of the 15 December 2003 dust storm in southwestern North America. Geomorphology 2009, 105, 18–27. [Google Scholar] [CrossRef]
- Rivera Rivera, N.I.; Gill, T.E.; Bleiweiss, M.P.; Hand, J.L. Source characteristics of hazardous Chihuahuan Desert dust outbreaks. Atmos. Environ. 2010, 44, 2457–2468. [Google Scholar] [CrossRef]
- Kandakji, T.; Gill, T.E.; Lee, J.A. Drought and land use/land cover impact on dust sources in Southern Great Plains and Chihuahuan Desert of the U.S.: Inferring anthropogenic effect. Sci. Total Environ. 2021, 755, 142461. [Google Scholar] [CrossRef]
- Kandakji, T.; Gill, T.E.; Lee, J.A. Identifying and characterizing dust point sources in the southwestern United States using remote sensing and GIS. Geomorphology 2020, 353, 107019. [Google Scholar] [CrossRef]
- Lee, J.A.; Baddock, M.C.; Mbuh, M.J.; Gill, T.E. Geomorphic and land cover characteristics of aeolian dust sources in West Texas and eastern New Mexico, USA. Aeolian Res. 2012, 3, 459–466. [Google Scholar] [CrossRef]
- Kaplan, M.L.; Vellore, R.K.; Lewis, J.M.; Underwood, S.J.; Pauley, P.M.; Martin, J.E.; Rabin, R.M.; Krishnan, R. Subtropical-polar jet interactions in Southern Plains dust storms. J. Geophys. Res. Atmos. 2013, 118, 893–12914. [Google Scholar] [CrossRef]
- Schultz, J.A.; Meisner, B.N. The 24 February 2007 North Texas wind and dust storm: An impact weather event. Natl. Weather Dig. 2009, 33, 165–184. [Google Scholar]
- Ponette-González, A.G.; Collins, J.D.; Manuel, J.E.; Byers, T.A.; Glass, G.A.; Weathers, K.C.; Gill, T.E. Wet dust deposition across Texas during the 2012 drought: An overlooked pathway for elemental flux to ecosystems. J. Geophys. Res. Atmos. 2018, 123, 8238–8254. [Google Scholar] [CrossRef]
- Park, S.H.; Gong, S.L.; Zhao, T.L.; Vet, R.J.; Bouchet, V.S.; Gong, W.; Makar, P.A.; Moran, M.D.; Stroud, C.; Zhang, J. Simulation of entrainment and transport of dust particles within North America in April 2001 (“Red Dust Episode”). J. Geophys. Res. Atmos. 2007, 112, D20209. [Google Scholar] [CrossRef]
- Sprigg, W.A.; Gill, T.E.; Tong, D.Q.; Li, J.; Ren, L.; Pelt RS, V. Are opportunities to apply airborne dust research being missed? Bull. Am. Meteorol. Soc. 2022, 103, E1587–E1594. [Google Scholar] [CrossRef]
- Doggett, A.L.; Gill, T.E.; Peterson, R.E.; Bory, A.J.M.; Biscaye, P.E. Meteorological characteristics of a severe wind and dust emission event; southwestern USA, 6–7 April 2001. In Proceedings of the 21st Conference on Severe Local Storms, San Antonio, TX, USA, 11 August 2002; pp. 78–80. Available online: https://ams.confex.com/ams/pdfpapers/47573.pdf (accessed on 1 December 2022).
- Castañón-Olivares, L.R.; Mexican Coccidioidomycosis Study Group. Coccidiodin skin testing survey in México. In Proceedings of the 56th Coccidioidomycosis Study Group Meeting, Tucson, AZ, USA, 24 March 2012. [Google Scholar]
- Castañón Olivares, L.R.; Millán Chiu, B.; Valera Bermejo, A.; Zavala Velázquez, N.; Sánchez Paredes, E.; Aroch Calderón, A. Cases of Coccidioidomycosis in the Estados Unidos Mexicanos during the Period 1965–2004; 49th Coccidioidomycosis Study Group: Bass Lake, CA, USA, 2 April 2005. [Google Scholar]
- Gastélum-Cano, J.M.; Dautt-Castro, M.; García-Galaz, A.; Felix-Murray, K.; Rascón-Careaga, A.; Cano-Rangel, M.A.; Islas-Osuna, M.A. The clinical laboratory evolution in coccidioidomycosis detection: Future perspectives. J. Med. Mycol. 2021, 31, 101159. [Google Scholar] [CrossRef]
- Dirección General de Información en Salud. Cubos Dinámicos. 2022. Available online: http://www.dgis.salud.gob.mx/contenidos/basesdedatos/BD_Cubos_gobmx.html (accessed on 1 July 2022).
- Castillo-López, M.; Castañón Olivares, L.R.; Ponce-Rosas, R. El impacto de las condiciones ambientales en la respuesta a la intradermorreacción con coccidioidina en personas de Hermosillo, Son. In Proceedings of the IX Congreso Nacional de Micología Médica, Guadalajara, Jalisco, Mexico, 18–21 October 2017. [Google Scholar]
- Candolfi Arballo, O.; Cabañillas, L.; Castañón-Olivares, L.R. Resultados preliminares de la Intradermorreacción con Coccidioidina en cuatro zonas del Estado de Baja California; X Congreso Nacional de Micología Médica: Oaxtepec, Mexico, 2019. [Google Scholar]
- Texas Demographic Center. Demographic Trends and Population Projections for Texas and the North Texas Region. 2021. Available online: https://demographics.texas.gov/resources/presentations/osd/2021/2021_01_15_leadershipnorthtexas.pdf (accessed on 1 August 2022).
- US Census Bureau. QuickFacts Texas. 2022. Available online: https://www.census.gov/quickfacts/TX (accessed on 1 August 2022).
- US Census Bureau. Annual Estimates of the Resident Population for Counties in Arizona: April 1, 2010 to July 1, 2019 (CO-EST2019-ANNRES-04). 2020. Available online: https://www.census.gov/data/tables/time-series/demo/popest/2010s-counties-total.html (accessed on 1 August 2022).
- Texas Department of State Health Services. Table I Reported Diseases—Texas, 2009–2018; 2021. Available online: https://www.dshs.texas.gov/idps-home/infectious-disease-data-statistics/texas-annual-reports/texas-annual-reports-2010s/2018-annual-report (accessed on 1 August 2022).
- Mayo Clinic. Brucellosis. 2021. Available online: https://www.mayoclinic.org/diseases-conditions/brucellosis/symptoms-causes/syc-20351738 (accessed on 1 December 2022).
- Chow, N.A.; Kangiser, D.; Gade, L.; McCotter, O.Z.; Hurst, S.; Salamone, A.; Wohrle, R.; Clifford, W.; Kim, S.; Salah, Z.; et al. Factors influencing distribution of Coccidioides immitis in soil, Washington state, 2016. Msphere 2021, 6, e00598-21. [Google Scholar] [CrossRef]
- Litvintseva, A.P.; Marsden-Haug, N.; Hurst, S.; Hill, H.; Gade, L.; Driebe, E.M.; Ralston, C.; Roe, C.; Barker, B.M.; Goldoft, M.; et al. Valley fever: Finding new places for an old disease: Coccidioides immitis found in Washington state soil associated with recent human infection. Clin. Infect. Dis. 2015, 60, e1–e3. [Google Scholar] [CrossRef]
- Han, W.; Yang, Z.; Di, L.; Mueller, R. CropScape: A Web service based application for exploring and disseminating US conterminous geospatial cropland data products for decision support. Comput. Electron. Agric. 2012, 84, 111–123. [Google Scholar] [CrossRef]
- Horrigan, L.; Lawrence, R.S.; Walker, P. How sustainable agriculture can address the environmental and human health harms of industrial agriculture. Environ. Health Perspect. 2002, 110, 445–456. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).